Supplemental Digital Content is available in the text.
Keywords: emergency medicine, medical education, quality improvement, trauma management
Introduction
A precise tool for analysis of trauma team performance is missing.
Objectives
To create a framework for trauma team performance analysis and feedback.
Methods
An observational study in a level I trauma centre in Lithuania was performed from January 1 2017 to August 31 2017. Audio/video review process was used to evaluate technical and nontechnical performance of the trauma team.
Results
In total, 143 trauma team activations were analysed. The mean rate of completion for the primary survey based on Advanced Trauma Life Support principles was 68.5%. Technical steps of patient resuscitation were measured in seconds during first hour of the treatment. The T-NOTECHS scale mean score was 11.99 (SD 2.9).
Conclusion
During the study period, we were able to measure the time needed for certain steps in trauma patient evaluation and management. Based on this analysis, a performance improvement program will be devised, including the HybridLab medical simulation, audio/video debriefing, and individualised feedback sessions.
Introduction
As a result of several studies published in the past decade that extrapolated the number of deaths due to medical errors, awareness of patient safety has risen significantly in all medical fields and institutions. Many strategies have been developed to mitigate errors and improve delivery of care [1–3]. Despite the well known importance of the role of the trauma team in management of severely injured patients, trauma care is considered the ‘perfect storm’ for errors [4]. Recent studies have reported that preventable deaths in trauma range from 2 to 29% [5–7]. Following analysis of the trauma care procedures, it seems that the emergency department is the most common location in which errors occur and human errors predominate [8].
Because nothing can be improved until it is measured, most of the mature trauma centres are using trauma registries’ data to audit trauma system [9], and based on the audit results various quality improvement programs are being conducted. However, data in the registries may not be in the best quality or missing [10]. In addition, trauma care quality indicators are still being debated [11].
In the era of new technologies and artificial intelligence, a tool for more precise analysis of trauma team technical and nontechnical performance is missing. The aim of this study was to create a framework for trauma team performance analysis in the emergency department.
Methods
Study setting
The study was conducted in the level 1 trauma centre Hospital of the Lithuanian University of Health Sciences Kauno Klinikos, which has 63 000 emergency visits annually. Ethics approval was obtained from the local bioethics committee. We agreed with the hospitals’ legal department that video registration was to be used only for quality control purposes. As long as the patients remained anonymous, informed consent was not required. The study was conducted from 1 January 2017 to 31 August 2017. All adult patients (≥18 years of age) who were resuscitated by the trauma team in the emergency department were included in the study. Demographic data were collected from the trauma registry. Trauma team members were not aware of the remote evaluation.
All data were analyzed using descriptive analysis with IBM SPSS statistics version 20. Data presented in frequency tables and mean ± SD.
Characteristics of the trauma team
In our institution, trauma teams were trained and formed in 2011. We are using two-tiered activation model (activation criteria are shown in Supplemental digital content 1, http://links.lww.com/EJEM/A255) where full trauma team is called the red team and reduced team yellow. The yellow team includes intensive care doctor, senior and junior surgical resident, trauma resident, radiology resident, and two nurses. The red team includes the same as the yellow team, plus surgical and trauma attendings. Not all of the members of the trauma team have an up to date Advanced Trauma Life Support (ATLS) certification. The trauma team activation system ensures the timely presence of the required specialists.
Data recording equipment and methods
The HybridLab system was installed in trauma bays for audit, quality assurance, and in situ bedside training purposes. Data protection was ensured by a service provider according to ISO-27000 data safety standards and European Union`s General Data Protection Regulation requirements.
Each trauma bay (TB1 and TB2) was equipped with three ceiling-mounted (height, 2.95 m) cameras that recorded high-resolution video and audio. We used DH-IPC-K200A cameras, which have full HD (1920 × 1080) recording capabilities with built-in microphones and three-dimensional noise reduction system. All cameras had the same lenses with an 86.5° viewing angle. Two cameras were located on the sides of the room and one was located at the back of the room for optimal viewing of the patient care area (Supplemental digital content 1, http://links.lww.com/EJEM/A255). Video and audio streams were stored on a DH-NVR5832 network video recorder, which has 32 TB of storage and is capable of recording, playback, and viewing. All recordings were available for one month following the event before being overwritten and were accessible to the researcher through secure login to ‘Smart Pro Surveillance System’.
Technical data collection
A specially designed application was created for precise measurement in seconds of time needed to complete specific tasks described in the ATLS guidelines. The timer was started when the patient entered the trauma bay. Because it is believed that the first hour is the most important [12], we evaluated no more than one hour of the recordings. Measured tasks included the following: time to decision to intubate, perform needle decompression, or chest drainage and duration from decision to action completed; time to pulse oximeter, heart monitor, blood pressure cuff attached, thorax and abdomen palpation, chest auscultation, thigh palpation, intravenous access, blood samples collected, temperature measured, protection from hypothermia, analgesia, back examined, Foley catheter; duration and time to radiological test results, eFAST, chest, and pelvic radiograph, head and neck computed tomography. We did not measure the time needed for immobilization because all trauma patients were fully immobilized by the emergency medical service.
Nontechnical data collection
Each trauma team was evaluated using the T-NOTECHS scale [13], which consists of five behaviour domains that were identified by an expert panel of trauma practitioners based on scoring instruments for existing teamwork and nontechnical skills: (1) leadership, (2) cooperation and resource management, (3) communication and interaction, (4) assessment and decision making, and (5) situation awareness/coping with stress. Each domain was scored on a five-point Likert scale.
Results
Demographics
During the study period, there were 162 trauma team activations, and 143 were analysed (19 cases were lost due to recording problems). Because trauma registry data are not linked to the ‘black box’ date, demographics were calculated for 162 patients. There were 112 (69.1%) males, with an average age of 44.1 years (SD 17.84). Prehospital average revised trauma score (RTS) was 7.54 (SD 0.79), and hospital average RTS was 7.59 (SD 0.71). Mechanisms of injury were as follows: penetrating 16 (9.9%) and blunt 146 (90.1%). Average injury severity score (ISS) was 10.3 (SD 7.89); and ISS greater than 15 was 26 (16%). Eight (5.6%) trauma team patients died.
Advanced Trauma Life Support compliance rate
The compliance rate for the ATLS protocol was based on completion of 11 items for the primary survey (Supplemental digital content 1, http://links.lww.com/EJEM/A255). None of the patients were evaluated with a secondary survey. The mean rate of completion for the primary survey was 68.5%.
Resuscitation times
Mean time from arrival to emergency department trauma bay to performance of various tasks needed for trauma patient evaluation and resuscitation was measured in minutes and seconds (Fig. 1 and Supplemental digital content 1, http://links.lww.com/EJEM/A255).
Fig. 1.
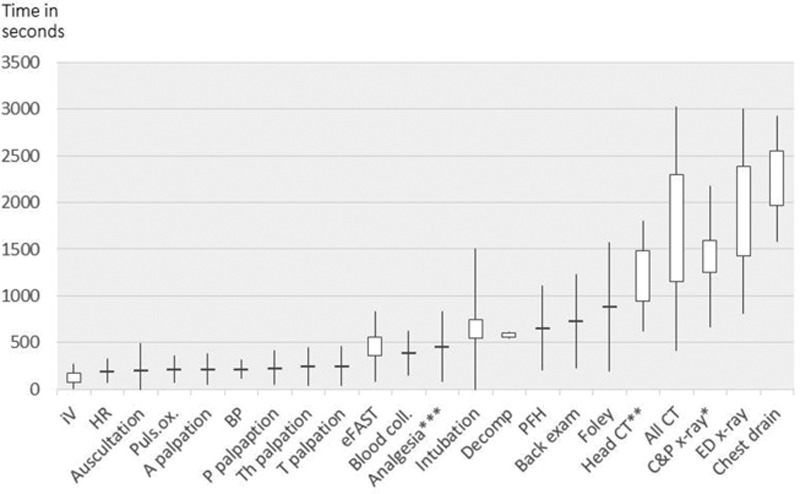
Resuscitation times. *Only the patients of whom radiographs were made in the shock room (C&P n = 24; ED radiograph n = 45). **Only the patients of whom head/neck CT were made (head/neck CT n = 51; all CT n = 32). ***Out 51 out of 84 patients of who required analgesic. A, abdomen; BP, blood pressure; C&P, chest and pelvis; CT, computed tomography; Decomp, needle decompression; ED, radiographs made not in the trauma bay; HR, heart rate; PFH, protection from hypothermia; T, thorax; Th, thigh.
We were able to measure very precisely vital signs and physical evaluation times (Supplemental digital content 1, http://links.lww.com/EJEM/A255). We registered all the procedures needed according to protocol and timing. For example, in 97% of cases (n = 132), an additional intravenous line was established at 2.92 minutes (176 s; SD 98 s) and the procedure took 1.8 minutes (109 s; SD 99 s). Twenty patients (13%) were intubated (all due to Glasgow Comma Scale < 9) at a mean time of 12.37 minutes (741 s; SD 767 s), which took 3.2 minutes (193 s; SD 73 s). The timer was started when the doctor ordered intubation. During the review process, we identified 84 patients who needed analgesics; 51 (61%) were provided adequate analgesia at 7.7 minutes (463 s; SD 374 s). All data can be found in Supplemental digital content 1, http://links.lww.com/EJEM/A255.
Nontechnical skills
Overall, 143 trauma team performances were evaluated using the T-NOTECHS scale. The mean score was 11.99 (SD 2.9) of a maximum 25. We observed that the trauma team performance in ‘leadership’ and ‘communication and interaction’ was average, resulting in mean scores of 2.66 (SD 0.99) and 2.27 (SD 0.75), respectively. ‘Cooperation and resource management’ and ‘situation awareness/coping with stress’ scores were better than average; however, performance in ‘assessment and decision making’ was poor, with an average score of 1.1 (SD 0.42).
Discussion
According to Lithuanian health statistical department data, since 2005 mortality due to trauma and external factors has decreased more than 40%, from 5549 deaths in 2005 to 3062 in 2016. The number of hospitalized patients following trauma has also decreased by 16% from 2012, from 50 855 to 43 840. These statistics explain why during the 8-month period of this study, we only had 162 trauma team activations and less than one-fifth of the patients were severely injured. These numbers indicate that the governmental programmes in place to decrease rates of injury and death due to injury are working. However, from the perspective of medical practice, it has become increasingly difficult to maintain the competencies of providing care for severely injured patients. The low level of ATLS guideline compliance rate supports the findings of Ivatury et al. [8]. That inadequacy in the fundamentals of resuscitation and the loss of competencies in the standardized approach to the trauma patient should be highlighted. Our finding of large variability in times with different trauma teams also supports loss of standardization.
To our knowledge, only a few studies have measured the specific time needed for certain steps during the trauma resuscitation. When comparing the results of patient evaluation times in our study to van Olden et al. [14], Bonjour et al. [15], and Lubbert et al. [16], we can see that in our hospital it takes approximately 30% more time to examine the patient and in some steps even longer (e.g., protection from hypothermia). This could be due to lack of briefing during which roles could be allocated, as well as shock room crowding and more importantly poor nontechnical skills, such as leadership and communication. The T-NOTECHS score supports this prediction because the average overall score of 11.99 was less than in Steinemann et al. [17] and DeMoor et al. [13], which reported scores of 16.3 and 16.5, respectively. It should be noted that like in most countries, Lithuania does not have a nontechnical skills curriculum for students or residents.
The trauma team is activated approximately once a day, so all the residents and attending physicians of different specialities, nurses, and support staff have lack of opportunities to get to know each other better, and to learn how to work in a multiprofessional team, for example, strengths and weaknesses of each team member, and nonverbal communication used. The trauma team did not have a shared mental model, which made it even more difficult to communicate and lead in a high-stress situation.
The framework used worked well in identifying pitfalls in trauma resuscitation. Based on these findings, a performance improvement programme will be developed, encompassing the HybridLab medical simulation technique [18], audio/video debriefing, and individualized feedback sessions. In trauma, it is difficult to measure the impact of training and it is highly debatable whether it should be measured by patient outcome (survival) or the process itself. In future studies, we will focus on process improvement and measure the impact on the above-mentioned times and the T-NOTECHS scale.
Conclusion
During the study period, we were able to precisely measure the time in seconds needed for certain steps in trauma patient resuscitation and management. The review process used was a straightforward procedure that could be performed by a nonmedical person. A specific performance improvement system can be devised based on these findings with a specific focus on certain clinical skills and aspects of nontechnical competences and teamwork.
Limitations
One of the limitations of this study is that there was only one video recording reviewer, who was senior, ATLS certified emergency medicine resident. Only one reviewer was chosen due to the will to keep the trauma team and personnel blinded from the study. However, this should not affect the time measurements, because it is a technical aspect and all the calculations were made by the application. However, the nontechnical evaluation was more complex and the T-NOTECHS scale does not have a clear and objective way to identify the components of good or bad performance and the scores vary between evaluators. Another limitation was poor sound quality during severely injured resuscitation, due to overcrowding and shouting.
Acknowledgements
Conflicts of interest
D.V., P.D. and N.J. are co-founders of HydridLab (http://www.hybridlab.com/). There are no conflicts of interest for the remaining authors.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website (www.euro-emergencymed.com).
References
- 1.Makary MA, Daniel M. Medical error-the third leading cause of death in the US. Bmj. 2016; 353:i2139. [DOI] [PubMed] [Google Scholar]
- 2.Aspden P, Corrigan JM, Wolcott J, et al. Patient Safety: Achieving a New Standard for Care. 2004, Washington, DC: The National Academies Press; [PubMed] [Google Scholar]
- 3.Kohn LT, Corrigan J, Donaldson MS.To Err is Human: Building a Safer Health System. 2000, Washington, DC: National Academy Press; [PubMed] [Google Scholar]
- 4.Gruen RL, Jurkovich GJ, McIntyre LK, Foy HM, Maier RV. Patterns of errors contributing to trauma mortality: lessons learned from 2,594 deaths. Ann Surg. 2006; 244:371–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Teixeira PG, Inaba K, Hadjizacharia P, Brown C, Salim A, Rhee P, et al. Preventable or potentially preventable mortality at a mature trauma center. J Trauma. 2007; 63:1338–1346; discussion 1346 [DOI] [PubMed] [Google Scholar]
- 6.Clarke DL, Gouveia J, Thomson SR, Muckart DJ. Applying modern error theory to the problem of missed injuries in trauma. World J Surg. 2008; 32:1176–1182 [DOI] [PubMed] [Google Scholar]
- 7.Sugrue M, Caldwell E, D’Amours S, Crozier J, Wyllie P, Flabouris A, et al. Time for a change in injury and trauma care delivery: a trauma death review analysis. ANZ J Surg. 2008; 78:949–954 [DOI] [PubMed] [Google Scholar]
- 8.Ivatury RR, Guilford K, Malhotra AK, Duane T, Aboutanos M, Martin N. Patient safety in trauma: maximal impact management errors at a level I trauma center. J Trauma. 2008; 64:265–270; discussion 270 [DOI] [PubMed] [Google Scholar]
- 9.The Scottish Trauma Audit Group. http://www.stag.scot.nhs.uk/Projects/Trauma.html. [Accessed 27 August 2019]
- 10.Porgo TV, Moore L, Tardif PA. Evidence of data quality in trauma registries: asystematic review. J Trauma Acute Care Surg. 2016; 80:648–658 [DOI] [PubMed] [Google Scholar]
- 11.Stelfox HT, Straus SE, Nathens A, Bobranska-Artiuch B. Evidence for quality indicators to evaluate adult trauma care: a systematic review. Crit Care Med. 2011; 39:846–859 [DOI] [PubMed] [Google Scholar]
- 12.Rogers FB, Rittenhouse KJ, Gross BW. The golden hour in trauma: dogma or medical folklore?. Injury. 2015; 46:525–527 [DOI] [PubMed] [Google Scholar]
- 13.DeMoor S, Abdel-Rehim S, Olmsted R, Myers JG, Parker-Raley J. Evaluating trauma team performance in a level I trauma center: validation of the trauma team communication assessment (TTCA-24). J Trauma Acute Care Surg. 2017; 83:159–164 [DOI] [PubMed] [Google Scholar]
- 14.van Olden GDJ, van Vugt AB, Biert J, Goris RJA. Trauma resuscitation time. Injury, Int. J. Care Injured. 2003; 34:191–195 [DOI] [PubMed] [Google Scholar]
- 15.Bonjour TJ, Charny G, Thaxton RE. Trauma resuscitation evaluation times and correlating human patient simulation training differences-what is the standard?. Mil Med. 2016; 181:e1630–e1636 [DOI] [PubMed] [Google Scholar]
- 16.Lubbert PH, Kaasschieter EG, Hoorntje LE, Leenen LP. Video registration of trauma team performance in the emergency department: the results of a 2-year analysis in a level 1 trauma center. J Trauma. 2009; 67:1412–1420 [DOI] [PubMed] [Google Scholar]
- 17.Steinemann S, Kurosawa G, Wei A, Ho N, Lim E, Suares G, et al. Role confusion and self-assessment in interprofessional trauma teams. Am J Surg. 2016; 211:482–488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kudreviciene A, Nadisauskiene R, Tameliene R, Tamelis A, Nedzelskiene I, Dobozinskas P, Vaitkaitis D. Initial neonatal resuscitation: skill retention after the implementation of the novel 24/7 HybridLab®learning system. J Matern Fetal Neonatal Med. 2017; 22:1–8 [DOI] [PubMed] [Google Scholar]


