Abstract
SUMMARY: A retrospective study was conducted on a cohort of 15 patients who underwent surgery because cholesteatoma or abscess was suspected. All patients had MR imaging prior to surgery with diffusion-weighted images (DWI) from which the apparent diffusion coefficient (ADC) value was calculated. Using this technique, we were able to determine 3 distinct ADC value ranges corresponding to the 3 groups of lesions found at surgery (pure cholesteatoma, cholesteatoma with infection, and abscess or infection). This needs to be confirmed by further studies with a wider range of patients.
Cholesteatoma is a locally aggressive middle ear lesion consisting of squamous cells with desquamatous debris that requires surgical treatment. Some may be superinfected. These processes may be difficult to distinguish from pure abscess on conventional imaging.
Currently, the most effective method for imaging cholesteatoma is CT, with MR imaging reserved for difficult cases such as the detection of recurrence. The MR examination should include T1-weighted, T1 postgadolinium contrast, T2-weighted, and diffusion-weighted/apparent diffusion coefficient (ADC) sequences. Cholesteatoma typically shows intermediate T1 signal intensity without significant enhancement after 30 to 45 minutes and hyperintense signal intensity on T2-weighted and diffusion-weighted (DW) images.1–5
Cholesteatoma shows increased DW signal intensity for the same reason as a brain epidermoid cyst, another lesion containing epidermoid cells, as previously reported in the literature.5 Although restricted diffusion does contribute to increased DW signal intensity, the increased signal intensity predominantly results from the effects of T2 shinethrough.6–9 Annet et al7 found that the mean ADC value was approximately 1.070 × 10−3 mm2/s (range, 1.280–0.807 × 10−3 mm2/s).7
A brain abscess also shows increased DW signal intensity; however, this is primarily caused by restricted diffusion from the increased viscosity of the fluid inside.10–11 Chang et al11 demonstrated that the mean ADC value in an abscess was 0.650 × 10−6 mm2/s.
From these differences, it can be inferred that the ADC value could be used to help differentiate epidermoid lesions from abscess. The aim of our study was to evaluate whether ADC values could be measured to show a pattern that could differentiate cholesteatoma from abscess and cholesteatoma with infection.
Materials and Methods
Patients
We conducted a retrospective cohort study on 15 patients (7 male and 8 female; age range, 6–72 years; mean, 36.7 years), who underwent MR imaging showing findings of either cholesteatoma or abscess before surgery from January 2007 to August 2008.
We divided this cohort into 3 different groups corresponding to the surgical findings: the first group had pure cholesteatoma, the second had a mixed-pattern lesion of cholesteatoma associated with infection, and a third group showed abscess and infection.
For each surgical group, we retrospectively measured the ADC value as found on the MR imaging study performed before surgery (Table 1).
Table 1:
ADC values for the 3 different surgical groups
| Patient No. | ADC Value (×10−3 mm2/s) |
||
|---|---|---|---|
| Group 1 | Group 2 | Group 3 | |
| 1 | 0.847 | 0.628 | 0.571 |
| 2 | 1.054 | 0.774 | 0.568 |
| 3 | 1.046 | 0.630 | 0.107 |
| 4 | 0.917 | ||
| 5 | 1.047 | ||
| 6 | 0.790 | ||
| 7 | 0.871 | ||
| 8 | 0.698 | ||
| 9 | 0.863 | ||
Note:—ADC indicates apparent diffusion coefficient.
Imaging Technique
We performed the MR imaging study on a 1.5T MR unit (1.5T Avanto; Siemens, Erlangen, Germany). All patients were evaluated with the following protocol:
T1 axial spin-echo fat saturated (17 slides; matrix, 384 × 384; voxel size, 0.6 × 0.6 × 1.5 mm; TR, 719 ms; TE, 13 ms; 2 averages).
T2 axial spin-echo (25 slides; matrix, 256 × 256; voxel size, 0.9 × 0.9 × 4 mm; TR, 4490 ms; TE, 100 ms; 1 average).
High-resolution T2 axial (gradient-echo, 64 slides; matrix, 320 × 384; voxel size, 0.5 × 0.5 × 0.4 mm; TR, 11.6 ms; TE, 5.8 ms).
DW acquisition axial and coronal (20 slides; TR, 4000 ms; TE, 107 ms; matrix, 128 × 128; voxel size, 1.5 × 1.5 × 3 mm; b = 0 and b = 1000s/mm2; 5 averages). ADC cartography was systematically done with use of these acquisition parameters.
Half-Fourier acquired single-shot turbo spin-echo diffusion-weighted acquisition axial and coronal (15 slides; TR, 2000 ms; TE, 132 ms; matrix, 128 × 64; voxel size, 2.5 × 1.2 × 3 mm; b = 1000 s/mm2; 5 averages).
T1 axial spin-echo fat saturated, 45 minutes after gadolinium chelate injection (17 slides; matrix, 384 × 384; voxel size, 0.6 × 0.6 × 1.5 mm; TR, 719 ms; TE, 13 ms; 2 averages).
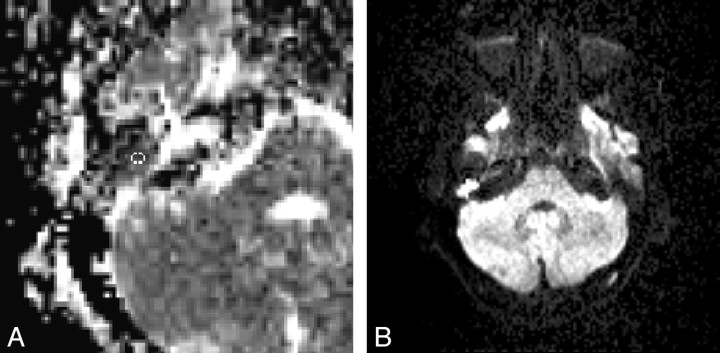
All examinations were reviewed by a radiologist who had 15 years’ experience in middle ear imaging. For each patient, this radiologist calculated the ADC value in a selected region of interest on the cartography on the Avanto workstation (Siemens) (Fig 1). These regions of interest were placed in an area matching the suspected cholesteatoma or abscess of the middle ear according to the usual sequences and were approximately 11 mm2 in volume.
Fig 1.
A, ADC value cartography and region of interest to calculate ADC value. B, DW image.
To test the reliability of the measurements, all were repeated twice (2 months apart) by the same radiologist experienced in otolaryngologic imaging. The second measurement was taken without checking the first results. The results are listed in Table 2. These results were subjected to the correlation test as detailed in Portney and Watkins.12
Table 2:
ADC values calculated twice to test the reliability of the measurements
| Patient No./Surgical Group | ADC Value (×10−3 mm2/s) First Calculation | ADC Value (×10−3 mm2/s) Second Calculation |
|---|---|---|
| 1/g1 | 0.847 | 0.866 |
| 2/g1 | 1.054 | 1.015 |
| 3/g1 | 1.046 | 1.026 |
| 4/g1 | 0.917 | 0.805 |
| 5/g1 | 1.047 | 1.054 |
| 6/g1 | 0.790 | 0.857 |
| 7/g1 | 0.871 | 0.832 |
| 8/g1 | 0.698 | 0.696 |
| 9/g1 | 0.863 | 0.824 |
| 1/g2 | 0.628 | 0.668 |
| 2/g2 | 0.774 | 0.670 |
| 3/g2 | 0.630 | 0.621 |
| 1/g3 | 0.571 | 0.531 |
| 2/g3 | 0.568 | 0.576 |
| 3/g3 | 0.107 | 0.075 |
Note:—g1 indicates group 1; g2, group 2; g3, group 3.
The size of each middle ear signal intensity abnormality was evaluated and an average for the cohort calculated. Finally, we retrospectively compared the diagnosis made by DWI only with the diagnosis inferred by using DWI and ADC values compared with the surgical results (Table 3).
Table 3:
Diagnosis made by DWI alone vs DWI and calculated ADC values
| Patient No./Surgical Group | Diagnosis Made by DWI Alone | Diagnosis Inferred by DWI with Calculated ADC Values |
|---|---|---|
| 1/g1 | G1 | G1 |
| 2/g1 | G1 | G1 |
| 3/g1 | G1 | G1 |
| 4/g1 | G1 | G1 |
| 5/g1 | G1 | G1 |
| 6/g1 | G1 | G1 or 2 |
| 7/g1 | G1 | G1 |
| 8/g1 | G1 | G2 |
| 9/g1 | G1 | G1 |
| 1/g2 | G1 | G2 |
| 2/g2 | G1 | G1 or 2 |
| 3/g2 | G1 or 2 | G2 |
| 1/g3 | G2 | G3 |
| 2/g3 | G1 or 2 | G3 |
| 3/g3 | G3 | G3 |
Note:—DWI indicates diffusion-weighted imaging; G1, diagnosed as a group 1 patient; G2, diagnosed as a group 2 patient; G3, diagnosed as a group 3 patient.
Results
The surgical results of the 15 patients included in the study showed that 9 had pure cholesteatoma (group 1), 3 had cholesteatoma with superinfection (group 2), and 3 had abscess or pure infection with no evidence of cholesteatoma (group 3). The calculated ADC values of these 3 groups are listed in Table 1.
In summary, the group 1 patients had an ADC value up to 0.698 × 10−3 mm2/s, the group 2 patients showed a lower ADC value (0.628 and 0.774 × 10−3 mm2/s), and the group 3 patients, containing abscess or pure infection without cholesteatoma, showed a ADC value under 0.571 × 10−3 mm2/s (taking into account the first measurement).
The range of signal intensity abnormality on which we performed the measurements was from 16 mm2 to 266 mm2. The calculated average is approximately 84 mm2.
All of the values were calculated twice and are listed in Table 2. We calculated the interclass correlation coefficient (ICC) using the method detailed in Portney and Watkins.12 The calculated ICC is 0.98, substantiating the reliability of the measurements. Table 3 shows 4 misdiagnoses with use of the DWI alone, whereas 1 diagnosis for the DWI combined with the ADC values (the latest were made retrospectively).
Discussion
To date, no study has attempted to use ADC values to differentiate cholesteatoma from abscess or mixed-pattern lesions. Considering the findings reported in the literature, we expected a high ADC value for the pure cholesteatoma with a mean ADC value of approximately 1 × 10−3 mm2/s. The cohort of 9 patients with surgically proved pure cholesteatoma had a mean ADC value of 0.903 × 10−3 mm2/s (calculated with the ADC values from Table 1). This result is consistent with what was expected.
Previous articles evaluating brain abscess ADC values showed relatively low values, including the article by Chang et al11 that found an average of approximately 0.650 × 10−3 mm2/s (calculated with the ADC values from Table 1). In our cohort of 3 patients, we obtained a mean ADC value of 0.415 × 10−3 mm2/s, which is somewhat lower than what was expected.
As expected, the mixed-pattern lesions showed intermediate ADC values, likely the result of the combination of both tissue ADC ranges. Our results showed a mean ADC value of 0.677 × 10−3 mm2/s (calculated with the ADC values from Table 1), that is, between 0.415 and 0.903 × 10−3 mm/s.
The concordance between the surgical findings and the calculated ADC value suggests that ADC values could be used to allow greater specificity to differentiate cholesteatoma from middle ear abscess or mixed-pattern lesions. Indeed, the comparison between the 2 methods (DWI alone vs DWI and calculated ADC values) shows that calculating the ADC value can improve the precision of the diagnosis (1 mistake with use of this method vs 4 mistakes otherwise).
In our study, the mean size of the middle ear abnormalities in DW images was 84 mm2 (range, 16–266 mm2). Compared with the study reported by De Foer et al,13 the lesion values are substantially higher, resulting mainly from the measurement technique. Indeed, as shown in Fig 1, the region of interest is placed on the center of the lesion. With a very small lesion, it is much more difficult, even impossible, to draw the region of interest without taking in the surrounding tissue, which would lead to false results. This is a limitation in the technique reported herein. To illustrate this, we show an example of a measurement for each group (Figs 2–4).
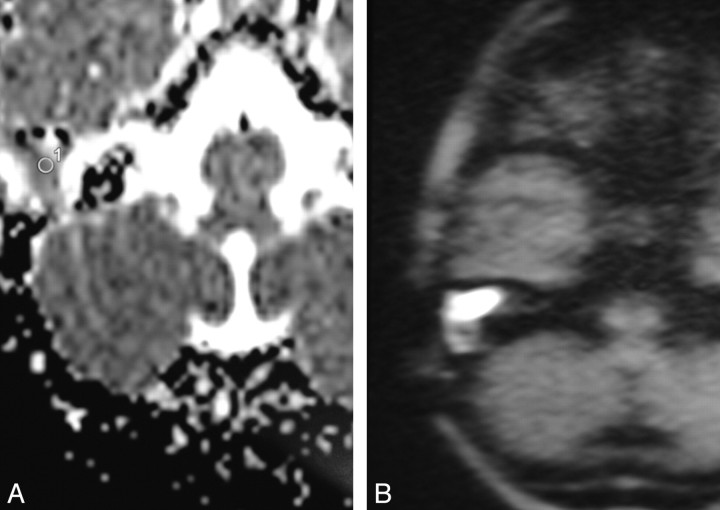
Fig 2.
A, corresponding calculated ADC value on ADC cartography (0.917 × 10−3 mm2/s). B, DW image of a group 1 patient.
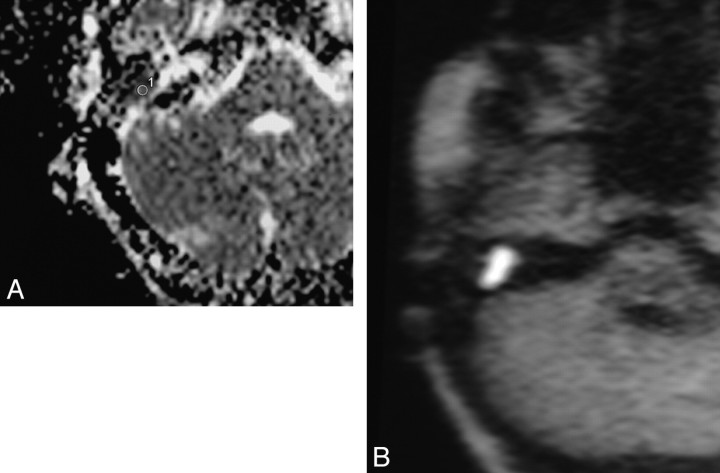
Fig 3.
A, corresponding calculated ADC value on ADC cartography (0.774 × 10−3 mm2/s). B, DW image of a group 2 patient.
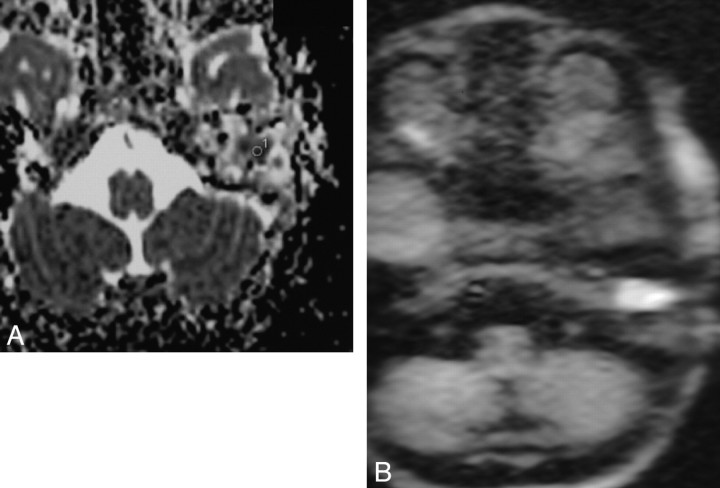
Fig 4.
A, corresponding calculated ADC value on ADC cartography (0.570 × 10−3 mm2/s). B, DW image of a group 3 patient.
Given the small sample size in this study, a larger study with a wider range of patients is recommended to confirm the results before drawing a definitive conclusion on the importance of ADC values to differentiate middle ear pathologic conditions.
Conclusions
In MR imaging of the middle ear, there is typically no reliable way to differentiate between abscess and cholesteatoma. Calculating the ADC value of a region of interest placed on the lesion, we were able to determine 3 distinct ADC value ranges corresponding to the 3 groups of lesions found at surgery (pure cholesteatoma, cholesteatoma with infection, and abscess or infection). One limitation seemed to be the size of the lesion because it is likely that the measurement cannot be adequately taken on very small lesions. These results need to be confirmed by additional studies with a larger sample size and a wider range of patients.
References
- 1.Kimitsuki T, Suda Y, Kawano H, et al. Correlation between MRI findings and second-look operation in cholesteatoma surgery. ORL J Otorhinolaryngol Relat Spec 2001;63:291–93 [DOI] [PubMed] [Google Scholar]
- 2.Heran F, Williams M. MRI of the ear. J Neuroradiol 2003;30:131–45 [PubMed] [Google Scholar]
- 3.Kosling S, Bootz F. CT and MR imaging after middle ear surgery. Eur J Radiol 2001;40:113–18 [DOI] [PubMed] [Google Scholar]
- 4.Vanden Abeele D, Coen E, Parizel PM, et al. Can MRI replace a second look operation in cholesteatoma surgery? Acta Otolaryngol 1999;119:555–61 [DOI] [PubMed] [Google Scholar]
- 5.Dubrulle F, Souillard R, Chechin D, et al. Diffusion-weighted MR imaging sequence in the detection of postoperative recurrent cholesteatoma. Radiology 2006;238:604–10 [DOI] [PubMed] [Google Scholar]
- 6.Schaefer PW, Grant PE, Gonzalez RG. Diffusion-weighted MR imaging of the brain. Radiology 2000;217:331–45 [DOI] [PubMed] [Google Scholar]
- 7.Annet L, Duprez T, Grandin C, et al. Apparent diffusion coefficient measurements within intracranial epidermoid cysts in six patients. Neuroradiology 2002;44:326–28 [DOI] [PubMed] [Google Scholar]
- 8.Hakyemez B, Aksoy U, Yildiz H, et al. Intracranial epidermoid cysts: diffusion-weighted, FLAIR and conventional MR findings. Eur J Radiol 2005;54:214–20 [DOI] [PubMed] [Google Scholar]
- 9.Chen S, Ikawa F, Kurisu K, et al. Quantitative MR evaluation of intracranial epidermoid tumors by fast fluid-attenuated inversion recovery imaging and echo-planar diffusion-weighted imaging. AJNR Am J Neuroradiol 2001;22:1089–96 [PMC free article] [PubMed] [Google Scholar]
- 10.Leuthardt EC, Wippold FJ, Oswood MC, et al. Diffusion weighted MR imaging in the preoperative assessment of brain abscesses. Surg Neurol 2002;58:395–402 [DOI] [PubMed] [Google Scholar]
- 11.Chang SC, Lai PH, Chen WL, et al. Diffusion-weighted MRI features of brain abscess and cystic or necrotic brain tumors: comparison with conventional MRI. Clin Imaging 2002;26:227–36 [DOI] [PubMed] [Google Scholar]
- 12.Portney LG, Watkins MP. Foundation of Clinical Research. Applications and Practice. Norwalk, Conn: Appleton and Lange;1993. :509–16
- 13.De Foer B, Vercruysse JP, Bernaerts A, et al. The value of single-shot turbo spin-echo diffusion-weighted MR imaging in the detection of middle ear cholesteatoma. Neuroradiology 2007;49:841–48 [DOI] [PubMed] [Google Scholar]