Abstract
BACKGROUND AND PURPOSE:
Recent studies on stent placement of significant stenoses at the origin of the vertebral artery reported excellent immediate results. Long-term outcomes, however, were disappointing due to high restenosis rates and stent breakage. In the present study, we evaluated the application of a short drug-eluting balloon-expandable coronary stent for the endovascular treatment of these frequent lesions.
MATERIALS AND METHODS:
In a period of 23 months, 48 patients (12 women, 36 men) with a mean age of 68 years (range, 46–82 years) harboring 52 significant ostial vertebral artery stenoses underwent treatment with short (8 mm) balloon-expandable paclitaxel-eluting coronary stents. Stents were deployed as closely as possible so that the proximal end was just at the origin of the vertebral artery, with high inflation pressure applied. Patients were under continuous medication with acetylsalicylic acid and clopidogrel before and after the treatment. Follow-up clinical assessment and angiography were performed in all patients.
RESULTS:
Periprocedural complications were not encountered. Stenosis severity was reduced from 62 ± 2% (mean ± standard error of the mean) preprocedurally to 15 ± 2% postprocedurally. Follow-up angiography at 7.7 ± 0.6 months revealed a mean stenosis degree of 24 ± 3%. None of the patients developed posterior circulation symptoms related to the treated segment during the follow-up period. Recurrent stenosis (>50%) at follow-up was found in 6 (12%) lesions.
CONCLUSIONS:
Stent placement of significant ostial vertebral artery stenosis by using short drug-eluting stents is safe and yields good midterm patency rates and excellent protection from posterior circulation ischemia.
Stenosis of the ostium (V0) and the proximal segment (V1) of the vertebral artery is a common cause of vertebrobasilar ischemia and an embolic source in the posterior circulation.1,2 Surgical treatment of these lesions is technically challenging and is associated with substantial morbidity and mortality.3,4 Endovascular treatment with balloon angioplasty alone yields unsatisfactory results due to elastic recoil, vessel dissection, and high restenosis rates.5,6 Studies on stent placement of ostial vertebral artery lesions by using bare metal stents have reported excellent immediate results and low rates of periprocedural complications; however, mid- and long-term results remained disappointing due to issues of stent fracture caused by mechanical strain7–9 and high rates of in-stent restenosis as a result of neointimal hyperplasia.7,10,11 The use of drug-eluting coronary stents (DES) for the prevention of in-stent restenosis in ostial vertebral artery stenotic lesions has been advocated recently.12–16 However, follow-up restenosis rates are widely scattered in these studies, ranging from 0% to 63%. This uncertainty may be partly attributable to the relatively small number of treated stenoses with angiographic follow-up (n = 2–8) in most of these studies, with the exception of the report of Gupta et al,15 who analyzed 27 vertebral ostial stenoses treated with DES and reported significant (>50%) in-stent restenosis in 7% of the cases after a mean follow-up period of 4 months. Another issue hampering the interpretation of the available studies with DES is that the investigators did not confine the applied stents to 1 type, sometimes not even within the same study.
In the present article, we report midterm clinical and angiographic follow-up results in 52 significant stenoses of the vertebral artery ostium, treated with stent angioplasty by using a short balloon-expandable DES.
Materials and Methods
Patients
Forty-eight patients (12 women, 36 men) with a mean age of 68 years (range, 46–82 years) harboring 52 significant ostial vertebral artery stenoses underwent stent placement of the vertebral artery origin during a 23-month period between April 2007 and February 2009 at our institution. Informed consent (including the fact that the stent was used off-label) was obtained from each patient before the intervention and follow-up angiography.
Stent-Placement Procedure
All patients received combined antiplatelet treatment with 100-mg aspirin and 75-mg clopidogrel daily for at least 2 days prior to the intervention or received a loading dose of 500-mg aspirin and 600-mg clopidogrel immediately prior to the procedure. The double antiplatelet medication was continued for at least 1 year postinterventionally. All interventions were performed with the patient under local anesthesia and monitored anesthesia care. An intravenous bolus of heparin (70 U/kg body weight) and aspirin (7 mg/kg body weight) was administered at the beginning of the procedure. Vascular access was obtained via the common femoral artery by using a 6F-8F introducer sheath. Baseline angiography was performed, and the severity of the stenosis of the vertebral artery origin was calculated by using the diameter of the ipsilateral V2 segment as a reference, similar to the method used to quantify carotid stenosis degree in the North American Symptomatic Carotid Endarterectomy Trial.17
A 6F-8F guiding catheter was then inserted into the subclavian artery, and the stenosis was passed under road-mapping with a 0.014-inch (0.35 mm) guidewire. A short (length, 8 mm; diameter, 4 mm) balloon-expandable paclitaxel-eluting coronary stent (Coroflex Please; B. Braun, Melsungen, Germany) was carefully placed into the stenosed segment under fluoroscopic guidance by using 11-cm image-intensifier diameter and an x-ray pulse rate of 30 frames per second. Care was taken to place the proximal end of the stent as close as possible to the upper contour of the subclavian artery. The stent was deployed first by manual inflation of the balloon to achieve better controllability, which was followed by controlled inflation to 13 atm by using a manometer. Stents of the same type and size were used in all patients in the present study. Following the deflation of the balloon, control angiography was performed and the degree of residual stenosis was determined.
Follow-Up
All patients were scheduled for follow-up, which included assessment of the neurologic status, history of neurologic symptoms, and MR imaging and angiographic examination at 6 weeks (at the time of writing, 6 patients), 12 weeks (13 patients), 6 months (15 patients), and 12 months (14 patients) after the endovascular treatment.
Results
The clinical characteristics of the study group are presented in Table 1.
Table 1:
Patient demographics and clinical characteristics
| Characteristic | Data |
|---|---|
| Male-female | 36:12 |
| Age (range) | 68 yr (46–82 yr) |
| Vascular risk factors | |
| Smoking | 10 (21%) |
| Hypertension | 23 (48%) |
| Diabetes | 13 (27%) |
| Hyperlipidemia | 13 (27%) |
| Coronary artery disease | |
| Previous posterior circulation stroke | 10 (21%) |
| Bilateral vertebral artery disease | 24 (50%) |
| Contralateral vertebral artery occlusion | 7 (15%) |
| Intracranial stenosis in the posterior circulation | 14 (29%) |
| Symptoms of vertebrobasilar ischemia | |
| Dizziness | 18 (38%) |
| Drop attack | 4 (8%) |
| Dysarthria | 2 (4%) |
| Vertigo | 19 (40%) |
| Nystagmus | 7 (15%) |
| Gait disturbance | 9 (19%) |
| Diplopia | 6 (13%) |
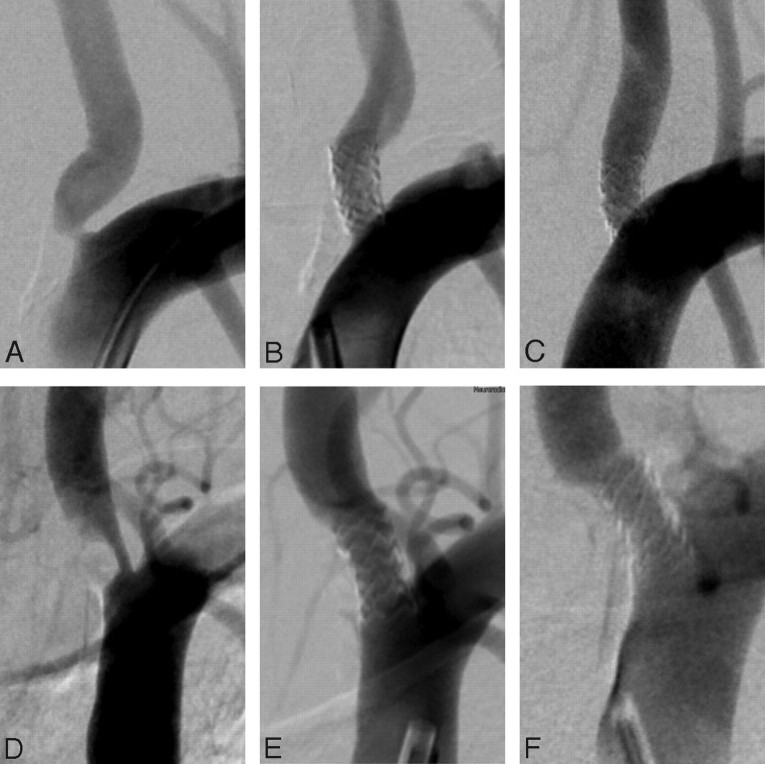
The degree of stenosis of vertebral artery origin was reduced from 62 ± 2% (mean ± standard error of the mean) preprocedurally to 15 ± 2% postprocedurally. An illustrative case is presented in Fig 1. Periprocedural technical or clinical complications were not encountered. None of the patients developed symptoms of vertebrobasilar ischemia related to the treated vertebral artery segment during the procedure or in the follow-up period.
Fig 1.
Representative angiographic images from patients with significant vertebral ostial stenosis. A–C, Preprocedural (A), postprocedural (B), and 5-month follow-up (C) images in a 62-year-old male patient. D–F, Preprocedural (D), postprocedural (E), and 4-month follow-up (F) images in a 68-year-old male patient with significant stenosis of the left vertebral ostium.
Angiographic follow-up performed at a mean of 7.7 ± 0.6 months (range, 2–15 months) revealed a mean stenosis degree of 24 ± 3%. In 6 cases (12%), the severity of the stenosis on the follow-up angiography exceeded 50%.
In 15 patients (29%), we had angiographic follow-up ≥12 months after treatment. In 3 of those, a recurrent in-stent stenosis of >50% was found; and in 1 of these patients, the in-stent restenosis was found to be progressive between 6- and 15-month follow-up angiography. Patients with significant restenosis are scheduled for retreatment using the same method.
Discussion
Stent treatment of significant stenoses of the vertebral artery ostium remains a major challenge with disappointing long-term results. Attempts to treat ostial stenoses by using bare metal stents were largely hampered by in-stent restenosis as a result of neointimal hyperplasia and by stent breakage as a consequence of mechanical strain in an anatomic location with strong pulsatile movement, unfavorable angulation of the subclavian and vertebral arteries, and tortuosity of the vertebral origin. A review of the previous studies on vertebral artery origin stent placement is given in Table 2. The literature on coronary stent placement has shown that the use of sirolimus- or paclitaxel-eluting stents (DES) significantly reduces restenosis rates by inhibiting neointimal hyperplasia.18 High inflation pressure facilitates stent-strut apposition and thereby the delivery of higher concentrations of the bioactive agent locally to the atherosclerotic lesion.19 Regarding the mechanical strain on the stent in the proximal segment of the vertebral artery, a short stent, with the proximal end placed exactly at the level of the vertebral ostium (ie, without hanging into the subclavian artery), faces less shearing force due to pulsation and tortuosity and is, therefore, less prone to breakage or dislodgement. In addition, experience in coronary stent placement confirms that the restenosis rate can be reduced by implanting short stents.20
Table 2:
Review of previous studies on stent angioplasty of stenotic lesions of the vertebral artery ostium
| Author | No. Patients | No. Treated Stenoses | Rate of Complication (%) |
Follow-Up |
Morbidity/Mortality Related to the Treated Stenosis in the Follow-Up Period (%) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Technical | Clinical | Period (months) | No. Stenoses | Rate of Significant Restenosis (%) | Rate of Stent Occlusion (%) | ||||
| Bare metal stents | |||||||||
| Chastain et al5 | 50 | 55 | 2 | 0 | 6 | 49 | 10 | 0 | 4/0 |
| Albuquerque et al7 | 33 | 33 | 3 | 0 | 16 | 30 | 43 | 0 | 0/0 |
| Lin et al22 | 58 | 67 | 0 | 7 | 11 | 32 | 25 | 1 | 3/0 |
| Weber et al10 | 38 | 38 | 5 | 2 | 11 | 26 | 36 | 0 | 2/0 |
| SSYLVIA Study11 | 6 | 6 | – | –* | 6 | 6 | 67 | 0 | –* |
| Cloud et al23 | 14 | 14 | 0 | 0 | 20 | 11 | 9 | 0 | 0/0 |
| Lin et al24 | 80 | 90 | 0 | 0 | 12 | 40 | 21 (short stenoses)29 (medium length) 50 (long stenoses) | 0 | 0/0 |
| Akins et al12 | 7 | 7 | 0 | 0 | 36 | 7 | 43 | 1 | 0/0 |
| Taylor et al25 | 44 | 48 | 0 | 0 | 7 | 48 | 48 | 0 | 0/0 |
| Drug-eluting stents | |||||||||
| Lin et al13 | 11 | 11 | 0 | 0 | 4 and 8 | 2 | 0 | 0 | 0/0 |
| Lugmayr et al14 | 7 | 8 | 0 | 0 | 6 | 8 | 63 | 0 | 28/0 |
| Gupta et al15 | 27 | 27 | 0 | 2 | 4 | 27 | 7 | 0 | 0/0 |
| Akins et al12 | 5 | 5 | 0 | 0 | 17 | 5 | 0 | 0 | 0/0 |
| Edgell et al16 | 5 | 5 | 0 | 0 | 15 | 5 | 0 | 0 | 1/0 |
| Our data | 48 | 52 | 0 | 0 | 7 | 52 | 12 | 0 | 0/0 |
Note:—SSYLVIA indicates Stenting of Symptomatic Atherosclerotic Lesions in the Vertebral or Intracranial Arteries.
The exact location of the treated stenoses responsible for the clinical complications is not given specifically in the article.
In the present study, we report midterm clinical and angiographic follow-up results in 52 ostial vertebral artery lesions treated with short balloon-expandable paclitaxel-eluting stents, placed exactly at the orifice of the vertebral artery and deployed with high inflation pressure. To our knowledge, this is the highest number of patients treated with DES so far. Our midterm (7 months) clinical follow-up data without any ischemic event in the posterior circulation indicates that stent placement of ostial vertebral artery stenotic lesions with DES is safe, even when performed without a distal protection device.21 The midterm rate of significant restenosis in 12% of patients, without target-lesion–related morbidity or mortality is acceptable. In principle, an additional rate of in-stent restenosis during the long-term follow-up is possible; however, in our series of patients with >1 year follow-up, it was infrequently observed (1 of 15 patients).
Conclusions
In this study, stent placement of vertebral artery stenosis by using short DES was safe and yielded good midterm patency rates. In our experience, short DES, deployed with high pressure and placed with the proximal end as close as possible to the level of the subclavian artery, are less prone to intimal hyperplasia, recurrent stenosis, and stent breakage.
References
- 1. Wityk RJ, Chang HM, Rosengart A, et al. Proximal extracranial vertebral artery disease in the New England Medical Center Posterior Circulation Registry. Arch Neurol 1998;55:470–78 [DOI] [PubMed] [Google Scholar]
- 2. Caplan LR, Amarenco P, Rosengart A, et al. Embolism from vertebral artery origin occlusive disease. Neurology 1992;42:1505–12 [DOI] [PubMed] [Google Scholar]
- 3. Spetzler RF, Hadley MN, Martin NA, et al. Vertebrobasilar insufficiency. Part 1. Microsurgical treatment of extracranial vertebrobasilar disease. J Neurosurg 1987;66:648–61 [DOI] [PubMed] [Google Scholar]
- 4. Blacker DJ, Flemming KD, Wijdicks EF. Risk of ischemic stroke in patients with symptomatic vertebrobasilar stenosis undergoing surgical procedures. Stroke 2003;34:2659–63 [DOI] [PubMed] [Google Scholar]
- 5. Chastain HD, 2nd, Campbell MS, Iyer S, et al. Extracranial vertebral artery stent placement: in-hospital and follow-up results. J Neurosurg 1999;91:547–52 [DOI] [PubMed] [Google Scholar]
- 6. Motarjeme A, Keifer JW, Zuska AJ. Percutaneous transluminal angioplasty of the vertebral arteries. Radiology 1981;139:715–17 [DOI] [PubMed] [Google Scholar]
- 7. Albuquerque FC, Fiorella D, Han P, et al. A reappraisal of angioplasty and stenting for the treatment of vertebral origin stenosis. Neurosurgery 53:607–14, 2003, discussion 614–16 [DOI] [PubMed] [Google Scholar]
- 8. Tsutsumi M, Kazekawa K, Onizuka M, et al. Stent fracture in revascularization for symptomatic ostial vertebral artery stenosis. Neuroradiology 2007;49:253–57 [DOI] [PubMed] [Google Scholar]
- 9. Kim SR, Baik MW, Yoo SH, et al. Stent fracture and restenosis after placement of a drug-eluting device in the vertebral artery origin and treatment with the stent-in-stent technique: report of two cases. J Neurosurg 2007;106:907–11 [DOI] [PubMed] [Google Scholar]
- 10. Weber W, Mayer TE, Henkes H, et al. Efficacy of stent angioplasty for symptomatic stenoses of the proximal vertebral artery. Eur J Radiol 2005;56:240–47 [DOI] [PubMed] [Google Scholar]
- 11. SSYLVIA Study Investigators. Stenting of Symptomatic Atherosclerotic Lesions in the Vertebral or Intracranial Arteries (SSYLVIA): study results. Stroke 2004;35:1388–92. [DOI] [PubMed] [Google Scholar]
- 12. Akins PT, Kerber CW, Pakbaz RS. Stenting of vertebral artery origin atherosclerosis in high-risk patients: bare or coated?—a single-center consecutive case series. J Invasive Cardiol 2008;20:14–20 [PubMed] [Google Scholar]
- 13. Lin YH, Hung CS, Tseng WY, et al. Safety and feasibility of drug-eluting stent implantation at vertebral artery origin: the first case series in Asians. J Formos Med Assoc 2008;107:253–58 [DOI] [PubMed] [Google Scholar]
- 14. Lugmayr H, Kastner M, Fröhler W, et al. Sirolimus-eluting stents for the treatment of symptomatic extracranial vertebral artery stenoses: early experience and 6-month follow-up [in German]. Rofo 2004;176:1431–35 [DOI] [PubMed] [Google Scholar]
- 15. Gupta R, Al-Ali F, Thomas AJ, et al. Safety, feasibility, and short-term follow-up of drug-eluting stent placement in the intracranial and extracranial circulation. Stroke 2006;37:2562–66 [DOI] [PubMed] [Google Scholar]
- 16. Edgell RC, Yavagal DR, Drazin D, et al. Treatment of vertebral artery origin stenosis with anti-proliferative drug-eluting stents. J Neuroimaging 2008. November 7 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 17. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis: North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 1991;325:445–53 [DOI] [PubMed] [Google Scholar]
- 18. Stone GW, Ellis SG, Cox DA, et al. A polymer-based, paclitaxel-eluting stent in patients with coronary artery disease. N Engl J Med 2004;350:221–31 [DOI] [PubMed] [Google Scholar]
- 19. Slottow TL, Waksman R. Drug-eluting stent safety. Am J Cardiol 2007;100:10M–17M. [DOI] [PubMed] [Google Scholar]
- 20. Dietz U, Holz N, Dauer C, et al. Shortening the stent length reduces restenosis with bare metal stents: matched pair comparison of short stenting and conventional stenting. Heart 2006;92:80–84. Epub 2005 May 9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Qureshi AI, Kirmani JF, Harris-Lane P, et al. Vertebral artery origin stent placement with distal protection: technical and clinical results. AJNR Am J Neuroradiol 2006;27:1140–45 [PMC free article] [PubMed] [Google Scholar]
- 22. Lin YH, Juang JM, Jeng JS, et al. Symptomatic ostial vertebral artery stenosis treated with tubular coronary stents: clinical results and restenosis analysis. J Endovasc Ther 2004;11:719–26 [DOI] [PubMed] [Google Scholar]
- 23. Cloud GC, Crawley F, Clifton A, et al. Vertebral artery origin angioplasty and primary stenting: safety and restenosis rates in a prospective series. J Neurol Neurosurg Psychiatry 2003;74:586–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lin YH, Liu YC, Tseng WY, et al. The impact of lesion length on angiographic restenosis after vertebral artery origin stenting. Eur J Vasc Endovasc Surg 2006;32:379–85 [DOI] [PubMed] [Google Scholar]
- 25. Taylor RA, Siddiq F, Suri MF, et al. Risk factors for in-stent restenosis after vertebral ostium stenting. J Endovasc Ther 2008;15:203–12 [DOI] [PubMed] [Google Scholar]