Abstract
SUMMARY: A 59-year-old woman treated chronically with enalapril, an angiotensin-converting enzyme inhibitor (ACE-I) presented with difficult swallowing and speaking. Although her symptoms were clinically consistent with an adverse angioedema reaction to the ACE-I, initial imaging was not entirely consistent with our conceptual understanding of angioedema. This case report will discuss the myriad possible imaging presentations of this disease, as well as the differential diagnosis for this atypical manifestation of ACE-I–induced angioedema.
Angiotensin-converting enzyme inhibitors (ACE-Is) have become extremely widespread medications, used to treat hypertension and congestive heart failure.1 Generally well tolerated, these medications have a well-known association with head and neck angioedema—swelling of the facial, labial, lingual, laryngeal, and glossopharyngeal tissues. Although this side effect is well known among clinicians, the imaging characteristics have not been well described in the extant literature, and the protean imaging manifestations of this disorder can lead to misdiagnosis. We report a case of angioedema in a patient chronically treated with enalapril, in whom initial imaging first suggested the possibility of tumor or infection.
Case Report
A 59-year-old woman with a medical history of human immunodeficiency virus (HIV) (CD4 count >600), diabetes mellitus, and hypertension presented to the emergency department following the sudden onset of tongue swelling, difficulty swallowing, mouth numbness, and a change in voice. Upon further questioning, the patient stated that she had experienced a similar episode a few months earlier, which had spontaneously resolved. Given that the patient had been taking enalapril, an ACE-I, for several months, she was treated with steroids and diphenhydramine (Benadryl) in the emergency department, before being admitted for further evaluation. Enalapril was discontinued at this time.
Given the history of HIV, to exclude other possible explanations, we obtained a contrast-enhanced CT scan of the neck. The CT scan revealed a large infiltrating hypoattenuated poorly circumscribed right peritonsillar masslike lesion with subtle enhancement extending into the right submandibular region, with associated compression of the oropharynx and hypopharynx, and left-to-right airway deviation (Fig 1). In addition, a well-defined enhancing lesion was also seen along the left foramen magnum, which was thought to represent a meningioma. Given the history of HIV, infection and neoplasm (especially lymphoma) were also placed in the imaging differential diagnosis. Angioedema was considered in the differential, though considered to be less likely, given the unilateral and somewhat focal nature of the abnormality. However, due to the ambiguity of the CT findings and to further evaluate the enhancing lesion along foramen magnum, a contrast-enhanced MR imaging of the neck was performed the next day, which now showed normal right peritonsillar and pharyngeal tissue, without evidence of fluid, mass, or abnormal enhancement (Fig 2A, -B).
Fig 1.
Axial contrast-enhanced CT scan of the neck demonstrates a hypoattenuated poorly circumscribed right peritonsillar/parapharyngeal masslike lesion, with associated compression of the oropharynx and hypopharynx. The mass extends to the right submandibular region. In addition, there is mild edema involving the tongue bilaterally.
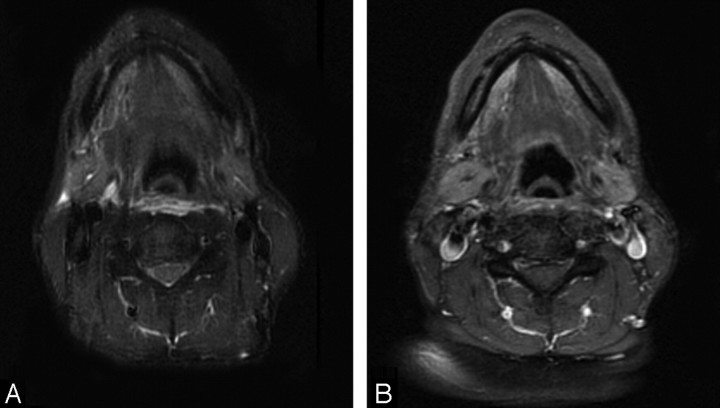
Fig 2.
A, Axial short tau inversion recovery image obtained 1 day after the previously discussed neck CT demonstrates no abnormal signal intensity at the level of the abnormality seen on CT. B, Similarly, postgadolinium T1 image demonstrates no abnormal enhancement or associated abnormality.
The patient was discharged the next day, with complete resolution of her symptoms. She was strictly instructed to avoid both ACE-I and angiotension receptor blockers in the future.
Discussion
Angioedema, also known as Quincke disease, is a transient swelling of the face, tongue, lips, extremities, and gastrointestinal tract.2 Potentially life-threatening as a result of airway compromise, many cases result from allergic reactions or sudden development of hypersensitivity reactions, though rare cases can be secondary to hereditary disorders, such as C1-esterase inhibitor deficiency.3 The most common cause of angioedema is considered to be ACE-Is, with an incidence of 0.1%–0.2% among those taking the medication. Angioedema is not thought to represent an immunologically mediated reaction or allergy, and ACE-Is are believed to result in angioedema through increased bradykinin activity.2 This bradykinin activity causes transient vasodilation, resulting in the extravasation of fluid into the extracellular space, thereby causing soft-tissue edema.2,4 Ostensibly through an immunologically mediated mechanism, several other drugs, such as rituximab, alteplase, fluoxetine, laronidase, lepirudin, and tacrolimus, can also cause angioedema.3 Nevertheless, ACE-Is are thought to account for up to 35% of all cases of angioedema and are a very widely used class of medications for hypertension and chronic heart failure, and should thus be considered high in the differential diagnosis of this disorder.2
Although patients are most likely to develop angioedema shortly after starting the medication, the reaction may take place long after the drug is first started, as in our patient.3 In fact, cases have been reported of angioedema occurring years after the drug was first started.1 The severity of the reaction can also vary, with some cases spontaneously resolving, whereas others rapidly progress to airway compromise. Treatment consists of stopping the medication, instituting steroids and antihistamines, and supportive care for airway protection.2 Given the risk of airway compromise, some patients may require intubation.1
A review of the literature suggests that ACE-I–induced angioedema primarily is localized in the head and neck, especially in the face, mouth, tongue, lips, and larynx.3 Intestinal/visceral angioedema is thought to be more rare in ACE-I–induced cases, being seen more often in organ transplant recipients and C1-esterase deficiency.4,5 The imaging characteristics of head and neck angioedema have not been described in the literature to any significant extent. One might expect to observe facial soft-tissue swelling, supraglottic edema, and pharyngeal/retropharyngeal free fluid and edema. Ostensibly, these abnormalities would tend to be diffuse and bilateral, though unilateral lingual edema on CT has been reported.2 Similarly, whereas the retropharynx is often not associated with this disorder, free fluid and soft-tissue fullness in the retropharynx on CT have also been described.6
Regarding our patient, the imaging differential diagnosis of this poorly circumscribed somewhat focal mass lesion in the right peritonsillar/parapharyngeal space with subtle enhancement is more apt to center on infection and neoplasm as the leading possibilities. Given the patient's immunocompromised status, infection was considered the most likely entity. Despite a lack of peripheral enhancement or evidence of loculation, peritonsillar/parapharyngeal phlegmon can have a very similar appearance. Although these infections are seen primarily in young adults, immunocompromised patients can develop peritonsillar infections at any age. Cross-sectional imaging typically demonstrates peritonsillar fluid collections, which can extend into the parapharyngeal space, as in this particular case.7 Alternatively, a number of vascular or neoplastic mass lesions could be considered in this location. For example, although lymphoma most often presents as a localized well-circumscribed enhancing mass, a more diffuse infiltrative appearance, as in our patient, can be seen in a minority of cases; however, most of these lesions still show some contrast enhancement.8 Although lymphadenopathy and multifocal disease are the norm, these features are not absolutely essentially for the diagnosis of lymphoma in this location. Other malignancies, though not consistent with the imaging features of our patient, in this location could include squamous cell carcinoma, sarcomas, and metastatic lesions. One interesting vascular mass lesion, which can have a very similar imaging appearance to that seen in this case, is a lymphangioma. Fluid-attenuated infiltrative masses with poorly defined borders and no enhancement on postcontrast images, lymphangiomas have been described in the right peritonsillar/parapharyngeal region, though they are rare in this location
Ultimately, from the standpoint of imaging alone, the unilateral focal nature of this process placed ACE-I–induced angioedema lower on the differential diagnosis. However, the diagnosis was ultimately supported by its rapid resolution following the discontinuation of enalapril. This case illustrates the protean and unusual manifestations of angioedema in the head and neck and the fact that no “classic” appearance of this entity has ever been described in the literature. Although unlikely to be unique or specific, this case helps us recognize the unexpected focal nature of imaging findings in angioedema, which might be underappreciated by clinicians and radiologists alike.
References
- 1.Oike Y, Ogata Y, Higashi D, et al. Fatal angioedema associated with enalapril. Intern Med 1993;32:308–10 [DOI] [PubMed] [Google Scholar]
- 2.Mlynarek A, Hagr A, Kost K. Angiotensin-converting enzyme inhibitor-induced unilateral tongue angioedema. Otolaryngol Head Neck Surg 2003;129:593–95 [DOI] [PubMed] [Google Scholar]
- 3.Bas M, Hoffmann TK, Kojda G. Evaluation and management of angioedema of the head and neck. Curr Opin Otolaryngol Head Neck Surg 2006;14:170–75 [DOI] [PubMed] [Google Scholar]
- 4.Shazad G, Korsten MA, Blatt C, et al. Angiotensin-converting enzyme (ACE) inhibitor-associated angioedema of the stomach and small intestine: a case report. Mt Sinai J Med 2006;73:1123–25 [PubMed] [Google Scholar]
- 5.De Backer AI, De Schepper AM, Vandevenne JE, et al. CT of angioedema of the small bowel. AJR Am J Roentgenol 2001;176:649–52 [DOI] [PubMed] [Google Scholar]
- 6.Altman KW, Woodring AJ, Pappano JE. Angioedema presenting in the retropharyngeal space in an adult. Am J Otolaryngol 1999;20:136–38 [DOI] [PubMed] [Google Scholar]
- 7.Alaani A, Griffiths H, Minhas SS, et al. Parapharyngeal abscess: diagnosis, complications, and management in adults. Eur Arch Otorhinolaryngol 2005;262:345–50 [DOI] [PubMed] [Google Scholar]
- 8.Huang SF, Zhang LF, He X, et al. Imaging features of Waldeyer's ring in non-Hodgkin's lymphoma and its clinical significance [in Chinese]. Ai Zheng 2004;23:1325–28 [PubMed] [Google Scholar]