SUMMARY:
Spinal cord infarction following lumbar transforaminal epidural steroid injection is a rare and devastating complication. We describe the case of a 55-year-old woman who developed spinal cord infarction following right L2-3 transforaminal epidural injection, diagnosed on the basis of clinical and MR imaging findings. Spinal angiography demonstrated occlusion of the right L2 segmental artery with reconstitution of the radicular branch from collaterals. The artery of Adamkeiwicz could not be demonstrated and was presumably occluded by the steroid injection.
Transforaminal epidural steroid injection (TF ESI) is a common procedure in the nonsurgical management of lumbosacral radiculopathy. The incidence of significant complications is low. Spinal cord infarction (SCI) following lumbar TF ESI is one of the rarest yet most devastating complications, with 5 cases reported in the literature.1–3 Inadvertent vascular penetration of a radiculomedullary artery by the procedure needle has been implicated as the likely etiology. Cord ischemia could result from vascular injury with thrombosis or embolism involving the artery of Adamkiewicz or from occlusion secondary to intra-arterial injection of steroid suspension. In this case, we describe the MR imaging and angiographic findings in a case of SCI following lumbar TF ESI. To our knowledge, the angiographic findings have never been reported.
Case Report
A 55-year-old woman with an acute-on-chronic disk herniation at L1–2 presented for TF ESI at L2–3 on the right. Initial placement of a 22-gauge spinal needle reportedly showed backbleeding on removal of the stylet, which apparently resolved once the needle was repositioned. Epidural placement of the needle tip was reportedly confirmed following injection of 2 mL of myelographic contrast (Fig 1), followed by therapeutic injection of an additional 1 mL of triamcinolone acetonide (Kenalog) and 0.25% bupivacaine. Within minutes of the injection, the patient developed bilateral lower extremity weakness, which progressed to flaccid paralysis.
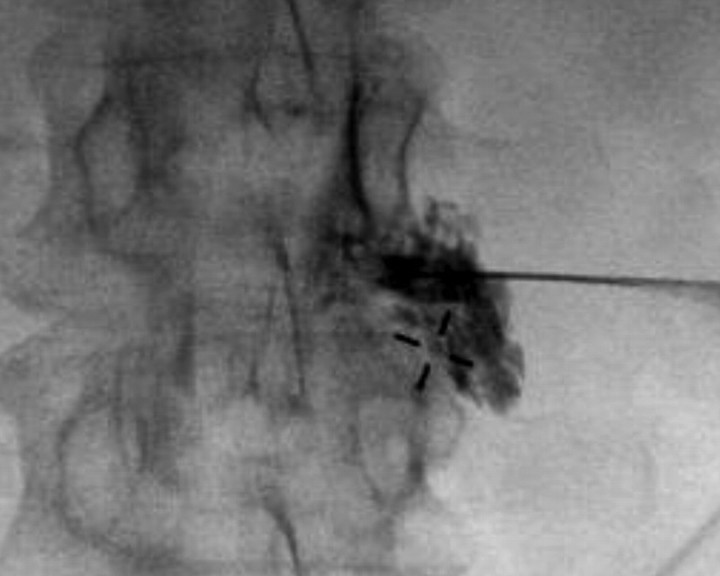
Fig 1.
Prone fluoroscopic image during right L2–3 TF ESI demonstrates epidural opacification before therapeutic injection.
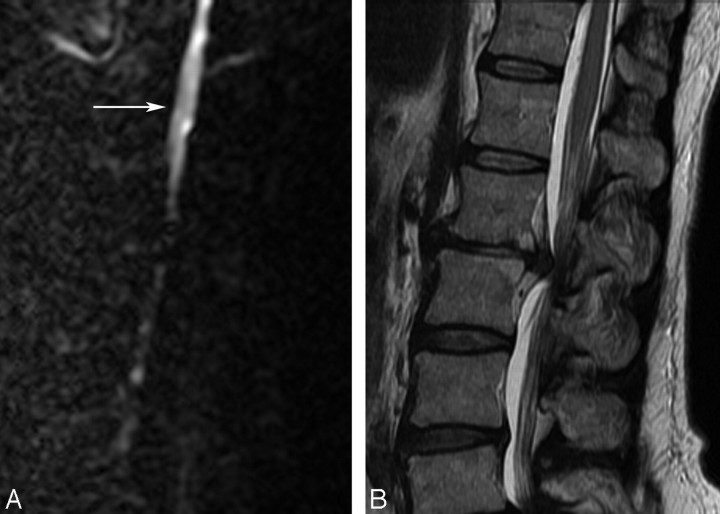
The patient underwent CT of the thoracolumbar spine within 1.5-hours of the injection, which demonstrated no evidence of epidural hematoma. MR imaging of the spine was performed approximately 4 hours after the injection, including sagittal and axial T1 (TR, 350; TE, 15.7), T2 (TR, 3950; TE, 105), and echo-planar diffusion-weighted imaging (b = 1000). T2-weighted images demonstrated subtly increased signal intensity within the central gray matter of the distal thoracic cord with restricted water diffusion in the same area (Fig 2).
Fig 2.
Sagittal DWI (left) and T2-weighted images of the thoracolumbar spine demonstrate restricted water diffusion in the distal cord and conus (white arrow). Note a large disk herniation at L1–2, for which the TF ESI was being performed.
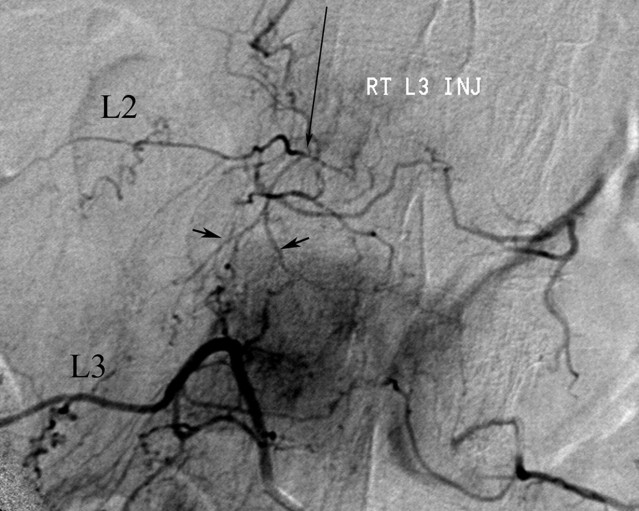
Catheter-directed spinal angiography was performed to evaluate potentially treatable causes of spinal cord ischemia, including spasm or dissection. The ostium of the right L2 segmental artery could not be selected and was presumed to be occluded. Injection of the right L3 segmental artery demonstrated collateral vessels coursing toward the right L2–3 foramen, with irregular attenuated reconstitution of the distal L2 segmental branch and radicular artery (Fig 3). Additionally, a thoracolumbar spinal angiogram failed to demonstrate the origin of the artery of Adamkiewicz.
Fig 3.
Angiogram of the right L3 segmental artery (L3) demonstrates prominent collateral vessels (short black arrows) in the region of the right L2 pedicle. The distal right L2 segmental (L2) and radicular (long black arrow) arteries are irregular and attenuated. The ostium of the right L2 segmental lumbar artery could not be found and was presumably occluded.
Acute spinal cord ischemia was diagnosed on the basis of the clinical and radiographic findings. The patient's symptoms have not improved, and she remains paraplegic.
Discussion
TF ESI is a common procedure used in the nonsurgical management of lumbosacral radiculopathy.4,5 The transforaminal approach allows concentrated delivery of medication to the ventral neural foramen and anterior epidural space, the areas most likely affected by disk pathology. However, needle placement via a transforaminal approach makes inadvertent vascular penetration of the radicular artery possible.
Minor complications include headache, back pain, worsening leg pain, facial flushing, and vasovagal reaction and have a reported incidence of 9.6%.6 Serious complications (eg, epidural hematoma, abscess, arachnoiditis) are uncommon, with an incidence of 0.9%.7 One of the rarest, yet most devastating, complications is spinal cord ischemia, which has been reported 5 times in the literature following lumbosacral TF ESI.1–3
The blood supply to the thoracic spinal cord is predominantly from the anterior spinal artery, and a poor collateral network with the smaller posterior spinal arteries places the cord at high risk of ischemia if the dominant blood supply is compromised. At every level in the thoracolumbar spine, radicular branches off the segmental intercostal or lumbar arteries supply the exiting nerve root and foraminal structures. At as many as 5–6 levels, the radicular arteries also contribute to the anterior spinal artery, termed “radiculomedullary arteries.” The dominant radiculomedullary artery is called the “artery of Adamkiewicz” and is the primary source of blood for the thoracic cord. The artery of Adamkiewicz originates between T9 and L2 on the left in 85% of people, though aberrant origins from every lumbar level and S1 have been reported.
Theories regarding the cause of the SCI after TF ESI implicate inadvertent penetration of the radicular artery within the neural foramen in combination with a low origin of the artery of Adamkiewicz. Penetration of the radicular artery could result in focal dissection and distal emboli. If the injured radicular artery was, in fact, the artery of Adamkiewicz, this could result in spinal cord ischemia. Another proposed mechanism of injury suggests that intra-arterial injection of steroid suspension results in a shower of thrombogenic particulates to the distal cord with resultant ischemia.8
The incidence of vascular penetration with transforaminal needle placement is reportedly 8.1% at lumbar levels.9 Additionally, the use of a “flash” or backbleeding is not a reliable predictor of inadvertent vascular penetration.9 In this case, a small amount of backbleeding was reported on initial needle placement, which apparently resolved with repositioning. Contrast injection before therapeutic injection reportedly demonstrated epidural opacification.
CT and MR imaging are primarily used to exclude surgically correctable pathology that may mimic cord ischemia clinically. In this case, CT demonstrated no evidence of epidural collection or explanation for the flaccid paralysis. Findings on T2-weighted MR images are often normal but may demonstrate cord expansion and hyperintense signal intensity in the central cord and/or gray matter.10 Diffusion-weighted imaging (DWI) can also be useful in the setting of acute cord ischemia, demonstrating restricted diffusion.10,11 In this case, MR imaging of the spine performed 4 hours after injection demonstrated increased T2 signal intensity in the gray matter and restricted diffusion in the lower thoracic cord. These findings are clinically useful because transient paralysis following subarachnoid injection of anesthetic has been reported.12
Catheter-directed spinal angiography in the setting of acute SCI following TF ESI has not been previously reported and was performed to evaluate potentially treatable lesions. In this case, the steroid injection presumably penetrated the right L2 radicular artery. The right L2 segmental artery origin could not be selected; however, if it was thrombosed back close to its origin, its presence would not have been detectable due to the inability to opacify the lumen. Irregular attenuated opacification of the distal right L2 segmental and radicular arteries via collaterals suggests that there was also spasm and/or thrombosis involving these vessels. The artery of Adamkiewicz was not demonstrated and putatively arose from the right L2 and was thrombosed. With such widespread vascular irregularity, we believe the SCI was likely secondary to inadvertent intra-arterial injection of thrombogenic particulate steroid. Although a focal dissection could theoretically result in distal emboli to the cord, it is unlikely to cause such widespread alteration in the appearance of the branches of the L2 segmental artery.
Conclusions
TF ESI is a common procedure in the nonsurgical management of chronic radicular pain. Although the incidence of serious complications is exceeding small, practitioners who perform this procedure should be aware of the potentially devastating complication of spinal cord ischemia. On the basis of the angiographic findings in our patient, the underlying etiology is likely related to inadvertent vascular penetration with intra-arterial injection of particulate steroid into the artery of Adamkiewicz, rather than a focal vascular injury.
References
- 1. Houten J, Errico T. Paraplegia after lumbosacral nerve root block: report of three cases. Spine J 2002;2:70–75 [DOI] [PubMed] [Google Scholar]
- 2. Huntoon M, Martin D. Paralysis after transforaminal epidural injection and previous spinal surgery. Reg Anesth Pain Med 2004;29:494–95 [DOI] [PubMed] [Google Scholar]
- 3. Somayaji H, Saifuddin A, Cassey A, et al. Spinal cord infarction following therapeutic computed tomography guided left L2 nerve root injection. Spine 2005;30:106–08 [DOI] [PubMed] [Google Scholar]
- 4. Lutz G, Vad V, Wisneski R. Fluoroscopic transforaminal lumbar epidural steroids: an outcome study. Arch Phys Med Rehabil 1998;79:1362–66 [DOI] [PubMed] [Google Scholar]
- 5. Vad V, Bhat A, Lutz G, et al. Transforaminal epidural steroid injections in lumbosacral radiculopathy. Spine 2002;27:11–16 [DOI] [PubMed] [Google Scholar]
- 6. Botwin K, Gruber R, Bouchlas C. Complications of fluoroscopically guided transforaminal lumbar epidural injections. Arch Phys Med Rehabil 2000;81:1045–50 [DOI] [PubMed] [Google Scholar]
- 7. Slipman C, Meyers J, Chou L, et al. Complications of fluoroscopically guided spinal injections. Arch Phys Med Rehabil 1995;76:1032 [Google Scholar]
- 8. Tiso R, Cutler T, Catania J, et al. Adverse central nervous system sequelae after selective transforaminal block: the role of corticosteroids. Spine J 2004;4:468–74 [DOI] [PubMed] [Google Scholar]
- 9. Furman M, O'Brien E, Zgleszewski T. Incidence of intravascular penetration in transforaminal lumbosacral epidural steroid injections. Spine 2000;25:2628–32 [DOI] [PubMed] [Google Scholar]
- 10. Kuker W, Weller M, Klose U, et al. Diffusion-weighted MRI of spinal cord infarction: high-resolution imaging and time course of diffusion abnormality. J Neurol 2004;251:818–24 [DOI] [PubMed] [Google Scholar]
- 11. Sibon I, Menegon P, Moonen C, et al. Early diagnosis of spinal cord infarct using magnetic resonance diffusion imaging. Neurology 2003;61:1622 [DOI] [PubMed] [Google Scholar]
- 12. McLain R, Fry M, Hecht S. Transient paralysis associated with epidural steroid injection. J Spinal Disord 1997;10:441–44 [PubMed] [Google Scholar]