Abstract
Objective
Since initial description by Forero for thoracic region, ultrasound guided erector spinae plane (ESP) block has experienced several surgeries for postoperative pain management, chronic pain or surgical anesthesia. Although ESP block has been reported to provide effective analgesia in the thoracic region, its effect in lumbar region still unclear. In this study we aimed to showed our successful experience with lumbar ESP block as a main anesthetic technique in fifteen high risk elderly patients undergoing hip surgery with mild propofol sedation.
Materials and Methods
In this observational study high risk elderly fifteen patients received lumbar ESP block as a main anesthetic technique with mild propofol sedation. 40 mL of local anesthetic mixture (20 mL bupivacaine 0.5%, 10 mL lidocaine 2%, and 10 mL normal saline) was administered between the erector spinae muscles and transverse process at the level of the 4th lumbar vertebra. Also we demonstrate magnetic resonance images and discuss the anatomic basis of lumbar ESP block.
Results
All patients’ surgeries were completed without requirement for general anesthesia or local anesthesia infiltration of the surgical site. All patients’ pain scores were <2/10 in the recovery room. Significant contrast spread was observed between the Th12 and L5 transverse process and erector spinae muscle and between multifidus muscle and iliocostal muscle at the L2–4 levels. Contrast material was observed at the anterior of the transverse process spreading to the paravertebral, foraminal and partially epidural area/spaces and also in the areas where the lumbar nerves enter the psoas muscle.
Conclusion
Lumbar ESP block when combined with mild sedoanalgesia provides adequate and safe anesthesia in high risk elderly patients undergoing hip surgery.
Keywords: hip surgery, erector spinae plane block, magnetic resonance imaging, high risk patient
Introduction
Ultrasound-guided erector spinae plane block (ESPB) is an interfascial plane block, first described by Forero et al. [1] in 2016, which is used in the treatment of thoracic neuropathic pain. It was later reported in the treatment of postoperative pain from surgical procedures, ranging from shoulder to hip surgery [2–5].
While ESPB is generally performed at the thoracic vertebral level, in 2017, we reported its effective use in postoperative analgesia in hip surgery. When performed at the lumbar 4th vertebral level, ESPB led to sensorial blockage between Th12 and L4 dermatomes [5]. In a case series published later where lumbar ESPB (L-ESPB) was reported to lead to effective postoperative analgesia in hip and proximal femoral surgery, a computerized tomography imaging demonstrated spread of local anesthetic to the lumbar plexus, leading to an effect similar to lumbar plexus block [6].
There are many advantages of using regional anesthesia techniques in hip surgery. First, it leads to perioperative and postoperative analgesia, therefore decreasing opioid requirement and the incidence of postoperative delirium [7]. Second, regional anesthesia techniques can be used as the main anesthetic method in patients where general or neuroaxial anesthesia should be avoided due to comorbidities. It also allows major procedures such as hip surgery to be completed under sedation.
The use of ultrasound-guided lumbar plexus block, sacral plexus block, paravertebral block, and fascia blocks used alone or in combination for main surgical anesthesia have been reported in many case reports or case series [8–11]. These blocks or their combinations can be lifesaving and improve the quality of life in patients with serious comorbidities.
In lieu of our previous studies and current literature, we hypothesized L-ESPB could be used as the main surgical anesthetic technique in high-risk patients scheduled to undergo hip surgery, as it has a near identical effect. Herein, we report our experience with L-ESPB and mild sedoanalgesia in high-risk patients undergoing hip surgery, demonstrate magnetic resonance images, and discuss the anatomic basis of L-ESPB. Also, we will evaluate the generalizability, feasibility, benefits, and risks, as well as patient and surgeon satisfaction with L-ESPB.
Materials and Methods
This study was conducted at two schools of medicine. At these two institutes, patients undergo preoperative multidisciplinary evaluation. Patients who have American Society of Anesthesiologists (ASA) IV and/or high risk due to comorbidity, use multiple medications, or suffer from respiratory, cardiac, neurologic, or neurological problems were included the study. For such patients where general or neuroaxial anesthesia should be avoided, the lumbar plexus block (alone or in combination with the sacral plexus block) and L-ESPB are routinely available regional anesthetic methods that can be used. This study included patients who underwent written informed consent between June 01, 2018, and December 31, 2018, to use L-ESPB with mild sedoanalgesia as the primary anesthetic technique. All patients were given detailed information preoperatively regarding the anesthesia procedure, including potential complications, by an anesthesia specialist. All surgical procedures were performed by one of two orthopedic surgeons.
Patients’ demographic information, the type of hip fracture and surgery, perioperative sedoanalgesic agents and their dosages, and postoperative pain scores were collected. Prospectively collected data were analyzed retrospectively.
Patients were given 4–6 lt/O2 in the block room. Patients underwent routine monitorization using electrocardiogram, peripheral oxygen saturation, and invasive arterial monitorization. Intravenous (iv) access was secured, and sedation with midazolam 1–2 mg and fentanyl 25–50 mcg was administered.
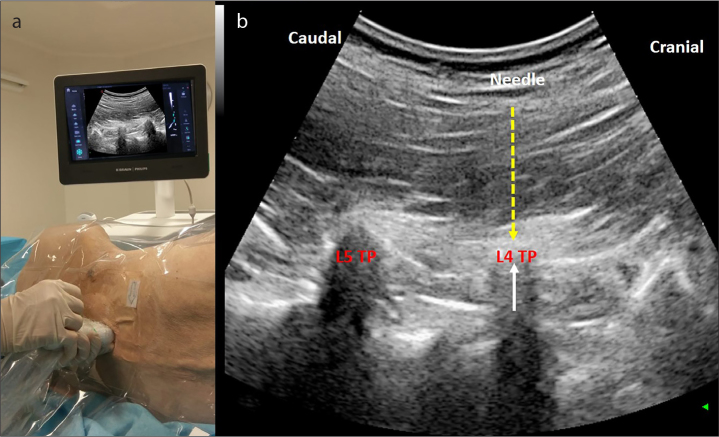
Patients were placed on their side so that the surgical side was placed superiorly. The 4th lumbar vertebra was identified, and a low-frequency convex transducer was placed on the sagittal plane in the midline and slowly moved laterally. The transverse process of the 4th lumbar vertebra was identified 4–6 cm laterally to the midline. A 22-gauge, 80-mm needle was inserted using the out-of-plane technique, until it touched the transverse process. Following negative aspiration, 40 mL of LA (20 mL bupivacaine 0.5%, 10 mL lidocaine 2%, and 10 mL normal saline) was administered between the erector spinae muscles and transverse process in the interfacial plane (Figure 1).
Figure 1. a, b.
a) Probe and ultrasound setup for the ESP block. b) Sonographic image of the L-ESP block.
TP: transverse process
Following block administration, the patients were placed in the supine position, and the spread of sensorial blockage was identified using the cold test after 30 minutes. This test was repeated at 45th and 60th minute if an adequate spread had not been achieved. An adequate spread was defined as dermatomal blockage between L1 and L4. Supplemental oxygen was administered via a facemask with capnography monitoring. Following determination of adequate dermatomal blockage, patients were transferred into the operating room. Propofol infusion at 1.5 mg/kg/hour was commenced and adjusted according to patient’s response during surgery. In patients reporting discomfort or showing facial grimace, 10 mg of ketamine was administered.
Patients were taken to the recovery room at the end of the procedure, and pain scores were assessed using an 11-point verbal rating scale (NRS) (0 meaning “no pain” and 10 meaning “worst pain imaginable”). A Likert scale was used at the 24th hour for patients and surgeons to determine satisfaction (1 meaning “not satisfied” and 5 meaning “completely satisfied”).
A 52-year-old male with a 3-year history of chronic lumbar neuropathic pain presenting at the Division of Pain Management had previously undergone epidural injection and transforaminal injection several times. The patient had undergone L-ESPB with relieved pain and requested L-ESPB to be repeated, 3 months after the initial procedure because the pain returned. Written informed consent was taken from the patient for magnetic resonance imaging (MRI) following L-ESPB. With the patient in the side position, 20 mL bupivacaine, 10 mL lidocaine, 8.6 mL saline, 125 mg/mL metilprednisolon 1 mL, and 0.4 mL gadobutrol (Gadovist 1.0 mmol/mL, BAYER, Istanbul, TURKEY) with 1/200.000 adrenaline were applied at the L4 level (total volume 40 mL). The NRS, which was 8/10 before the procedure, was observed to be 0/10 10 minutes after L-ESPB was performed. The magnetic resonance images were taken 60 minutes following L-ESPB.
Statistical Analysis
Data were analyzed using the The Statistical Package for the Social Sciences (SPSS) version 21 (IBM Corp.; Armonk, NY, USA) package program. Continuous quantitative data were presented as number, mean±standard deviation. A paired samples test was applied to non-parametric data for statistical evaluation of repeated measurements. A p<0.05 was considered significant.
Results
Patients’ demographic data are given in Table 1. Eleven patients underwent hemiarthroplasty (partial hip prosthesis), and 4 underwent intramedullary femur nailing.
Table 1.
Age, gender, comorbidities, side of surgery, hip pathology, and type of surgery for all patients
| No. | Age - Gender | Comorbidities | Side | Hip Pathology | Type of Surgery |
|---|---|---|---|---|---|
| 1 | 86/M | CRF+Pulmonary HT+Advanced COPD, SpO2: 88% | R | Femoral neck fx | Hemiarthroplasty |
| 2 | 92/F | AD+CRF+DM | L | Intertrochanteric femoral fx | Hemiarthroplasty |
| 3 | 94/F | Advanced dementia+COPD | R | Subtrochanteric femoral fx | Intramedullary Nailing-Long |
| 4 | 88/M | Advanced dementia+CHF + COPD, SpO2: 86% | L | Capitis femoris fx | Hemiarthroplasty |
| 5 | 84/M | CHF+CRF, LVEF: 15% | L | Subtrochanteric femoral fx | Intramedullary Nailing-Long |
| 6 | 81/M | Cachexia+AD+CRF | R | Subtrochanteric femoral fx | Intramedullary Nailing-Long |
| 7 | 84/F | DM+COPD+PAP:70 mmHg+Advanced dementia, SpO2: 70% | R | Intertrochanteric femoral fx | Hemiarthroplasty |
| 8 | 82/F | DM+HT+Acute SVE, SpO2: 65% | L | Intertrochanteric femoral fx | Hemiarthroplasty |
| 9 | 80/F | Advanced TI, PAP: 70 mmHg, SpO2: 50% | R | Intertrochanteric femoral fx | Hemiarthroplasty |
| 10 | 85/F | Advanced COPD+PAP:52 mmHg+Parkinsonism, SpO2:76 % | L | Intertrochanteric femoral fx | Hemiarthroplasty |
| 11 | 90/F | Cachexia+Advanced AS+HT, PAP: 45 mmHg | L | Intertrochanteric femoral fx | Hemiarthroplasty |
| 12 | 78/M | CABG+AVF+Active pneumonia | L | Intertrochanteric femoral fx | Hemiarthroplasty |
| 13 | 88/M | Advanced AS+CAD+Active pneumonia | L | Subtrochanteric femoral fx | Intramedullary Nailing-Long |
| 14 | 72/F | CHF+HT+AF+SVE+Asthma | L | Intertrochanteric femoral fx | Hemiarthroplasty |
| 15 | 84/F | HT+DM+CRF+Stomach cancer+Ischemic acute SVE | R | Intertrochanteric femoral fx | Hemiarthroplasty |
R: right; L: left; CRF: chronic renal failure; HT: hypertension; COPD: chronic obstructive pulmonary disease; AD: Alzheimer’s disease; CHF: chronic heart failure; LVEF: left ventricular ejection fraction; PAP: pulmonary artery pressure; SVE: cerebrovascular event; SpO2: partial oxygen saturation at room air; TI: tricuspid insufficiency; CABG: coronary artery bypass grafting; AVR: aortic valve replacement; AS: aortic stenosis; AF: atrial fibrillation; fx: fracture
All surgical procedures were completed without requirement for general anesthesia or local anesthesia infiltration of the surgical site. Surgical time and perioperative propofol and intraoperative ketamine requirement are shown in Table 2. All patients’ NRS scores were <2/10 in the recovery room. All surgeons reported a 5/5 satisfaction score with the anesthetic technique. Of the 15 patients, 3 were unable to report satisfaction due to impaired cognition, 3 reported 4/5 satisfaction, and the remaining 5/5.
Table 2.
Perioperative outcome measures. Values are median (IQR [range])
| Median | IQR | Range | |
|---|---|---|---|
| Block onset time (min) | 30 | 30–30 | 30–45 |
| Duration of surgery (min) | 100 | 80–125 | 45–170 |
| Propofol infusion rate (mg.kg−1.h−1) | 1.5 | 1.25–2 | 1–2.5 |
| Number of intraoperative ketamine (10 mg dose) | 0 | 0–1.55 | 0–2 |
| Duration of first analgesic requirement (hour) | 8 | 7.5–9.5 | 6–14 |
IQ: interquartile range
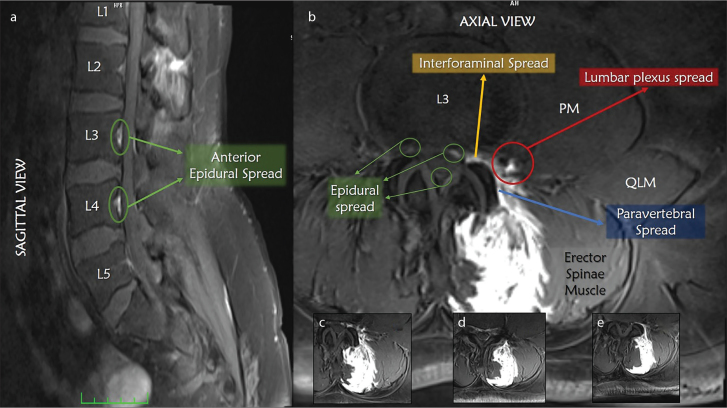
A significant contrast spread was observed between the Th12 and L5 transverse process and erector spinae muscle and between the multifidus muscle and iliocostal muscle at the L2–4 levels. Contrast material was observed at the anterior of the transverse process, spreading to the paravertebral, foraminal, and partially epidural area/spaces and also in the areas where the lumbar nerves enter the psoas muscle (Figure 2).
Figure 2. a–e.
Magnetic resonance imaging scan (T1-weighted with fat saturation) with gadolinium contrast injected at the level of L4. a) Sagittal view and epidural spread. Axial views b) L3, c) L2, d) L4, and e) L5 b).
PM: psoas major; QLM: quadratus lumborum muscle
Yellow arrow: interforaminal spread; red arrow: lumbar plexus spread; blue arrow: paravertebral spread; green arrows: epidural spread
Discussion
This study has demonstrated that the combination of L-ESPB and mild sedoanalgesia is suitable for use in high-risk patients. We have also demonstrated that a high volume of LA in L-ESPB spreads to the lumbar plexus. Therefore L-ESPB acts as lumbar plexus block both radiologically and clinically.
Surgical procedures for hip fractures have a higher mortality when compared to other orthopedic procedures due to the age and comorbidities associated with this group of patients. Depending on the location of the fracture and expected outcomes, partial or total hemiarthroplasty or proximal femoral nail can be performed for proximal fractures, whereas open reduction and internal fixation can be performed for more distal fractures [12, 13].
Not only that there are many nerves that require blockage in hip surgery, but also these nerves may vary. However, it is generally accepted that the hip joint is innervated by the ventral rami of the spinal nerve roots of the lower part of the lumbar plexus (L2–L4) and the upper part of the sacral plexus (L4–S1) [14]. Nerves innervating the hip joint include the nerve to the rectus femoris (or. femoral nerve), branches from the anterior division of the obturator nerve, and the nerve to the quadratus femoris (or. sacral plexus). The cutaneous innervation is from the lateral femoral cutaneous nerve (or. lumbar plexus, L2–L3), lateral cutaneous branch of iliohypogastric nerve (T12 and L1) and subcostal nerve (T12 thoracic nerve). These nerves innervate the area of the superior lateral gluteal region and the proximal lateral thigh, which are the areas involved in skin incision of posterolateral approach to hip joint [15, 16].
Despite their comparatively more difficult application, plexus blocks can be a lifesaving regional anesthesia technique in high-risk patients undergoing hip surgery where general or neuroaxial anesthesia should be avoided. These techniques frequently include the lumbar plexus block, paravertebral block, and sacral plexus blocks with the support of sedoanalgesia [8–10, 17]. There are only a few reports of interfascial plane blocks being used as the main anesthetic method. The use of transversus abdominis plane block and transversalis fascia plane block was reported to contribute as a part of anesthesia modality in hip surgery [11, 15].
In this study, we used L-ESPB as the surgical anesthetic method in hip surgery. LA differs in L-ESPB when compared to ESPB from the thoracic levels in that its spread cephalad and caudally is not so extensive. In a previous study, we demonstrated the LA spread for L-ESPB on computerized tomography from the dorsal of the transverse process from T12 to S1 and also between L1 and L5 to the anterior of the transverse process and to the L2–L4 foraminaes, spreading around the psoas muscle with significant contrasting around the lumbar plexus.
A contrast MRI scan performed and reported in this study demonstrated in more detail that LA spreads to the L2–L5 nerve roots and even to the epidural space. Images also demonstrated a significant LA spread into the psoas muscle, which we believe is why L-ESPB blocks all components of the lumbar plexus. We believe that the LA spread around the psoas muscle led to blockage of the subcostal, ilioinguinal, and iliohypogastric nerves.
The bone innervation of this area is through the upper segment of the sacral plexus (L4–S1). Fibers originating from the L5 root innervate the trochanter major and the posterolateral aspect of the femur, while fibers from S1 innervate the posterior aspect of the femur neck and the posteromedial aspect of the lower half of the femur. MRI images of our patient undergoing L-ESPB demonstrated that LA spread to most nerve roots of the upper sacral plexus. However, no LA spread was observed to the root of S1, which innervates the posterior aspect of the femur neck. However, there are several reports that low-dose sedoanalgesia is effective for pain caused during surgery in this area [9, 10, 18–21].
What advantages could L-ESPB offer over the lumbar plexus block? Foremost, the needle is inserted in an area distant to the vessel and nerves, leading to less risk with regard to nerve damage, vessel damage, and the inadvertent application of LA intravascularly. Complications reported for lumbar plexus block include hematoma, nerve injuries, sciatic spread, and cardiac arrest associated with local anesthesia toxicity [22–24]. Logically, the risk of observing these complications in L-ESPB is significantly lower. In L-ESPB, not only the lumbar plexus, but the dorsal ramus of the lumbar nerves is also blocked, preventing any back pain secondary to perioperative manipulations. L-ESPB also provides an extended sensorial coverage when compared to the lumbar plexus block as LA spreads to the L4–L5 nerve roots that are part of the upper portion of the sacral plexus. This could make L-ESPB advantageous in certain conditions. When considering the cutaneous innervation regarding hip surgery, a large portion of the surgical field lies between L2–L4 dermatomes. L-ESPB is adequate in causing complete blockage of this field.
The use of L-ESPB in hip surgery either combined with another block for surgical anesthesia or for use in postoperative analgesia was previously reported [6, 25]. In that study, the combination of L-ESPB and transmuscular QLB provided sufficient surgical anesthesia in high-risk patients undergoing hemiarthroplasty with minimal sedoanalgesia. Transmuscular QLB provides effective postoperative analgesia for congenital hip dislocation in pediatrics, and also adult hip surgery has been previously reported by our regional anesthesia team [26, 27]. However, our study is the first to report the use of L-ESPB with low-dose sedation as an effective, safe, and feasible method in high-risk and advanced-age patients, in lieu of magnetic resonance images and anatomical bases. Although not statistically analyzed, all patients’ perioperative hemodynamic parameters were stable. Comparison of L-ESPB with neuroaxial anesthesia techniques will be useful.
The first limitation to our study is that it does not evaluate perioperative hemodynamic data, postoperative analgesia requirements, and long-term pain evaluation. Another limitation is adjusting our propofol infusion according to clinical observation and the response of the patient during surgery. Target-controlled infusion of propofol using the Marsh model or adjusting propofol infusion doses with Bispectral index monitorization could have been more appropriate. Finally, this manuscript should be considered a feasibility study and the report of a new technique and its anatomical bases. More generalizable results can be achieved through randomized controlled studies.
The L-ESPB block, when combined with mild sedoanalgesia, provides adequate and safe anesthesia in high-risk and advanced-age patients undergoing hip surgery. Larger controlled studies, as well as comparisons with other regional anesthesia techniques, are required. Also, anatomic studies to further confirm the spread of local anesthetics and the nerves targeted will be useful.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the Ethics Committee of Ataturk University.
Informed Consent: Written informed consent was obtained from the patient who participated in this Study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – A.A., S.T.; Design - A.A., S.T., M.Ç.; Supervision - Z.O., H.A.A.; Resources - M.E.A.; Materials - A.A., S.T., M.E.A.; Data Collection and/or Processing - A.A., S.T., M.E.A.; Analysis and/or Interpretation - Z.O., H.A.A.; Literature Search - A.A., S.T., M.Ç.; Writing Manuscript - A.A., S.T., M.Ç.; Critical Review - Z.O., H.A.A.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The Erector Spinae Plane Block: A Novel Analgesic Technique in Thoracic Neuropathic Pain. Reg Anesth Pain Med. 2016;41:621–7. doi: 10.1097/AAP.0000000000000451. [DOI] [PubMed] [Google Scholar]
- 2.Forero M, Rajarathinam M, Adhikary SD, Chin KJ. Erector spinae plane block for the management of chronic shoulder pain: a case report. Can J Anaesth. 2018;65:288–93. doi: 10.1007/s12630-017-1010-1. [DOI] [PubMed] [Google Scholar]
- 3.Bonvicini D, Tagliapietra L, Giacomazzi A, Pizzirani E. Bilateral ultrasound-guided erector spinae plane blocks in breast cancer and reconstruction surgery. J Clin Anesth. 2018;44:3–4. doi: 10.1016/j.jclinane.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 4.Chin KJ, Malhas L, Perlas A. The Erector Spinae Plane Block Provides Visceral Abdominal Analgesia in Bariatric Surgery: A Report of 3 Cases. Reg Anesth Pain Med. 2017;42:372–6. doi: 10.1097/AAP.0000000000000581. [DOI] [PubMed] [Google Scholar]
- 5.Tulgar S, Senturk O. Ultrasound guided Erector Spinae Plane block at L-4 transverse process level provides effective postoperative analgesia for total hip arthroplasty. J Clin Anesth. 2018;44:68. doi: 10.1016/j.jclinane.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 6.Tulgar S, Selvi O, Senturk O, Ermis MN, Cubuk R, Ozer Z. Clinical experiences of ultrasound-guided lumbar erector spinae plane block for hip joint and proximal femur surgeries. J Clin Anesth. 2018;47:5–6. doi: 10.1016/j.jclinane.2018.02.014. [DOI] [PubMed] [Google Scholar]
- 7.Morrison RS, Magaziner J, Gilbert M, et al. Relationship between pain and opioid analgesics on the development of delirium following hip fracture. J Gerontol A Biol Sci Med Sci. 2003;58:76–81. doi: 10.1093/gerona/58.1.M76. [DOI] [PubMed] [Google Scholar]
- 8.Ke X, Li J, Liu Y, Wu X, Mei W. Surgical anesthesia with a combination of T12 paravertebral block and lumbar plexus, sacral plexus block for hip replacement in ankylosing spondylitis: CARE-compliant 4 case reports. BMC Anesthesiol. 2017;17:86. doi: 10.1186/s12871-017-0358-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Amiri HR, Zamani MM, Safari S. Lumbar plexus block for management of hip surgeries. Anesth Pain Med. 2014;4:e19407. doi: 10.5812/aapm.19407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morimoto M, Kim JT, Popovic J, Jain S, Bekker A. Ultrasound-guided lumbar plexus block for open reduction and internal fixation of hip fracture. Pain Pract. 2006;6:124–6. doi: 10.1111/j.1533-2500.2006.00074.x. [DOI] [PubMed] [Google Scholar]
- 11.Stuart-Smith K. Hemiarthroplasty performed under transversus abdominis plane block in a patient with severe cardiorespiratory disease. Anaesthesia. 2013;68:417–20. doi: 10.1111/anae.12108. [DOI] [PubMed] [Google Scholar]
- 12.Panula J, Pihlajamaki H, Mattila VM, et al. Mortality and cause of death in hip fracture patients aged 65 or older: a population-based study. BMC Musculoskelet Disord. 2011;12:105. doi: 10.1186/1471-2474-12-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ju DG, Rajaee SS, Mirocha J, Lin CA, Moon CN. Nationwide Analysis of Femoral Neck Fractures in Elderly Patients: A Receding Tide. J Bone Joint Surg Am. 2017 Nov 15;99:1932–40. doi: 10.2106/JBJS.16.01247. [DOI] [PubMed] [Google Scholar]
- 14.Birnbaum K, Prescher A, Hessler S, Heller KD. The sensory innervation of the hip joint--an anatomical study. Surg Radiol Anat. 1997;19:371–5. doi: 10.1007/s00276-997-0371-5. [DOI] [PubMed] [Google Scholar]
- 15.Nielsen TD, Moriggl B, Barckman J, et al. Cutaneous anaesthesia of hip surgery incisions with iliohypogastric and subcostal nerve blockade: A randomised trial. Acta Anaesthesiol Scand. 2019;63:101–10. doi: 10.1111/aas.13221. [DOI] [PubMed] [Google Scholar]
- 16.Halaszynski T, Uskova A. Regional Anesthesia for Hip Surgery. In: Scuderi GR, Tria AJ, editors. Minimally Invasive Surgery in Orthopedics. Cham: Springer International Publishing; 2016. pp. 1–7. [DOI] [Google Scholar]
- 17.Aksoy M, Dostbil A, Ince I, et al. Continuous spinal anaesthesia versus ultrasound-guided combined psoas compartment-sciatic nerve block for hip replacement surgery in elderly high-risk patients: a prospective randomised study. BMC Anesthesiol. 2014;14:99. doi: 10.1186/1471-2253-14-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gurkan Y, Aksu C, Kus A, Toker K, Solak M. One operator’s experience of ultrasound guided lumbar plexus block for paediatric hip surgery. J Clin Monit Comput. 2017;31:331–6. doi: 10.1007/s10877-016-9869-x. [DOI] [PubMed] [Google Scholar]
- 19.Karaca S. Is lumbar plexus block sufficient for hip fracture surgery? Pain Pract. 2008;8:147. doi: 10.1111/j.1533-2500.2008.00181_1.x. author reply 147–8. [DOI] [PubMed] [Google Scholar]
- 20.Sarkar Mitra T, Mukherjee A, Agarwal G, Rupert E. Lumbar plexus block: Safe anesthesia for hip surgery. Anesth Essays Res. 2012;6:241–3. doi: 10.4103/0259-1162.108356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xu ZH, Tang S, Luo AL, Huang YG. [Application of lumber plexus blockade for hip fracture repair in elderly patients]. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2010;32:328–31. doi: 10.3881/j.issn.1000-503X.2010.03.019. [DOI] [PubMed] [Google Scholar]
- 22.Zanette G, Robb N, Micaglio M, Manani G, Facco E. Cardiac arrest during continuous psoas compartment block for hip surgery. Anaesth Intensive Care. 2007;35:143–4. [PubMed] [Google Scholar]
- 23.Joubert F, Gillois P, Bouaziz H, Marret E, Iohom G, Albaladejo P. Bleeding complications following peripheral regional anaesthesia in patients treated with anticoagulants or antiplatelet agents: A systematic review. Anaesth Crit Care Pain Med. 2019;38:507–16. doi: 10.1016/j.accpm.2018.12.009. [DOI] [PubMed] [Google Scholar]
- 24.Njathi CW, Johnson RL, Laughlin RS, Schroeder DR, Jacob AK, Kopp SL. Complications After Continuous Posterior Lumbar Plexus Blockade for Total Hip Arthroplasty: A Retrospective Cohort Study. Reg Anesth Pain Med. 2017;42:446–50. doi: 10.1097/AAP.0000000000000589. [DOI] [PubMed] [Google Scholar]
- 25.Tulgar S, Ermis MN, Ozer Z. Combination of lumbar erector spinae plane block and transmuscular quadratus lumborum block for surgical anaesthesia in hemiarthroplasty for femoral neck fracture. Indian J Anaesth. 2018;62:802–5. doi: 10.4103/ija.IJA_230_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ahiskalioglu A, Yayik AM, Alici HA, Ezirmik N. Ultrasound guided transmuscular quadratus lumborum block for congenital hip dislocation surgery: Report of two pediatric cases. J Clin Anesth. 2018;49:15–6. doi: 10.1016/j.jclinane.2018.05.018. [DOI] [PubMed] [Google Scholar]
- 27.Yayik AM, Cesur S, Ozturk F, Ahiskalioglu A, Celik EC. [Continuous quadratus lumborum type 3 block provides effective postoperative analgesia for hip surgery: case report]. Rev Bras Anestesiol. 2019;69:208–10. doi: 10.1016/j.bjan.2018.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]