With great interest, we read the article by Uotani and colleagues1 in the February issue of the American Journal of Neuroradiology. The authors compared intravenous and intra-arterial contrast agent application for the localization of the Adamkiewicz artery (AKA) in different patients scheduled for thoracic or thoracoabdominal aortic aneurysm repair with use of CT angiography (CTA). Intra-arterial injection seemed to perform much better than intravenous injection regarding AKA localization (94% vs 60%, respectively).
The focus of this study was visualization of the AKA and its direct segmental supplier. The continuity between the AKA and the segmental artery could not be visualized in all cases, possibly because of the proximity of vertebral bony structures with similar signal intensity on CT. However, occlusion of the segmental artery might also be a possible explanation. Two thirds of the patient population had an atherosclerotic aortic aneurysm, but an indirect supply to the aorta was not visualized in any of the patients. This finding is interesting because, in other studies, it has been found that the segmental artery directly connecting to the AKA was occluded in up to 40% of patients.2 In these cases, the AKA supply was provided through an open segmental artery originating 1 or more levels above or below the occluded segmental artery.
Apart from the segmental supply to the AKA, there are alternative routes by which the anterior spinal axis might be supplied. From our own experience2 and that of others,3 we know that spinal cord function is not always crucially dependent on segmental supply directly connecting to the AKA. Collaterals can substitute the spinal cord supply to maintain spinal cord function.3 Recently, these collateral pathways have been visualized with MR angiography (MRA)2 (Fig 1) and correlated with intraoperative spinal cord motor-evoked potentials. It is interesting to note in this study that when the segmental supply to the AKA was inside the cross-clamped aortic region and connecting collaterals originating from outside the cross-clamped aortic area were noticed, this had a predictive value of 97% for stable spinal cord function. This finding can be of crucial importance for the surgeon during the preoperative and intraoperative strategic planning. Therefore, we believe that preoperative imaging in thoracoabdominal aortic aneurysm surgery should not only locate the AKA with its segmental supply but should also locate the possible collateral supply.
Fig 1.
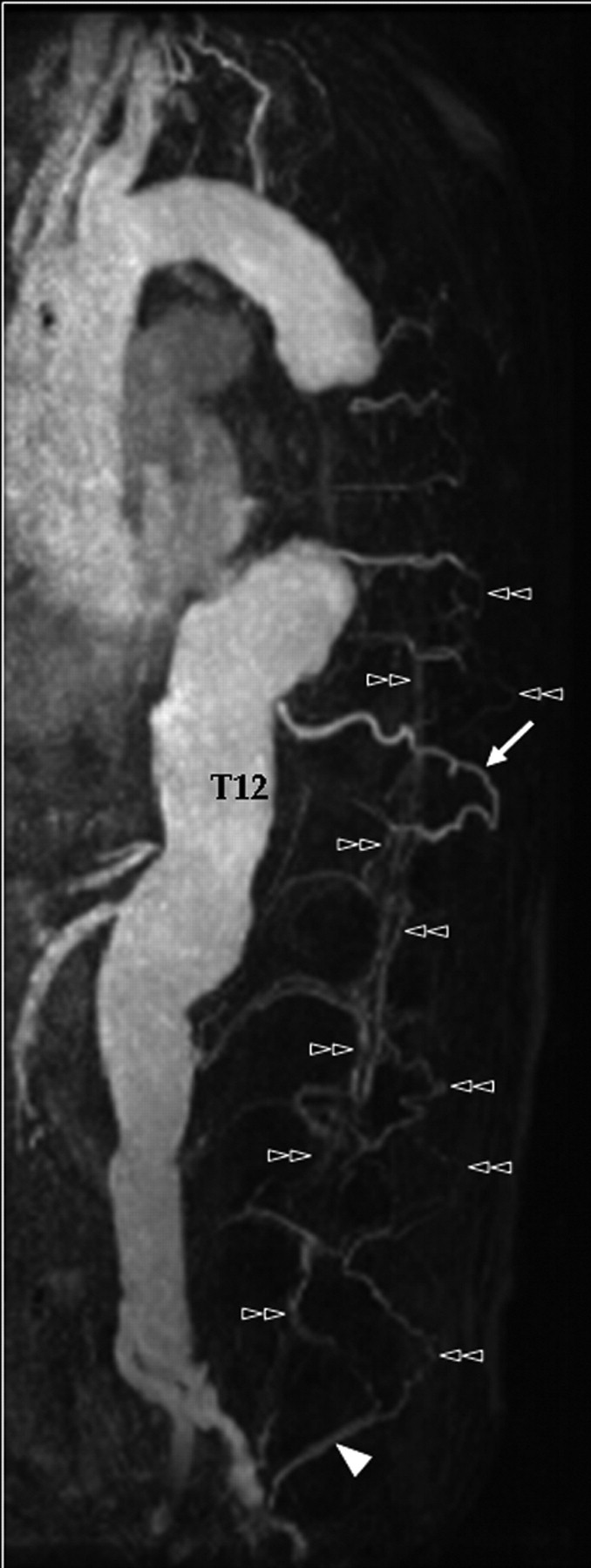
Preoperative contrast-enhanced MRA of a 66-year-old man with a type II thoracoabdominal aortic aneurysm. This example shows a well-developed network of collateral arteries (double arrowheads) originating from the iliolumbar arteries (arrowhead). Note that many of the segmental arteries are occluded at their aortic origin. The AKA in this patient originated at the left aspect of T12. The direct connecting segmental artery was occluded at its aortic origin and was preoperatively most likely supplied by the well-developed T11 segmental artery (arrow).
An important aspect that is mentioned by Uotani et al1 is that a multiphase approach is necessary to convincingly separate the AKA from the similar spatially shaped outlet vein. With the use of CTA, this would mean that the patient is exposed twice to a high effective dose (we calculated 20 mSv for total thoracoabdominal aortic coverage). A smaller vertebral coverage as used in the protocol of Uotani1 (coverage T7-L3) can be used to lower the effective dose. However, in our opinion, this is not an option because of the possibility of missing the location of the AKA and its (indirect) segmental supply. Moreover, regarding visualization of the collateral supply, such a protocol is insufficient because collaterals most often originate from the pelvic circulation2 (Fig 1).
The alternative to CTA is MRA. In the opinion of Uotani et al,1 the true diagnostic value of MRA regarding detection of the AKA is unknown. However, we have prospectively validated 2-phase MRA with digital subtraction angiography regarding AKA localization and have shown excellent agreement.4 In addition, the detection rate of the AKA with use of this MRA technique has shown to be nearly 100% in several studies.
In summary, Uotani et al1 demonstrated better detection of the AKA with CTA by using intra-arterial contrast enhancement. However, because this CTA protocol does not enable visualization of collateral supply to the anterior spinal axis and has not yet been validated, the true diagnostic value has to be proven. As for now, noninvasive MRA provides not only reliable information on the AKA origin but also provides information on the role of collateral circulation. Finally, because preoperative imaging provides only anatomic and no functional information, we advocate conjunctive use of intraoperative monitoring with motor-evoked potentials.
References
- 1.Uotani K, Yamada N, Kono AK, et al. Preoperative visualization of the artery of Adamkiewicz by intra-arterial CT angiography. AJNR Am J Neuroradiol 2008;29:314–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Backes WH, Nijenhuis RJ, Mess WH, et al. Magnetic resonance angiography of collateral blood supply to the spinal cord in thoracic and thoracoabdominal aortic aneurysm patients. J Vasc Surg 2008;48:261–71 [DOI] [PubMed] [Google Scholar]
- 3.Griepp RB, Ergin MA, Galla JD et al. Looking for the Adamkiewicz: a quest to minimize paraplegia after operations for aneurysms of the descending thoracic and thoracoabdominal aorta. J Thorac Cardiovasc Surg 1996;112:1202–13 [DOI] [PubMed] [Google Scholar]
- 4.Nijenhuis RJ, Mull M, Wilmink JT, et al. MR angiography of the great anterior radiculomedullary artery (Adamkiewicz artery) validated by digital subtraction angiography. AJNR Am J Neuroradiol 2006;27:1565–72 [PMC free article] [PubMed] [Google Scholar]


