Abstract
BACKGROUND AND PURPOSE: Vertebroplasty is commonly used for osteoporotic and neoplastic compression fractures, yet little evidence exists for its use in traumatic nonosteoporotic compression fractures. The purpose of this study was to evaluate the safety and efficacy of percutaneous vertebroplasty for patients with traumatic nonosteoporotic compression fractures.
MATERIALS AND METHODS: We performed a retrospective review of 819 patients (982 procedures) who underwent percutaneous vertebroplasty, to identify patients who had normal bone mineral densitometry scores or had no previous diagnosis of osteoporosis, multiple myeloma, or history of long-term steroid use. Follow-up evaluations included pain at rest and with activity (assessed with the visual analog scale [VAS]), medication use, and mobility. Roland-Morris Disability Questionnaire (RDQ) scores were also collected. Statistical analysis included a 2-tailed t test comparing postprocedure outcomes with baseline values.
RESULTS: Fifteen patients (53% women) were included. Mean age and t-score were 60 years and −0.35, respectively. We found significant improvements in the VAS scores, both at rest and with activity, and in the RDQ scores, starting at the 2-hour follow-up. Additionally, we found marked decreases in medication use and improvements in mobility. The complication rate was low and characterized by asymptomatic extravasation of cement.
CONCLUSIONS: From our study, we have shown that vertebroplasty can be successfully and safely used in patients with traumatic nonosteoporotic compression fractures. Vertebroplasty in these patients should be used after failure of conservative treatments and may be used in place of more invasive spinal reconstruction techniques.
Vertebroplasty has been widely and successfully used in the treatment of osteoporotic and neoplastic vertebral compression fractures. Traditionally, vertebroplasty is used for the treatment of painful primary and secondary osteoporotic compression fractures refractory to medical therapy, pain-inducing fractures caused by invading neoplasms, and in cases of painful osteonecrosis.1 However, the literature regarding the use of vertebroplasty for traumatic, nonosteoporotic, and/or non-neoplastic, compression fractures remains limited, with studies restricted to a small number of patients.2-5
The use of vertebroplasty for patients with traumatic vertebral fractures is complicated by the complexity of the injuries and the multifaceted demographics of the patient population itself.6 Of particular concern is the potential for traumatic vertebral fractures to have more endplate fracturing, leading to increased cement leakage.5 Additionally, the characteristics of the nonosteoporotic bone itself may influence the efficacy of vertebroplasty. Due to the lack of knowledge about this patient population, this study serves to evaluate the use of vertebroplasty for traumatic compression fracture repair through a retrospective study.
Materials and Methods
Patient Population
We performed a retrospective review of 982 procedures on 819 patients in our institution between February 1999 and June 2008. The typical flow of patients in our practice is for patients to be initially evaluated in our Spine Center, staffed by physical medicine and rehabilitation physicians primarily, with input from spine surgeons on an as-needed basis. Patients are then referred to the neuroradiology practice, where a single experienced physician evaluates the patient and plans therapy. Patients who had a traumatic compression fracture and underwent vertebroplasty were further evaluated for inclusion in our study. Some of the patients in our current study had been included in a data base that was used for previous studies of vertebroplasties that were not specific to traumatic injuries7-17 and had not been previously evaluated independently. Institutional review board approval was granted for this study, and all patient information was handled in accordance with Health Insurance Portability and Accountability Act standards. Patients with unstable burst fractures or with fractures extending into the posterior elements were not treated with vertebroplasty.
Selection Criteria
The patients approved for vertebroplasty and inclusion in our study presented after a traumatic event with a resulting vertebral compression fracture, in which the pain was refractory to conservative treatment. A traumatic event was defined as an event that resulted in sudden physical injury, such as an accident or severe fall. We excluded patients who had a history of osteoporosis or multiple myeloma or had a concomitant contributory history of steroid use. To define this population, we separated patients experiencing a traumatic injury on the basis of bone mineral densitometry (BMD) t-scores, using the lowest t-scores for the lumbar spine, total proximal hip, hip trochanter, or hip neck. Lumbar spine measurements were not used for patients in whom only 1 vertebral level was examined. Two vertebral levels are needed for a diagnostic measurement, according to the International Society of Clinical Densitometry (ISCD). The SDs for BMD t-scores set by the ISCD are the following: t-scores of −2.5 or less indicate osteoporosis, t-scores between −1 and −2.5 are considered osteopenic, and t-scores of −1 and higher are considered to represent bone attenuation. Only patients undergoing a traumatic injury who had a normal BMD t-score (−1 or higher) were included in this study. When no BMD t-scores were available, a thorough chart and radiologic review was performed on each patient's medical records. Those patients whose records stated the diagnosis of osteoporosis or multiple myeloma or who had a history of significant steroid use or prior vertebral fractures were excluded from this study.
Procedure Details
Patients with traumatic compression fractures were treated with vertebroplasty when their pain was not relieved with conservative medical management, including bracing, analgesics, and/or physical therapy.18,19 Vertebroplasty was performed with the patient under conscious sedation or general anesthesia and as specified previously.9,20 All vertebroplasty procedures were preformed under the guidance of biplane fluoroscopy, and an 11- or 13- gauge needle was used to traverse the right, left, or both pedicles. The needles were inserted into the anterior one third of the vertebral body closest to the midline as possible, without compromising the medial wall of the pedicle or the anterior cortex of the vertebral body. The needle was then cleared with saline. Patients without osteoporosis, in general, have very hard bone, and placement of the needle into the vertebral body required greater force and effort. Additionally, due to the attenuated nature of the bone in patients without osteoporosis, there is a potential for decreased capacitance to accept cement, compared with patients with osteoporosis. This can potentially result in greater injection pressure and a reduced amount of cement injected into the vertebral body. After needle insertion, polymethylmethacrylate (PMMA) cement, as previously described,20,21 was injected into the vertebral body until the injected cement reached the posterior one fourth of the vertebral body or if epidural, venous, or transendplate extravasation of cement was observed.7-9 Patients were kept supine for 2 hours after the procedure before being discharged.
Outcome Measurements
Patients approved for vertebroplasty were evaluated preoperatively and postoperatively for both quantitative and qualitative measurements. Quantitative measurements were collected by using the Roland-Morris Disability Questionnaire (RDQ)14 and the Visual Analog Scale (VAS) for “pain at rest” and “pain with activity,” with zero being no pain and 10 being the worst pain ever experienced. Qualitative data were also collected for patient mobility and narcotic medication usage. The preoperative and 2-hour postoperative data were collected by trained nurses in the hospital, and follow-up data at 1 week, 1 month, 6 months, and 1 year were collected over the phone by trained nurses.
Statistical Analysis
VAS and RDQ scores were analyzed by using a 2-tailed t test at each follow-up point to evaluate the change in pain and RDQ score from preoperative values. The VAS and RDQ scores were also averaged at each follow-up period to allow further comparison.
Results
Fifteen patients who met our inclusion criteria for this study were selected. The average age of our patients was 60 years of age(range, 32–86 years), and 7/15 were men. Only 1 vertebral level was repaired in each of the 15 patients. Eleven patients sustained a fracture following a fall, 2 patients were in motor vehicle crashes, 1 patient was hit by a golf cart, and 1 patient was injured in a surfing/boogie boarding accident. Four patients had extraspinal injuries, which may have caused increased pain and diminished mobility in addition to their vertebral fracture: Two patients had multiple fractures resulting from motor vehicle crashes, 1 patient had an elbow fracture, and 1 patient had myotonic dystrophy. The levels treated varied, with 4/15 (27%) fractures occurring at L1, and 3/15 (20%), at L2. The remaining fractures occurred at T4 (2/15), T8 (2/15), T10 (1/15), L3 (1/15), and L5 (1/15). Preoperatively, we also collected data on mobility and medication usage. Regarding mobility, 5/15 (33%) patients could walk >1 block, 6/15 (40%) patients had resisted mobility, 1/15 (6%) patients could walk <1 block, and 3/15 (20%) patients were bedridden. For medication usage, 8 (53%) patients were on a regular regimen of narcotics, 5 (33%) were on occasional narcotics, and 1 (6%) patient was on non-narcotic analgesics. Fourteen patients (93%) were evaluated with preoperative spinal MR imaging, and the remaining patient was evaluated with preoperative bone scanning, which demonstrated increased uptake at the site of the fracture. The mean loss of height was 50% (range, 20%–75%). Vertebroplasty was performed on 14/15 patients with conscious sedation and 1/15 with general anesthesia. The average cement volume injected into each vertebra was 2.3 mL There was an average of 4 months (SD = 3.24) between the date of the injury and the performance of vertebroplasty. This was a longer time between fracture and procedure than is generally recommended (ie, usually 6–12 weeks).21
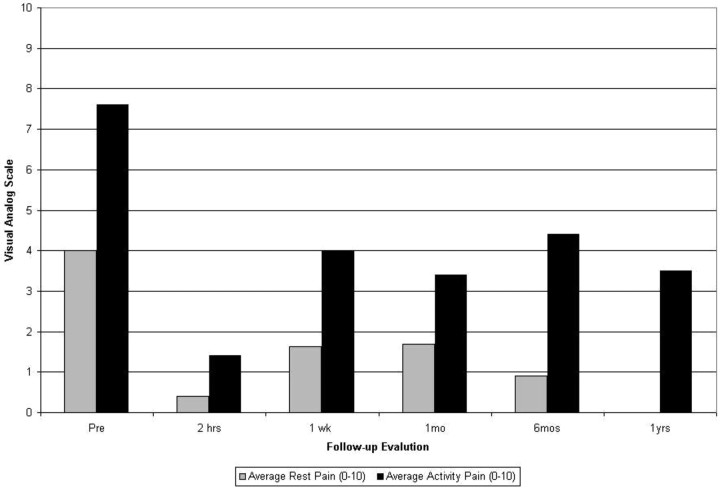
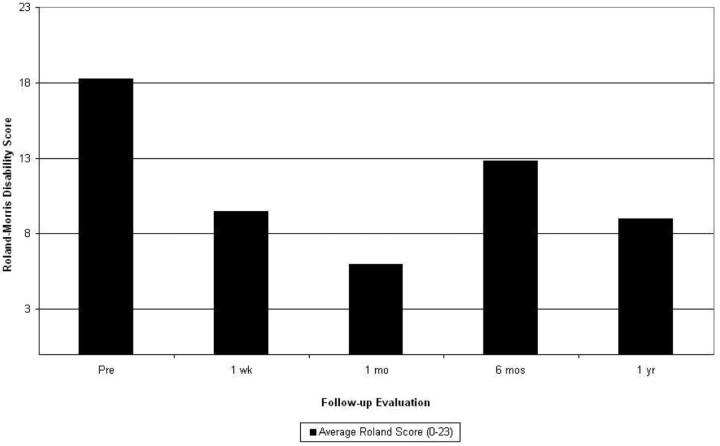
Quantitatively, we measured our patients’ pain at rest and with activity preoperatively; 2 hours postoperatively; and at 1 week, 1 month, 6 months, and 1 year. We found a significant decrease, compared with preoperative values, in “pain at rest” at all follow-up evaluations and at 2 hours (P = .0006), 1 week (P = .0197), 1 month (P = .0282), 6 months (P = .0027), and 1 year (P = .0002). With activity, we found a significant decrease in pain at the 2-hour postoperative follow-up (P = .0136). We also collected and analyzed the RDQ scores at all follow-up periods and found a significant decrease in RDQ scores at the 1-month follow-up (P = .001). Furthermore, throughout the 1-year follow-up period, our patients experienced, on average, a sustained decrease in pain at rest and with activity (Fig 1) and in their RDQ scores (Fig 2), compared with their preoperative scores. VAS and RDQ scores were collected from 33% of patients at 2 hours, 53% of patients at 1 week, 67% of patients at 1 month, 53% of patients at 6 months, and 20% of patients at 1 year. We were unable to collect follow-up data from 4 patients beyond 1 month due to the proximity in time between their procedure and the date of this study. In addition, we found a marked increase in mobility and a decrease in medication usage in our patients during the 1-year follow-up period (Table).
Fig 1.
Graph shows average pain at rest and with activity following vertebroplasty based on the VAS.
Fig 2.
Graph shows average RDQ score following vertebroplasty.
Percentage of patients available for follow-up with improvement in mobility and medication usage following vertebroplasty
| 1 week | 1 month | 6 months | 1 year | |
|---|---|---|---|---|
| Mobility | 90% (9/10) | 100% (7/7) | 71% (5/7) | 100% (3/3) |
| Medication usage | 70% (7/10) | 88% (7/8) | 71% (5/7) | 100% (3/3) |
Case Report
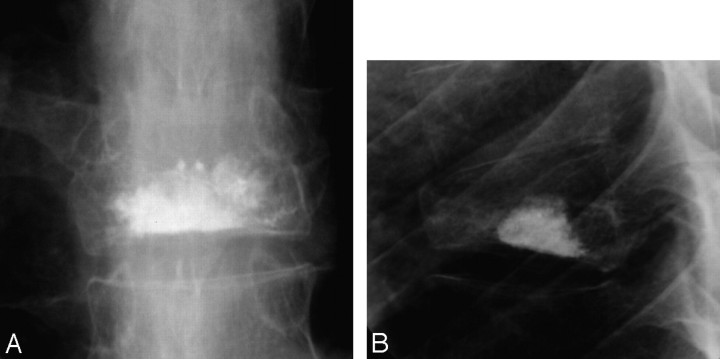
A 32-year-old man presented to our spine center with a traumatic compression fracture sustained while boogie boarding in Mexico. He had >50% anterior compression of T8 and 23° of kyphosis (Fig 3). The patient was originally treated with a Taylor brace and thoracic exercises, but after 9 months of intractable pain, it was determined that more aggressive measures were needed. Before the spine surgeon performed a T8 corpectomy and T7–9 instrumented fusion, the patient was referred to us for evaluation for vertebroplasty. The patient was reluctant to proceed with open surgical intervention. He was found to be an appropriate candidate for vertebroplasty, and it was concluded that vertebroplasty would be a less invasive procedure and should be attempted first before corpectomy and instrumented fusion. Transpedicular trocars were inserted bilaterally, and a total of 3 mL of PMMA cement was injected in the T8 vertebral body. Relatively high pressure needed to be exerted to inject the cement into the vertebra, due to the hardness and attenuation of the patient's bones. However, adequate filling of the vertebral body was achieved, and there were no clinical complications (Fig 4). At follow-up, the patient reported an 80% reduction in pain and improvement in mobility. He also went from occasional narcotic usage preoperatively to using no medications, either narcotic or non-narcotic analgesics, by his 1-week follow-up. He has continued using no medication up to his 2-year follow-up and has been able to return to many of his previous activities.
Fig 3.
A, Sagittal T2-weighted MR image from a 32-year-old man with a T8 traumatic compression fracture. B, Sagittal T1-weighted MR image.
Fig 4.
A, T8 vertebral body postvertebroplasty, anteroposterior view. B, T8 vertebral body, postvertebroplasty lateral view.
Complications
Extravasation of cement into the disk space occurred in 3 patients and paravertebrally in 1 patient without complication. One patient had a cement embolus to an anterior midline epidural vein, which was asymptomatic and did not require any additional hospitalization. No other complications occurred. The volume of injected cement was thought to be adequate by the operator in all 15 patients.
Discussion
We began this investigation to determine if vertebroplasty can be used in patients who have experienced a traumatic vertebral compression fracture and who have no history of osteoporosis, multiple myeloma, or long-term steroid use. The use of vertebroplasty for traumatic compression fractures is particularly important due to the inherent problems with more conventional treatments for these injuries, such as hardware failure, loss of reduction, and substantial narcotic usage.7,22 Through this study, we observed that vertebroplasty can be performed as efficiently and safely on patients with traumatic compression fractures as on traditional vertebroplasty candidates. We observed a significant decrease in “pain at rest” at all follow-up evaluations, beginning at the 2-hour follow-up. Additionally, we found a significant improvement in “pain with activity” at the 2-hour follow-up. Our patients also reported increased mobility and decreased narcotic usage; 71% of our patients experienced an increase in mobility throughout the 1-year follow-up period, and >70% of our patients reported a decrease in or have completely stopped their narcotic usage. Many of the patients who were bedridden or had restricted mobility were able to return to their normal activities, while using non-narcotic analgesics or no medications.
The vertebroplasty procedures were completed with limited asymptomatic complications. Concern has been raised that performing vertebroplasty on patients with traumatic fractures might increase the rate of cement extravasation and posterior displacement due to possible endplate fractures and damage to the posterior and anterior longitudinal ligaments.5,23 We observed only a few cases of cement leakage, and in all patients, the leakage was asymptomatic. Our results should give hope to practitioners concerned about the use of vertebroplasty in traumatic cases due to atypical extravasation of cement, because this was not detected in our study. Of note, appropriate caution should still be used with this procedure. The complications observed in our study are similar and no more hazardous than complications reported from other studies of groups in which the use of vertebroplasty was well accepted.24-26
Several small studies have demonstrated encouraging results for the use of vertebroplasty for the treatment of painful nonosteoporotic vertebral compression fractures.2,5 A small study of patients with traumatic compression fractures found a decrease in pain in all subjects with limited extravasation of cement, all of which was asymptomatic.3 Our results confirmed these results with a larger patient population and for a longer duration of follow-up. Additionally, our results are similar to those of a previous study of a large patient series of vertebroplasty outcomes predominantly in patients with osteoporosis.7 The similarity in the results of these 2 studies and our own displays the efficacy of vertebroplasty for patients with traumatic vertebral compression fractures.
Regarding the technical aspects of the procedure, we also were able to inject, on average, 2.3 mL of cement into the vertebra of our patients with traumatic vertebroplasty. This is comparable to injection volumes in other studies, as seen in a previous study of 1000 vertebroplasty procedures in which the average volume of cement injected was 3.3 mL per level.7 This detail is important because it was unknown how the bones of patients without osteoporosis would accept the injection of cement and, thus, affect the efficacy of their vertebroplasty. As seen from our results, the age and attenuation of our patients’ bones did not adversely effect the injection of cement. Additionally, a longer period between the date of injury and the performance of the vertebroplasty was observed in this study, compared with other studies of vertebroplasty, traumatic and nontraumatic. Our disinclination to use this technique with nonosteoporotic traumatic compression fractures might account for the delay, because there was limited evidence supporting the use of vertebroplasty in this subgroup of patients. Because there is now a larger body of evidence supporting vertebroplasty for traumatic fractures, this time delay may decrease and would be an interesting factor, in regard to patient outcomes, to investigate further.
Our study has its limitations. Although this study is the largest, to our knowledge, of this specific group of vertebroplasty candidates, it still involved a small group of patients. The study provided good evidence that vertebroplasty can be used for patients who undergo a traumatic vertebral fracture, but a follow-up study with a large patient series would be ideal. Also, this is a retrospective study that can be influenced by bias and is also influenced by losses to follow-up, especially at 6 months and 1 year. Four of the 15 procedures were performed 1 month before the start of this study; therefore, adequate time had not passed to allow the complete collection of follow-up data from these patients. Additionally, 4 patients had extraspinal injuries, and these may have influenced both our preoperative and postoperative data, because their pain and mobility may have been influenced not only by their vertebral fracture and resulting vertebroplasty but also by the additional fractures sustained and an ongoing disease process, as observed in 1 patient.
Most interesting, 5 of our patients had no signs of edema on their MR imaging. Performing vertebroplasty with no sign of edema has been a controversial issue. There is debate that in the absence of edema, there is no active healing of the vertebra; thus, vertebroplasty would not be beneficial to these patients. A small study has examined the effects of edema on vertebroplasty outcomes for patients with multiple myeloma and has found success in both patients with and without edema.27 The results from our study regarding edema are limited, and further study would be interesting in this area. Additionally, further study of patients with traumatic compression fractures is needed. Ideally, the study would involve a larger patient population, a longer follow-up duration, and younger patients. A larger population would allow confirmation of the results we attained in this study, and a longer follow-up period would allow examination of the long-term results of vertebroplasty for the treatment of traumatic vertebral compression fractures. A study involving traumatic fractures, which compared the results of vertebroplasty with the results of conservative treatment, would also be interesting. If vertebroplasty was found to be a more effective treatment for traumatic fractures, it could be used as a first-line treatment instead of a second effort, after the failure of conservative treatments.
Conclusions
Patients who present with traumatic fractures experience a high level of pain and disability, with many on a regular regimen of narcotics. More than half of our patients were younger than 60 years of age when they underwent vertebroplasty, and it is of great importance that these patients be able to return to their daily activities and have long-lasting results. On the basis of our results, vertebroplasty for patients with traumatic nonosteoporotic vertebral compression fractures is a safe and effective method to decrease pain, increase mobility, and decrease narcotic usage.
References
- 1.McGraw JK, Cardella J, Barr JD, et al. Society of Interventional Radiology quality improvement guidelines for percutaneous vertebroplasty. J Vasc Interv Radiol 2003;14 (9 pt 2):S311–15 [DOI] [PubMed] [Google Scholar]
- 2.Chen J, Lee S. Percutaneous vertebroplasty for the treatment of burst fractures. J Neurosurg Spine 2004;1:228–31 [DOI] [PubMed] [Google Scholar]
- 3.Huet H, Cabal P, Gadan R, et al. Burst-fractures and cementoplasty. J Neuroradiol 2005;32:33–41 [DOI] [PubMed] [Google Scholar]
- 4.Amoretti N, Hovorka E, Marcy P, et al. Burst fracture of the spine involving vertebrae presenting no other lesions: the role of vertebroplasty. Clin Imaging 2005;29:379–82 [DOI] [PubMed] [Google Scholar]
- 5.Chen J, Lee S. Percutaneous vertebroplasty for treatment of thoracolumbar spine bursting fracture. Surg Neurol 2004;62:494–500 [DOI] [PubMed] [Google Scholar]
- 6.Stadhouder A, Buskens E, de Klerk LW, et al. Traumatic thoracic and lumbar spinal fractures: operative or nonoperative treatment—comparison of two treatment strategies by means of surgeon equipoise. Spine 2008;33:1006–17 [DOI] [PubMed] [Google Scholar]
- 7.Layton KF, Thielen KR, Koch CA, et al. Vertebroplasty, first 1000 levels of a single center: evaluation of the outcomes and complications. AJNR Am J Neuroradiol 2007;28:683–89 [PMC free article] [PubMed] [Google Scholar]
- 8.McDonald RJ, Trout AT, Gray LA, et al. Vertebroplasty in multiple myeloma: outcomes in a large patient series. AJNR Am J Neuroradiol 2008;29:642–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koch CA, Layton KF, Kallmes DF. Outcomes of patients receiving long-term corticosteroid therapy who undergo percutaneous vertebroplasty. AJNR Am J Neuroradiol 2007;28:563–66 [PMC free article] [PubMed] [Google Scholar]
- 10.Dansie DM, Luetmer PH, Lane JI, et al. MRI findings after successful vertebroplasty. AJNR Am J Neuroradiol 2005;26:1595–600 [PMC free article] [PubMed] [Google Scholar]
- 11.Kaufmann TJ, Trout AT, Kallmes DF. The effects of cement volume on clinical outcomes of percutaneous vertebroplasty. AJNR Am J Neuroradiol 2006;27:1933–37 [PMC free article] [PubMed] [Google Scholar]
- 12.Rad AE, Kallmes DF. Pain relief following vertebroplasty in patients with and without localizing tenderness on palpation. AJNR Am J Neuroradiol 2008;29:1622–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Trout AT, Gray LA, Kallmes DF. Vertebroplasty in the inpatient population. AJNR Am J Neuroradiol 2005;26:1629–33 [PMC free article] [PubMed] [Google Scholar]
- 14.Trout AT, Kallmes DF, Gray LA, et al. Evaluation of vertebroplasty with a validated outcome measure: the Roland-Morris Disability Questionnaire. AJNR Am J Neuroradiol 2005;26:2652–57 [PMC free article] [PubMed] [Google Scholar]
- 15.Trout AT, Kallmes DF, Kaufmann TJ. New fractures after vertebroplasty: adjacent fractures occur significantly sooner. AJNR Am J Neuroradiol 2006;27:217–23 [PMC free article] [PubMed] [Google Scholar]
- 16.Trout AT, Kallmes DF, Lane JI, et al. Subsequent vertebral fractures after vertebroplasty: association with intraosseous clefts. AJNR Am J Neuroradiol 2006;27:1586–91 [PMC free article] [PubMed] [Google Scholar]
- 17.Trout AT, Kallmes DF, Layton KF, et al. Vertebral endplate fractures: an indicator of the abnormal forces generated in the spine after vertebroplasty. J Bone Miner Res 2006;21:1797–802 [DOI] [PubMed] [Google Scholar]
- 18.Wu SS, Lachmann E, Nagler W. Current medical, rehabilitation, and surgical management of vertebral compression fractures. J Womens Health (Larchmt) 2003;12:17–26 [DOI] [PubMed] [Google Scholar]
- 19.Tezer M, Erturer RE, Ozturk C, et al. Conservative treatment of fractures of the thoracolumbar spine. Int Orthop 2005;29:78–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jensen ME, Evans AJ, Mathis JM, et al. Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fractures: technical aspects. AJNR Am J Neuroradiol 1997;18:1897–904 [PMC free article] [PubMed] [Google Scholar]
- 21.Kallmes DF, Jensen ME. Percutaneous vertebroplasty. Radiology 2003;229:27–36 [DOI] [PubMed] [Google Scholar]
- 22.Afzal SAS, Dhar SA. Short-segment pedicle screw instrumentation and augmentation vertebroplasty in lumbar burst fractures: an experience. Eur Spine J 2008;17:336–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Verlaan JJ, van de Kraats EB, Oner FC, et al. Bone displacement and the role of longitudinal ligaments during balloon vertebroplasty in traumatic thoracolumbar fractures. Spine 2005;30:1832–39 [DOI] [PubMed] [Google Scholar]
- 24.Eck JC, Nachtigall D, Humphreys SC, et al. Comparison of vertebroplasty and balloon kyphoplasty for treatment of vertebral compression fractures: a meta-analysis of the literature. Spine J 2007;8:488–97 [DOI] [PubMed] [Google Scholar]
- 25.Laredo JD, Hamze B. Complications of percutaneous vertebroplasty and their prevention. Semin Ultrasound CT MR 2005;26:65–80 [DOI] [PubMed] [Google Scholar]
- 26.Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine: current options and considerations for treatment. Spine J 2006;6:479–87 [DOI] [PubMed] [Google Scholar]
- 27.Layton KF, Thielen KR, Cloft HJ, et al. Acute vertebral compression fractures in patients with multiple myeloma: evaluation of vertebral body edema patterns on MR imaging and the implications for vertebroplasty. AJNR Am J Neuroradiol 2006;27:1732–34 [PMC free article] [PubMed] [Google Scholar]