http://aasldpubs.onlinelibrary.wiley.com/hub/journal/10.1002/(ISSN)2046-2484/video/15-S1-interview-lewis a video presentation of this article
Abbreviations
- AASLD
American Association for the Study of Liver Diseases
- AFIP
Armed Forces Institute of Pathology
- DILI
drug‐induced liver injury
- FDA
US Food and Drug Administration
- NIH
National Institutes of Health
- NLM
National Library of Medicine
- RUCAM
Roussel Uclaf Causality Assessment Method
- VA
Veterans Administration
In the arena of scientific medicine, it is not often that a field of study owes its recognition and formative development to a single individual, but in the case of liver injury caused by drugs and other therapeutic xenobiotics, one remarkable man is universally credited as the Patriarch of Drug Hepatotoxicity. Hyman Joseph Zimmerman was born in Rochester, NY, in 1914, quipping later that his birth might have helped start World War I.1 It probably would never have crossed his mind that the subsequent world conflict would serendipitously play a role in his entry into the discipline of hepatology, and more poignantly later propel him into the renowned and unique position of acclaimed leader of the field that, so to speak, he created and popularized. In 1932, he graduated from the University of Rochester with a degree in chemistry. While he was denied admission to its medical school because of its despicable ethnic quota system in place at the time, he was later able to enroll at Stanford University School of Medicine in 1934 where he completed his medical education. His initial interest on completing his medical internship, first at Stanford University and then at Strong Memorial Hospital in Rochester, was to pursue the discipline of endocrinology. Fortunately for hepatology, events changed that instead focused his interest on liver disease. With World War II now in full swing, he was drafted into the army and was first assigned to the School of Tropical Medicine at Walter Reed Army Medical Center in Washington, DC, with the anticipation that he would ultimately be sent to the Pacific Theater of Operations. Instead, following D‐Day in 1944, the army sent him to Europe to join the newly formed 239th General Hospital in a small town called Chalons‐sur‐Marne (later renamed Châlons‐en‐Champagne in 1998), situated about 170 km east of Paris. There he managed a ward of 100 beds filled with soldiers who had acquired trench foot while fighting during the Battle of the Bulge. As chance would have it, the ward began to be filled with soldiers with “catarrhal jaundice,” a condition unappealing to the other military hospital physicians. In contrast, Hy willingly accepted these patients and within 6 weeks, he had cared for nearly 300 soldiers affected by a form of infectious hepatitis and gastroenteritis, which he deduced was being transmitted by contaminated snow scooped up from the ground and melted to make coffee in the field by the GIs.1 His analysis of the clinical and laboratory features of that illness is one of the seminal papers on what would later be found to be hepatitis A, born on the battlefields of the Bulge in Belgium and Luxembourg.2
Following the end of the war, Hy returned stateside in December 1945 and served on the staff at the Lowell General Hospital in Massachusetts for about 6 months before being discharged from the service. At the time, the field of prospective medical residents was crowded, with many other experienced former army physicians seeking residency positions. He landed a position on the George Washington University Medical Center service of Gallinger Hospital in Washington, DC (later named DC General Hospital) and began an academic career that lasted more than 50 years. During this residency, his interest in liver disease was further inspired through his tendency to perform liver biopsies on his patients whenever possible. He learned the technique from a friendly surgeon who would perform a laparoscopy so that Hy could develop a feel for the percutaneous technique. However, he believed that the histopathology department at Gallinger Hospital was doing a poor job processing the biopsy specimens he procured, converting them, in his words, into “chopped liver.”1 Not trusting these valuable specimens to his own laboratory, he took them (in his words, “bootlegged”) out of the hospital to the Armed Forces Institute of Pathology (AFIP), which was then located on Independence Avenue (about 10 minutes away), where they would be handled with the proper level of care. The building also housed the Surgeon General’s Library, which was the forerunner of the National Library of Medicine (NLM). It was at the AFIP that Hy first met Dr. Hans Smetana, who headed the hepatic disease section. Dr. Smetana (the grandnephew of the famous Czech composer, Bedrich Smetana) had come to the United States as a political refugee. He took Hy under his wing, processing his liver biopsies and then reading the slides together. Hy developed great expertise in reading liver biopsies, leading his future friend and collaborating researcher, Dr. Kamal Ishak, to marvel when they first met at his prowess as a nonpathologist (more of his collaboration with Dr. Ishak is included later in this review).
After completing his chief residency in 1948, and finding that no jobs were immediately available in Washington, he became a consultant for a year in private practice, focusing on liver diseases that had no other devotees in Washington at the time. Soon after, however, Hy accepted an appointment to become an Assistant Chief of the Medical Service at the Washington, DC, Veterans Administration (VA) Hospital, thus beginning his long association with VA hospitals and their academic affiliations. In high demand, Hy was invited over the next two decades to be chief of several medical services, first at the VA Hospital in Omaha, followed by the Westside VA Hospital in Chicago, and later on the Boston VA before returning to Washington, DC, to the now renamed Veterans Affairs Medical Center. The VA system became the perfect venue for Hy to hone his clinical observations about drug‐induced liver injury (DILI) and other liver disorders. He worked initially in enzymology and described the liver‐related biochemical tests to define hepatic injury that are still in use today,3 as well as in the field of viral hepatitis (where he would have a hand in studying and describing nearly all of the named viruses). In addition, he published seminal articles on most of the important systemic diseases and infections that affect the liver, including sarcoidosis, tuberculosis, pneumococcal pneumonia, lupoid [autoimmune] hepatitis, steatohepatitis, congestive heart failure, and alcoholic liver disease. He also spent as much time as he could in the library and in scanning as much of the literature as possible before the advent of the computer, from which his love for cataloging his immense number of reprints likely took root. At the time of his death, the entire basement level of his home and his garage (the car having long been relegated to sit in the driveway) had been overtaken with several dozen library‐grade card catalogs and countless five‐drawer steel filing cabinets stuffed to their limits with his enormous collection of reprints. In addition, bookshelves lined the walls and sagged under the weight of more than 40 sets of complete bound journals from every medical discipline.
Blessed with a prodigious memory—and to the amazement of all his students—Hy could quote chapter and verse (i.e., the author, journal, volume, year, and page number) of almost any article he wished to cite. But it was his detailed descriptions of various forms of DILI for which he is most well‐known and celebrated. His early forays into defining the mechanisms and clinical features of DILI and chemical‐induced liver injury in the 1950s, 1960s, and 1970s (including iproniazid, nitrofurantoin, aureomycin, chlorpromazine, dantrolene, isoniazid, endotoxin, chlordiazepoxide, tricyclic antidepressants, tetracycline, aspirin, erythromycin estolate, halothane, papaverine, diphenylhydantoin, sulfonamides, D‐galactosamine, ethionine, anabolic steroids, chloroform, carbon tetrachloride, and other chlorinated hydrocarbons, among others),3 paralleled the work on DILI of some of the other original pioneer members of the American Association for the Study of Liver Diseases (AASLD). Among these were Hans Popper (who called DILI a “penalty for progress”4), Fenton Schaffner, Irwin Arias, and other notable researchers who, together with Hy, authored seminal articles on the burgeoning subject of DILI in a 1963 special edition of the Annals of the New York Academy of Sciences devoted to the topic.5 We do not mean to imply that DILI was not reported before Hy’s publications. The hepatotoxicity of arsenic, chloroform, and phosphorus was recognized in the 18th and 19th centuries, cinchophen used for the treatment of gout was arguably, in the 1920s, the first identified cause of an idiosyncratic hepatotoxic drug reaction, whereas puzzling hepatitis‐like drug reactions associated with early antithyroid preparation use were reported in the 1940s. However, what set Hy apart was his ability to characterize, define, and classify all of the major clinical, pathological, and laboratory signatures of drugs and chemicals causing liver injury and their pathophysiology, in his uniquely eloquent, lucid, and informative style. Hy drew attention to the differences between intrinsic versus idiosyncratic hepatoxicity and between hepatic versus cholestatic reactions, and he pointed out that there are different forms of cholestasis, namely, hepatocellular, hepatocanalicular, and ductular. Indeed, his extensive, groundbreaking research on DILI coupled with his engaging way with words became the basis for his single‐authored tour de force textbook Hepatotoxicity: The Adverse Effects of Drugs and Other Chemicals on the Liver, published in its first edition in 1978.6 The textbook, encyclopedic in its content—remember all of those reprints?—quickly became known as the bible of DILI.
Hyman J. Zimmerman’s official bookplate photograph for the second edition of Hepatotoxicity: The Adverse Effects of Drugs and Other Chemicals on the Liver (1999).14 (Courtesy of Lippincott Williams and Wilkins.)

As one of the world’s leading authorities on hepatotoxicity, his advice was regularly sought after both by the pharmaceutical industry and by regulatory agencies. Serving as a consultant to the US Food and Drug Administration (FDA) and drug manufacturers alike, he helped introduce several concepts into the growing field of hepatic safety, including liver test monitoring to prevent serious liver injury to allow certain drugs to remain on the market, and critically reviewing clinical trial data during drug development to determine whether hepatic safety was an issue. Indeed, his most enduring legacy remains his key clinical observation that drug injury severe enough to produce hepatocellular jaundice was associated with a risk for acute liver failure and death (or need for liver transplant) of 10% or higher, depending on the agent. Known simply as Hy’s Law, a term coined by Dr. Robert Temple of the FDA in the 1980s,7, 8, 9 it was based on Hy’s remarks at a Fogarty conference on guidelines for detecting hepatotoxicity held at the National Institutes of Health (NIH) in 1978,10 and reflected one of his many prophetic statements that appeared in the first edition of his book. To this day, it remains a cornerstone of hepatic safety assessment, as emphasized in the current FDA guidance on monitoring and avoidance of hepatotoxicity. Numerous drugs have been abandoned during early‐phase testing, have failed to win approval, or have been withdrawn after marketing because of the danger that the presence of a Hy’s Law case predicts.11 Hy was never comfortable with the eponymous term, and eschewed using it himself, given his humility and desire to avoid the limelight. However, we know of no other law in science or medicine that goes by just a first, rather than a last, name and, moreover, a contraction of that (Hy not Hyman). It is Newton’s law of gravity (not Isaac’s law); Einstein’s theory of relativity (not Albert’s theory), and so forth. The term Hy’s Law is known to all in the field of hepatology, reflecting the respect and admiration afforded him throughout his career, and is a measure of how approachable and gentlemanly he was to everyone with whom he interacted. “Chairman Hy” was another title he was given whenever he would make rounds—and much like the old EF Hutton slogan: “Whenever Hy talked, everyone listened.” And even when he was unable to talk due to the effects of lingual cancer that was to end his life, his words were an integral part of the inaugural conference started in 1999 by his friend at the FDA, Dr. John Senior, to initially educate FDA reviewers and staff about the rapidly growing clinical issues regarding drug‐related hepatic safety. The principles relating to DILI that Hy espoused, and the many related questions with which he struggled, grew into what would become an annual conference of FDA regulatory scientists (championed by Dr. John Senior), members of academia and the AASLD, and members of the pharmaceutical industry, which tackled all aspects of hepatotoxicity.12
The “Chairman” at the University of Chicago circa 1960. (Courtesy of Diane Zimmerman.)

Upon his return to Washington, DC, in 1965, Hy contacted the new head of the Hepatopathology Section at the AFIP, Dr. Kamal Ishak, intending to arrange liver biopsy teaching sessions for his fellowship trainees. Thus began a professional bond and a lifelong personal friendship between Hy and Dr. Ishak, culminating in Hy’s final years spent as a visiting scholar at the AFIP. The teaching program for Hy’s fellows grew to become weekly biopsy sessions with other AFIP hepatopathologists, including Drs. Lionel Rabin and Zachary Goodman. Over the years, these biopsy reading sessions attracted numerous local, national, and international hepatologists and hepatopathologists, who would often bring their own liver biopsy slides to be reviewed by the AFIP staff and other attendees. Referred to by Hy as a “monastery for histopathology,”1 these AFIP sessions helped refine the clinical‐morphological signatures of hepatotoxic agents that became the hallmark of the Ishak‐Zimmerman descriptions of the various DILIs that were starting to appear more regularly.13 Even during an intervening period of 3 years when Hy was Chief of Medicine at the VA Medical Center in Boston, he arranged to fly back to Washington, DC, to attend these AFIP sessions on a monthly basis so as not to miss out on these master‐class sessions.
Dr. Zimmerman conducting a physical examination at the University of Chicago, circa 1960. (Courtesy of University of Chicago.)

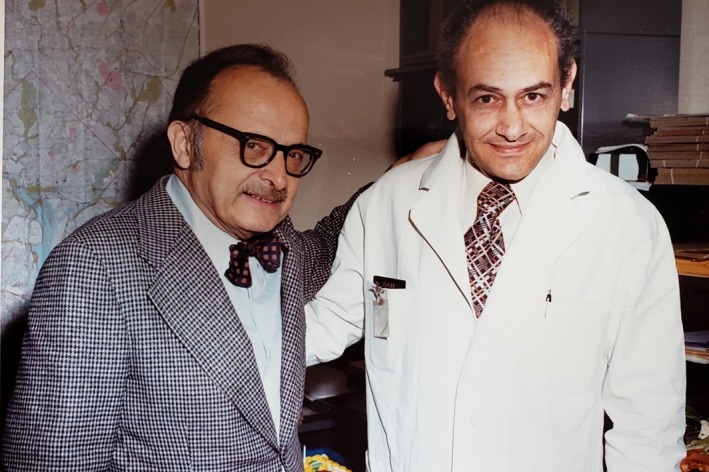
Hy and Dr. Kamal Ishak at an early meeting at the AFIP circa 1965. (Courtesy of Diane Zimmerman.)
Between the first and eagerly awaited second edition of Hy’s textbook on hepatotoxicity,14 more than 20 years elapsed, during which time he collected and memorized more reprints and wrote countless manuscripts and book chapters detailing the clinical, pathological, and laboratory features of nearly all of the newly established hepatotoxic drugs and chemicals of those decades. Anyone who attended a Grand Rounds presentation where Hy was in the audience (always in the front row) marveled at his uncanny ability to simultaneously review a sheaf of new reprints, fall asleep during the lecture, but awaken just in time to lead the applause and ask the most insightful question of the presenter. During those years, Hy was the senior author on seminal papers that analyzed the liver safety data on such drugs as diclofenac, sulindac, captopril, ketoconazole, labetalol, valproate, phenylbutazone, amiodarone, enflurane, allopurinol, and amoxicillin‐clavulanate, to name just a few. Many of these cases were sent to Hy for his review, courtesy of the FDA reviewing divisions, who granted him special access to data when they were concerned about a growing number of hepatotoxicity reports from recently approved products in both the premarketing and the postmarketing settings. Boxes containing case reports from the FDA were parceled out among his fellows and junior faculty for their initial review. Hy would then assess the findings, and was famous for carrying a red pencil with which he would then deftly edit the initial draft and turn it into an acceptable publication. As a result, several agents were withdrawn or had their use restricted (e.g., ticrynafen, tacrine, pemoline). In addition, several drugs under review by the FDA (e.g., benoxaprofen) were not approved on the basis of Hy’s analyses. Most often, these manuscripts were accepted by the journals without requiring much revision—probably because there were very few individuals with the knowledge or credentials to challenge Hy’s conclusions about the specific hepatic injury or the writing style. However, given that causality assessment was an inexact science then, as it is today, at times some of these manufacturers and their experts would contest the findings, and editorials rebutting the results would appear (e.g., enflurane15, 16). Even though he might flash a bit of anger because of the annoyance of such challenges, he was always mostly gentlemanly in his responses, preferring to “keep his powder dry,” as he was fond of saying. It should be noted that Hy’s overall conclusions regarding the hepatotoxic potential of drugs were rarely, if ever, proved to be wrong.
Hy (fourth from right, second row), Kamal (to the left of Hy), Leonard Seeff (beginning of second row on right), and the staff of the Hepatopathology Department of the AFIP with Lionel Rabin (to the left of Hy), circa early 1970s. (Courtesy of Diane Zimmerman.)

Hy lecturing on the mechanisms of DILI circa 1970. (Courtesy of Diane Zimmerman.)

One of the most difficult aspects of defining and diagnosing DILI arises from the fact that it can mimic nearly all other causes of acute and chronic and benign and malignant liver diseases. Hy espoused many of the clinical elements and causality assessment principles used to diagnose DILI in his papers, monographs, and textbooks. Indeed, his often expert opinion–based methodology is still in wide use today. It is somewhat curious, then, that although he was part of a select panel of eight expert international hepatologists (and one of just two Americans, the other being Dr. Willis Maddrey) who developed the Roussel Uclaf Causality Assessment Method (RUCAM) scoring system for DILI in the late 1980s and early 1990s, Hy (and the other invitees) declined to be listed as authors of these seminal manuscripts.17, 18 According to Dr. Maddrey (personal communication, 2018), the reasons were relatively straightforward. Although Hy and the others enjoyed the meeting (having been flown over to Paris on the Concorde), they believed it was still a work in progress that required further validation. And although it was a step in the right direction, Hy did not think it was ready for primetime (more of “keeping your powder dry”). Thirty years later, we are still trying to perfect the RUCAM and causality assessment.19, 20, 21
Hy at his desk at George Washington University Hospital circa 1985—always writing or editing! (Courtesy of Diane Zimmerman.)

One particular area of interest that proved somewhat controversial for Hy was the issue of the interaction between acetaminophen and alcohol. Based on his clinical observations of patients at the VA starting in 1980, the term “therapeutic misadventure” was coined to indicate that potentiation of liver injury in heavy users of alcohol could occur in unsuspecting patients taking therapeutic doses of acetaminophen, and not a result of intentional overdose.22, 23 Acetaminophen manufacturers were deeply disturbed by this view and countered with editorials and studies to deny his claims, especially in the United Kingdom, where intentional paracetamol overdose was the leading cause of suicide.24 Summarily dismissed was the notion that therapeutic doses of acetaminophen might potentially be harmful among regular alcohol users. Nevertheless, current labeling on acetaminophen products does acknowledge the need to take alcohol into account.
Although his landmark textbook on hepatotoxicity has been updated with more recent compendia, these are multi‐authored efforts, reflecting the ever‐widening field of DILI, and all pay silent homage to the Herculean effort required to complete his original single‐authored tome.
Drs. Kamal Ishak, Hy Zimmerman, and a visiting Hans Popper at one of the AFIP’s hepatopathology biopsy sessions. (Courtesy of Diane Zimmerman.)

Hy attending the International Association for the Study of Liver Diseases meetings in South Africa, with Kamal Ishak. Back row (left to right): Adrian Di Bisceglie, Chris Kassianides, Tony Bass, Neville Pimstone, Steve Porter, unknown bearded man, Tarek Hassanein. Second row (left to right): David Van Thiel, Carlo Tamburo, obscured blond woman, Doris Strader. Front row (left to right): Cheryl Winchell, Kamal Ishak, Hy, and Jay Hoofnagle. (Photograph was taken by Leonard Seeff.)

Considered the father of modern‐day drug hepatotoxicity, nearly 350 of his former and current students, research fellows, colleagues, and friends gathered together in the spring of 1987 in Bethesda, Maryland, to pay tribute to his decades of work in hepatotoxicity. This Festschrift in his honor was highlighted by presentations of the latest advancements in all fields of hepatology by his trainees and disciples, all of whom (as eloquently stated by Dr. James Finkelstein, the Chief of the Medical Service at the VA at the time) were “members of the Hyman J. Zimmerman alumni association; the faculty and students of a unique college.”25 It is noteworthy that Hy’s original classifications and clinical‐pathological descriptions of the hepatotoxins contained in his textbook, along with their postulated mechanisms of injury, are still relevant more than two decades after his passing. Moreover, his prediction about the 10% or higher mortality rate associated with acute liver failure from drugs has been validated in several global drug registries, including the NIH‐sponsored U.S. DILI Network.26 Always an enthusiastic supporter of the NLM (with his own smaller version in his basement), Hy would no doubt smile with complete satisfaction at the creation of LiverTox, a virtual textbook on DILI, spearheaded by Jay Hoofnagle and other former trainees from the Liver Diseases section at the NIH and his former colleagues at the NLM.27 He would be intrigued by the ongoing research efforts to identify the precise genetic and pharmacological risk factors for DILI that he could only hint at during his career. No doubt, the lecture named in his honor at the annual meetings of the AASLD will ensure that his legacy endures for the new generation of hepatologists who will follow in his footsteps.28, 29 Largely due to Hy’s efforts, hepatotoxicity remains alive and well as a clinical discipline and research venue. Those of us fortunate enough to have worked with Hy, and to have been mentored and befriended by this remarkable man and clinician, recognize that we have all been the recipients of a truly special medical education.
Hy and Kamal relaxing at the Zimmerman home with Jim and Stephanie Lewis, 1987. (Personal collection by Dr. Lewis.)

Standing in front of the AFIP liver biopsy conference room are (from left to right): Hy, Dr. Laura Seeff (on rotation, daughter of Leonard Seeff and goddaughter of Dr. Zimmerman), Dr. Leonard Seeff, and Dr. Kamal Ishak, 1992. (Personal collection by Dr. Seeff.)

Series Editor’s Postscript
This wonderful contribution to the current series is a fitting tribute to Hy Zimmerman. I was privileged to have met him on several occasions and had the opportunity myself to honor him in one of my Landmark articles.8 In contrast with his small frame, he truly was a giant when it came to scholarship, integrity, and honor—a true mensch. I am aware of the fact he was initially denied admission to the University of Rochester School of Medicine because of a deceitful administrative device, termed Numerus Clausus, which was crudely used as an ethnic gatekeeper. I recall with pride that when the shameful Eppinger affair (see Reuben A. First do no harm. Hepatology 2005;42:1464‐1470 and 2006;43(2 suppl 1):S243‐S249) scandal broke on the front page of the Sunday edition of the New York Times during an annual AASLD meeting, he unhesitatingly welcomed the revelation. Dark forces always need to be illuminated, and Hy was no exception when it came to his experiences (whether it was against Jewish quotas for medical school admission and other racial bigotry, or confronting past evildoers from Nazi Germany). He was indeed a giant among his peers.
Biographies


Potential conflict of interest: Nothing to report.
References
- 1. Dr Kennedy CS, Hyman J. Zimmerman oral history interview. Armed Forces Institute of Pathology & Charles Stuart Kennedy; January 28, 1993. Available at: https://archive.org/stream/ZimmermanHyman/zimmerman%252C%2520hyman_djvu.txt [Google Scholar]
- 2. Zimmerman HJ, Lowry CF, Uyeyama K, et al. Infectious hepatitis: Clinical and laboratory features of 295 cases. Am J Med Sci 1947;213:395‐409. [DOI] [PubMed] [Google Scholar]
- 3. Zimmerman HJ. Clinical and laboratory manifestations of hepatotoxicity. Ann NY Acad Sci 1963;104:954‐987. [Google Scholar]
- 4. Popper H, Rubin E, Cardiol D, et al. Drug‐induced liver disease—A penalty for progress. Arch Intern Med 1965;115:128‐136. [DOI] [PubMed] [Google Scholar]
- 5. Smetana HF, Schaffner F, Drill VA, et al. Hepatotoxicity of therapeutic agents. Ann NY Acad Sci 1963;104:821‐1092. [Google Scholar]
- 6. Zimmerman HJ. Hepatotoxicity: The Adverse Effects of Drugs and Other Chemicals on the Liver. New York: Appleton‐Century‐Crofts; 1978. [Google Scholar]
- 7. Temple R. Hy’s law: Predicting serious hepatotoxicity. Pharmacoepidemiol Drug Saf 2006;15:241‐243. [DOI] [PubMed] [Google Scholar]
- 8. Reuben A. Landmarks in Hepatology: Hy’s law. Hepatology 2002;39:574‐578. [Google Scholar]
- 9. Lewis JH. Hy’s Law, the Rezulin rule and other predictors of severe drug‐induced hepatotoxicity: Putting risk‐benefit into perspective. Pharmacoepidemiol Drug Saf 2006;15:221‐229. [DOI] [PubMed] [Google Scholar]
- 10. Davidson CS, Leevy CM, Chamberlayne EC, eds. Guidelines for the detection of hepatotoxicity due to drugs and chemicals. NIH publication 79‐313. U.S. Dept of Health, Education, and Welfare, Public Health Service, National Institutes of Health; 1979. [Google Scholar]
- 11. Lewis JH. The art and science of diagnosing and managing drug‐induced liver injury in 2015 and beyond. Clin Gastroenterol Hepatol 2015;13:2173‐2189. [DOI] [PubMed] [Google Scholar]
- 12. Senior JR. How can “Hy’s law” help the clinician? Pharmacoepidemiol Drug Saf 2006;15:235‐239. [DOI] [PubMed] [Google Scholar]
- 13. Ishak KG, Zimmerman HJ. Morphologic spectrum of drug‐induced hepatic disease. Gastroenterol Clin North Am 1995;24:1027‐1045. [PubMed] [Google Scholar]
- 14. Zimmerman HJ. Hepatotoxicity: The Adverse Effects of Drugs and Other Chemicals on the Liver. 2nd ed Philadelphia: Lippincott Williams & Wilkins; 1999. [Google Scholar]
- 15. Lewis JH, Zimmerman HJ, Ishak KG, et al. Enflurane hepatotoxicity: A clinicopathologic study of 24 cases. Ann Intern Med 1983;98:984‐992. [DOI] [PubMed] [Google Scholar]
- 16. Eger EI 2nd, Smuckler EA, Ferrell LD, et al. Is enflurane hepatotoxic? Anesth Analg 1986;65:21‐30. [PubMed] [Google Scholar]
- 17. Danan G, Benichou C. Causality assessment of adverse reactions to drugs. I. A novel method based on the conclusions of international consensus meetings: Application to drug‐induced liver injuries. J Clin Epidemiol 1993;46:1323‐1330. [DOI] [PubMed] [Google Scholar]
- 18. Benichou C, Danan G, Flahault A. Causality assessment of adverse reactions to drugs. II. An original model for validation of drug causality assessment methods: Case reports with positive rechallenge. J Clin Epidemiol 1993;46:1331‐1336. [DOI] [PubMed] [Google Scholar]
- 19. Shapiro MA, Lewis JH. Causality assessment of drug‐induced hepatotoxicity: Promises and pitfalls. Clin Liver Dis 2007;11:477‐505. [DOI] [PubMed] [Google Scholar]
- 20. Rockey DC, Seeff LB, Rochon J, et al.; for the US Drug‐Induced Liver Injury Network . Causality assessment in drug‐induced liver injury using a structured expert opinion process: comparison to the Roussel‐Uclaf Causality Assessment Method. Hepatology 2010;51:2117‐2126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Danan G, Teschke R. Drug‐induced liver injury: Why is the Rousssel Uclaf Causality Assessment Method (RUCAM) still used 25 years after its launch? Drug Saf 2018;41:735‐743. [DOI] [PubMed] [Google Scholar]
- 22. Seeff LB, Cuccherini BA, Zimmerman HJ, et al. Acetaminophen hepatotoxicity in alcoholics. A therapeutic misadventure. Ann Intern Med 1986;104:399‐404. [DOI] [PubMed] [Google Scholar]
- 23. Zimmerman HJ, Maddrey WC. Acetaminophen (paracetamol) hepatotoxicity with regular intake of alcohol: Analysis of instances of therapeutic misadventure. Hepatology 1995;22:767‐773. [PubMed] [Google Scholar]
- 24. Prescott LF. Therapeutic misadventure with paracetamol: Fact or fiction? Am J Ther 2000;7:99‐114. [DOI] [PubMed] [Google Scholar]
- 25. Seeff LB, Lewis JH, eds. Festschrift for Hyman J. Zimmerman, MD. Current Perspectives in Hepatology. New York: Plenum Publishing Corporation; 1989. [Google Scholar]
- 26. Chalasani N, Bonkovsky HL, Fontana R, et al. Features and outcomes of 899 patients with drug‐induced liver injury: The DILIN prospective study. Gastroenterology 2015;148:1340‐1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hoofnagle JH, Serrano J, Knoben JE, et al. LiverTox: A website on drug‐induced liver injury. Hepatology 2013;57:873‐874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Seeff LB. Presentation of the AASLD Distinguished Achievement Award to Hyman J. Zimmerman, MD. Hepatology 1987;7:213‐215. [DOI] [PubMed] [Google Scholar]
- 29. Seeff LB. Obituary: Hyman J. Zimmerman, MD. JAMA 2000;283:812. [Google Scholar]


