Unfortunately, the diagnosis of the involvement of the central nervous system by tuberculosis remains difficult; therefore, one should be familiar with the various radiologic features because neurotuberculosis can mimic numerous other disease entities. Parenchymal tuberculosis is more common in human immunodeficiency virus (HIV)-infected patients and can occur with or without meningitis. The most frequent form is tuberculous granuloma (tuberculoma). Other presentations are tuberculous abscess, focal cerebritis, and “allergic” tuberculous encephalopathy.1–3 We report a case of neurotuberculosis with extensive parenchymal lesions involving middle cerebellar peduncles (MCPs) that resolved partially after treatment.
A 58-year-old woman was admitted with subacute onset of slurred speech for approximately 48 hours. She had no relevant medical history. Shortly thereafter, slurred speech, impairment of limb coordination, and progressive difficulty walking developed. Neurologic examination revealed marked dysarthria with scanning speech, gait ataxia, horizontal nystagmus on bilateral gaze, and dysmetria of all 4 limbs. Findings of laboratory results and chest radiography were normal. Findings of antinuclear antibody, angiotensin-converting enzyme, Cryptococcus antigen, syphilis, toxoplasma, and HIV serologies were all negative. MR imaging showed, in T2-weighted and fluid-attenuated inversion recovery (FLAIR) sequences, areas with increased signal intensity in the central mesencephalon, bilateral MCP, cingulate cortex area involving the callosum corpus, and left perisylvian area (Fig 1). CSF examination revealed a negative Gram staining, a total protein level of 1 g/L, a glucose level of 3.2 mmol/L, and 12 cell/μL. Findings of bacterial, mycobacterial, and fungal stains and cultures were negative. The CSF polymerase chain reaction study was positive for Mycobacterium tuberculosis. The patient was started on a 4-drug therapy (ethambutol, pyrazinamide, isoniazid, and rifampicin), and she recovered fully 6 months later. A new MR imaging showed a minimal hyperintensity in the MCP, midbrain, and left perisylvian area (Fig. 1).
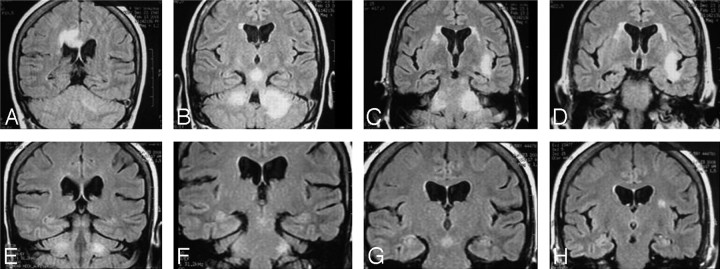
Fig 1.
Coronal FLAIR MR images show hyperintense lesions in the cingulate cortex area involving the corpus callosum (A), central midbrain (B), asymmetric bilateral MCP (B and C), and left perisylvian area (C and D). Five months later, images show minimal hyperintense lesions in both the MCP (E and F), central midbrain (G), and left perisylvian area (H).
Bilateral involvement of the MCP is well known in olivopontocerebellar atrophy but is relatively rare in other diseases. It was observed in various pathologic conditions: metabolic diseases; neoplasm; cerebrovascular diseases, including posterior reversible encephalopathy syndrome; and inflammatory and demyelinating diseases.4 We present an HIV-negative patient with extensive involvement of brain parenchyma by tuberculosis, in which the MR imaging lesions are not typical and resemble more of a parainfectious demyelinating pattern than that of either a tuberculoma or meningitis. We found no documented cases of bilateral involvement of the MCP caused by neurotuberculosis.1–4)
References
- 1. Pui MH, Memon WA. Magnetic resonance imaging findings in tuberculous meningoencephalitis. Can Assoc Radiol J 2001; 52: 43– 49 [PubMed] [Google Scholar]
- 2. Bernaerts A, Vanhoenacker F, Parizel PM, et al. Tuberculosis of the central nervous system: overview of neuroradiological findings. Eur Radiol 2003; 13: 1876– 90 [DOI] [PubMed] [Google Scholar]
- 3. Kais N, Allani R, Abdelmalek R, et al. Value of magnetic resonance imaging in central nervous system tuberculosis. Presse Med 2008; 37( 4 pt 2): 634– 42 [DOI] [PubMed] [Google Scholar]
- 4. Okamoto K, Tokiguchi S, Furusawa T, et al. MR features of diseases involving bilateral middle cerebellar peduncles. AJNR Am J Neuroradiol 2003; 24: 1946– 54 [PMC free article] [PubMed] [Google Scholar]