Abstract
Background
Child malnutrition still remains a major cause of childhood morbidity and mortality in Bangladesh. This study aims to determine the prevalence and identify the associated risk factors of child malnutrition in Bangladesh using multilevel logistic regression model on data from the Bangladesh Demographic and Health Survey (BDHS), 2014.
Methods
A total sample of 6965 children aged 0–59 months was extracted from BDHS 2014. We performed descriptive analysis and multilevel generalized linear regression analysis with clustered data structure.
Results
Our findings show that among children the prevalence of moderate and severe values was respectively: 25 and 12% for stunting; 11 and 3.1% for wasting; 25 and 7.9% for underweight. The probability of stunting increased with age, with highest rate among children aged 36–47 months, which was significantly higher than children aged less than 6 months (OR = 6.71, 95% CI = 4.46, 10.10). Female children are found to be 11% less likely to be stunted than male children (OR = 0.89, 95% CI = 0.78, 1.02). Children with birth interval less than 24 months were significantly more likely to be stunted than children of first birth by 36% (OR = 1.36, 95% CI = 1.11, 1.67). Mothers with a normal BMI were 16% less likely to have children with stunting compared to mothers who are underweight (OR = 0.84, 95% CI = 0.76, 0.93). Other factors which were associated with a higher risk of stunting included parents with lower educational levels, children from the poorest wealth index, and mothers aged less than 20 years as first birth.
Conclusion
Government and non-government organization should generate effective program to aware women of reproductive age about adverse effect of short birth interval, and to aware parents about standard height and weight according to age and gender of children. Overall, necessary steps may be taken to make people educated and to reduce household wealth inequality to improve nutritional status of children.
Keywords: Child malnutrition, Stunting, Prevalence, Multilevel generalized linear regression, Odds ratio, Bangladesh
Background
Malnutrition is defined by the World Health Organization as any deficiencies, excesses, or imbalances in a person’s intake of energy and/or nutrients [1]. Child nutrition status is an imperative indicator of poverty in a population; and poverty, malnutrition and disease are intertwined each other [2, 3]. Malnutrition has been referred as the single greatest threat to the world’s public health, especially for the developing countries, by the World Health Organization [1]. The nutritional status of under-five children is the most sensitive indicator of a society, country as well as world public health status. Malnutrition is an underlying cause of 45% of child death- accounting for almost one-half of the global total of children’s deaths [4]. Rates of child malnutrition in Bangladesh are among the highest in the world, with rates of stunting affecting more than 54% of preschool-age children, underweight in 56% and wasting in 17% [5]. In Bangladesh, nutrition-attributable mortality rate in children is about 53 per 1000 live birth according to Bangladesh Demographic and Health Survey 2011 [6]. Survivors are left vulnerable to illnesses, stunted growth and intellectual impairment. The prevalence of stunting in children has been steadily decreasing, from 51% in 2004 to 37% in 2014 [7, 8]. However, the average annual rate of reduction (AARR) of stunting in Bangladesh is 2.7 which is much less than the required 3.9 AARR [9] to reach the global World Health Assembly (WHA) target to have 40% reduction in child malnutrition by 2025 [10]. At current rate, Bangladesh is not likely to achieve the WHA target for reducing childhood malnutrition.
To further enable decline of malnutrition rate in children and reach zero hunger goals as set by international targets, comprehensive preventive policies targeting evidence-based high-risk groups is crucial. Numerous studies have focused on child malnutrition in Bangladesh and/or it’s associated risk factors [11–39]. However, in studies assessing risk factors, most utilized standard logistic regression as the statistical model; few have used multivariate approach such as one study using Bangladesh Demographic and Health Survey (BDHS) data from 2011 [40], and multilevel analysis using BDHS data from 2007 [11]. This study clearly demonstrated the significant variation of child malnutrition to hierarchical factors such as residence and division. Therefore, to determine child malnutrition in correct level, the variation due to hierarchical factors should be adjusted in the model through method of multilevel analysis [41–44]. To fill this gap in literature using the most recent datasets, our study aimed to identify the significant risk factors of stunting among under-five children in Bangladesh using multilevel generalized linear regression model using BDHS 2014 data.
Methods
Sample selection
The data used for the present study has been derived from BDHS, 2014, a nationally-representative survey conducted by the National Institute for Population Research and Training (NIPORT) of the Ministry of Health and Family Welfare [45]. The 2014 BDHS collected data on the nutritional status of children by measuring the height and weight of all children aged between 0 and 59 months in the selected households. The sample for the BDHS-2014 is nationally representative and covers the entire population residing in non-institutional dwelling units in the country. The survey used a sampling frame from the list of enumeration areas (EAs) of the 2011 Population and Housing Census of the People’s Republic of Bangladesh, provided by the Bangladesh Bureau of Statistics (BBS). The primary sampling unit (PSU) for the survey is an EA created to have an average of about 120 households. With the design, the survey selected 18,000 residential households, which were expected to result in completed interviews with about 18,000 ever-married women of age 15–49 years. A total of 17,863 ever-married women of age 15–49 years were interviewed, for a response rate of 98% (Fig. 1). Details about the survey collection method can be found in literature [46]. For the current study, the data has been screened for the under-five children for whom height and weight are available (Fig. 2). Therefore, the study uses a sample of size 6965 extracted from 7886 of BDHS 2014 data.
Fig. 1.
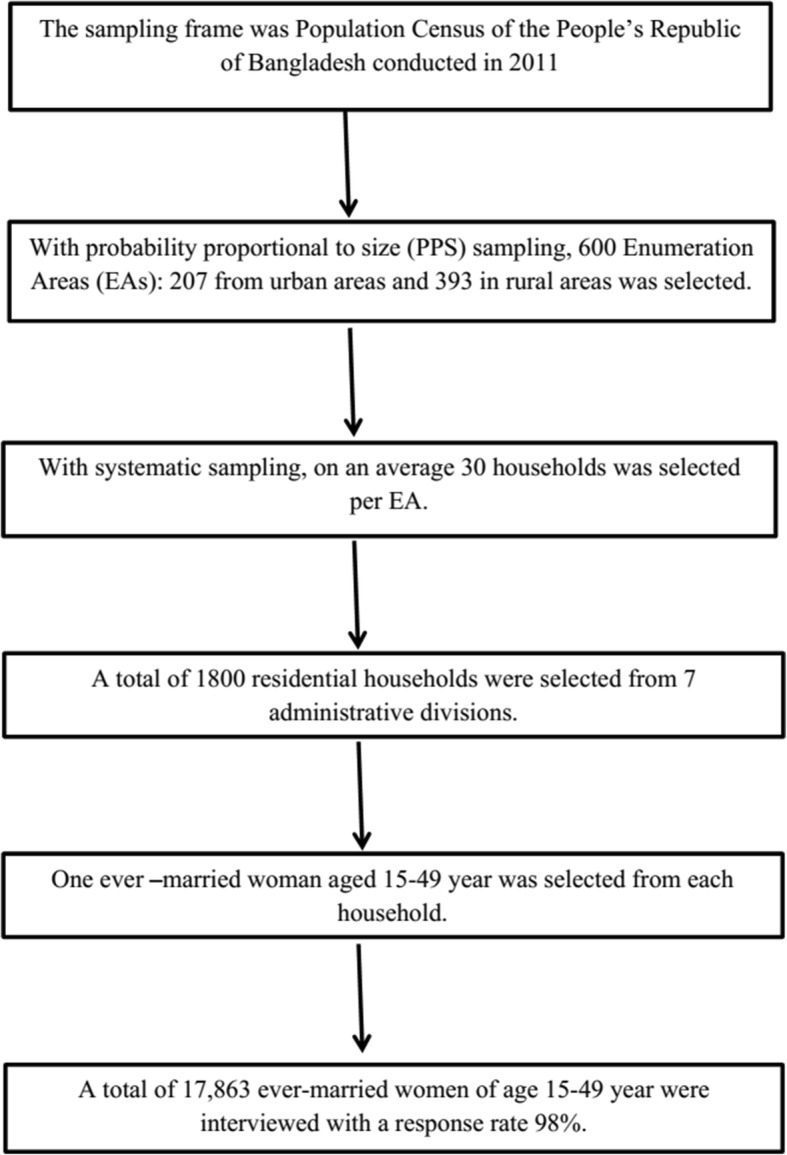
Study design of Bangladesh Demographic Health Survey, 2014
Fig. 2.
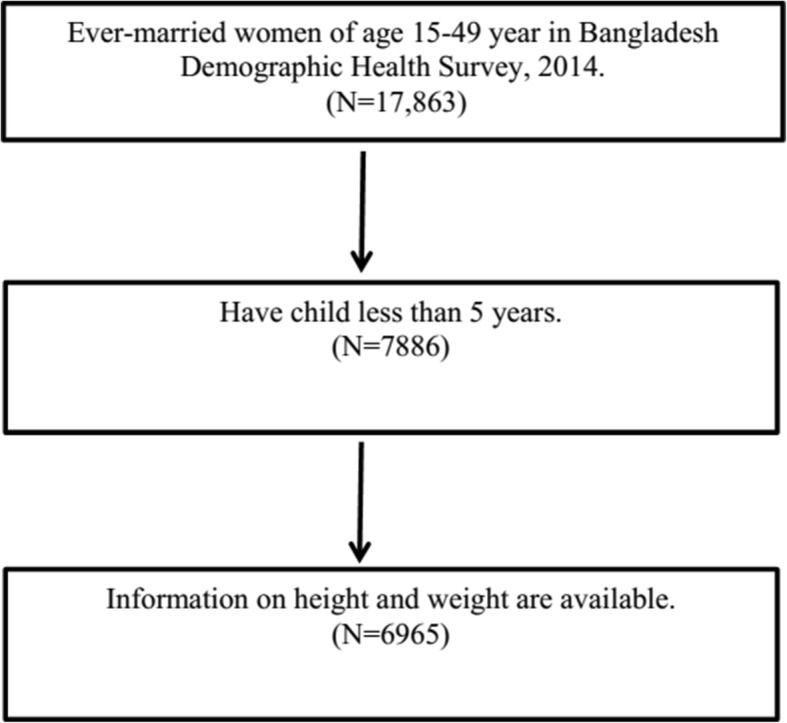
Data screening for under-five children in Bangladesh
Three standard indices of physical growth that describe the nutritional status of children are: (i) Height-for-age, (ii) Weight-for-height, and (iii) Weight-for-age. Each of these indices provides different information about growth and body composition that can be used to assess nutritional status of under-five children. The nutritional status of children in the survey population is compared with the World Health Organization (WHO) Child Growth Standards to create z-scores [46] resulting the indicators as stunting, wasting and underweight. Standard deviations below the reference median of the WHO reference population in terms of height-for-age was defined as stunted (− 2 SD) or severely stunted (− 3 SD). Similarly, standard deviations below the reference median of the WHO reference population in terms of weight-for-age was defined as wasted (− 2 SD) or severely wasted (− 3 SD); standard deviations below the reference median of the WHO reference population in terms of weight-for-height was defined as underweight (− 2 SD) or severely underweight (− 3 SD). However, z-scores computed for the three health indicators height-for-age, weight-for-height, and weight-for-age were used in this study.
Size of child at birth or a child’s birth weight was recorded based on mother’s perception [46]. A child’s birth weight less than 2.5 kg was considered as less than average, and lager than 2.5 was considered as larger than average. Mother’s BMI was classified as underweight if it was less than 18.5 kg/m2, normal if it was between 18.5–24.9 kg/m2, overweight if it was between 25 and 29.9 kg/m2, and obese if it was above 30 kg/m2. For the educational level, primary level was defined as completing grade 5, secondary level was defined as completing grade 10. The wealth index was created in three steps. In the first step, a subset of household indicators (for example, access to safe drinking water, sanitation facilities, structure of housing, crowdedness of housing, type of fuel used for cooking, household possessions etc.) common to urban and rural areas was used to create wealth scores for households in both areas. Categorical variables were transformed into separate dichotomous (0–1) indicators. Those indicators and those that were continuous were then examined using a principal components analysis to produce a common factor score for each household. In the second step, separate factor scores were produced for households in urban and rural areas using area specific indicators. The third step combined the separate area-specific factor scores to produce a nationally applicable combined wealth index by adjusting area-specific scores through a regression on the common factor scores. The resulting combined wealth index had a mean of zero and a standard deviation of one. Once the index was computed, national-level wealth quintiles (from lowest to highest) were obtained by assigning the household score to each de jure household member, ranking each person in the population by his or her score, and then dividing the ranking into five equal categories, each comprising 20% of the population. Computations for wealth index were done by the authority of the survey and details can be found in survey literature [46]. In this study, stunting was used as the indicator of nutritional status of under-five children and used as the response variable in generalized linear regression analysis.
Statistical analysis
We performed descriptive analysis to determine the characteristics of the study participants, which were presented with the frequency and percentage. Then, bivariate analyses were performed to compare child malnutrition (stunting, wasting and underweight) to the confounding variable. P-values had been obtained from bivariate simple linear regression to z-scores to check the association sex residence and division with child malnutrition. Lastly, multilevel generalized linear regression analysis had been performed with logit link and binomial family to identify significantly associated risk factors of child malnutrition. Various socio-demographic and economic variables were considered as risk factors. Division and residence of the respondents have been considered as the hierarchical variables. Two-level logistic regression (model-1 and model-2) and three level (model-3) logistic regression have been performed. In model-1 (two level) division has been considered as second level sources of variation; in model-2 (two level) residence has been considered as second level sources of variation; and in model-3 (three level) division has been considered as second level and residence has been as third level sources of variation. Statistical software StataSE version 13 (Stata Corp, USA) has been used to carry out statistical analyses. Missing values had been avoided in advanced analysis.
Results
A total of 6965 children aged 0–59 months had been included in the study, of whom 3571 (51.3%) were male and 3394 (48.7%) were female (Table 1). A significant percentage (19.1%) of children was below average size at birth. Among the mothers 73% gave their first birth at before age 20 years and 22.4% mothers were underweighted. About 20.9% mothers had no antenatal visits during pregnancy and 15.4% mothers had no formal education. Among the respondents 68.6% were from rural area and 21.7% were of poorest wealth index.
Table 1.
Characteristics of the study subjects, BDHS-2014
| Characteristic | Total (sample size = 6965) Frequency(Percentage) | Male (sample size =3571) | Female (sample size = 3394) |
|---|---|---|---|
| Frequency(Percentage) | Frequency(Percentage) | ||
| Age in months | |||
| mean | 29.56 | 29.42 | 29.72 |
| < 6 | 558 (8.01) | 302(8.46) | 256 (7.54) |
| 6–11 | 786 (11.28) | 396 (11.09) | 390 (11.49) |
| 12–23 | 1456 (20.90) | 744 (20.83) | 712 (20.98) |
| 24–35 | 1405 (20.17) | 719 (20.13) | 686 (20.21) |
| 36–47 | 1377 (19.77) | 701 (19.63) | 676 (19.92) |
| 48–59 | 1383 (19.86) | 709 (19.85) | 674 (19.86) |
| Size of child at birth | |||
| Very large | 96 (2.28) | 55 (2.55) | 41 (2.01) |
| Larger than average | 456 (10.84) | 251 (11.61) | 205 (10.03) |
| Average | 2849 (67.75) | 1466 (67.84) | 1383 (67.66) |
| Smaller than average | 544 (12.94) | 271 (12.54) | 273 (13.36) |
| Very small | 260 (6.18) | 118 (5.46) | 142 (6.95) |
| Live birth between births | |||
| Yes | 4 (0.09) | 2 (0.09) | 2 (0.10) |
| No | 4261 (99.91) | 2204 (99.91) | 2057 (99.90) |
| Preceding birth interval (months) | |||
| First birth | 2700 (38.84) | 1365 (38.31) | 1335 (39.40) |
| < 24 | 476 (6.85) | 243 (6.82) | 233 (6.88) |
| 24–47 | 1388 (19.97) | 733 (20.57) | 655 (19.33) |
| 48 + | 2387 (34.34) | 1222 (34.30) | 1165 (34.39) |
| Age of mother at 1st birth (years) | |||
| < 20 | 5085 (73.01) | 2608 (73.03) | 2477 (72.98) |
| 20–30 | 1838 (26.39) | 940 (26.32) | 898 (26.46) |
| 30 + | 42 (0.60) | 23 (0.64) | 19 (0.56) |
| Mother’s BMI | |||
| Underweight | 1556 (22.42) | 797 (22.41) | 759 (22.44) |
| Normal | 4067 (58.60) | 2096 (58.93) | 1971 (58.26) |
| Overweight | 1097 (15.81) | 543 (15.27) | 554 (16.38) |
| Obese | 220 (3.17) | 121 (3.40) | 99 (2.93) |
| Frequency of antenatal visits during pregnancy | |||
| No antenatal care visits | 848 (20.95) | 434 (20.80) | 414 (21.11) |
| Antenatal visits | 3196 (78.95) | 1651 (79.11) | 1545 (78.79) |
| Don’t know | 4 (0.10) | 2 (0.10) | 2 (0.10) |
| Duration of breastfeeding | |||
| Ever Breastfed | 535 (13.15) | 275 (13.13) | 260 (13.18) |
| Never breastfed | 46 (1.13) | 22 (1.05) | 24 (1.22) |
| Still breastfeeding | 3481 (85.59) | 1798 (85.82) | 1683 (85.34) |
| Don’t know | 5 (0.12) | 0 (0.00) | 5 (0.25) |
| Mother’s educational level | |||
| No education | 1076 (15.45) | 588 (16.47) | 488 (14.38) |
| Primary | 1934 (27.77) | 957 (26.80) | 977 (28.79) |
| Secondary | 3219 (46.22) | 1631 (45.67) | 1588 (46.79) |
| Higher | 736 (10.57) | 395 (11.06) | 341 (10.05) |
| Mother’s employment status | |||
| Yes | 1747 (25.09) | 885 (24.79) | 862 (25.40) |
| No | 5217 (74.91) | 2685 (75.21) | 2532 (74.60) |
| Father’s educational level | |||
| No education | 1736 (24.93) | 875 (24.50) | 861 (25.38) |
| Primary | 2100 (30.16) | 1047 (29.32) | 1053 (31.04) |
| Secondary | 2118 (30.42) | 1119 (31.34) | 999 (29.45) |
| Higher | 1009 (14.49) | 530 (14.84) | 479 (14.12) |
| Father’s occupation | |||
| Professional | 651 (9.38) | 335 (9.40) | 316 (9.35) |
| Sales | 1384 (19.94) | 705 (19.79) | 679 (20.09) |
| Agricultural-self employ | 642 (9.25) | 346 (9.71) | 296 (8.76) |
| Agricultural-employ | 1046 (15.07) | 527 (14.80) | 519 (15.36) |
| Services | 583 (8.40) | 272 (7.64) | 311 (9.20) |
| Skilled manual | 2460 (35.44) | 1280 (35.93) | 1180 (34.91) |
| Household and domestic | 132 (1.90) | 71 (1.99) | 61 (1.80) |
| Don’t work | 44 (0.63) | 26 (0.73) | 18 (0.53) |
| Division | |||
| Barisal | 812 (11.66) | 416 (11.65) | 396 (11.67) |
| Chittagong | 1320 (18.95) | 667 (18.68) | 653 (19.27) |
| Dhaka | 1213 (17.42) | 620 (17.36) | 593 (17.47) |
| Khulna | 774 (11.11) | 399 (11.17) | 375 (11.05) |
| Rajshahi | 875 (12.56) | 442 (12.38) | 433 (12.76) |
| Rangpur | 865 (12.42) | 456 (12.77) | 409 (12.05) |
| Sylhet | 1106 (15.88) | 571 (15.99) | 535 (15.76) |
| Type of Place of residence | |||
| Urban | 2188 (31.41) | 1129 (31.62) | 1059 (31.20) |
| Rural | 4777 (68.59) | 2442 (68.38) | 2335 (68.80) |
| Wealth index | |||
| Poorest | 1515 (21.75) | 794 (22.23) | 721 (21.24) |
| Poorer | 1307 (18.77) | 674 (18.87) | 633 (18.65) |
| Middle | 1379 (19.80) | 677 (18.96) | 702 (20.68) |
| Richer | 1420 (20.39) | 732 (20.50) | 688 (20.27) |
| Richest | 1344 (19.30) | 694 (19.43) | 650 (19.15) |
The data showed that among the children 12.2% were severely stunted, 24.9% were moderately stunted and 62.9% were well nourished (Table 2). It was found that 3.2% children were severely wasted and 11.7% were moderately wasted. About 8.3% of the children were found to be severely underweight, while 24.7% were moderately underweight.
Table 2.
Prevalence of stunting, wasting and underweight of under-five children in Bangladesh, BDHS-2014
| Category | Stunting (Height for age) Frequency (%) | Wasting (Weight for height) Frequency (%) | Underweight (Weight for age) Frequency (%) |
|---|---|---|---|
| Severely malnourished | 833 (11.96) | 213 (3.06) | 552 (7.93) |
| Moderately malnourished | 1714 (24.61) | 792 (11.37) | 1708 (24.52) |
| Normal (well-nourished) | 4418 (63.43) | 5960 (85.57) | 4705 (67.55) |
From Table 3, it had been found that stunting and underweight differ significantly to residence and division. It had been also found that rural children are more stunted than urban children and children of Sylhet division are mostly stunted. However, wasting differs significantly to gender, residence and division.
Table 3.
Comparing nutritional status of under-five children to gender, residence and division, BDHS-2014
| Category | Height for age (Stunted) | Weight for height (Wasted) | Weight for age (Underweight) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Severely malnourished Frequency (%) | Moderately malnourished Frequency (%) | Normal (Well- nourished) Frequency (%) | Severely malnourished Frequency (%) | Moderately malnourished Frequency (%) | Normal (Well- nourished) Frequency (%) | Severely malnourished Frequency (%) | Moderately malnourished Frequency (%) | Normal (Well- nourished) Frequency (%) | |
| Sex | |||||||||
| Male | 441 (12.35) | 900 (25.20) | 2230 (62.45) | 132 (3.70) | 411 (11.51) | 3028 (84.79) | 271 (7.59) | 874 (24.47) | 2426 (67.94) |
| Female | 392 (11.55) | 814 (23.98) | 2188 (64.47) | 81 (2.39) | 381 (11.23) | 2932 (86.39) | 281 (8.28) | 834 (24.57) | 2279 (67.15) |
| P-value | 0.092 | 0.008 | 0.329 | ||||||
| Residence | |||||||||
| Urban | 224 (10.24) | 479 (21.89) | 1485 (67.87) | 62 (2.83) | 196 (8.96) | 1930 (88.21) | 147 (6.72) | 445 (20.34) | 1596 (72.94) |
| Rural | 609 (12.75) | 1235 (25.85) | 2933 (61.40) | 151 (3.16) | 596 (12.48) | 4030 (84.36) | 405 (8.48) | 1263 (26.44) | 3109 (65.08) |
| P-value | < 0.001 | < 0.001 | < 0.001 | ||||||
| Division | |||||||||
| Barisal | 83 (10.22) | 225 (27.71) | 504 (62.07) | 34 (4.19) | 107 (13.18) | 671 (82.64) | 60 (7.39) | 212 (26.11) | 540 (66.50) |
| Chittagong | 186 (14.09) | 315 (23.86) | 819 (62.05) | 41 (3.11) | 152 (11.52) | 1127 (85.38) | 108 (8.18) | 339 (25.68) | 873 (66.14) |
| Dhaka | 122 (10.06) | 282 (23.25) | 809 (66.69) | 28 (2.31) | 121 (9.98) | 1064 (87.72) | 81 (6.68) | 253 (20.86) | 879 (72.46) |
| Khulna | 53 (6.85) | 166 (21.45) | 555 (71.71) | 24 (3.10) | 80 (10.34) | 670 (86.56) | 38 (4.91) | 168 (21.71) | 568 (73.39) |
| Rajshahi | 82 (9.37) | 182 (20.80) | 611 (69.83) | 32 (3.66) | 118 (13.49) | 725 (82.86) | 59 (6.74) | 218 (24.91) | 598 (68.34) |
| Rangpur | 87 (10.06) | 216 (24.97) | 562 (64.97) | 32 (3.70) | 105 (12.14) | 728 (84.16) | 74 (8.55) | 209 (24.16) | 582 (67.28) |
| Sylhet | 220 (19.89) | 328 (29.66) | 558 (50.45) | 22 (1.99) | 109 (9.86) | 975 (88.16) | 132 (11.93) | 309 (27.94) | 665 (60.13) |
| P-value | < 0.001 | 0.095 | < 0.001 | ||||||
Table 4 represents odds ratio (OR) with 95% confidence interval (CI) obtained from multilevel generalized linear regression with binomial family and logit link to nutritional status of under-five children. From the results of Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), Intraclass Correlation Coefficient (ICC) and Median Odds Ratio (MOR), Model-III was the best. Our results showed that the odds of being stunting significantly increased with age, with highest OR in 36–47 months age group (OR = 6.71, 95% CI = 4.56,10.10). Children of preceding birth interval of less than 24 months was also significantly associated with increased odds of stunting (OR = 1.36, 95% CI = 1.11, 1.67). Conversely, female children was found to be 11% less likely to be stunted than male children (OR = 0.89, 95% CI = 0.78, 1.02). Other risk factors which significantly reduced the OR of stunting included children of mothers with normal BMI (OR = 0.84, 95% CI = 0.76, 0.93), higher educational level in mother or father (OR = 0.71, 95% CI = 0.53, 0.97 and OR = 0.61, 95% CI = 0.53, 0.70 respectively), and children of richest wealth index (OR = 0.42, 95% CI = 0.31, 0.57).
Table 4.
Odds Ratio from multilevel generalized linear regression to stunting status of children in Bangladesh, BDHS-2014
| Variable | Odds Ratio (95% Confidence Interval) | ||
|---|---|---|---|
| Model 1a | Model 2b | Model 3 c | |
| Age in months | |||
| < 6 (RC) | 1.00 | 1.00 | 1.00 |
| 6–11 | 1.94 (1.27–2.97) | 1.89 (1.52–2.35) | 1.94 (1.27–2.96) |
| 12–23 | 5.08 (3.75–6.90) | 4.91 (3.82–6.32) | 5.09 (3.76–6.88) |
| 24–35 | 5.87 (4.15–8.28) | 5.72 (5.44–6.02) | 5.88 (4.16–8.31) |
| 36–47 | 6.71 (4.47–10.07) | 6.55 (5.96–7.20) | 6.71 (4.46–10.10) |
| 48–59 | 4.47 (3.07–6.51) | 4.40 (4.33–4.47) | 4.48 (3.08–6.53) |
| Sex of child | |||
| Male (RC) | 1.00 | 1.00 | 1.00 |
| Female | 0.89 (0.78–1.02) | 0.89 (0.85–0.93) | 0.89 (0.78–1.02) |
| Preceding birth interval (months) | |||
| First birth (RC) | 1.00 | 1.00 | 1.00 |
| < 24 | 1.36 (1.11–1.67) | 1.47 (1.22–1.77) | 1.36 (1.11–1.67) |
| 24–47 | 1.15 (0.96–1.39) | 1.25 (1.14–1.38) | 1.16 (0.96–1.40) |
| 48+ | 0.88 (0.77–1.02) | 0.88 (0.83–0.93) | 0.89 (0.77–1.02) |
| Age of mothers at 1st birth (years) | |||
| < 20 (RC) | 1.00 | 1.00 | 1.00 |
| 20–30 | 0.87 (0.77–0.98) | 0.90 (0.77–1.06) | 0.87 (0.76–0.98) |
| 31 + | 0.88 (0.48–1.59) | 0.90 (0.53–1.53) | 0.87 (0.49–1.56) |
| Mother’s BMI | |||
| Underweight (RC) | 1.00 | 1.00 | 1.00 |
| Normal | 0.84 (0.77–0.93) | 0.83 (0.78–0.89) | 0.84 (0.76–0.93) |
| Overweight | 0.62 (0.51–0.76) | 0.60 (0.54–0.67) | 0.62 (0.51–0.76) |
| Obese | 0.65 (0.46–0.93) | 0.60 (0.49–0.73) | 0.65 (0.46–0.92) |
| Mother’s educational level | |||
| No education (RC) | 1.00 | 1.00 | 1.00 |
| Primary | 0.96 (0.73–1.26) | 0.93 (0.90–0.97) | 0.96 (0.73–1.26) |
| Secondary | 0.76 (0.60–0.96) | 0.71 (0.61–0.83) | 0.76 (0.61–0.96) |
| Higher | 0.71 (0.52–0.97) | 0.64 (0.39–1.03) | 0.71 (0.53–0.97) |
| Mother’s employment status | |||
| No (RC) | 1.00 | 1.00 | 1.00 |
| Yes | 1.1 (0.99–1.24) | 1.03 (0.89–1.18) | 1.10 (0.98–1.23) |
| Father’s education level | |||
| No education (RC) | 1.00 | 1.00 | 1.00 |
| Primary | 0.85 (0.74–0.97) | 0.85 (0.85–0.85) | 0.85 (0.75–0.97) |
| Secondary | 0.69 (0.58–0.82) | 0.68 (0.57–0.79) | 0.70 (0.59–0.82) |
| Higher | 0.61 (0.52–0.70) | 0.59 (0.51–0.68) | 0.61 (0.53–0.70) |
| Father’s occupation | |||
| Professional (RC) | 1.00 | 1.00 | 1.00 |
| Sales | 1.04 (0.86–1.25) | 1.02 (0.86–1.22) | 1.03 (0.86–1.24) |
| Agricultural – self employ | 1.06 (0.79–1.43) | 1.03 (0.99–1.07) | 1.06 (0.79–1.42) |
| Agricultural - employ | 1.04 (0.79–1.37) | 1.02 (0.94–1.11) | 1.04 (0.79–1.36) |
| Services | 1.22 (0.98–1.53) | 1.24 (0.93–1.66) | 1.22 (0.97–1.52) |
| Skilled manual | 1.1 (0.82–1.46) | 1.08 (0.84–1.39) | 1.09 (0.82–1.45) |
| Household and domestic | 0.72 (0.51–1.02) | 0.81 (0.74–0.89) | 0.72 (0.50–1.03) |
| Don’t work | 1.16 (0.55–2.43) | 1.23 (1.09–1.38) | 1.16 (0.55–2.43) |
| Wealth index | |||
| Poorest (RC) | 1.00 | 1.00 | 1.00 |
| Poorer | 0.79 (0.63–0.99) | 0.80 (0.78–0.82) | 0.79 (0.63–0.99) |
| Middle | 0.77 (0.70–0.84) | 0.78 (0.74–0.82) | 0.77 (0.69–0.85) |
| Richer | 0.63 (0.49–0.82) | 0.64 (0.41–1.00) | 0.62 (0.47–0.82) |
| Richest | 0.43 (0.32–0.57) | 0.45 (0.31–0.65) | 0.42 (0.31–0.57) |
| No. of observation | 6900 | 6900 | 6900 |
| AIC | 8191.249 | 8243.575 | 8190.982 |
| BIC | 8464.82 | 8517.146 | 8471.393 |
| Intraclass Correlation Coefficient (ICC) | |||
| Division | 0.0166945 | 0.0146549 | |
| Residence | 0.0004238 | 0.0187098 | |
| Median Odds Ratio (MOR) | |||
| Division | 1.252 | 1.234 | |
| Residence | 1.036 | 1.117 | |
| Random-effects Parameters Estimate (95% CI) | |||
| Residence | 0.04 (0.00–0.57) | 0.12 (0.04–0.33) | |
| Division | 0.24 (0.13–0.42) | 0.22 (0.11–0.44) | |
| P-value | < 0.001 | 1.00 | < 0.001 |
RC stands for ‘reference category’
aModel 1: two level generalized linear regression considering division as second level hierarchical factor
bModel 2: two level generalized linear regression considering residential status as second level hierarchical factor
cModel 3: three level generalized linear regression considering residential status as third level and division as second level hierarchical factors
Discussion
In our multilevel analysis, we have found that children of age group 12–47 months, male, born with preceding birth interval less than 24 months, having underweight mothers, having mothers and fathers with lower education level and of poorest wealth index are more likely to be stunted.
Results from multilevel logistic regression show that as children grow up they become more likely to be stunted. This result is consistent with other studies in Bangladesh [17, 36] and also in neighboring countries: India [47], Nepal [48–50], China [51]. An increasing pattern of stunting by age is found to be undeviating with increasing pattern of communicable childhood diseases by age [52]. As discussed by Hong, Banta and Betancourt [23], this may partly be due to starting other foods along with breastfeeding to a child after 6 months of age, which increases the likelihood of taking polluted foods and minimizes the essential safety provided by breast milk. Moreover, children initiate crawling nearby at this age and are more probable to be carried out-of-doors, which makes them exposure to additional toxicities. Among the under five children, it is most likely to be stunted between age 12–47 months. Therefore, caring at early childhood is more likely to be protective and stunting becomes more prospective as the child becomes more dependent for caloric intake from foods which should be improved. More elaborative researches are needed to demonstrate in this regard.
Male children are found to be insignificantly more stunted than female. Gender has been identified a risk factor in many studies [25, 30, 33, 34]. Standard binary logistic regression (single level) also gave insignificant evidence about gender to be determinant of child malnutrition with BDHS-2014 data [17].
Coherent with other studies [26, 30, 33, 34] children of second birth order with less than 24 months birth interval are more likely to be stunted than children of first birth order and children of second birth order with more than 48 months birth interval. The association between stunting and second-order births with shorter interval may be due to competition for food within a household and mother may fail to take care two babies together within limited household.
Similar to our findings some studies confirmed association of child malnutrition with mother’s malnutrition [53]. In a traditionally patriarchal society such as Bangladesh, the availability and accessibility of nutritious foods for under-five children is highly dependent on the conduct of maternal duties and responsibilities towards their children which may be impaired when mothers are malnourished.
Education of parents is found to be a preventive factor of child malnutrition which is expected. Education always plays a positive role in health and diseases [37, 39]. Educated parents have more knowledge about health, nutrition, proper child care, health services, hygiene, proper food for children etc. Educated parents also contribute positively to promote the household income which is supportive to provide nutritional diet to their children. Moreover, Islam and his colleagues [54] discussed in this aspect that educated mothers are able to use insufficient family income and offered healthcare services efficiently, can minimize the family size, can sustain improved health stimulating behaviors and can afford better healthcare to their children [55, 56]. All these features may subsidize to keep children in virtuous nourishment.
Nutritional status is called a reflecting indicator of a family’s economic condition. This study also shows that children of families with poorest wealth index are most likely to be stunted, as found in other studies conducted in Bangladesh and in other countries [46–50, 57, 58]. This can be attributed to the fact that higher socioeconomic households have more ability to allocate necessary resources regarding nutrition for their children than poorer families. Reasonably allocation of more resources to their children improves their health conditions by reducing multiple health risks.
However, parent’s employment status does not found to have any significant role in managing child malnutrition.
Main strength of the study is that the data used in this study is a nationally representative, large sample size and enough information on child malnutrition. The study also has some limitations. The data don’t have information on some important factors like amount of diet given to children, mobility pattern of children etc. Some existed variables in the data including size of child at birth, antenatal visits, duration of breast feeding etc. are not included in the model due to a lot of missing information.
Conclusion
In conclusion, this study clearly reveals that multilevel modeling should be used for hierarchical data to predict significant determinant child malnutrition in correct level. This study also has been identified using multilevel generalized linear regression model that under-five children who are male, of second birth order with less than 24 months, of underweight mothers, of lower educated parents and of poorest family are on high risk to be stunted. Therefore, policy makers and government should pay their attention more to take proper initiative to promote nutritional status in Bangladesh. Government may take necessary steps to aware women of reproductive age about adverse effect of short birth interval. Government and non-government organizations related to the health and nutrition should generate effective program to increase awareness of parents about the standard height and weight according to age and gender of the children. In addition, government may implement child care leave for employed parents with under-five children. Government also may establish childcare center with proper infrastructure, so that employed parents are not obligatory to leave their children at home under illiterate maid. Government may also encourage employed couples to stay with their older parents (or relatives) through some intervention to avoid the same. Overall, necessary steps may be taken to make people educated and to reduce household wealth inequality to improve nutritional status of children.
Acknowledgements
Authors would like to acknowledge Jenny Jung, Yale Fox International Fellow, Yale University, New Haven, CT, United States of America for her constructive feedback to update the paper in English.
Abbreviations
- AARR
Average Annual Rate of Reduction
- AIC
Akaike Information Criterion
- BDHS
Bangladesh Demographic and Health Survey
- BIC
Bayesian Information Criterian
- BMI
Body Mass Index
- CI
Confidence Interval
- ICC
Intraclass Correlation Coefficient
- MOR
Median Odds Ratio
- NIPRT
National Institute of Population Research and Training
- OR
Odds Ratio
- SD
Standard Deviation
- WHA
World Health Assembly
- WHO
World Health Organization
Authors’ contributions
Access of data and material collection: PS. Statistical analysis and interpretation: PS and MMR. Drafting the manuscript: PS, MMR and JA. Contributed to discussion and finishing: PS, MMR and JA. All authors have read and approved the manuscript.
Funding
Not applicable.
Availability of data and materials
Available at: https://dhsprogram.com.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Papia Sultana, Email: papia.stat@ru.ac.bd.
Md. Mahfuzur Rahman, Email: mdmahfuzur08@gmail.com.
Jahanara Akter, Email: jahanaraju1978@gmail.com.
References
- 1.World Health Organization. [cited 2019 Mar 10]. Available from: https://www.who.int/topics/malnutrition/en/.
- 2.Pena M, Bacallao J. Malnutrition and poverty. Annu Rev Nutr. 2002;22:241–253. doi: 10.1146/annurev.nutr.22.120701.141104. [DOI] [PubMed] [Google Scholar]
- 3.Farhadi S, Ovchinnikov RS. The relationship between nutrition and infectious diseases: a review. Biomed Biotechnol Res J. 2018;2:168–172. doi: 10.4103/bbrj.bbrj_69_18. [DOI] [Google Scholar]
- 4.World Health Organization. [cited 2019 Mar 10]. Available from: https://www.who.int/news-room/fact-sheets/detail/malnutrition.
- 5.Nutrition country profiles: Bangladesh. [cited 2019 Mar 10]. Available from: http://www.fao.org/ag/agn/nutrition/bgd_en.stm.
- 6.Hossain A, Islam S, Munira S, Farzana S, Sarker S, Ahmed R, et al. Infant and child mortality status of Bangladesh: a study on demographic and health survey. Asian J Soc Sci Stud. 2018;3(10):43–53. doi: 10.20849/ajsss.v3i1.330. [DOI] [Google Scholar]
- 7.Bangladesh demographic and health survey (BDHS), 2007. Dhaka: National Institute of Population Research and Training; 2007. p. 346. [cited 2017 Oct 24]. Available from: https://www.unicef.org/bangladesh/BDHS2007_Final.pdf.
- 8.Bangladesh Demographic and Health Survey (BDHS), 2011. Dhaka: NIPORT, Mitra and Associates, and ICF International; 2013. [cited 2017 Oct 24]. Available from: https://dhsprogram.com/pubs/pdf/fr265/fr265.pdf.
- 9.de Onis M, Dewey KG, Borghi E, Onyango AW, Blössner M, Daelmans B, et al. The World Health Organization's global target for reducing childhood stunting by 2025: rationale and proposed actions. Matern Child Nutr. 2013;9(2):6–26. doi: 10.1111/mcn.12075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Global target 2025. [cited 2017 Oct 24]. Available from: https://www.who.int/nutrition/global-target-2025/en/.
- 11.Alom J, Quddus MA, Islam MA. Nutritional status of under-five children in Bangladesh: a multilevel analysis. J Biosoc Sci. 2012;44(05):525–535. doi: 10.1017/S0021932012000181. [DOI] [PubMed] [Google Scholar]
- 12.McGregor GS, Cheung YB, Cueto S, Glewwe P, Richter L, Strupp B. Development potential in the first 5 years for children in developing countries. Lancet. 2007;369(9555):60–70. doi: 10.1016/S0140-6736(07)60032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Faruque ASG, Ahmed AMS, Ahmed T, Islam MM, Hossain MI, Roy SK, et al. Nutrition: basis for healthy children and mothers in Bangladesh. J Health Popul Nutr. 2008;26(3):325–339. doi: 10.3329/jhpn.v26i3.1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hasan MT, Soares MRJ, Williams GM, Mamun AA. Forecasting the progress towards the target of millennium development goal 1C in children under 5 years of age in Bangladesh. Public Health Nutr. 2015;18(10):1728–1736. doi: 10.1017/S1368980014003279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahmed CN, Hossain T, Mandal MI, Mothabbir BN, Rahman G, Islam M, et al. Community-based management of acute malnutrition in Bangladesh: feasibility and constraints. Food Nutr Bull. 2014;35:277–285. doi: 10.1177/15648265140352S103. [DOI] [PubMed] [Google Scholar]
- 16.Bairagi R, Chowdhury MK. Socioeconomic and anthropometric status and mortality of young children in rural Bangladesh. Int J Epidemiol. 1994;23:1179–1184. doi: 10.1093/ije/23.6.1179. [DOI] [PubMed] [Google Scholar]
- 17.Das S, Gulshan J. Different forms of malnutrition among under five children in Bangladesh: a cross sectional study on prevalence and determinants. BMC Nutrition. 2017;3:1. doi: 10.1186/s40795-016-0122-2. [DOI] [Google Scholar]
- 18.Das S, Hossain MZ. Levels and determinants of child undernutrition in Bangladesh. Pak J Nutr. 2008;24:301–323. [Google Scholar]
- 19.Das S, Hossain MZ, Islam MA. Predictors of child chronic malnutrition in Bangladesh. Proc Pak Acad Sci. 2008;45:137–155. [Google Scholar]
- 20.Das S, Rahman RM. Application of ordinal logistic regression analysis in determining risk factors of child malnutrition in Bangladesh. Nutr J. 2011;10(1):124. doi: 10.1186/1475-2891-10-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fakir AMS, Khan MWR. Determinants of malnutrition among urban slum children in Bangladesh. Health Econ Rev. 2015;5:22. doi: 10.1186/s13561-015-0059-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hasan MT, Magalhaes RJS, Williams GM, Mamun AA. The role of maternal education in the 15-year trajectory of malnutrition in children under 5 years of age in Bangladesh. Matern Child Nutr. 2016;12(4):929–939. doi: 10.1111/mcn.12178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hong R, Banta JE, Betancourt JA. Relationship between household wealth inequality and chronic childhood under-nutrition in Bangladesh. Int J Equity Health. 2006;5:15. doi: 10.1186/1475-9276-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Islam A, Biswas T. Chronic Stunting among under 5 children in Bangladesh a Situation Analysis. Adv Pediatr Res. 2015;2:18. [Google Scholar]
- 25.Islam MS, Jothi JS, Islam M, Huq AKO. Nutritional status of rural and urban under-five children in Tangail District, Bangladesh. Int J Innov Appl Stud. 2014;8(2):841–848. [Google Scholar]
- 26.Jesmin A, Yamamoto SS, Malik AA, Haque A. Prevalence and determinants of chronic malnutrition among preschool children: A cross-sectional study in Dhaka City, Bangladesh. J Health Popul Nutr. 2001;29:494–509. doi: 10.3329/jhpn.v29i5.8903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khan REA, Raza MA. Nutritional status of children in Bangladesh: measuring composite index of anthropometric failure (CIAF) and its determinants. Pakistan J Commerce Soc Sci. 2014;8(1):11–23. [Google Scholar]
- 28.Mohsena M, Goto R, Taylor CGNM. Socioeconomic and demographic variation in nutritional status of under-five Bangladeshi children and trend over the twelve-year period 1996–2007. J Biosoc Sci. 2017;49(2):222–238. doi: 10.1017/S0021932016000328. [DOI] [PubMed] [Google Scholar]
- 29.Mondal D, Minak J, Alam M, Liu Y, Dai J, Korpe P, et al. Contribution of enteric infection, altered intestinal barrier function, and maternal malnutrition to infant malnutrition in Bangladesh. Infect Dis Soc Am. 2011;54(2):185–192. doi: 10.1093/cid/cir807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mostafa KS. Socio-economic determinants of severe and moderate stunting among under-five children of rural Bangladesh. Malays J Nutr. 2011;17(1):105–118. [PubMed] [Google Scholar]
- 31.Muaz SSA, Hasan MR, Shamim SA, Dev A, Kamar S. Nutritional status of 1-5 years children of the tea Workers in Sylhet Division. Bangladesh J Child Health. 2010;34(1):11–16. doi: 10.3329/bjch.v34i1.5696. [DOI] [Google Scholar]
- 32.Rahman A, Biswas SC. Nutritional status of Under-5 children in Bangladesh. S Asian J Popul Health. 2009;2(1):1–11. [Google Scholar]
- 33.Rahman A, Chowdhury S, Hossain D. Acute malnutrition in Bangladeshi children: levels and determinants. Asia Pac J Public Health. 2009;21(3):294–302. doi: 10.1177/1010539509335399. [DOI] [PubMed] [Google Scholar]
- 34.Rayhan MI, Khan MSH. Factors causing malnutrition among under five children in Bangladesh. Pak J Nutr. 2006;5(6):558–562. doi: 10.3923/pjn.2006.558.562. [DOI] [Google Scholar]
- 35.Srinivasan CS, Zanello G, Shankar B. Rural-urban disparities in child nutrition in Bangladesh and Nepal. BMC Public Health. 2013;13:581. doi: 10.1186/1471-2458-13-581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Talukder A. Factors associated with malnutrition among under-five children: illustration using Bangladesh demographic and health survey, 2014 data. Children. 2017;4:88. doi: 10.3390/children4100088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rahman MS, Howlader T, Masud MS, Rahman ML. Association of Low-Birth Weight with Malnutrition in Children under Five Years in Bangladesh: Do Mother’s Education, Socio-Economic Status, and Birth Interval Matter? PloS One. 2016;11(6):e0157814. doi: 10.1371/journal.pone.0157814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ahmed T, Mahfuz M, Ireen S, Ahmed AMS, Rahman S, Islam MM, et al. Nutrition of children and women in Bangladesh: trends and directions for the future. J Health Popul Nutr. 2012;30(1):1–11. doi: 10.3329/jhpn.v30i1.11268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rahman MM, Saima U, Goni MA. Impact of maternal household decision-making autonomy on child nutritional status in Bangladesh. Asia Pac J Public Health. 2015;27(5):509–520. doi: 10.1177/1010539514568710. [DOI] [PubMed] [Google Scholar]
- 40.Rabbi AMF, Karmaker SC. Determinants of child malnutrition in Bangladesh – a multivariate approach. Asian J Med Sci. 2014;6(2):85–90. doi: 10.3126/ajms.v6i2.10404. [DOI] [Google Scholar]
- 41.Goldstein H. Multilevel Statistical Models. 2. London: Edward Arnold; 1995. [Google Scholar]
- 42.Snijders TAB, Bosker RJ. Multilevel analysis - an introduction to basic and advanced multilevel modeling. Thousand Oaks: CA SAGE Publications; 1999. [Google Scholar]
- 43.Akombi BJ, Agho KE, Hall JJ, Merom D, Burt TA, Renzaho AMN. Stunting and severe stunting among children under-5 years in Nigeria: a multilevel analysis. BMC Pediatr. 2017. 10.1186/s12887-016-0770-z. [DOI] [PMC free article] [PubMed]
- 44.Alemu ZA, Ahemed AA, Yalew AW, Birhanu BS, Zaitchik BF. Individual and community level factors with a significant role in determining child height-for-age Z score in east Gojjam zone, Amhara regional state, Ethiopia: a multilevel analysis. Archives of Public Health. 2017. 10.1186/s13690-017-0193-9. [DOI] [PMC free article] [PubMed]
- 45.Bangladesh Demographic and Health Survey (BDHS), 2014. Dhaka: NIPORT, Mitra and Associates, and ICF International; 2016. [cited 2017 Oct 24]. Available from: https://dhsprogram.com/pubs/pdf/FR311/FR311.pdf.
- 46.National Institute of Population Research and Training - NIPORT/Bangladesh, Mitra and Associates/Bangladesh, and ICF International. Bangladesh Demographic and Health Survey 2014. Dhaka: NIPORT, Mitra and Associates, and ICF International; 2016. [cited 2016 Apr 8]. Available from: https://dhsprogram.com/pubs/pdf/FR311/FR311.pdf.
- 47.Meshram II, Arlappa N, Balakrishna N, Mallikharjuna Rao K, Laxmaiah A, Brahmam GN. Trends in the prevalence of under-nutrition, nutrient and food intake and predictors of under-nutrition among under five year tribal children in India. Asia Pac J Clin Nutr. 2012;21(4):568–576. [PubMed] [Google Scholar]
- 48.Sah N. Determinants of child malnutrition in Nepal: a case analysis from Dhanusha, central Terai of Nepal. J Nepal Health Res Counc. 2004;2(2):50–55. [Google Scholar]
- 49.Sapkota VP, Gurung CK. Prevalence and predictors of underweight, stunting and wasting in under-five children. J Nepal Health Res Counc. 2009;7(15):120–126. [Google Scholar]
- 50.Ruwali D. Nutritional status of children under five years of age and factors associated in Padampur VDC, Chitwan. Health Prospect. 2011;10:14–18. doi: 10.3126/hprospect.v10i0.5639. [DOI] [Google Scholar]
- 51.Zhai F-Y, Wang H-J, Chang S-Y, Fu D, Ge K, Popkin BM. The current status, trend, and influencing factors to malnutrition of infants and children in China. J Community Nutr. 2004;6(2):78–85. [Google Scholar]
- 52.Casa JA, Dachs N, Bambas A. Health disparities in Latin America and the Caribbean: The role of social and economic determinants. Washington DC: Pan American Health Organization; 2001. pp. 22–49. [Google Scholar]
- 53.Khalid N, Aslam Z, Kausar F, Irshad H, Anwer P. Maternal malnutrition and its kick on child growth: an alarming trim for Pakistan. J Food Nutr Popul Health. 2017;1(3):24. [Google Scholar]
- 54.Islam MM, Alam M, Tariquzzaman M, Kabir MA, Pervin R, Begum M, Khan MMH. Predictors of the number of under-five malnourished children in Bangladesh: application of the generalized poisson regression model. BMC Public Health, 2013; 13(11). Doi:10.1186/1471-2458-13-11. [DOI] [PMC free article] [PubMed]
- 55.Hien NN, Kam S. Nutritional status and the characteristics related to malnutrition in children under five years of age in Nghean, Vietnam. J Prev Med Publ Health. 2008;41(4):232–240. doi: 10.3961/jpmph.2008.41.4.232. [DOI] [PubMed] [Google Scholar]
- 56.Frost MB, Forste R, Haas DW. Maternal education and child nutritional status in Bolivia: finding the links. Soc Sci Med. 2005;60(2):395–407. doi: 10.1016/j.socscimed.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 57.Babatunde RO, Olagunju FI. Prevalence and determinants of malnutrition among under-five children of farming households in Kwara state, Nigeria. J Agric Sci. 2011;3(3):173–181. [Google Scholar]
- 58.Sarkar D, Haldar SK. Socioeconomic Determinants of Child Malnutrition in India: Evidence from NFHS-III. 2014. [cited 2017 Oct 24]. Available from: http://ssrn.com/abstract=2420293 or 10.2139/ssrn.2420293.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Available at: https://dhsprogram.com.


