Abstract
PURPOSE
In low- and middle-income countries, there has been an exponential increase in cancer incidence. According to the International Atomic Energy Agency, the biggest gap in radiotherapy availability and need is in Nigeria, where each machine serves an estimated 25.7 million people. This study aimed to characterize the barriers to radiotherapy and to identify areas for intervention.
METHODS
This was a cross-sectional study conducted at the University College Hospital in Ibadan, Nigeria, from June 2017 to August 2017. Demographic, sociocultural, and infrastructural factors relating to radiotherapy were collected through a questionnaire (N = 186). Ordinal logistic regression was used to identify the factors leading to delays in referral and delays in treatment initiation.
RESULTS
Patients traveled from 20 of Nigeria’s 36 states. The median age was 50 years (range, 19-79 years). The most common cancers treated were breast (37.5%), cervical (16.3%), head and neck (11.9%), and prostate (10.9%). In ordinal logistic regression, sociocultural factors, including the inability to pay (odds ratio [OR], 1.99; P = .034), a bad hospital experience (OR, 7.05; P = .001), and travel time (OR, 1.36; P = .001), increased the odds of referral delay to radiotherapy. In contrast, there was no significant relationship between time to treatment initiation and sociocultural factors including age, education, and inability to pay. Infrastructural barriers, including machine breakdown (OR, 2.92; P = .001), worker strikes (OR, 2.64; P = .001), and power outages (OR, 2.81; P = .022), increased the odds of treatment delay.
CONCLUSION
Although delays caused by patient factors are reported extensively, patients overcame these barriers in the hopes of curative treatment. However, staff and equipment malfunctions prevented patients from receiving timely radiotherapy. Policies aimed at addressing machine maintenance, health care worker satisfaction, and the aging power grid in Nigeria must be implemented in the future to strengthen the health care system to care for patients with cancer.
INTRODUCTION
In the past, cancer was often thought to be a problem of the developed world, but low- and middle-income countries (LMICs) now bear the majority of the global cancer burden.1,2 By 2030, 70% of newly reported cancers are expected to be in LMICs.3,4 Despite advances in cancer therapy, substantial gaps in survival rates exist between developed countries and LMICs.1 For all cancers, the case fatality rate is 1.6 times higher in LMICs than in higher-income countries.4 These countries together account for 80% of the disability-adjusted life-years lost to cancer globally, yet only 5% of the global resources for cancer are currently being spent there.1,4
Radiotherapy is a critical component of the multidisciplinary management of cancer. Using evidence-based estimates developed over the past 20 years, > 50% of all patients with cancer will need radiotherapy as part of their treatment.5,6 Multimodality management of cancer, including surgery, radiotherapy, and chemotherapy, is integral to the curative management of many cancers diagnosed worldwide, including breast, lung, head and neck, and cervical cancers.7 Unfortunately, there is a severe shortage of quality radiotherapy services in LMICs, especially in Africa. Nigeria is the most populous country in Africa, accounting for nearly one sixth of the continent’s population. According to the International Atomic Energy Agency, the biggest gap between radiotherapy availability and need is in Nigeria.8 In comparison with the developed world, where there is 1 megavoltage linear accelerator per 250,000 people, Nigeria has 1 accelerator per 25.7 million, a 100-fold difference.9
Previous studies often focused on the cultural and social factors leading to cancer treatment delays.10,11 However, the infrastructural barriers to effective radiotherapy delivery have not been studied in depth. Understanding the patient and facility factors associated with suboptimal delivery of available radiotherapy services in Nigeria is important to maximize care and access for patients with cancer. To further characterize these factors, a quantitative survey was distributed to patients undergoing radiotherapy at a major teaching hospital in Nigeria to evaluate the barriers impeding radiotherapy delivery and to identify areas for future development and intervention to reduce these barriers.
Context
Key Objective
What are the major factors that delay curative radiotherapy treatment of patients with cancer in Nigeria?
Knowledge Generated
Patients overcome significant sociocultural barriers to seek curative treatment in clinic but are met with inadequate infrastructure that continues to delay their treatment. Machine breakdowns, worker strikes, and power outages are 3 major factors that increase the odds of treatment delay.
Relevance
The health system is failing patients who overcome tremendous barriers to seek care and will require significant investment in infrastructure in the coming decades to care for the growing number of patients with cancer.
METHODS
This was a cross-sectional study conducted at the University College Hospital (UCH) in Ibadan, Oyo State, Nigeria, from June 2017 to August 2017. Patients who were 18 years of age or older attending the radiotherapy clinic at UCH or who were referred for treatment were recruited to complete a questionnaire. The questionnaire was administered verbally in English or in Yoruba with the assistance of a dialect concordant translator. The study received institutional review board approval from the University of Chicago and the University of Ibadan (UCIRB No.13304B, UI/IRC/02/0003).
The first part of the questionnaire (Data Supplement) included sections on demographics, educational background, ethnicity, and socioeconomic status. The second part of the questionnaire was adapted from 2 instruments used by oncology researchers in Nigeria12 and in Haiti,13 and assessed the personal and institutional factors that contributed to delays in treatment. The questionnaire was revised with input from the Department of Radiation and Cellular Oncology at the University of Chicago and public health researchers in Nigeria.
Patient characteristics were summarized using proportions and frequencies. The primary measures were delays in presentation, defined as length of time from diagnosis to clinic visit, and delays in initiation of radiotherapy, defined as length of time from clinic visit to treatment initiation. Univariate ordinal logistic regression was applied to the data to estimate the odds ratio (OR) of delay according to patient and infrastructural characteristics. ORs and 95% CIs were calculated for each variable.
Data were collected using paper questionnaires and were entered into Research Electronic Data Capture (REDCap) hosted at the University of Chicago.14 Statistical analyses and visualizations were completed in Stata 14.1 (StataCorp, College Station, TX) and R 3.3.2.
RESULTS
Study Population
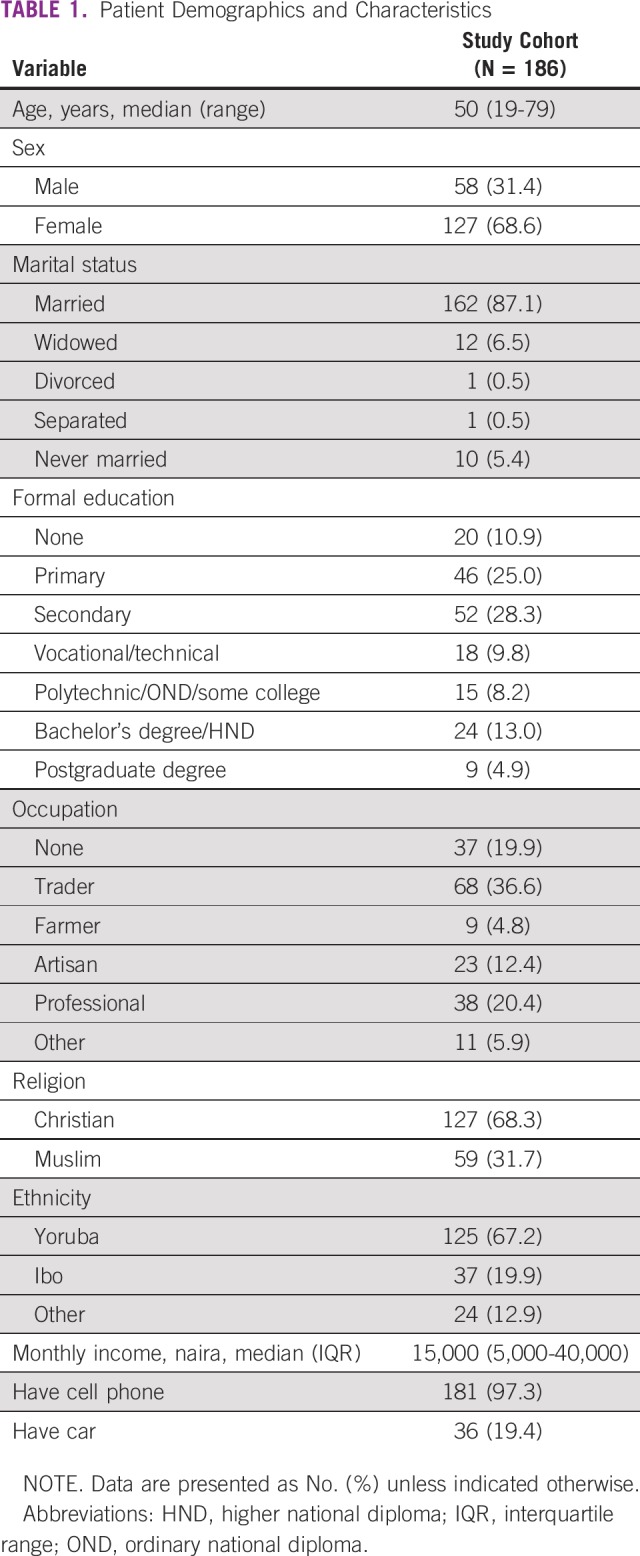
A convenient sample of 186 patients from UCH in Ibadan were interviewed in the study; over the study period (June-August 2017), 70 patients underwent radiotherapy treatment at the clinic. Participant characteristics are listed in Table 1. The median age was 50 years (range, 19-79 years). Patients were referred from a wide range of hospitals across 20 states in Nigeria, and 1 patient traveled internationally from the neighboring country of Benin Republic. The median monthly income of the patients was 15,000 naira (N; interquartile range, 5,000 to 40,000N), which converts to approximately 50 dollars per month. Cell phone ownership was high (97.3%), but only a minority (19.4%) owned a car for transport. Trust in medical professionals was high. On a 5-point scale from “never” to “always,” 91.8% of patients reported that in their opinion, “doctors (or nurses) always do everything possible for [their] cancer.” Furthermore, 92.5% of patients believed that it is possible to cure cancer.
TABLE 1.
Patient Demographics and Characteristics
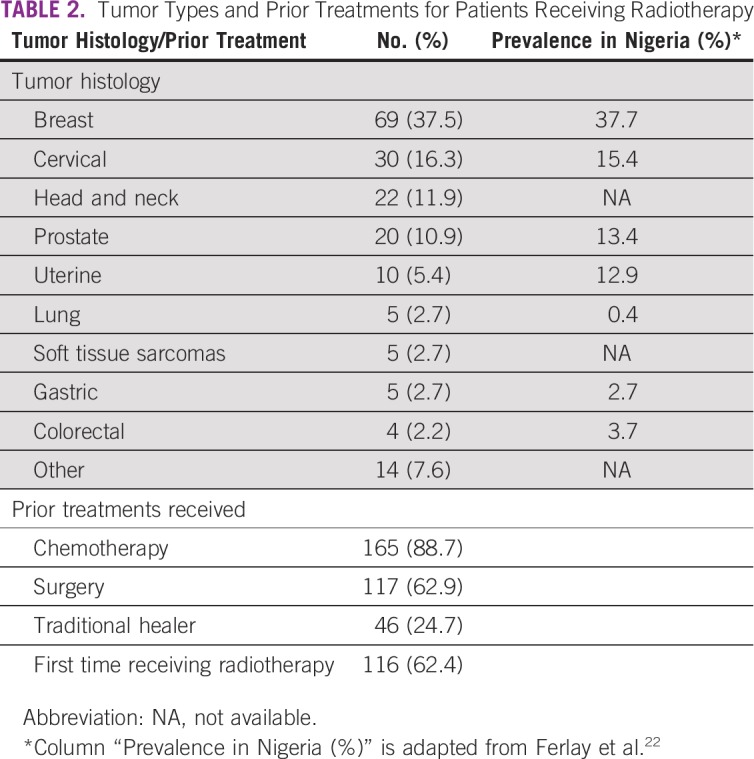
The most common cancers treated were breast (37.5%), cervical (16.3%), head and neck (11.9%), and prostate (10.9%). The prevalence of these indications was closely matched to the 5-year prevalence in Nigeria (Table 2). Radiotherapy was frequently used in combination with other treatments. A total of 88.7% of patients had received prior chemotherapy, and 62.9% had received prior surgery. In addition, some patients (24.7%) sought treatments with a traditional healer, outside of the hospital setting. More than one half (62.4%) of the patients surveyed were receiving radiotherapy for the first time, whereas 37.6% had received previous radiotherapy, either as part of their initial treatment before disease progression requiring a second course of radiotherapy, or as part of their first radiotherapy course before it was interrupted at another treatment site. The reported intent of radiotherapy was curative in 83.8% of cases and palliative in 4.6% of cases. A total of 11.6% of patients did not know the treatment intent of their radiotherapy. The proportion of patients reporting receiving curative-intent treatment was concordant with clinic records, in which treatment intent was curative for 86% of patients.
TABLE 2.
Tumor Types and Prior Treatments for Patients Receiving Radiotherapy
Factors Leading to Delays in Clinic Visit
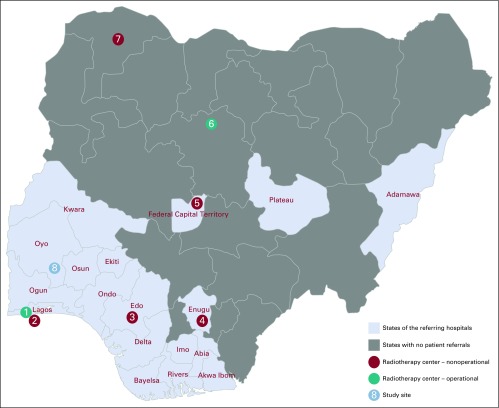
Specific sociocultural and infrastructural factors leading to delays in clinic visit and delays in radiotherapy treatment initiation were identified (Table 3). In ordinal logistic regression, sociocultural factors increased the odds of delay to radiotherapy clinic visit. These factors included the inability to pay (OR, 1.99; P = .034), a previous bad hospital experience (OR, 7.05; P = .001), and trying another treatment first (OR, 2.45; P = .034). Significant infrastructural factors included the time to reach the clinic (OR, 1.36; P < .001). A total of 41.9% of patients spent > 3 hours to reach the UCH radiotherapy clinic. Of these, 12.4% spent > 8 hours traveling. Patients traveled from 20 states and as far as 800 miles by road to receive radiotherapy (Fig 1).
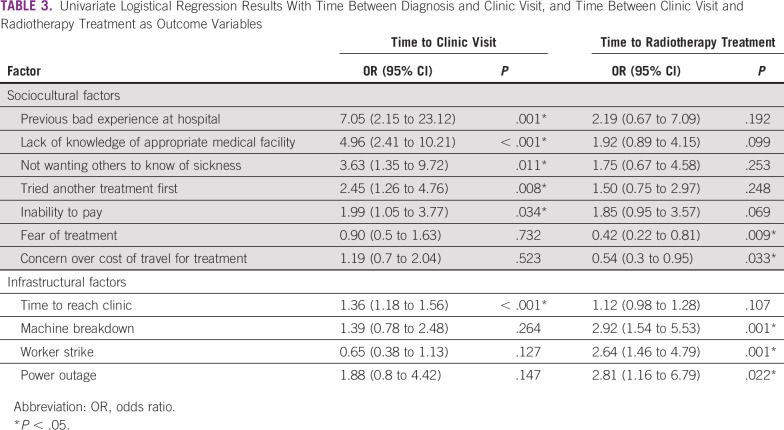
TABLE 3.
Univariate Logistical Regression Results With Time Between Diagnosis and Clinic Visit, and Time Between Clinic Visit and Radiotherapy Treatment as Outcome Variables
FIG 1.
Map of referring hospitals and radiotherapy sites in Nigeria. Of the functional radiotherapy centers in southern Nigeria at this time, the only site in addition to the study site was a private hospital, Eko Hospital. (1) Eko Hospital, Lagos State (cobalt-60); (2) Lagos University Teaching Hospital, Lagos State (linear accelerator [LINAC]); (3) University of Benin Teaching Hospital, Edo State (LINAC); (4) University of Nigeria Teaching Hospital, Enugu State (LINAC); (5) National Hospital Abuja, Federal Capital Territory (LINAC); (6) Ahmadu Bello University Teaching Hospital, Kaduna State (cobalt-60); (7) Usmanu Danfodiyo University Teaching Hospital, Sokoto State (LINAC); (8) Study site: University College Hospital, Oyo State (cobalt-60).
To reach UCH, most used public transportation (85.5%). All patients paid out of pocket for their treatment expenses, and 61% borrowed money from family and friends for their cancer treatments. Cancer care was delayed for 24.3% of patients because of an inability to pay, with an average delay of 7.6 weeks (standard deviation [SD], 14.0 weeks) in these cases. The 3 most commonly cited sociocultural barriers were, “I thought treatment might be too expensive” (54.8%), “I thought it was too expensive to travel to clinic” (53.8%), and “The clinic was too far away for me to travel to” (46.7%).
Factors Leading to Delays in Initiation of Radiotherapy
No significant relationship was observed between time to initiation of radiotherapy after consultation and sociocultural factors including age, education, use of a traditional healer, and inability to pay. In contrast, infrastructural barriers increased the odds of radiotherapy delay (Table 3). These factors included machine breakdowns (OR, 2.92; P = .001), worker strikes (OR, 2.64; P = .001), and power outages (OR, 2.81; P = .022).
Health care worker strikes delayed the treatment of 55.7% of patients, leading to a patient-reported average delay of 5.8 weeks (SD, 4.9 weeks). Machine breakdowns delayed the treatment of 68.6% of patients, for an average of 8.5 weeks (SD, 9.4 weeks). In comparison, relatively few patients (11.8%) reported treatment delays caused by power outages.
DISCUSSION
In this study, a cross-sectional survey was conducted at the only operational facility in a major teaching hospital in Nigeria to characterize the barriers experienced by patients receiving radiotherapy in a low-resource setting. Despite the presence of radiotherapy machines in Nigeria, the results here show that infrastructural factors limit the availability of radiotherapy delivery, driving major delays in patient care and curative treatment after diagnosis.
To our knowledge, no study to date had quantified patient and systems-level barriers to radiotherapy at a functioning radiotherapy center in an LMIC. At the time of this study, UCH was one of the 3 working radiotherapy facilities out of 8 in Nigeria (Fig 1). Because the other functional site in Lagos was a private hospital accessible only by a small number of patients with the resources to pay out-of-pocket expenses, the study site was the only functioning radiotherapy facility for the majority of patients in Nigeria. Despite recruiting from a single center, patients traveled from 20 different states to receive potentially “curative” treatment. A delay in the initiation of radiotherapy leads to an increased risk of cancer recurrence.15,16 Although radiotherapy machines are present in Nigeria, the wait times for these machines continue to increase.17 To our knowledge, this is the first study of its kind to identify system-level factors that contribute to delays in initiating quality cancer care, including radiotherapy, in the multidisciplinary management of patients with cancer in Nigeria.
Machine breakdown was a major contributor to treatment delay. The low number of functioning machines reflects a lack of routine maintenance in radiotherapy facilities and leads to measurable delays in patient care. The costs and logistics of maintenance are not factored into the establishment of radiotherapy centers in Nigeria.9 Although engineers are present to troubleshoot equipment issues, lack of machine parts and funds for repair hinder their progress. The overwhelming demand for the few functioning treatment machines in existing facilities increases the likelihood of machine breakdowns. Combined with the lack of backup parts and manufacturer maintenance centers in Africa, months may pass before a facility becomes operational again. In fact, patient-reported delays caused by machine breakdown averaged 8.5 weeks in this study.
Health care worker strikes are a common occurrence in the Nigerian health care system. In the period between 2013 to 2015, there were >8 documented strikes by doctors, nurses, and other allied health care workers.18 In radiotherapy, strikes contributed to patient delays averaging 5.8 weeks. The causes for worker strikes in Nigeria are complex, and they include dissatisfaction with salary, management, infrastructure, and hospital funding.18,19 These issues should be addressed in context to prevent delays in the diagnosis, treatment, and management of patients with potentially curable cancers.
Power outages reflect Nigeria’s ongoing problems with its electrical supply,20 and they present a significant challenge to machine uptime in radiotherapy. Hospitals often rely on diesel generators in times of power outage, further decreasing the treatment capacity of existing radiotherapy centers. Although power outage was a significant predictor of treatment delays, only 12% of patients reported it as a factor that delayed their treatment. This may be attributed to the transient nature of power outages in hospitals, allowing patients to be treated without months-long delays as caused by machine breakdowns and worker strikes.
The system-level challenges encountered by patients are reflective of the conditions present in all the referring hospitals in the 20 states represented in this study, and not at a single site. For instance, 4 of these states had radiotherapy facilities that were nonfunctional after equipment breakdown, leading to the referral of patients to the UCH facility. A previous study of 50 patients by Anakwenze et al12 showed that when the radiotherapy facility was inoperable at UCH, a median delay of 12 months between diagnosis and initiation of radiotherapy was reported, as well as a high proportion of patients who experienced machine breakdowns; this finding is consistent with the findings in this report. The survey of this expanded cohort over an operational radiotherapy period allowed assessment of the experiences of patients with cancer in a wide catchment area who came for radiotherapy.
As in other LMICs, cancer incidence in Nigeria continues to rise, and it is associated with a high mortality rate.21,22 These findings can be attributed to limitations in cancer screening programs, sociocultural barriers, delays in diagnosis resulting in advanced stage at treatment, and lack of access to timely treatments with chemotherapy, surgery, and radiotherapy.1,7,11,23-25
Sociocultural factors remained significant in this study, and they add to findings of previous studies documenting these delays in presentation and cancer diagnosis in similar settings.11,23-25 The inability to pay significantly increased the odds of delay to clinic visit in this study. The cost of cancer treatment in Nigeria remains a significant barrier to presentation; a full course of treatment with radiotherapy costs between N60,000 to N120,000 ($300 to $600) in public hospitals and may be as high as N500,000 ($1,667) in private facilities.9 Compared with the median monthly income of N15,000 ($50) in this patient population, it is unsurprising that a majority of patients borrowed money from family and friends for treatment. Similarly, the use of alternative healers increased the odds of delay to clinic, with 25% of patients visiting traditional healers before they were treated with radiotherapy. This is a failure of the Nigerian health system to provide quality care to vulnerable patients with cancer, who then often default to traditional healers.
Importantly, although sociocultural factors contributed to delays before patients presented to the radiotherapy clinic, there was no significant relationship between delays in receiving treatment after consultation and sociocultural factors including age, education, the use of a traditional healer, and inability to pay. These findings suggest that despite significant sociocultural challenges to clinic presentation, a proportion of patients with cancer overcome them with the goal of receiving curative treatment of their disease. To care for these patients and to provide them with adequate cancer care, resources should be devoted to solving the infrastructural problems that delay radiotherapy delivery, such as machine breakdowns, strikes, and power outages.
Radiotherapy is an essential component of cancer control programs and multidisciplinary cancer care. The projected rise in cancer incidence as the global burden of disease continues to shift to noncommunicable diseases will result in an increasing demand for radiotherapy services. Estimates showed that by 2020, 84 LMICs with existing radiotherapy access would need an additional 9,169 radiotherapy treatment machines, 12,149 radiation oncologists, 9,915 medical physicists, and 29,140 radiation therapy technologists, in addition to the capacity that would need to be developed in 55 LMICs with no current radiotherapy facilities.26 In their commentary on Nigeria, Irabor et al9 describe the decay of radiotherapy resources because of poor maintenance, funding, and health policies. To build sustainable radiotherapy treatment capacity in LMICs, private and public efforts in the future must take these lessons into account. Organizations must concentrate efforts on supporting existing urban centers with radiotherapy capacity, maintaining high system uptime. In LMICs, radiotherapy must be integrated into a comprehensive cancer program that targets prevention,27 timely diagnosis, and biomarker-based treatments of potentially curable aggressive early-onset cancers, such as breast cancer,28 so that patients diagnosed with curable cancer might have a chance at survival.
This study has several limitations. It was cross sectional in nature, and patients were asked to recall the months and years of their diagnosis, referral, and treatment, which may have led to inaccuracies in the reported time intervals. Patients with cancer, particularly in rural areas, who failed to present to the hospital for diagnosis and treatment are not represented in this sample. Furthermore, the total number of patients presenting in clinic who were eligible to interview over the recruitment period was not reliably tracked. Finally, the study was conducted at 1 institution in southwest Nigeria and may not be applicable to all of Nigeria or to other LMICs. However, as one of the 3 functioning radiotherapy facilities at the time of the study, the catchment area included patients from 20 of Nigeria’s 36 states. Furthermore, the incidence of tumor types reflected the overall prevalence of each site in Nigeria,22 providing evidence that these results are generalizable and could be applicable to the broader population.
Studies of the barriers to cancer care in LMICs often focus on personal sociocultural barriers that prevent patients from presenting to the hospital. The findings here indicate that for radiotherapy, system-level barriers, including infrastructural breakdowns in power, personnel, and equipment, are the major drivers of treatment delay after diagnosis in Nigeria. The health system is failing patients who overcome tremendous barriers to seek treatment and will require significant investments in its infrastructure for quality cancer care in the coming decades. As the burden of cancer continues to grow, it is now more important than ever to address radiotherapy access as part of efforts to strengthen the health care delivery system for cancer in Nigeria and other LMICs.
ACKNOWLEDGMENT
We thank our translator, Modupe Adenusi; the Healthy Life Foundation; the University of Chicago Center for Global Health; and the staff in the UCH Radiotherapy Department for their logistical and administrative support.
Presented at the American Society for Radiation Oncology Annual Meeting, San Antonio, TX, October 21-24, 2018, and at the Consortium of Universities for Global Health Annual Conference, New York, NY, March 15-18, 2018.
Supported by the University of Chicago Pritzker School of Medicine Summer Research Program; National Institutes of Health Grants No. NIDDK T35DK062719-30, P30DK42086; NIH D43 TW009112; NIH CTSA UL1 TR000430; and the Breast Cancer Research Foundation.
AUTHOR CONTRIBUTIONS
Conception and design: Jim Leng, Atara I. Ntekim, Chidinma P. Anakwenze, Daniel W. Golden, Olufunmilayo I. Olopade
Collection and assembly of data: Jim Leng, Olufunmilayo I. Olopade
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/site/misc/authors.html.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Daniel W. Golden
Stock and Other Ownership Interests: RadOnc Questions, HemOnc Review
Open Payments Link: https://openpaymentsdata.cms.gov/physician/937714/general-payments
Olufunmilayo I. Olopade
Employment: CancerIQ (I)
Leadership: CancerIQ
Stock and Other Ownership Interests: CancerIQ, Tempus
Research Funding: Novartis (Inst), Roche/Genentech (Inst)
Other Relationship: Tempus, Color Genomics, Roche/Genentech, Bio Ventures for Global Health
Uncompensated Relationships: Healthy Life for All Foundation, (Healthy Life for All Foundation, https://openpaymentsdata.cms.gov/physician/olopade)
No other potential conflicts of interest were reported.
REFERENCES
- 1.Farmer P, Frenk J, Knaul FM, et al. Expansion of cancer care and control in countries of low and middle income: A call to action. Lancet. 2010;376:1186–1193. doi: 10.1016/S0140-6736(10)61152-X. [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine (US) Committee on Cancer Control in Low- and Middle-Income Countries . Cancer Control Opportunities in Low- and Middle-Income Countries. Washington, DC: National Academies Press; 2007. [PubMed] [Google Scholar]
- 3.Boyle P, Levin B. (eds): World Cancer Report 2008. IARC Publications, https://publications.iarc.fr/Non-Series-Publications/World-Cancer-Reports/World-Cancer-Report-2008 [Google Scholar]
- 4.Economist Intelligence Unit Breakaway: The global burden of cancer— challenges and opportunities. http://graphics.eiu.com/upload/eb/EIU_LIVESTRONG_Global_Cancer_Burden.pdf
- 5.Borras JM, Barton M, Grau C, et al. The impact of cancer incidence and stage on optimal utilization of radiotherapy: Methodology of a population based analysis by the ESTRO-HERO project. Radiother Oncol. 2015;116:45–50. doi: 10.1016/j.radonc.2015.04.021. [DOI] [PubMed] [Google Scholar]
- 6.Delaney G, Jacob S, Featherstone C, et al. The role of radiotherapy in cancer treatment: Estimating optimal utilization from a review of evidence-based clinical guidelines. Cancer. 2005;104:1129–1137. doi: 10.1002/cncr.21324. [DOI] [PubMed] [Google Scholar]
- 7.Atun R, Jaffray DA, Barton MB, et al. Expanding global access to radiotherapy. Lancet Oncol. 2015;16:1153–1186. doi: 10.1016/S1470-2045(15)00222-3. [DOI] [PubMed] [Google Scholar]
- 8.Abdel-Wahab M, Bourque J-M, Pynda Y, et al. Status of radiotherapy resources in Africa: An International Atomic Energy Agency analysis. Lancet Oncol. 2013;14:e168–e175. doi: 10.1016/S1470-2045(12)70532-6. [DOI] [PubMed] [Google Scholar]
- 9.Irabor OC, Nwankwo KC, Adewuyi SA. The stagnation and decay of radiation oncology resources: Lessons from Nigeria. Int J Radiat Oncol Biol Phys. 2016;95:1327–1333. doi: 10.1016/j.ijrobp.2016.04.026. [DOI] [PubMed] [Google Scholar]
- 10.Ukwenya AY, Yusufu LMD, Nmadu PT, et al. Delayed treatment of symptomatic breast cancer: The experience from Kaduna, Nigeria. S Afr J Surg. 2008;46:106–110. [PubMed] [Google Scholar]
- 11.Pruitt L, Mumuni T, Raikhel E, et al. Social barriers to diagnosis and treatment of breast cancer in patients presenting at a teaching hospital in Ibadan, Nigeria. Glob Public Health. 2015;10:331–344. doi: 10.1080/17441692.2014.974649. [DOI] [PubMed] [Google Scholar]
- 12.Anakwenze CP, Ntekim A, Trock B, et al. Barriers to radiotherapy access at the University College Hospital in Ibadan, Nigeria. Clin Transl Radiat Oncol. 2017;5:1–5. doi: 10.1016/j.ctro.2017.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sharma K, Costas A, Damuse R, et al. The Haiti Breast Cancer Initiative: Initial findings and analysis of barriers-to-care delaying patient presentation. J Oncol. 2013;2013:206367. doi: 10.1155/2013/206367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang J, Barbera L, Brouwers M, et al. Does delay in starting treatment affect the outcomes of radiotherapy? A systematic review. J Clin Oncol. 2003;21:555–563. doi: 10.1200/JCO.2003.04.171. [DOI] [PubMed] [Google Scholar]
- 16.Chen Z, King W, Pearcey R, et al. The relationship between waiting time for radiotherapy and clinical outcomes: A systematic review of the literature. Radiother Oncol. 2008;87:3–16. doi: 10.1016/j.radonc.2007.11.016. [DOI] [PubMed] [Google Scholar]
- 17.Grover S, Xu MJ, Yeager A, et al. A systematic review of radiotherapy capacity in low- and middle-income countries. Front Oncol. 2015;4:380. doi: 10.3389/fonc.2014.00380. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4302829/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oleribe OO, Ezieme IP, Oladipo O, et al. Industrial action by healthcare workers in Nigeria in 2013-2015: An inquiry into causes, consequences and control—A cross-sectional descriptive study. Hum Resour Health. 2016;14:46. doi: 10.1186/s12960-016-0142-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adebimpe W, Owolade O, Adebimpe M. Health worker’s perception of the use of strikes as a tool for dispute resolution in Lagos State, Nigeria. J Soc Sci Public Policy. 2010;2:19–23. [Google Scholar]
- 20.Aliyu AS, Ramli AT, Saleh MA. Nigeria electricity crisis: Power generation capacity expansion and environmental ramifications. Energy. 2013;61:354–367. [Google Scholar]
- 21.Jedy-Agba E, Curado MP, Ogunbiyi O, et al. Cancer incidence in Nigeria: A report from population-based cancer registries. Cancer Epidemiol. 2012;36:e271–e278. doi: 10.1016/j.canep.2012.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 23.Smith RA, Caleffi M, Albert U-S, et al. Breast cancer in limited-resource countries: Early detection and access to care. Breast J. 2006;12:S16–S26. doi: 10.1111/j.1075-122X.2006.00200.x. [DOI] [PubMed] [Google Scholar]
- 24.Ajape AA, Babata A, Abiola OO. Knowledge of prostate cancer screening among native African urban population in Nigeria. Nig Q J Hosp Med. 2010;20:94–96. doi: 10.4314/nqjhm.v20i2.58044. [DOI] [PubMed] [Google Scholar]
- 25.Nwankwo KC, Aniebue UU, Aguwa EN, et al. Knowledge attitudes and practices of cervical cancer screening among urban and rural Nigerian women: A call for education and mass screening. Eur J Cancer Care (Engl) 2011;20:362–367. doi: 10.1111/j.1365-2354.2009.01175.x. [DOI] [PubMed] [Google Scholar]
- 26.Datta NR, Samiei M, Bodis S. Radiation therapy infrastructure and human resources in low- and middle-income countries: Present status and projections for 2020. Int J Radiat Oncol Biol Phys. 2014;89:448–457. doi: 10.1016/j.ijrobp.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 27.Jemal A, Bray F, Forman D, et al. Cancer burden in Africa and opportunities for prevention. Cancer. 2012;118:4372–4384. doi: 10.1002/cncr.27410. [DOI] [PubMed] [Google Scholar]
- 28.Pitt JJ, Riester M, Zheng Y, et al. Characterization of Nigerian breast cancer reveals prevalent homologous recombination deficiency and aggressive molecular features Nat Commun 94181.2018[Erratum: Nat Commun 20191] [DOI] [PMC free article] [PubMed] [Google Scholar]