Brain white matter hyperintensities (WMHs) on MR imaging are reported to increase with age1 and do not decrease,2 though their pathogenesis is not well understood. Here, we report an interesting case in which a patient showed attenuation of WMHs at 1 year after the incidence of cerebral infarction.
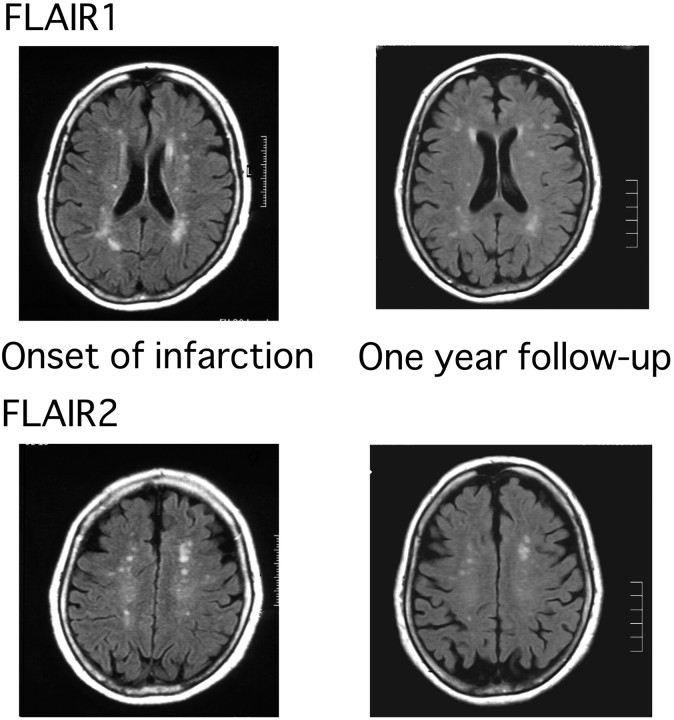
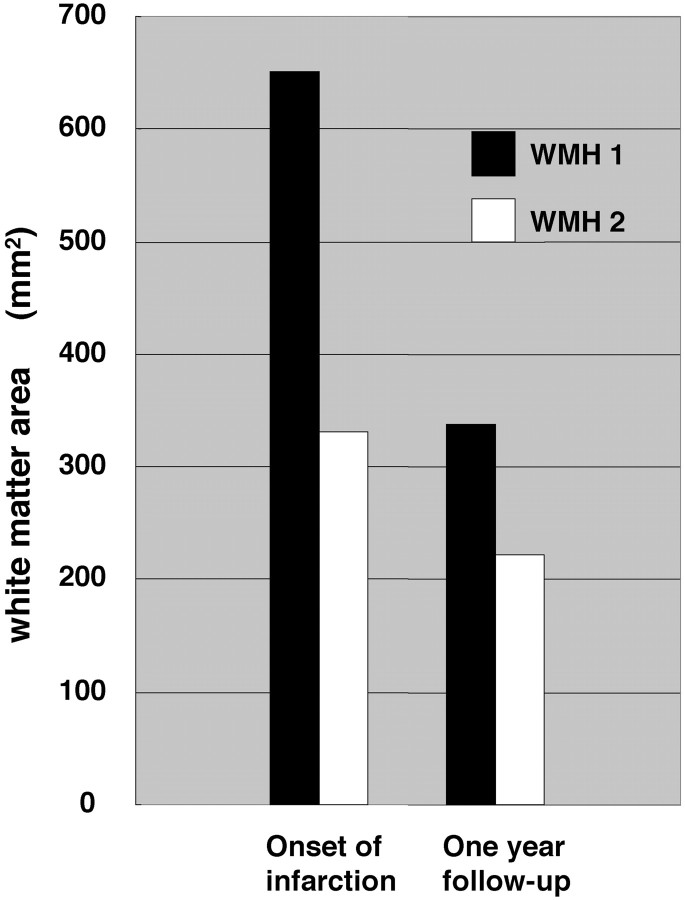
A 78-year-old female outpatient with hypertension and dyslipidemia presented with sudden onset of left homonymous hemianopia. She showed no other neurologic abnormality. The next day, brain MR imaging scans showed an acute infarct in the right occipital lobe. The symptom persisted thereafter with a little amelioration. When follow-up MR imaging scans were performed 1 year later, it was found that the WMHs attenuated (Fig 1). Measurement of the WMH area with MetaMorph 6.2 (Universal Imaging, Downingtown, Pa) confirmed this finding (Fig 2). Because the temporal decrease in WMHs was consistent in 2 different regions of the brain (fluid-attenuated inversion recovery [FLAIR] images 1 and 2), we could rule out a “chance appearance” of the attenuation of WMHs because of the difference in the levels of the 2 temporal images. Because the area of WMHs was apart from the infarct lesion, the change of WMHs was not considered to be from the direct effect of infarction.
Fig 1.
Attenuation of WMHs at 2 different levels (FLAIR 1 and FLAIR 2).
Fig 2.
WMH area was measured with use of MetaMorph 6.2. WMH 1 refers to the area of WMHs at the FLAIR 1 level (Fig 2), and WMH 2 refers to the area of WMHs at the FLAIR 2 level.
WMHs have not been reported to regress,2 though their pathogenesis is not well understood. The proposed mechanisms of their appearance are ischemia; blood-brain barrier dysfunction; and endothelial injury, which are not mutually exclusive.3 In this case, 1 possible explanation for the attenuation of WMHs could be that the blood-brain barrier was disturbed immediately after the onset of infarction, causing leakage of cerebral fluid into the white matter and this recovered afterward.
Image Analysis
The WMH area was quantified by a technician (who was not a physician) in a blind manner with use of MetaMorph 6.2. On acquired FLAIR images, 1) the scale was set; 2) unnecessary white areas such as bone were removed; 3) the average number of pixels in “normal white matter” fields in each image were measured (79 and 82 pixels), and the highest number of pixels in the 2 temporal images was set as the threshold for the ensuing measurement of WMHs; and 4) all of the areas above the threshold were selected, and their size was measured.
Sources of Funding
This study was supported by the Mitsui Sumitomo Insurance Welfare Foundation (2006) and the Japan Health Foundation.
References
- 1.Sachdev P, Wen W, Chen X, et al. Progression of white matter hyperintensities in elderly individuals over 3 years. Neurology 2007;68:214–22 [DOI] [PubMed] [Google Scholar]
- 2.Schmidt R, Fazekas F, Kapeller P, et al. MRI white matter hyperintensities: three-year follow-up of the Austrian Stroke Prevention Study. Neurology 1999;53:132–39 [DOI] [PubMed] [Google Scholar]
- 3.O'Sullivan M. Leukoaraiosis. Pract Neurol 2008;8:26–38 [DOI] [PubMed] [Google Scholar]