http://aasldpubs.onlinelibrary.wiley.com/hub/journal/10.1002/(ISSN)2046-2484/video/15-S1-interview-krowka a video presentation of this article
Abbreviations
- AASLD
American Association for the Study of Liver Diseases
- ECMO
ECMO, extracorporeal membrane oxygenation
- ERA
endothelin receptor antagonist
- ERS
European Respiratory Society
- HPS
hepatopulmonary syndrome
- ILTS
International Liver Transplant Society
- IPVD
intrapulmonary vascular dilatation
- IV
intravenous
- LD
liver disorder
- l‐NAME
NG‐nitro‐l‐arginine methyl ester
- LT
liver transplant
- MELD
Model for End‐Stage Liver Disease
- MIGET
multiple inert gas elimination technique
- mPAP
mean pulmonary artery pressure
- NIH
National Institutes of Health
- PaO2
partial pressure of arterial oxygen
- PBC
primary biliary cirrhosis
- PH
pulmonary hypertension
- POPH
portopulmonary hypertension
- PV
pulmonary vasoactive
- PVR
pulmonary vascular resistance
- REVEAL
Registry to EValuate Early And Long‐term pulmonary artery hypertension disease management
- 99mTcMAA
technetium macroaggregated albumin
- UNOS
United Network for Organ Sharing
- WHO
World Health Organization
With the advent of successful liver transplantation came a renewed interest in what we now appreciate as two distinct adverse pulmonary vascular consequences of advanced liver disease: hepatopulmonary syndrome (HPS) and portopulmonary hypertension (POPH). The interest was not simply academic. Indeed, once these entities were recognized and accurately characterized, it was clear that their natural histories and effects on both attempts at and outcomes of liver transplantation could be quite concerning.
Given millennia of experience with cirrhosis, had these pulmonary complications always been around and were they simply not recognized as such because of the absence of characterization of the syndromes, lack of diagnostic criteria, and/or failure to appreciate their clinical importance? Perhaps. And so, as a prelude to a historical review of these entities, and to help clarify the frequent confusion between the two syndromes, a concise, comparative summary of characteristics of each syndrome is provided in Table 1.
Table 1.
Distinctions between HPS and POPH
| Characteristics | HPS | POPH |
|---|---|---|
| Clinical issue* | Arterial hypoxemia caused by IPVD | Pulmonary artery hypertension |
| Diagnostic criteria† | PaO2 < 80 mm Hg | mPAP > 25 mm Hg; PVR > 3 wood units |
| LD | Usually cirrhosis | Always portal hypertension |
| Severity | Poor correlation with LD | Poor correlation with LD |
| Frequency seen | 5%‐32% | 5%‐10% |
| Medical treatments‡ | Wear supplemental oxygen | PV medications |
| 5‐Year survival rate | 23% (no treatments) | 4%‐14%; 40% survival rate with PV therapy only |
| LT§ | An “indication” | A “contraindication” if mPAP > 45 mm Hg |
| Treatment outcomes‖ | Complete resolution with LT | Unpredictable, 50% resolution with LT |
IPVDs were determined by contrast‐enhanced transthoracic echocardiography.
PaO2 determined by arterial blood gas in the sitting position breathing room air; right heart catheterization measures/calculates mPAP and PVR, respectively.
Several available for POPH, but only one randomized, placebo‐controlled trial conducted; no controlled trials in HPS to date.
Increased LT risk. Expedited LT consideration if pretransplant PaO2 < 60 mm Hg (HPS); if mPAP < 35 mm Hg with PV therapy (POPH).
Time resolution of HPS related to severity of hypoxemia; PV therapy in POPH can be discontinued in 50% after LT.
Early History
Hepatopulmonary Syndrome
Why does arterial blood lack oxygen in the setting of liver disease? That simple question was first addressed in 1894 by Dr. M. Fluckiger1 with the support of Professor F. D. von Recklinghausen, who conducted the autopsy on his 37‐year‐old patient who died of massive hematemesis and cirrhosis of the liver caused by syphilis. Subsequently, complex explanations for arterial hypoxemia over the years have culminated in the description of an entity, coined by Kennedy and Knutson2 in 1977 as the “hepatopulmonary syndrome.” It was not until 1998 that a seminal review article regarding the pulmonary vascular disorders in portal hypertension was published by French investigators.3 This article described potential pathophysiological mechanisms based on clinical experiences; it paved the way for the first animal model for HPS described by Chang4 from Northwestern University and subsequently expanded on and continued in‐depth by Fallon and colleagues5 at the University of Alabama.
Portopulmonary Hypertension
The observation that pulmonary hypertension (PH) could complicate portal hypertension was first made by Mantz and Craig6 at the University of Minnesota in 1951. The link between PH and portal hypertension was initially thought to be caused by pulmonary emboli originating from the portal venous territory and passing through portosystemic shunts to reach the pulmonary circulation. In addition to emboli, subsequent autopsy studies have demonstrated other pathologies.7 Specifically, thrombosis in the pulmonary arteries could be caused by constriction of its peripheral, that is, muscular arterial branches, by endothelial/smooth muscle proliferation, intimal lesions including proliferation and fibrosis, dilatation lesions and platelet aggregates, but not an embolic phenomenon. The constellation of these nonembolic changes was termed “plexogenic arteriopathy,” which derives from the Latin word plexus meaning a “braid.” The network/web morphology metaphor is borrowed from neuroanatomy—remember nerve plexuses. The term “plexiform” has been used to indicate the stage of the lesion, but it is best given a wide berth to avoid confusion.8 The unifying idea was an obstruction to pulmonary arterial flow caused by mediators emanating from or bypassing the portal circulation. The entity was termed “portopulmonary hypertension,” a phrase arguably first used by Yoshida et al.9 in 1993. Despite the clinical and hemodynamic characterizations of PH in the setting of liver disease, no experimental animal model exists to date for POPH.
The First “Liver‐Lung” Conference
In 1990, a small group of clinicians convened at the Mayo Clinic satellite practice in Jacksonville, Florida, for what was arguably the first international gathering to discuss “liver‐lung” problems (Fig. 1). This was the first national or international conference that I could find that included a talk on the topic of HPS; a fitting (and appreciative) lecturer for the inaugural presentation was Dame Sheila Sherlock (1918‐2001)10 of the Royal Free Hospital in London (Fig. 2). Interestingly, the topic of pulmonary artery hypertension as a complication of liver disease was given scant attention, but subsequent anecdotes of liver transplant (LT) failures in the setting of that disorder would soon become apparent in the late 1990s.
Figure 1.
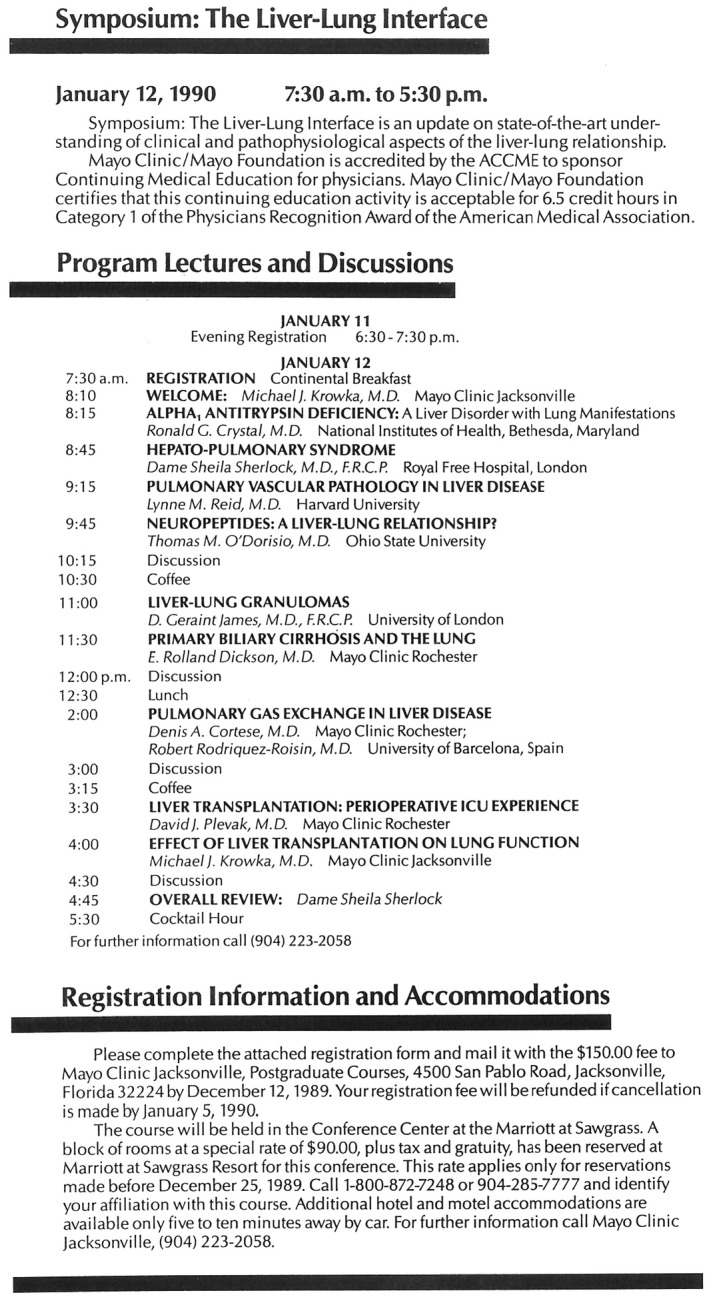
The first liver‐lung conference that had HPS as a unique meeting topic. The conference was held at the Mayo Clinic, Jacksonville, Florida, campus and featured renowned physicians who spoke to an audience of approximately 30 people.
Figure 2.
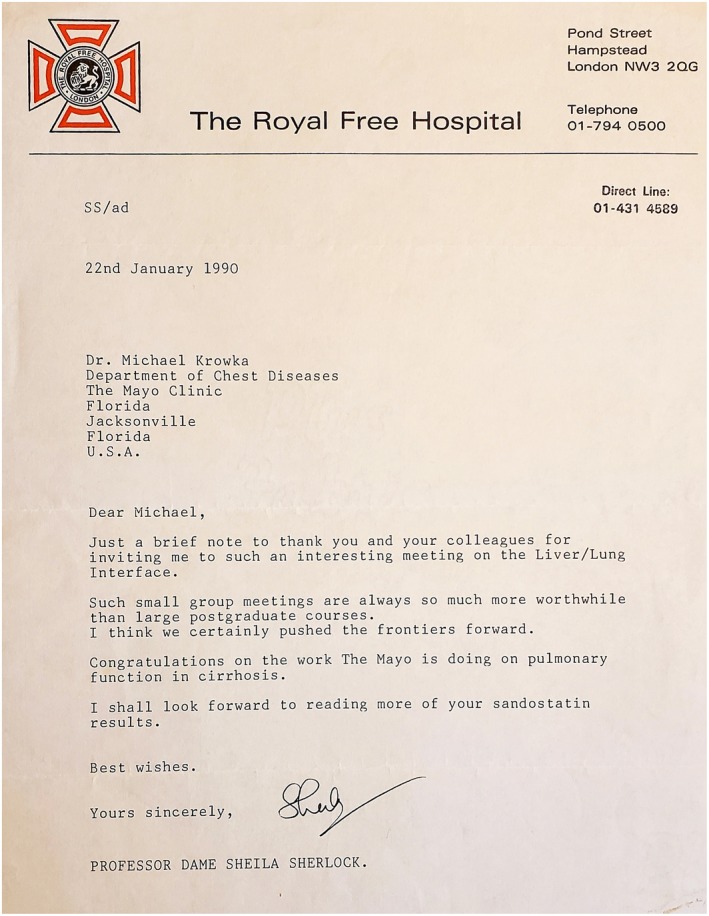
A thank‐you letter from Dame Sheila Sherlock after the liver‐lung conference at Mayo Jacksonville. The subsequent “proof‐of‐concept” use of Sandostatin, referred to in her letter to treat HPS, was a failure.
As a final aside, the liver‐lung theme also included a lecture on sarcoidosis, provided by the husband of Prof. Sherlock, David Geraint (Gerry) James (1922‐2010), M.D., F.R.C.P.
Committee at Work
During the 2000 European Respiratory Society (ERS) Annual Congress held in Florence, Italy, experts in pulmonology and hepatology held a symposium entitled “Advances in Understanding Pulmonary Complications in Hepatic Diseases.” From this symposium was born the ERS Task Force on Pulmonary‐Hepatic Disorders that subsequently published its landmark paper in 200449 (Fig. 3) that had three goals: (1) to increase awareness of HPS and POPH; (2) to improve diagnosis and management; and (3) to suggest and stimulate research. The diagnostic criteria and suggestions put forth by that Task Force remain the guideposts followed today.
Figure 3.
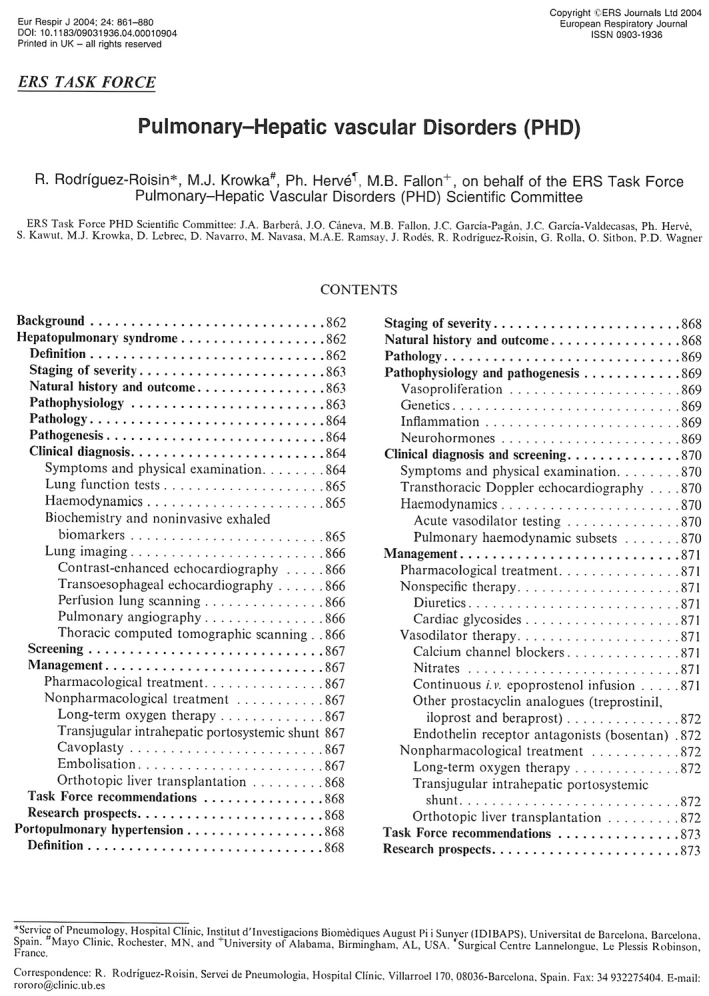
ERS Task Force Recommendations for the Screening, Diagnosis and Management of Pulmonary‐Hepatic Vascular Disorders. Two international consensus conferences were held to characterize and develop diagnostic criteria for the pulmonary vascular syndromes in liver disease. The final Consensus Conference, held in Barcelona, Spain, chaired by Dr. Rodriguez‐Roisin from Barcelona and Dr. Krowka from Rochester, Minnesota. The diagnostic criteria agreed on and published from that gathering are still followed as of this writing, as exemplified by this report from the ERS Task Force.
Transplant Disappointments and Successes
There has been a remarkable evolution of experience and expectations when confronted with these pulmonary vascular syndromes in LT candidates. No proven medical therapies for HPS have evolved via controlled trials, the most recent being a National Institutes of Health (NIH)–sponsored, multicenter, prospective, randomized, placebo‐controlled trial using sorafenib to attenuate angiogeneis11 (although supplemental oxygen can improve hypoxemia). POPH can be improved, but not be cured, with pulmonary artery vasomodulators alone. Hence with poor outcomes of the “natural histories” of both syndromes, attempts and experiences to resolve them with liver transplantation have evolved.
Notably, only one randomized, placebo‐controlled trial has been accomplished in patients with POPH, PORTICO.12 This trial recently reported a significant reduction in pulmonary vascular resistance (PVR) and mean pulmonary artery pressure (mPAP; compared with controls) using the endothelin receptor antagonist (ERA) macitentan over a 12‐week period. Implications of these findings for liver transplantation will be of interest.
Hepatopulmonary Syndrome
In a 1968 report, Starzl et al.,13 while at the University of Colorado, described the extended survival after orthotopic homotransplantation of three children who “had evidence of the venous‐to‐arterial intrapulmonary shunts.” Interestingly, the oxygen saturations were 85% to 88% breathing room air and did not improve breathing pure oxygen. The shunts were calculated to be approximately 50% of the cardiac output and did improve significantly over a 10‐day period posttransplant. However, in 1984, Van Thiel et al.14 from the University of Pittsburgh proposed, but without providing specific data, that a partial pressure of arterial oxygen (PaO2) <50 mm Hg due to pulmonary shunts should be an “absolute contraindication” to liver transplantation. These authors had noted “empirically that shunts that do not close postoperatively for periods of up to several weeks and that the resultant hypoxemia experience post‐operatively, is yet another adverse factor that frequently turns a hopeful situation into a hopeless effort.”
By the early 1990s, a series of case reports demonstrated that varying degrees of HPS could resolve after LT in adults and children. Over time, with mounting successes combined with a dismal outlook if transplant was not done (5‐year survival rate of 23%), HPS became an ”indication” for LT.15 Importantly, because of the poor correlation between the severity of HPS and the severity of liver disease, current American Association for the Study of Liver Diseases (AASLD) guidelines from the AASLD and the International Liver Transplant Society (ILTS) suggest holding an “expedited review” for transplant consideration. To that end, in the setting of HPS, a “Model for End‐Stage Liver Disease (MELD) score exception” policy currently exists for moderate to severe HPS (PaO2 < 60 mm Hg).16 It remains prudent to advise that the transplant be done in experienced centers, especially when the arterial hypoxemia is severe (PaO2 < 50 mm Hg), because of the challenges in the immediate posttransplant critical care time period.17 Despite the severity of HPS, expecting complete resolution of the syndrome posttransplant in the era of MELD exceptions has become the norm.18
Portopulmonary Hypertension
Outcomes after LT attempts in the setting of POPH and the reporting of those outcomes, have followed a rather tumultuous course since the first descriptions in the early 1990s. Yoshida et al.,9 from the University of Western Ontario, described two interesting cases of POPH: one (extrahepatic portal hypertension) treated with a single lung transplant and one (chronic active hepatitis) treated with a LT. Pulmonary artery hypertension recurred in the transplanted lung 5 months posttransplant but was cured in the other patient with a successful LT. This was the first suggestion that the liver was the culprit inducing pulmonary artery hypertension. Over the years, private discussions at national meetings alluded to the unexpected occurrences of intraoperative death when transplant was attempted in the setting of POPH, as first reported in the literature by Ramsay et al.,19 at Baylor Medical Center, Dallas, Texas. Subsequent descriptions of transplant attempts and outcomes in the setting of POPH were summarized in a literature review and substantiated in a multicenter database experience.20, 21 In analyzing POPH transplant outcomes in 75 patients, a pretransplant mPAP >35 mm Hg appeared to be associated with poor survival during the transplant hospitalization (35% mortality rate). Variable use of intravenous (IV) prostacyclin to treat POPH was a very limited, yet a hopeful and an anecdotal approach to improve POPH posttransplant survival.
POPH 5‐year survival rates without medical treatment and with uncontrolled medical treatments, but not LT, have ranged from 14% to 40%, respectively.22, 23 There has never been a controlled trial to assess pulmonary vasodilator therapy impact in liver transplantation. Intuitively, it seemed reasonable to treat transplant patients with POPH before they experienced development of moderate‐to‐severe POPH and to attempt transplant if treatments could improve the hemodynamic and right ventricular function. To that end, and because of the poor correlation between the severity of POPH and the severity of liver diseases, a MELD exception for POPH was proposed and initiated in 2006.24
This approach has been justified because approximately 50% of patients with POPH, treated successfully prior to transplant (i.e., mPAP deceased to <35 mm Hg), could discontinue the pulmonary vascular modulators and be considered hemodynamically cured of POPH.25
However, it is currently cautioned that POPH, by itself, is not an indication for LT, especially in those with low native MELD score (<15), due to the unpredictable risks and outcomes after transplantation.26 For those with MELD score >15 and baseline PVR >450 dyne/s/cm5, wait‐list mortality is increased, but transplant risk appears to lessen if mPAP can be decreased to <35 mm Hg with acceptable right ventricle function.27 The latter parameter is perhaps the most important and in need of further study.
Some Final Conjectures
We have not identified specific circulating mediators directly linked to either HPS or POPH. Current thinking points toward the lack of a “good substance” emanating from the hepatic veins as the cause for intrapulmonary vascular dilatation (IPVD) in HPS, and the lack of clearance of a “bad substance” that invokes pulmonary vasoconstriction and endothelial/smooth muscle proliferation causing obstruction to flow in POPH. Time and more study will determine whether these ideas are sound.
Interestingly, we have also seen that HPS can spontaneously resolve (seen in alcoholic patients with cirrhosis who stop drinking; personal observations). Such resolution has never been reported in POPH, but a fascinating and more concerning “resolution” of HPS has been reported by Aucejo et al.28 from the Cleveland Clinic. These authors described HPS resolution posttransplant, which transitioned into posttransplant pulmonary artery hypertension. The thought has been that the pulmonary vascular pathophysiology of HPS and POPH, respectively, could coexist, and that HPS could essentially “offload” the right ventricle pretransplant at the expense of worsening oxygenation. With posttransplant resolution of vascular dilatations caused by HPS, any obstruction to pulmonary blood flow is now unopposed and manifests itself as evolving pulmonary artery hypertension. This clinical picture, albeit uncommon, has been well documented and necessitated the initiation of pulmonary vasomodulator therapy. As Koch et al.29 have pointed out, indeed pulmonary artery hypertension (should we still call it POPH?) may evolve de novo after LT for reasons that remain unclear.
The historical lessons of HPS and POPH are fascinating and evolving. The possible links (and causative circulating mediators) between these two syndromes remain enigmatic. For those interested in a more detailed chronological perspective of HPS and POPH, Tables 2 and 3 summarize selected key studies and contributions that have led to the current understanding of syndrome pathophysiology and the specific implications for LT.
Table 2.
HPS: A Chronology of Selected Milestones
| Year | First Author | Observation/Contribution |
|---|---|---|
| 1884 | Fluckiger1 | Cyanosis, clubbing in cirrhosis first described |
| 1938 | Keys30 | Hypoxemia in cirrhosis caused by rightward shift of the hemoglobin/oxygen (Hgb‐O2) curve |
| 1953 | Wilson31 | Hypoxemia in cirrhosis due to “venous admixture” rather than Hgb‐O2 curve shift |
| 1956 | Rydel32 | First clinic pathological case report of HPS |
| 1957 | Calabresi33 | Unusual portal to pulmonary vein connections described |
| 1960 | Rodman34 | “Unsaturation of arterial blood” due to venous admixture common in cirrhosis |
| 1963 | Mellemgaard35 | Portal to pulmonary vein connections unlikely to contribute to hypoxemia |
| 1966 | Berthelot36 | Lung pathologies of vascular dilatation and possible angiogenesis described |
| 1968 | Starzl13 | First LTs attempted in the setting of presumed intrapulmonary shunting |
| 1977 | Kennedy2 | The term “hepatopulmonary syndrome” first coined |
| 1984 | Van Thiel14 | HPS with PaO2 < 50 mm Hg an “absolute contraindication” to LT |
| 1987 | Krowka37 | Small series using almitrine bismesylate for HPS; no improvement in PaO2 |
| 1988 | Maddrey38 | HPS with PaO2 < 50 mm Hg a “relative contraindication” to LT |
| 1989 | Edell39 | MIGET characterized reasons for the hypoxemia of HPS |
| 1990 | Krowka40 | Screening for HPS using contrast‐enhanced transthoracic echocardiography described |
| 1990 | Stoller41 | HPS resolves in an adult with PBC after LT |
| 1992 | LaBerge42 | HPS resolves in two children after LT |
| 1992 | Chang4 | Common bile duct ligation experimental model in a rat developed for HPS |
| 1996 | Krowka15 | Mayo cases and literature review: progressive HPS an “indication” for HPS |
| 1997 | Fallon5 | First describes nitric oxide implication in the rat model of HPS |
| 1998 | Whyte43 | Use of 99mTcMAA lung‐brain scanning quantifies HPS severity |
| 1999 | Martinez44 | Association between HPS and other common respiratory disorders described |
| 1999 | Egawa45 | Living donor LT for HPS reported and excellent long‐term outcomes |
| 2000 | Schenk46 | Small series showing IV methylene blue improved HPS hypoxemia in intensive care unit setting |
| 2003 | Taille47 | Resolution of HPS post‐LT dependent on severity pretransplant |
| 2003 | Schenk48 | HPS reported as an independent risk for poor outcome in liver disease |
| 2004 | Rodriguez‐Roisin49 | ERS consensus committee defines HPS diagnostic criteria |
| 2005 | Swanson50 | 5‐Year natural history (without transplant) of HPS described |
| 2006 | Fallon16 | MELD exception criteria (PaO2 < 60 mm Hg) for HPS began |
| 2006 | Gomez51 | Nebulized l‐NAME decreased exhaled nitric oxide but does not improve PaO2 in HPS |
| 2008 | Rodriguez‐Roisin52 | New England Journal of Medicine review article: hepatopulmonary syndrome: liver‐induced lung vascular disorder |
| 2008 | Fleming53 | Use of ECMO after LT for refractory HPS |
| 2010 | Roberts54 | Genetic risk factors for HPS described |
| 2010 | Gupta17 | Excellent LT outcome in severe HPS (PaO2 < 50 mm Hg) |
| 2013 | Iyer18 | Excellent LT outcomes for HPS in the era of MELD exception |
| 2014 | Goldberg55 | Impact of MELD exception for HPS described from the UNOS database |
| 2016 | Krowka26 | ILTS consensus practice guidelines for HPS published |
| 2019 | Raevens56 | Excellent HPS outcomes after LT: Eurotransplant experience |
| 2019 | Kawut11 | First randomized, controlled trial in HPS (sorafenib); no improvement in PaO2 |
Table 3.
POPH: A Chronology of Selected Milestones
| Year | First Author | Observation/Contribution |
|---|---|---|
| 1951 | Mantz6 | First case report of POPH; embolic thrombi suspected from portal system |
| 1960 | Naeye57 | Series of six POPH cases, some without embolic thrombi; other pathology suggested |
| 1968 | Senior58 | Reported that POPH could follow years after portosystemic shunt surgery |
| 1979 | LeBrec59 | Series of POPH cases suggesting toxic splanchnic bed substances as possible etiology |
| 1983 | McDonnell60 | US autopsy series; 1.5% incidence rate of POPH in cirrhosis |
| 1987 | Edwards61 | POPH autopsy series describing “plexogenic arteriopathy” |
| 1990 | Groves62 | NIH registry of PH; 9% had cirrhosis of the liver |
| 1991 | Hadengue63 | POPH did not correlate with portal hypertension; cardiac output main factor in survival |
| 1991 | Robalino64 | Literature review: 5‐year POPH survival rate with “standard” vasodilator treatment was 4% |
| 1993 | Yoshida9 | First report that LT alone could not reverse severe POPH |
| 1996 | Castro65 | Mayo series showing LT could be safely done when mPAP < 35 mm Hg |
| 1997 | Ramsay19 | First description of intraoperative deaths during LT because of POPH |
| 1999 | Tuder66 | Pulmonary artery prostacyclin endothelium deficiency in POPH autopsy specimens |
| 1999 | Krowka67 | Mayo series showing IV prostacyclin improved PVR, mPAP, and cardiac output up to 30 months in POPH |
| 2000 | Krowka20 | POPH literature review: pre‐LT mPAP > 35 mm Hg a risk factor for post‐LT death |
| 2004 | Krowka21 | Multicenter POPH database; 35% mortality rate post‐LT if mPAP > 35 mm Hg |
| 2005 | Hoeper68 | German experience using ERA‐Bosentan in POPH |
| 2006 | Krowka24 | MELD exception policy initiated; mPAP must be less than 35 mmHg with POPH treatment |
| 2006 | Aucejo28 | First description of PH evolving after LT for HPS |
| 2006 | Krowka69 | Mayo POPH echo/right‐heart catheterization screening study; if RVSP > 50 mm Hg, POPH in 66% |
| 2008 | Swanson22 | Mayo Clinic outcomes for POPH; 14% 5‐year survival rate if no medical treatment |
| 2008 | Le Pavec70 | POPH in the French PH registry; 5‐year POPH survival rate of 68% |
| 2008 | Kawut71 | Clinical risks factor for POPH described |
| 2009 | Roberts72 | Genetic factors in POPH first reported |
| 2009 | Simonneau73 | POPH recognized and classified in the WHO Group I of PH |
| 2009 | Koch29 | Series describing PH de novo after LT |
| 2010 | Bandara74 | First report of living donor LT for POPH |
| 2011 | Cartin‐Ceba75 | Small series first report ERA‐ambrisentan for POPH; normalization of PVR occurred |
| 2011 | Talwalkar76 | Spontaneous portosystemic shunts correlated with severity of POPH |
| 2012 | Krowka23 | US REVEAL registry: 40% 5‐year survival rate in POPH with medical treatment only |
| 2014 | Goldberg77 | UNOS POPH MELD exception study: post‐LT outcomes for POPH: 3‐year survival rate of 64% |
| 2015 | DuBrock78 | Current and proposed medical treatments for POPH summarized |
| 2016 | Verma79 | Multicenter UK LT outcomes in POPH; 42.9% deaths within 5 years of LT |
| 2017 | DeMartino80 | LT safely done if mPAP > 35 mm Hg when PVR/echo of right ventricle normal |
| 2017 | DuBrock27 | UNOS POPH MELD exception study: pre‐LT PVR and MELD wait‐list death correlates |
| 2018 | Reymond81 | Multicenter French LT outcomes in POPH; 61% normalized PVR post‐LT |
| 2019 | Nikolic82 | Bone morphogenetic protein deficiency in POPH/first animal model/biomarker described |
| 2019 | Krowka12 | PORTICO; first randomized, placebo‐controlled trial in POPH using ERA‐macitentan |
One final and simple observation should be stressed. Despite the risks in treating and transplanting patients with either HPS or POPH, it remains remarkable that replacement of the liver can result in total reversal of the severe dysfunction of a distal organ (e.g., the lungs) that otherwise would have dismal outcomes.
Series Editor’s Postscript
In his fastidious review of the progress that has been made in recognizing and characterizing both HPS and POPH, Michael Krowka has given us a step‐by‐step account of the history of these two syndromes, since the term HPS was first coined in 1977. Although the mediators of these circulatory abnormalities in the lungs of patients with cirrhosis have yet to be identified, it is tempting to speculate that these syndromes either result from the effects of pulmonary “vasculotoxins” released from the diseased liver into the hepatic veins and hence into the pulmonary arteries, or from the cirrhosis‐related deficiency of a pulmonary “vasculoprotective“ agent.
Fortunately, this Gordian knot can be cut, so to speak, by a LT surgeon, because liver replacement can cure both syndromes. Very occasionally POPH can supervene posttransplant, sometimes when HPS was present preoperatively. The detailed histories of HPS and POPH that Michael Krowka has labored to provide here will serve us well by giving context to future developments in this field.
Biography
Potential conflict of interest: Nothing to report.
References
- 1. Fluckiger M. Vorkommen von trommelschlagelformigen fingerendphalangen ohne chronische veriinderungen an den lungen oder am herzen. Wiener Medizinische Wochenschrift 1884;49:1457‐1458. [Google Scholar]
- 2. Kennedy TC, Knudsen RJ. Exercise‐aggravated hypoxemia and orthodeoxia in cirrhosis. Chest 1977;72:305‐309. [DOI] [PubMed] [Google Scholar]
- 3. Hervé P, Lebrec D, Brenot F, et al. Pulmonary vascular disorders in portal hypertension. Eur Respir J 1998;11:1153‐1166. [DOI] [PubMed] [Google Scholar]
- 4. Chang SW, Ohara N. Pulmonary circulatory dysfunction in rats with biliary cirrhosis. Am Rev Respir Dis 1992;148:798‐805. [DOI] [PubMed] [Google Scholar]
- 5. Fallon MB, Abrams GA, Luo B, et al. The role of endothelial nitric oxide synthase in the pathogenesis of a rat model of hepatopulmonary syndrome. Gastroenterology 1997;113:606‐614. [DOI] [PubMed] [Google Scholar]
- 6. Mantz FA, Craig E. Portal axis thrombosis with spontaneous portacaval shunt and resultant cor pulmonale. Arch Pathol Lab Med 1951;52:91‐97. [PubMed] [Google Scholar]
- 7. Krowka MJ, Edwards WD. A spectrum of pulmonary vascular pathology in portopulmonary hypertension. Liver Transpl 2000;6:2412‐2422. [DOI] [PubMed] [Google Scholar]
- 8. Wagenvoort CA. Plexogenic arteriopathy. Thorax 1994;49(suppl):S39‐S45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yoshida EM, Erb SR, Pflugfelder PW, et al. Single‐lung versus liver transplantation for the treatment of portopulmonary hypertension: A comparison of two patients. Transplantation 1993;55:688‐690. [PubMed] [Google Scholar]
- 10. Reuben A. There is nothin’ like a Dame. Hepatology 2002;35:983‐985. [DOI] [PubMed] [Google Scholar]
- 11. Kawut SM, Ellenberg SS, Krowka MJ, et al. Sorafenib in hepatopulmonary syndrome (SHPS): A randomized, double‐blind placebo‐controlled trial. Liver Transpl; 10.1002/lt.25438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Krowka MJ, Sitbon O, Kim N, et al. A randomized, placebo controlled trial of macitentan in portopulmonary hypertension (PORTICO). Lancet Respir Med 2019; 10.1016/S2213-2600(19)30091-8 (in press). [DOI] [PubMed] [Google Scholar]
- 13. Starzl TE, Groth CG, Brettschneider L, et al. Extended survival in 3 cases of orthotopic homotransplantation of the human liver. Surgery 1968;63:549‐563. [PMC free article] [PubMed] [Google Scholar]
- 14. Van Thiel DH, Schade RR, Gavaler JS, et al. Medical aspects of liver transplantation. Hepatology 1984;4(suppl 1):79S‐83S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Krowka MJ, Porayko MK, Plevak DJ, et al. Hepatopulmonary syndrome with progressive hypoxemia as an indication for liver transplantation: Case reports and literature review. Mayo Clin Proc 1996;72:44‐53. [DOI] [PubMed] [Google Scholar]
- 16. Fallon MB, Mulligan DC, Gish RG, et al. Model for end‐stage liver disease (MELD) exception for hepatopulmonary syndrome. Liver Transpl 2006;12:S105‐S107. [DOI] [PubMed] [Google Scholar]
- 17. Gupta S, Castel H, Rao RV, et al. Improved survival after liver transplantation in patients with hepatopulmonary syndrome. Am J Transplant 2010;10:354‐363. [DOI] [PubMed] [Google Scholar]
- 18. Iyer V, Swanson KL, Cartin‐Ceba R, et al. Hepatopulmonary syndrome: Favorable outcomes in the MELD exception era. Hepatology 2013;57:2427‐2435. [DOI] [PubMed] [Google Scholar]
- 19. Ramsay MAE, Simpson BR, Nguyen AT, et al. Severe pulmonary hypertension in liver transplant candidates. Liver Transpl Surg 1997;3:494‐500. [DOI] [PubMed] [Google Scholar]
- 20. Krowka MJ, Plevak DJ, Findlay JF, et al. Pulmonary hemodynamics and per‐operative cardiopulmonary mortality in patients with portopulmonary hypertension undergoing liver transplantation. Liver Transpl 2000;6:453‐458. [DOI] [PubMed] [Google Scholar]
- 21. Krowka MJ, Mandell MS, Ramsay MAE, et al. Hepatopulmonary syndrome and portopulmonary hypertension: A report of the multicenter liver transplant database. Liver Transpl 2004;10:174‐182. [DOI] [PubMed] [Google Scholar]
- 22. Swanson KL, Wiesner RH, Nyberg SL, et al. Survival in portopulmonary hypertension: Mayo clinic experience categorized by treatment subgroups. Am J Transplant 2008;8:2445‐2453. [DOI] [PubMed] [Google Scholar]
- 23. Krowka MJ, Miller DP, Barst RJ, et al. Portopulmonary hypertension: A report from the US‐based REVEAL registry. Chest 2012;141:906‐915. [DOI] [PubMed] [Google Scholar]
- 24. Krowka MJ, Fallon MB, Mulligan DC, et al. Model for end‐stage liver disease (MELD) exception for portopulmonary hypertension. Liver Transpl 2006;12:S114‐S116. [DOI] [PubMed] [Google Scholar]
- 25. Krowka MJ. The liver‐lung vascular connection. BRN Rev 2017;23:204‐219. [Google Scholar]
- 26. Krowka MJ, Fallon MB, Kawut SM, et al. International Liver Transplant Society Practice Guidelines: Diagnosis and management of hepatopulmonary syndrome and portopulmonary hypertension. Transplantation 2016;100:144‐1452. [DOI] [PubMed] [Google Scholar]
- 27. DuBrock HM, Goldberg DS, Sussman NL, et al. Predictors of waitlist mortality in portopulmonary hypertension. Transplantation 2017;101:1609‐1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Aucejo F, Miller C, Vogt D, et al. Pulmonary hypertension after liver transplantation in patients with antecedent hepatopulmonary syndrome: A report of 2 cases and review of the literature. Liver Transpl 2006;12:1278‐1282. [DOI] [PubMed] [Google Scholar]
- 29. Koch DG, Caplan M, Reuben A. Pulmonary hypertension after liver transplantation: Case presentation and review. Liver Transpl 2009;15:407‐415. [DOI] [PubMed] [Google Scholar]
- 30. Keys A, Snell AM. Respiratory properties of the arterial blood in normal man and in patients with disease of the liver: Position of the oxygen dissociation curve. J Clin Invest 1938;17:59‐67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wilson RH, Ebert RV, Borden CW, et al. The determinations of blood flow through nonventilated portions of the normal lung and diseased lung. Am Rev Tuberc 1953;68:177‐187. [DOI] [PubMed] [Google Scholar]
- 32. Rydell R, Hoffbauer FW. Multiple pulmonary arteriovenous fistulae in juvenile cirrhosis. Am J Med 1956;21:450‐459. [DOI] [PubMed] [Google Scholar]
- 33. Calabresi P, Abelman WH. Portocaval and portopulmonary anastomoses in Laennec’s cirrhosis and in heart failure. J Clin Invest 1957;36:1257‐1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Rodman T, Sobel M, Close HP. Arterial oxygen saturation and the ventilation‐perfusion defect of Laennec’s cirrhosis. N Engl J Med 1960;263:73‐77. [DOI] [PubMed] [Google Scholar]
- 35. Mellemgaard K, Winkler K, Tygstrup N, et al. Sources of venoarterial admixture in portal hypertension. J Clin Invest 1963;42:1399‐1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Berthelot P, Walker JG, Sherlock S, et al. Arterial changes in the lungs in cirrhosis of the liver: Lung spider nevi. N Engl J Med 1966;274:291‐298. [DOI] [PubMed] [Google Scholar]
- 37. Krowka MJ, Cortese DA. Severe hypoxemia associated with liver disease: Mayo Clinic experience and the experimental use of almitrine bismesylate. Mayo Clin Proc 1987;62:164‐173. [DOI] [PubMed] [Google Scholar]
- 38. Maddrey WC, Van Thiel DH. Liver transplantation: An overview. Hepatology 1988;8:948‐959. [DOI] [PubMed] [Google Scholar]
- 39. Edell ES, Cortese DA, Krowka MJ, et al. Severe hypoxemia and liver disease. Am Rev Respir Dis 1989;140:1631‐1635. [DOI] [PubMed] [Google Scholar]
- 40. Krowka MJ, Tajik AJ, Dickson ER, et al. Intrapulmonary vascular dilatation (IPVD) in liver transplant candidates. Chest 1990;97:1165‐1170. [DOI] [PubMed] [Google Scholar]
- 41. Stoller JK, Moodie D, Schiavone WA, et al. Reduction of intrapulmonary shunt and resolution of digital clubbing associated with primary biliary cirrhosis after liver transplantation. Hepatology 1990;11:54‐58. [DOI] [PubMed] [Google Scholar]
- 42. LaBerge JM, Brandt ML, Lebecque P, et al. Reversal of cirrhosis‐related pulmonary shunting in two children by orthotopic liver transplantation. Transplantation 1992;53:1135‐1138. [PubMed] [Google Scholar]
- 43. Whyte MKB, Hughes JMB, Peters AM, et al. Analysis of intrapulmonary right to left shunt in hepatopulmonary syndrome. J Hepatol 1998;29:85‐93. [DOI] [PubMed] [Google Scholar]
- 44. Martinez G, Barbera JA, Navasa M, et al. Hepatopulmonary syndrome associated with cardiorespiratory disease. J Hepatol 1999;30:882‐889. [DOI] [PubMed] [Google Scholar]
- 45. Egawa H, Hasahara M, Inomata Y, et al. Long‐term outcome of living related liver transplantation for patients with intrapulmonary shunting and strategy for complications. Transplantation 1999;67:712‐717. [DOI] [PubMed] [Google Scholar]
- 46. Schenk P, Madl C, Rezaie‐Majd S, et al. Methylene blue improves hepatopulmonary syndrome. Ann Intern Med 2000;133:701‐706. [DOI] [PubMed] [Google Scholar]
- 47. Taille C, Cadranal J, Bellocq A, et al. Liver transplantation for hepatopulmonary syndrome: A ten‐year experience in Paris, France. Transplantation 2003;75:1482‐1489. [DOI] [PubMed] [Google Scholar]
- 48. Schenk P. Prognostic significance of hepatopulmonary syndrome in patients with cirrhosis. Gastroenterology 2003;125:1042‐1052. [DOI] [PubMed] [Google Scholar]
- 49. Rodriguez‐Roisin R, Fallon MB, Kawut SM, et al. Pulmonary‐hepatic disorders (PHD). Eur Respir J 2004;24:861‐880. [DOI] [PubMed] [Google Scholar]
- 50. Swanson KL, Wiesner RH, Krowka MJ. Natural history of hepatopulmonary syndrome: Impact of liver transplantation. Hepatology 2005;41:1122‐1129. [DOI] [PubMed] [Google Scholar]
- 51. Gomez FP, Barbera JA, Roca J, et al. Effects of nebulized NG‐nitro‐L‐arginine methyl ester (L‐NAME) in patients with hepatopulmonary syndrome. Hepatology 2006;43:1084‐1091. [DOI] [PubMed] [Google Scholar]
- 52. Rodriguez‐Roisin R, Krowka MJ. Hepatopulmonary syndrome—a liver‐induced lung vascular disorder. N Engl J Med 2008;358:2378‐2387. [DOI] [PubMed] [Google Scholar]
- 53. Fleming GM, Cornell TT, Welling T, et al. Hepatopulmonary syndrome: Use of extracorporeal life support for life threatening hypoxia following liver transplantation. Liver Transpl 2008;14:966‐970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Roberts KE, Kawut SM, Krowka MJ, et al. Genetic risk for hepatopulmonary syndrome in patients with advanced liver disease. Gastroenterology 2010;139:130‐139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Goldberg DS, Krok K, Batra S, et al. Impact of the hepatopulmonary syndrome MELD exception policy on outcomes of patients after liver transplantation: An analysis of the UNOS database. Gastroenterology 2014;146:1256‐1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Raevens S, Rogiers X, Geerts A, et al. Outcome of liver transplantation for hepatopulmonary syndrome: A Eurotransplant experience. Eur Respir J 2019;53:180‐196. [DOI] [PubMed] [Google Scholar]
- 57. Naeye RL. “Primary” pulmonary hypertension with co‐existing portal hypertension: A retrospective study of 6 cases. Circulation 1960;22:376‐384. [DOI] [PubMed] [Google Scholar]
- 58. Senior RM, Britton RC, Turino GM, et al. Pulmonary hypertension associated with cirrhosis of the liver and with portocaval shunts. Circulation 1968;37:88‐96. [DOI] [PubMed] [Google Scholar]
- 59. LeBrec D, Capron JP, Dhumeaux D, et al. Pulmonary hypertension complicating portal hypertension. Am Rev Respir Dis 1979;120:849‐856. [DOI] [PubMed] [Google Scholar]
- 60. McDonnell PJ, Toye PA, Hutchins GM. Primary pulmonary hypertension and cirrhosis: Are they related? Am Rev Respir Dis 1983;127:437‐441. [DOI] [PubMed] [Google Scholar]
- 61. Edwards BS, Weir EK, Edwards WD, et al. Coexistent pulmonary hypertension and portal hypertension: Morphologic and clinical features. J Am Coll Cardiol 1987;10:1233‐1238. [DOI] [PubMed] [Google Scholar]
- 62. Groves BM, Brundage BH, Elliot CG. Pulmonary hypertension associated with hepatic cirrhosis In: Fishman AP, ed. The pulmonary circulation: Normal and abnormal. Philadelphia: University of Pennsylvania Press; 1990:359‐369. [Google Scholar]
- 63. Hadengue A, Benhayun MK, Lebrec D, et al. Pulmonary hypertension complicating portal hypertension: Prevalence and relation to splanchnic hemodynamics. Gastroenterology 1991;100:1023‐1030. [DOI] [PubMed] [Google Scholar]
- 64. Robalino BD, Moodie DS. Association between primary pulmonary hypertension and portal hypertension: Analysis of its pathophysiology and clinical, laboratory and hemodynamic manifestations. J Am Coll Cardiol 1991;17:492‐498. [DOI] [PubMed] [Google Scholar]
- 65. Castro M, Krowka MJ, Schroeder DR, et al. Frequency and clinical implications of increased pulmonary artery pressures in liver transplant patients. Mayo Clin Proc 1996;71:543‐551. [DOI] [PubMed] [Google Scholar]
- 66. Tuder RM, Cool CD, Geraci MW, et al. Prostacyclin synthase expression is decreased in the lungs from patients with severe pulmonary hypertension. Am J Respir Crit Care Med 1999;159:1925‐1932. [DOI] [PubMed] [Google Scholar]
- 67. Krowka MJ, McGoon MD, Frantz RP, et al. Improvement in pulmonary hemodynamics during intravenous epopostenol (prostacyclin): A study of 15 patients with moderate to severe portopulmonary hypertension. Hepatology 1999;30:641‐648. [DOI] [PubMed] [Google Scholar]
- 68. Hoeper MM, Halank M, Marx C, et al. Bosentan therapy for portopulmonary hypertension. Eur Respir J 2005;25:502‐508. [DOI] [PubMed] [Google Scholar]
- 69. Krowka MJ, Swanson KL, Frantz RP, et al. Portopulmonary hypertension: Results of a 10 year screening program for portopulmonary hypertension. Hepatology 2006;44:1502‐1510. [DOI] [PubMed] [Google Scholar]
- 70. Le Pavec J, Souza R, Herve P, et al. Portopulmonary hypertension: Survival and prognostic factors. Am J Respir Crit Care Med 2008;178:637‐643. [DOI] [PubMed] [Google Scholar]
- 71. Kawut S, Krowka MJ, Trotter JF, et al. Clinical risk factors for portopulmonary hypertension. Hepatology 2008;48:196‐203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Roberts KE, Fallon MB, Krowka MJ, et al. Genetic risk factors for portopulmonary hypertension in patients with advanced liver disease. Am J Respir Crit Care Med 2009;179:835‐842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Simonneau G, Robbins I, Beghetti M, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol 2009;54:S43‐S54. [DOI] [PubMed] [Google Scholar]
- 74. Bandara M, Gordon FD, Sarwar A, et al. Successful outcomes following living donor liver transplantation for portopulmonary hypertension. Liver Transpl 2010;16:983‐989. [DOI] [PubMed] [Google Scholar]
- 75. Cartin‐Ceba R, Swanson KL, Iyer V, et al. Safety and efficacy of ambrisentan for the treatment of portopulmonary hypertension. Chest 2011;139:109‐114. [DOI] [PubMed] [Google Scholar]
- 76. Talwalkar JA, Swanson KL, Krowka MJ, Kamath P. Prevalence of spontaneous portosystemic shunts in portopulmonary hypertension and effects on treatment. Gastroenterology 2011;141:1673‐1679. [DOI] [PubMed] [Google Scholar]
- 77. Goldberg DS, Batra SJ, Sahay SJ, et al. MELD exceptions for portopulmonary hypertension: Current policy and future implementation. Am J Transplant 2014;14:2081‐2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. DuBrock HM, Channick RN, Krowka MJ. What’s new in the treatment of portopulmonary hypertension. Expert Rev Gastroenterol Hepatol 2015;9:983‐992. [DOI] [PubMed] [Google Scholar]
- 79. Verma S, Hand F, Armstrong MJ, et al. Portopulmonary hypertension: Still an appropriate consideration for liver transplantation? Liver Transpl 2016;22:1637‐1642. [DOI] [PubMed] [Google Scholar]
- 80. DeMartino ES, Cartin‐Ceba R, Findlay JK, et al. Frequency and outcomes of patients with increased mean pulmonary artery pressure at the time of liver transplantation. Transplantation 2017;101:101‐107. [DOI] [PubMed] [Google Scholar]
- 81. Reymond M, Barbier L, Salame E, et al. Does portopulmonary hypertension impede transplantation in cirrhotic patients? A French multicenter retrospective study. Transplantation 2018;102:616‐622. [DOI] [PubMed] [Google Scholar]
- 82. Nikolic I, Yung LM, Yang P, et al. Bone morphogenetic protein 9 is a mechanistic biomarker of portpulmonary hypertension. Am J Respir Crit Care Med 2019;199:891‐902. [DOI] [PMC free article] [PubMed] [Google Scholar]


