Abstract
Colombia is experiencing an epidemiologic transition, with an increasing incidence of cancerous neoplasms prevalent in high-income countries, while infection-associated tumors remain highly prevalent. According to international standards, Colombia has a deficit of radiotherapy machines (a shortage of about 47 machines) and radiation oncology specialists (a shortage of about 19 to 149 specialists based on number of centers and incident cases, respectively) to meet the national demand, which may induce an inappropriate dynamic in radiation oncology services. Estimates based on cancer incidence trends and the rate of new specialists in radiation oncology expected to graduate per year suggest that the current deficit will remain unchanged or may even increase during the next decades. The situation is critical because of the existence of a single training program in the country for a population of 45 million inhabitants and the low availability of educational programs offered in the Latin American region to cover the national demand. A comprehensive analysis of radiotherapy services should include data on medical physicists, radiotherapists, and the oncology nursing workforce; however, we found no reliable information available. A better balance between the educational programs offered and the demand for radiotherapy is highly valuable.
CONTEXT
Key Objective
To determine the shortage of radiation oncology workforce according with the current and future demand in Colombia.
Knowledge Generated
Colombia, a high middle-income country, has increased access to oncology care and radiotherapy; however, the radiation oncology workforce does not meet the growing demand, thus inducing a relevant shortage (deficit between 19 and 149 radiation oncologists based on the number of centers and incident cases, respectively).
Relevance
The number of new radiation oncologists per year suggests no reduction of the shortage in the next 20 years. Better planning of the educational offer is highly desirable.
INTRODUCTION
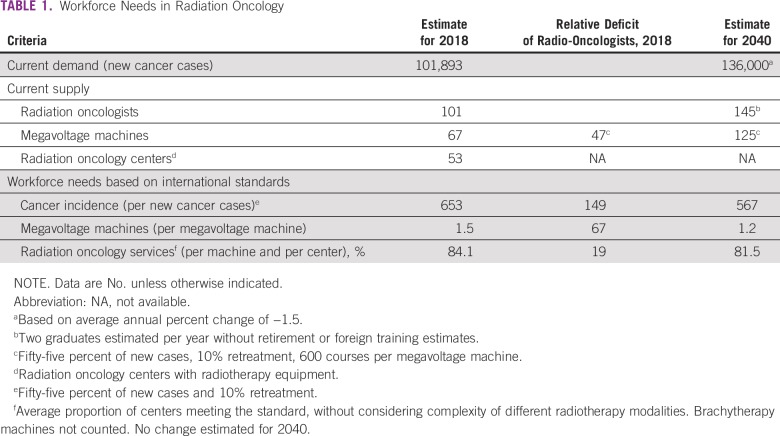
Cancer is the second highest cause of death in Colombia, after cardiovascular disease.1 Accordingly, cancer incidence rates have decreased from 213.7 and 212.9 per 100,000 from 1995 to 1999, respectively, and to 151.5 and 145.6 per 100,000 from 2007 to 2011 for men and women, respectively.2 Similarly, mortality rates have decreased from 96.7 and 83.7 per 100,000 in 1995 to 84.8 and 68.3 in 2013 for men and women, respectively.3 Despite the declining incidence, the aging population will result in an increase in the absolute number of new cases, from 101,893 in 2018 (not including nonmelanoma skin cancer) to about 136,000 new cases per year in 2040 (average annual percentage change, 1.5).4
There are several analyses of radiotherapy supply and demand in the international arena, usually divided according to developed and developing countries. The most common approaches to assessing the needs of the radiation oncology workforce include estimations by number of inhabitants, new cases of cancer and radiation oncology services or radiotherapy equipment.
The estimation per inhabitant was the most common approach for several years. Accordingly, some analyses revealed a huge gap in radiotherapy supply between high-income countries and low- and middle-income countries (LMICs), with 1 radiotherapy machine per 120,000 inhabitants for the former and one radiotherapy machine per five million inhabitants for the latter.5 However, assessing needs per inhabitant does not take into account epidemiology profiles, a variable that may have a significant impact on the final estimates. Cancer incidence is lower in LMICs, and the most frequent types of cancer in these scenarios are those associated with infection (such as cervix and stomach cancers), which may have different radiotherapy needs than the most frequent types of cancer observed in high-income countries. Indeed, cancer incidence and mortality reduction in Colombia is mainly due to risk factor control, which generates an epidemiologic transition, with a decreasing incidence of infection and tobacco-associated cancers, but an increase in tumors such as prostate, breast, colon, and pediatric cancers.6
A review of global access to radiation oncology services based on cancer incidence found variable capacity to treat the disease, ranging from 32% of patients in Mongolia to 59% of patients in Comoro Islands,7 with a relative deficit of megavoltage equipment from 781 machines in low-income countries to 2,567 machines in high- and middle-income countries. Therefore, from this perspective, the International Atomic Energy Agency (IAEA) estimates that Latin America has a deficit of about 350 megavoltage machines in the higher-income countries, whereas countries with the lowest income in the region would have an appropriate equipment supply,5 thus indicating an overall 88% coverage of radiotherapy equipment needs.8 Additionally, despite no estimates on radiation oncology workforce having been provided, we may assume a deficit of similar, or even greater, magnitude, considering that equipment and workforce do not have a linear relationship, particularly with the development of new technologies. In this article, we review the situation of the radiation oncology workforce in Colombia based on the available information from accredited sources using international standards for the analysis.
SUPPLY AND DEMAND OF RADIATION ONCOLOGY
Currently, there are 101 radiation oncologists affiliated with the Colombian Association of Radiation Oncology (ACRO) who report being based in Colombia.9 The National Registry of Health Service Providers (REPS) reported 53 radiation oncology services in the country for the year 2017, the IAEA Directory of Radiotherapy Centres (DIRAC) reports 67 megavoltage machines,10 and the Colombian Geological Service reports 28 authorized facilities to provide brachytherapy.9,11
In 2005, a study on supply and demand of oncology services by the Colombian National Cancer Institute (INC) reported 14 megavoltage, 26 cobalt, 13 x-ray, and 25 brachytherapy machines to deliver radiotherapy in Colombia.12 The data suggest a significant change in radiation oncology supply, with almost a total replacement of cobalt and x-ray machines by linear accelerators and a reduction in brachytherapy supply. Although the absolute number of machines does not suggest an increase in the installed capacity, technology renewal with megavoltage machines (from 14 in 2005 to 67 in 2019) led to a significant increase in radiation oncology supply in the country. Because technology renewal has already taken place, an increase in the total number of megavoltage machines is expected in the near future, with the consequent need for specialists in radiation oncology.
Furthermore, the epidemiologic transition in the country shows a growing demand for infrastructure and workforce for cancer care, with a relevant role for radiation oncology. According to the IAEA, considering the epidemiologic profile of LMICs, an optimal radiotherapy treatment rate with megavoltage machines corresponds to 55% of new cases of cancer, with a 10% retreatment rate.5 A megavoltage machine should provide 600 courses of treatment per year; thus, according to this standard, with the incidence for 2018, Colombia would require 110 megavoltage machines, and considering the epidemiologic transition toward an incidence equivalent to a high-income country, about 125 machines would be required by 2040 (Table 1).
TABLE 1.
Workforce Needs in Radiation Oncology
In turn, the radiation oncology workforce should respond at a rate of not less than one specialist for every 250 new cases of cancer.13 Based on estimates for 2018, about 66,000 cases of cancer would require radiotherapy annually, with a requirement of about 265 specialists in radiation oncology, thereby indicating a deficit of about 149 radiation oncologists at present (Table 1). In addition, for 2040, the demand would amount to 300 radiation oncologists. The reported standard is an average from 12 countries reporting guidelines on staffing of radiation oncology services, with a range of 200 to 350 new cases per specialist14; hence, a higher rate could be assumed for Colombia, considering that in most reporting countries, radiation oncologists also prescribe chemotherapy.15 If we use the maximum rate, the requirement would be 189 specialists, and the current deficit would be 88.
The assessment of workforce needs based on radiotherapy equipment does not have a clear standard. Although supply guidelines are variable among European countries, they agree to have no less than one radiation oncologist per machine, plus one additional per radiation oncology service and another additional radiation oncologist if different complex radiotherapy modalities are provided.15 Therefore, based on this standard and the number of megavoltage machines and radiation oncology services with radiotherapy equipment (without considering brachytherapy), Colombia would need at least 118 specialists in radiation oncology. However, this figure underestimates the demand because most radiation oncology centers in the country perform different complex radiotherapy modalities.
Moreover, according to the REPS, in 2016, 51 health centers had radiotherapy equipment (enabled as therapeutic support), and 46 health centers had outpatient consultation in radiation oncology; these data may indicate that some radiation oncology services do not have a permanent presence of specialists in radiation oncology.16 Additionally, 11 of 35 districts lack radiation oncology services, and despite the general distribution being concordant with the number of new patients, the rate of radiation oncology services by number of cases varies from one service per 274 cases in Atlantico to one per 1,119 cases in Tolima.17
For some European countries, the ideal standard is having at least 2.5 specialists per machine.15 Thus, using this standard, Colombia would need 168 specialists in radiation oncology to properly cover the existing number of megavoltage machines (without brachytherapy) and 275 specialists considering the deficit of radiotherapy equipment previously described, which is a number close to workforce needs estimates based on cancer incidence in the country.
Regarding the job market, data from the National Observatory of Employment for Education are inconsistent with significant annual variations in both income levels and number of radiation oncology specialists affiliated with the social security system18; additionally, the information does not agree with data by ACRO or INC. However, based on the cancer incidence and availability of radiation oncology services, we may assume a significant work overload (high number of patients per specialist), which results in lower quality because of reduced time of the specialist in activities such as review of treatment plans, monitoring of the beginning of treatment, review of the positioning images, and clinical follow-up. The Colombian Geologic Service and the Ministry of Health define regulations for quality and safety of radiotherapy services, the former on management of radiation sources and the latter on the use of radiotherapy equipment and service organization.19,20 Furthermore, the Ministry of Health demands compliance with the IAEA TecDoc 115121; however, in all cases, verification of regulatory compliance is restricted to new services and a routine examination every 4 to 5 years. In addition, the verification is in charge of local health authorities, most of them without proper training or skills on the topic.
Unfortunately, data on compliance with quality standards are not available in the country, and given the limited data and variability in international standards, it is not possible to reach a definitive conclusion. Yet, it is clear that the dynamics of radiation oncology services in Colombia is not consistent, and the supply does not correspond to international standards; Colombia bears a significant deficit of radiotherapy machines and radiation oncology specialists to meet the national demand and be congruent with the technologic development of the medical specialty.
Estimates on the shortage of human resources largely differ according to the international standard concerned. Ideally, the country should consider the demand based on the number of new cases; however, availability of human resources without equipment is not valuable, and accordingly, short-term plans might prioritize the supply to ensure minimum quality by radio-oncology service and megavoltage machine (relative deficit, 19 and 67 radiation oncologists, respectively).
SITUATION OF THE EDUCATIONAL PROGRAMS
In the European Union, significant efforts have been made to harmonize the legislation of country members around practice and training of medical specialties, where scientific societies have played a relevant role. With this aim, the European Society for Radiotherapy and Oncology and the European Union of Medical Specialists agreed on minimum standards for specialized training in the area, including a minimum of 5 years of training, which were subsequently ratified by scientific societies from 28 countries.22 Despite the efforts and regulations developed, a recent survey revealed great heterogeneity in the structure, duration, and quality of residency programs in radiation oncology among European countries.23
In the United States, according to the Accreditation Council for Graduate Medical Education, there were 95 accredited programs in radiation oncology in 2019.24 The standard duration of residency programs in the United States is 4 years, with a prerequisite of a 1-year transition in family medicine, internal medicine, surgery, or pediatrics. Apart from residency programs, the American Association of Residents in Radiation Oncology reports a total of 24 universities for 2018 offering special training or fellowship programs in different areas of radiotherapy, including brachytherapy, radiosurgery, proton therapy, and translational research.25
In Latin America, training programs in radiation oncology are active in Costa Rica, Uruguay, Argentina, Brazil, Chile, Cuba, Mexico, and Peru. Residency programs in Latin America last from 3 to 4 years, and a master’s program in advanced radiotherapy was launched in Chile in 2017 (the only program for special training in radiation oncology found in the region), which was offered as an international program in partnership with the IAEA.
Currently, there is only one residency program for training in radiation oncology in Colombia, which is offered by the INC, with a duration of 4 years. The National Information System of Higher Education reports an additional residency program registered to the Ministry of Education; however, it has not been certified and consequently is not active. The situation is in contrast to the United States, where the rate of training programs in radiation oncology is 1 per 3.3 million inhabitants, whereas in Colombia, it is 1 per 45 million inhabitants.
With a maximum of four graduates per year in the single training program existing in Colombia (there were two graduates per year during the last 2 years according to the National Observatory on Employment), it would require almost 20 years to address the current workforce deficit, without considering retirements during that period. Apparently, the available training programs in the region do not solve the situation because they are producing the workforce needed to cover their own demand for cancer treatment; however, it has been suggested (I. Bobadilla, personal communication, April 2019) that there has been a significant increase in affiliations with ACRO during the last decade by specialists coming from abroad.
In conclusion, the state of the art highlights the need to combine surgery, radiotherapy, and systemic treatment to achieve the best possible outcomes for patients with cancer. In this scenario, the IAEA estimates that, in developing countries, about 55% of new cases of cancer may require radiotherapy treatment, either with curative or palliative intention.
Our analysis is restricted to the radiation oncologist workforce; a more comprehensive approach would require information on medical physicists, radiotherapists, and oncology nurses. We did not find reliable information on other human resources for radiation oncology services. A publication from 2014 reports the deficit of medical physicists and radiotherapists in Colombia according to the IAEA DIRAC26; however, we did not find data on human resources in the cited source.10 The Colombian Association of Medical Physics, reported 41 medical physicists registered in 2017,27 suggesting a significant shortage in the country according to IAEA staffing recommendations.28
Colombia is undergoing an epidemiologic transition, with an increasing cancer incidence for neoplasms prevalent in high-income countries, such as breast and prostate cancers, but with infection-associated tumors remaining highly prevalent. To tackle the double burden of disease, proper workforce development is mandatory, in which specialists in radiation oncology play a relevant role.
The situation is critical because of the lack of training programs, thereby generating an inappropriate dynamic in radiation oncology services, which may induce low access and a low quality of care. As indicated, there is only one residency program in radiation oncology in Colombia, and there are two training programs in medical physics and two training programs for radiotherapists. In an open market, as in the Colombian health system, stricter follow-up on compliance with quality standards would be highly desirable; nonetheless, an increased supply in the radiation oncology workforce would be expected to have a positive impact on both the workforce market and professional practice.
AUTHOR CONTRIBUTIONS
Conception and design: Raúl Murillo, Juan Carlos Galvis, Iván Hidalgo, Alejandro Marín, Jorge Emilio Muñoz, Ricardo Sánchez
Collection and assembly of data: All authors
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/site/misc/authors.html.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
No potential conflicts of interest were reported.
REFERENCES
- 1. Ministerio de Salud y Protección Social: Análisis de Situación de Salud (ASIS), Colombia 2016. MinSalud: Dirección de Epidemiología y Demografía. Bogotá; 2016. [Google Scholar]
- 2. Pardo C, Piñeros M, Murillo R: Incidencia estimada y mortalidad por cáncer en Colombia 1995-1999. Bogotá, Colombia, Instituto Nacional de Cancerología, 2005. [Google Scholar]
- 3.International Agency for Research on Cancer–World Health Organization WHO-IARC Cancer Mortality Database. http://www-dep.iarc.fr/WHOdb/WHOdb.htm
- 4.International Agency for Research on Cancer–World Health Organization Global Cancer Observatory. http://gco.iarc.fr/
- 5.Rosenblatt E, Zubizarreta E. Radiotherapy in Cancer Care: Facing the Global Challenge. (eds): Vienna, Austria, International Atomic Energy Agency, 2017. [Google Scholar]
- 6.Piñeros M, Gamboa O, Hernández-Suárez G, et al. Patterns and trends in cancer mortality in Colombia 1984-2008. Cancer Epidemiol. 2013;37:233–239. doi: 10.1016/j.canep.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 7.Yap ML, Zubizarreta E, Bray F, et al. Global access to radiotherapy services: Have we made progress during the past decade? J Glob Oncol. 2016;2:207–215. doi: 10.1200/JGO.2015.001545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zubizarreta E, Van Dyk J, Lievens Y. Analysis of global radiotherapy needs and costs by geographic region and income level. Clin Oncol (R Coll Radiol) 2017;29:84–92. doi: 10.1016/j.clon.2016.11.011. [DOI] [PubMed] [Google Scholar]
- 9.Asociación Colombiana de Radioterapia Oncológica http://www.acro.net.co/miembros%20activos.php : Miembros activos .
- 10. https://dirac.iaea.org/ International Atomic Energy Agency: Directory of Radiotherapy Centres (DIRAC).
- 11.Servicio Geológico Colombiano Instalaciones autorizadas para el empleo de material radiactivo. https://www2.sgc.gov.co/ProgramasDeInvestigacion/AsuntosNucleares/Documents/Xue_v1.0.1_-_Instalaciones_Autorizadas.pdf
- 12.Plazas MC, Ospino R, Mejía A, et al. Evaluación de los Servicios de Radioterapia en Colombia. Bogotá, Colombia, : Instituto Nacional de Cancerología; 2005. [Google Scholar]
- 13.Grover S, Xu MJ, Yeager A, et al. A systematic review of radiotherapy capacity in low- and middle-income countries. Front Oncol. 2015;4:380. doi: 10.3389/fonc.2014.00380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Slotman BJ, Cottier B, Bentzen SM, et al. Overview of national guidelines for infrastructure and staffing of radiotherapy. ESTRO-QUARTS: Work package 1. Radiother Oncol. 2005;75:349–354. doi: 10.1016/j.radonc.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 15.Dunscombe P, Grau C, Defourny N, et al. Guidelines for equipment and staffing of radiotherapy facilities in the European countries: Final results of the ESTRO-HERO survey. Radiother Oncol. 2014;112:165–177. doi: 10.1016/j.radonc.2014.08.032. [DOI] [PubMed] [Google Scholar]
- 16.Murcia E, Aguilera J, Wiesner C, et al. Oncology services supply in Colombia. Colomb Med (Cali) 2018;49:89–96. doi: 10.25100/cm.v49i1.3620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aguilera-López J, Murcia-Monroy EM. Boletín Servicios Oncológicos en Colombia. Bogotá, Colombia, : Instituto Nacional de Cancerología; 2016. [Google Scholar]
- 18.de Educación M. Observatorio Laboral para la Educación. https://www.mineducacion.gov.co/sistemasinfo/Sistemas-de-Informacion-en-Ed-Superior-especializados/212301:Observatorio-Laboral-para-la-Educacion
- 19.Servicio Geológico Colombiano Autorización para la ejecución de todas las prácticas y actividades asociadas al empleo de fuentes radiactivas. https://www2.sgc.gov.co/ProgramasDeInvestigacion/AsuntosNucleares/Paginas/Autorizacion-ejecucion-practicas.aspx
- 20.Ministerio de Salud y Protección Social Regulación de uso de equipos generadores de radiación ionizante y prestación de servicios de protección radiológica y control de calidad. https://www.minsalud.gov.co/salud/MT/Paginas/radiaciones-ionizantes.aspx
- 21. Oganismo Internacional de Energía Atómica: Aspectos físicos de la garantía de calidad en radioterapia: Protocolo de control de calidad. IAEA-TECDOC-1151. Vienna, Austria, OIEA, 2000. [Google Scholar]
- 22. Union Européenne des Médecins Spécialistes: Training requirements for the specialty of radiation oncology. European standards of postgraduate medical specialist training. UEMS 2013/20. https://www.uems.eu/media-and-library/documents/adopted-documents/2023.
- 23.Bibault JE, Franco P, Borst GR, et al. Learning radiation oncology in Europe: Results of the ESTRO multidisciplinary survey. Clin Transl Radiat Oncol. 2018;9:61–67. doi: 10.1016/j.ctro.2018.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Accreditation Council for Graduate Medical Education: Accreditation Data System (ADS). ADS Public. https://apps.acgme.org/ads/public/
- 25.Association of Residents in Radiation Oncology (ARRO) Resident resources: Certification resources. https://www.astro.org/Affiliate/ARRO/Resident-Resources
- 26.Datta NR, Samiei M, Bodis S. Radiation therapy infrastructure and human resources in low- and middle-income countries: Present status and projections for 2020. Int J Radiat Oncol Biol Phys. 2014;89:448–457. doi: 10.1016/j.ijrobp.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 27.Asociación Colombiana de Física Médica y Protección Radiológica https://www.acofimpro.com/CONTENIDO/QUIENES%20SOMOS/INTEGRANTES.html Integrantes.
- 28. International Atomic Energy Agency: Staffing in radiotherapy: An activity based approach. IAEA Human Health Reports No. 13. Vienna, Austria, IAEA, 2015. [Google Scholar]