Abstract
Objective Historical results of arthroplasty of the first metatarsophalangeal joint (1MTP) are relatively poor; however, improvements in the understanding of the normal foot biomechanics, implant materials and design currently make arthroplasty a reasonable option in appropriately selected patients. The present study aimed to compare the clinical and radiographic results of 1MTP arthrodesis and arthroplasty in the treatment of hallux rigidus and to present a rationale for patient selection for arthroplasty.
Methods A total of 36 patients (38 feet) with hallux rigidus submitted to surgery (12 arthrodesis and 26 arthroplasties) were prospectively included in the study. Pain was assessed using the visual analogue scale (VAS) and the functional status was assessed using the American Orthopedic Foot and Ankle Society Hallux Metatarsophalangeal-Interphalangeal (AOFAS-HMI) scale. Complications and radiographic results were also analyzed, and survival rates were calculated for both procedures.
Results All of the patients reported significant improvement in pain and functional status after surgery. Patients submitted to arthroplasty had better functional results on the AOFAS-HMI scale (89.7 versus 65.7 points; p < 0.001) and better pain relief (VAS 1.6 versus 3.9 points; p = 0.002) when compared with the group submitted to arthrodesis. There was one case of infection in the arthroplasty group and 2 cases of pseudarthrosis in the arthrodesis group.
Conclusion Arthrodesis provides pain relief and satisfactory results but alters the biomechanics of gait. Like arthrodesis, arthroplasty improves pain significantly, being a more physiological alternative to preserve the biomechanics of the foot. While the two surgical methods yielded good clinical results, selected patients submitted to arthroplasty had better clinical scores and lower revision rates.
Keywords: hallux rigidus, arthroplasty, arthrodesis, comparative study, joint replacement
Introduction
Hallux rigidus is a degenerative disorder of the first metatarsophalangeal joint (1MTP), with a prevalence of 2.5% in people > 50 years old, affecting preferentially women (2:1). 1 2 The cause is considered to be idiopathic, although almost two thirds of patients have a positive familiar history and 79% have bilateral involvement. This condition is also frequently associated with other diseases such as hallux valgus interphalangeus and metatarsus adductus. 1 3 Clinically, it is characterized by pain, stiffness and functional limitation, particularly with 1MTP dorsiflexion. Physical findings are the presence of a dorsal prominence above the first metatarsophalangeal joint correlating with dorsal metatarsal head bone spur and associated inflammation, swelling, tenderness to palpation and decreased range of motion (ROM) of the 1MTP. 4
The most common classification of hallux rigidus was first described by Coughlin et al and is based on clinical and radiographic findings. 5 Nonoperative treatment for mild cases (stages I and II) provides clinical improvement, and consists of oral or topical nonsteroidal anti-inflammatory medications, intra-articular injection of corticosteroids or sodium hyaluronate, supportive orthotics, physical therapy and lifestyle modifications. Surgical treatment is indicated when conservative treatment fails and in later stages of the disease. It consists of joint debridement and synovectomy, cheilectomy, and decompression osteotomy in early stages and hemiarthroplasty, total joint arthroplasty, resurfacing and arthrodesis in advanced stages. 3 6
Arthrodesis of the 1MTP joint was first described by Broca in 1852 and is still considered the gold standard treatment for hallux rigidus stage III and IV. It allows pain relief and results from long-term studies have shown favorable patient outcomes. 5 7 8 Arthroplasty of the 1MTP was first developed in the 1950s as an alternative to arthrodesis to preserve joint motion and normal foot biomechanics. Several different implants have been developed, but the initial results were disappointing. 9 10 More recent improvements in the understanding of the normal biomechanics of the foot, implant materials and design, however, have yielded better results and currently make them a reasonable alternative to 1MTP fusion. 11 12 13
The aim of the present study was to compare the clinical results of 1MTP arthrodesis and arthroplasty in the treatment of hallux rigidus and to present a rationale for patient selection for arthroplasty.
Material and Methods
Study Design and Participants
Between 2007 and 2015, 38 feet in 36 patients with stage III and IV hallux rigidus underwent surgical treatment. A total of 12 patients were submitted to arthrodesis, and 24 patients (26 feet) underwent total 1MTP arthroplasty. Exclusion criteria were active infection/ inflammation, severe bone loss or rapid joint destruction, avascular necrosis, 1MTP joint instability, Charcot neuroarthropathy, and metal allergy/intolerance. Patients with deviation of the metatarsophalangeal axis ( hallux varus or valgus) , abnormalities of the foot arch (pes planus or cavus ) or retraction of the Achilles-calcaneal-plantar system were not selected for arthroplasty and underwent arthrodesis. Only patients with a minimum follow-up of 2 years were included in the study.
The work presented in the pesent study was approved by the local ethics committee and has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Surgical Procedures and Postoperative Care
All of the patients were operated by the same surgeon in the same institution. Surgery was performed under either general or epidural anesthesia, with the patient lying supine on the operating table. A bump was used under the ipsilateral hip to internally rotate the lower limb to a neutral angle and a thigh tourniquet was used for exsanguination. All of the patients were given preoperative prophylactic antibiotic, which was maintained for the first 24 hours after surgery.
First metatarsophalangeal joint arthrodesis was performed either with a dorsal plate and screws (seven patients) or with crossed screws alone (five patients) as previously described. 14 15 16
For 1MTP arthroplasty, the same prosthesis was used (Metis, Newdeal SA Integra Lifesciences ILS, Plainsboro Township, NJ, USA). This is a 3-component, noncemented hydroxapatite coated, nonrestrictive, titanium modular prosthesis. A medial incision was made from the middle of the phalanx to the middle of the metatarsal to expose the first metatarsal-phalangeal joint. To prepare the articular surfaces, the osteophytes and cartilage were removed and a bunionectomy (when necessary) was performed. After determining the size of the metatarsal component, the metatarsus was cut using a metatarsal cutting guide and the implant was tested. Importantly, whenever the patient had index plus, the metatarsal cut was performed to reduce its length to the same length of the second metatarsal (index plus minus). The phalanx was then prepared with reamers and the appropriate sized implant was chosen and tested. Range of motion and laxity of the test implants was checked to choose the inlay thickness. Fluoroscopy was used to assess the correct alignment of the different components. The final phalanx, metatarsal and inlay implants were inserted under press-fit ( Fig. 1 ). A preliminary report of these results has been published previously. 17
Fig. 1.

Intraoperative photograph of 1MTP replacement showing correct fit of the implants.
After surgery, all of the patients underwent thromboprophylaxis. The suture material was removed 15 days after surgery. The group submitted to arthrodesis started partial weight-bearing at 2 weeks and full weight-bearing at 6 weeks. The group submitted to arthroplasty initiated partial weight-bearing with a Barouk-type shoe at 2 weeks and full weight-bearing at 6 weeks.
Outcome Variables
Follow-up time, time until revision, the age of the patients at surgery, and complications were recorded. Patients were seen at 2 and 6 weeks, 3 months, 6 months and yearly. Patients submitted to arthrodesis were discharged after treatment completion without complications while patients submitted to arthroplasty were seen yearly to check for clinical or radiographic signs of complications.
Functional evaluation was performed using the American Orthopaedic Foot and Ankle Society Hallux Metatarsophalangeal-Interphalangeal Score (AOFAS-HMI) preoperatively and at the final follow-up visit. The AOFAS-HMI measures pain, function and alignment on a scale of 1 to 100 points. Pain assessment was performed using the visual analogue scale (VAS) preoperatively and at the final follow-up visit. The VAS score measures pain on a scale of 1 to 10, with 0 indicating the absence of pain and 10 indicating the worst pain imaginable.
To assess implant alignment and evidence of radiolucent lines, standard AP and lateral radiographs at the latest follow-up were obtained. A radiolucent line > 1 mm on any of prosthesis interfaces was considered to be loosening of the implant.
Statistical Analysis
IBM SPSS Statistics for Windows, Version 23 (IBM Corp. Armonk, NY, USA), was used for statistical analysis. Descriptive statistics were calculated. Means were calculated for normally distributed data. The chi-squared test, the t -test and the Mann-Whitney U-test, depending on the variable analyzed, were used to compare both groups. Survival curves were calculated for both groups of patients with revision surgery as the endpoint, using the Kaplan-Meier method with a 95% confidence interval (CI). The criterion for statistical significance was set at p < 0.05 for all comparisons.
Results
There was a predominance of women in both groups (83.3% in the arthrodesis and 61.15% in the arthroplasty group, p < 0.05). The mean age was 57.6 years old (50–70 years old) in the arthrodesis group, and 64.3 years old (56–83 years old) in the arthroplasty group ( p = 0.005). The mean follow-up time was 40.1 months (31–70 months) and 80.7 months (26–110 months), respectively ( Table 1 ).
Table 1. Demographics of patients submitted to arthrodesis and to arthroplasty.
| Arthrodesis ( n = 12) | Arthroplasty ( n = 26) | p - value | |
|---|---|---|---|
| Gender | 10 female (83.3%) 2 male (16.7%) |
16 female (61.15%) 10 male (38.46%) |
0.179 |
| Age | 57.6 (50–70) | 63.5 (59–83) | 0.005 |
| Follow-up | 40.1 (31–70) | 80.7 (26–110) | <0.001 |
Clinical scores improved in patients in both groups. The AOFAS-HMI score improved from an average of 40.2 to 65.7 points in the arthrodesis group ( p < 0.001) and from an average of 43.2 to 89.7 points ( p < 0.001) in the arthroplasty group. The AOFAS-HMI scores at the last follow-up were, however, higher in the arthroplasty than in the arthrodesis group ( p < 0.001). The VAS scores also improved significantly in the arthrodesis (7.8 to 3.9 points, p < 0.001) and in the arthroplasty (8.0 to 1.6 points, p < 0.001) groups. The VAS scores at the last follow-up were significantly lower in the arthroplasty than in the arthrodesis group (1.6 points versus 3.9 ; p = 0 0.002) ( Table 2 ).
Table 2. Pre- and post- operative AOFAS-HMI and VAS scores in patients submitted to arthrodesis and to arthroplasty.
| SCORES | Arthrodesis ( n = 12) | Arthroplasty ( n = 26) | p - value * | ||||
|---|---|---|---|---|---|---|---|
| Preop | Postop | p - value | Preop | Postop | p - value | ||
| AOFAS-HMI | 40.2 (37–50) | 65.7 (55–77) | < 0.001 | 43.2 (34.1–53.1) | 89.7 (67–100) | < 0.001 | < 0.001 |
| VAS | 7.8 (5–10) | 3.9 (0–6) | < 0.001 | 8.0 (5–10) | 1.6 (0–3) | < 0.001 | .002 |
Abbreviations: AOFAS-HMI, American Orthopedic Foot and Ankle Society Hallux Metatarsophalangeal-Interphalangeal score; VAS, visual analogue scale.
*(arthrodesis versus arthroplasty at last follow-up).
There were 3 complications in the arthrodesis group: 1 (5.5%) case of transfer metatarsalgia and 2 (16.6%) cases of nonunion, which were submitted to a fusion revision with autograft. One nonunion case occurred in a fusion using crossed screws, while the other occurred in a fusion using a dorsal plate. There was one case of early wound infection in the arthroplasty group that was managed with antibiotics and wound care. No other complications were recorded, such as neurovascular injury or loosening of the prosthesis.
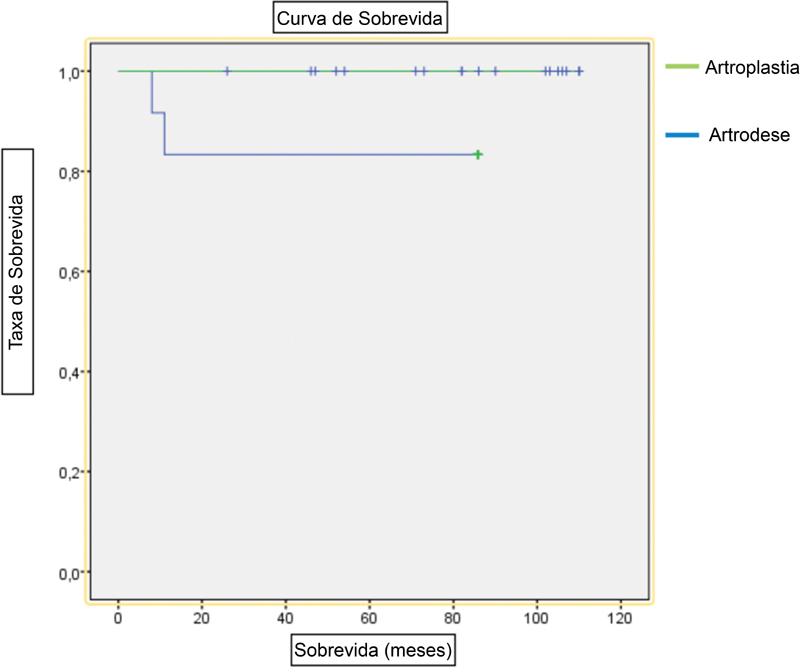
With revision surgery as the endpoint, the prosthesis survival rate was 100% and the arthrodesis survival rate was 83% ( Fig. 2 ).
Fig. 2.
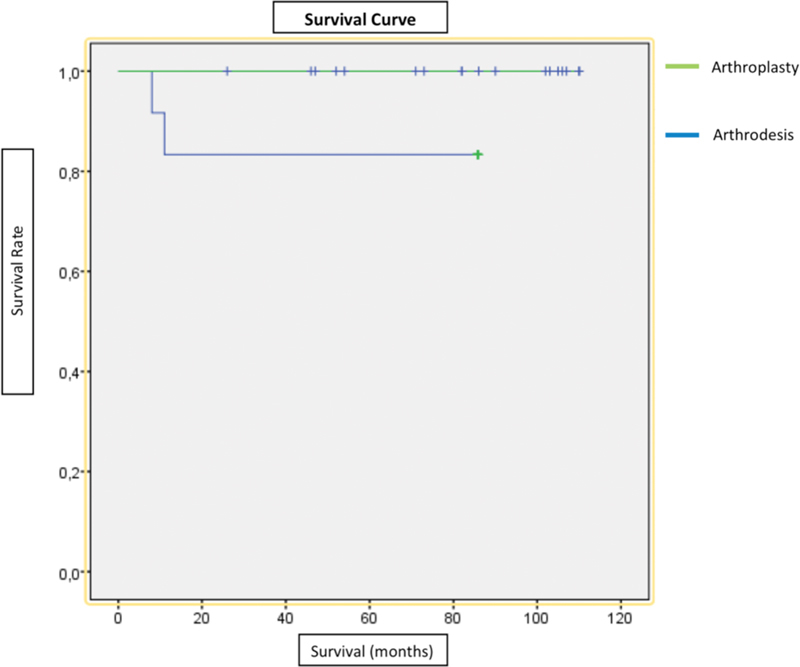
Survival curves of arthroplasty and arthrodesis.
Figs. 3 and 4 illustrate the preoperative and postoperative cases of arthrodesis and arthroplasty. Video 1 shows a patient with a bilateral arthroplasty.
Fig. 3.

Pre- and postoperative X-ray images of a 62 year old man with hallux rigidus submitted to arthrodesis with crossed-screws. ( A ) Preoperative standing anteroposterior X-ray; ( B ) Preoperative standing lateral X-ray; ( C ) Postoperative standing AP X-ray 2 years after surgery; ( D ) Postoperative standing lateral X-ray 2 years after surgery.
Fig. 4.

Pre- and postoperative X-ray images of a 58 year old woman with hallux rigidus submitted to 1MTP arthroplasty. ( A ) Preoperative standing anteroposterior X-ray; ( B ) Preoperative standing lateral X-ray; ( C ) Postoperative standing anteroposterior X-ray 3 years after surgery; ( D ) Postoperative standing lateral X-ray 3 years after surgery.
Video 1
Video of a 54 year old male submitted to a bilateral 1MTP arthroplasty.
Discussion
Hallux rigidus affects ∼ 10% of the population, with a higher prevalence in women between the age of 60 and 70 years old. 6 18 First metatarsophalangeal joint arthrodesis eliminates 1MTP movement, decreasing pain and stabilizing the medial foot column, and still is the gold standard treatment for patients with advanced arthritis. 19 20 21 This, however, is not exempt of complications. Approximately 10% of fusion patients will develop nonunions, requiring further surgeries, 22 23 and some patients will continuously complain of foot stiffness and altered gait patterns, with decreased step length and loss of ankle plantar flexion at toe-off on the fused foot. 18 This is particularly important in patients with bilateral hallux rigidus , in which a bilateral fusion will alter normal stride and gait biomechanics.
First metatarsophalangeal joint arthroplasty has the potential to maintain foot gait and biomechanics closer to the physiological. While the results with previous MTP implants were disappointing, a better understanding of foot biomechanics has allowed the development of newer implants with better clinical results and survival rates. A meta-analysis including 3049 1MTP replacements with a mean follow of 61 months has reported a 94.5% satisfaction rate after these procedures. 12
In the present study, a significant improvement in pain, functional and clinical scores were found in both groups, including in the arthroplasty group. This is in agreement with some of the most recent literature on 1MTP joint replacement. 6 18 19 24 While a few studies have compared the results of 1MTP arthrodesis and arthroplasty, most of them analyze prosthesis from previous generations, which have been associated with poorer results. 12 24 25 26 27 28 In the present study, however, patients in the arthroplasty group had better clinical and functional results than those submitted to fusion.
The complication rate was also lower in the arthroplasty than in the arthrodesis group (5.5% versus 22.1%). A total of 16.6% of the patients submitted to fusion developed nonunions, requiring further revision surgery. This nonunion rate is equivalent to previously published reports using similar techniques with plate or screw fusion. 12 19 22 While other authors have reported relevant malunion rates after fusion, 29 no cases were seen in the present study. Infection is also a major concern when performing an arthroplasty. In the present study, the only complication in the arthroplasty group was an infection, which is in agreement with previous reports. 24
The superior clinical results found here possibly reflect the careful patient selection for arthroplasty. It is the opinion of the author that patients selected for arthroplasty should not have a metatarsus primus elevatus, retraction of the achilles-calcaneal-plantar system and any malalignment of the first radius of the foot. Special attention must also be paid to the length of the first ray; in patients with index plus, and to avoid overstressing the arthroplasty, the first metatarsal length should be shortened to plus-minus to preserve the normal biomechanics of the foot. Only in these cases, in which a structural and anatomical adaptation of the prosthesis was possible, arthroplasties were performed, with the remaining cases being selected for fusion.
The main strengths of the present paper are the fact that it is a comparative study in which all of the patients were operated by the same surgeon, who used a standardized technique, and the fact that he did not participate in the data collection and, therefore, did not influence data analysis. Additionally, the follow-up of the patients in the arthroplasty was relatively high (mean 6.75 years, maximum 9.17 years), and no additional complications were identified despite close clinical and radiographic evaluation.
The present study also has some limitations, since it is retrospective in nature and the sample is relatively small. Furthermore, patients were not randomly assigned to each group and were selected to undergo prosthesis or fusion depending on first ray alignment and patient characteristics. As aforementioned, it is the opinion of the author that this patient selection is key to the success of this technique.
Conclusions
In conclusion, the two surgical methods used had satisfactory results. First metatarsophalangeal joint arthroplasty demonstrated superior clinical and functional results, being a good alternative for suitable candidates. However, a larger sample and longer follow-up are necessary to obtain conclusive results.
Conflito de Interesses Os autores declaram não haver conflito de interesses.
Estudo conduzido no Departamento de Ortopedia, Centro Hospitalar do Porto, Hospital de Santo António, Porto, Portugal.
Study conducted at Department of Orthopedics, Centro Hospitalar do Porto, Hospital de Santo António, Porto, Portugal.
Referências
- 1.Coughlin M J, Shurnas P S. Hallux rigidus: demographics, etiology, and radiographic assessment. Foot Ankle Int. 2003;24(10):731–743. doi: 10.1177/107110070302401002. [DOI] [PubMed] [Google Scholar]
- 2.Ho B, Baumhauer J. Hallux rigidus. EFORT Open Rev. 2017;2(01):13–20. doi: 10.1302/2058-5241.2.160031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hamid K S, Parekh S G. Clinical Presentation and Management of Hallux Rigidus. Foot Ankle Clin. 2015;20(03):391–399. doi: 10.1016/j.fcl.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 4.Polzer H, Polzer S, Brumann M, Mutschler W, Regauer M. Hallux rigidus: Joint preserving alternatives to arthrodesis - a review of the literature. World J Orthop. 2014;5(01):6–13. doi: 10.5312/wjo.v5.i1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coughlin M J, Shurnas P S. Hallux rigidus. Grading and long-term results of operative treatment. J Bone Joint Surg Am. 2003;85(11):2072–2088. [PubMed] [Google Scholar]
- 6.Dülgeroğlu T C, Metineren H. Treatment of End-Stage Hallux Rigidus Using Total Joint Arthroplasty: A Short-Term Clinical Study. J Foot Ankle Surg. 2017;56(05):1047–1051. doi: 10.1053/j.jfas.2017.05.017. [DOI] [PubMed] [Google Scholar]
- 7.Beertema W, Draijer W F, van Os J J, Pilot P. A retrospective analysis of surgical treatment in patients with symptomatic hallux rigidus: long-term follow-up. J Foot Ankle Surg. 2006;45(04):244–251. doi: 10.1053/j.jfas.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 8.DeFrino P F, Brodsky J W, Pollo F E, Crenshaw S J, Beischer A D. First metatarsophalangeal arthrodesis: a clinical, pedobarographic and gait analysis study. Foot Ankle Int. 2002;23(06):496–502. doi: 10.1177/107110070202300605. [DOI] [PubMed] [Google Scholar]
- 9.Konkel K F, Menger A G, Retzlaff S A. Mid-term results of Futura hemi-great toe implants. Foot Ankle Int. 2008;29(08):831–837. doi: 10.3113/FAI.2008.0831. [DOI] [PubMed] [Google Scholar]
- 10.Swanson A B, Lumsden R M, Swanson G D. Silicone implant arthroplasty of the great toe. A review of single stem and flexible hinge implants. Clin Orthop Relat Res. 1979;(142):30–43. [PubMed] [Google Scholar]
- 11.Brewster M. Does total joint replacement or arthrodesis of the first metatarsophalangeal joint yield better functional results? A systematic review of the literature. J Foot Ankle Surg. 2010;49(06):546–552. doi: 10.1053/j.jfas.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 12.Cook E, Cook J, Rosenblum B, Landsman A, Giurini J, Basile P. Meta-analysis of first metatarsophalangeal joint implant arthroplasty. J Foot Ankle Surg. 2009;48(02):180–190. doi: 10.1053/j.jfas.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 13.Sullivan M R. Hallux rigidus: MTP implant arthroplasty. Foot Ankle Clin. 2009;14(01):33–42. doi: 10.1016/j.fcl.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 14.Dening J, van Erve R H. Arthrodesis of the first metatarsophalangeal joint: a retrospective analysis of plate versus screw fixation. J Foot Ankle Surg. 2012;51(02):172–175. doi: 10.1053/j.jfas.2011.10.044. [DOI] [PubMed] [Google Scholar]
- 15.Foote K M, Teasdall R D, Tanaka M L, Scott A T. First metatarsophalangeal arthrodesis: a biomechanical comparison of three fixation constructs. J Surg Orthop Adv. 2012;21(04):223–231. doi: 10.3113/jsoa.2012.0223. [DOI] [PubMed] [Google Scholar]
- 16.Mohammed R, Gadgil A. Molded arthrodesis of the hallux metatarsophalangeal joint using the crossed-screw technique: surgical technique, results and functional outcomes. Foot Ankle Surg. 2012;18(02):132–135. doi: 10.1016/j.fas.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 17.Silva L F, Sousa C V, Rodrigues Pinto R, Santos C, Geada J M. Preliminary Results from the Metis-Newdeal((R)) Total Metatarsophalangeal Prosthesis. Rev Bras Ortop. 2015;46(02):200–204. doi: 10.1016/S2255-4971(15)30240-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baumhauer J F, Singh D, Glazebrook M, Blundell C, De Vries G, Le I L, Nielsen D, Pedersen M E, Sakellariou A, Solan M, Wansbrough G, Younger A S, Daniels T; for and on behalf of the CARTIVA Motion Study Group.Prospective, Randomized, Multi-centered Clinical Trial Assessing Safety and Efficacy of a Synthetic Cartilage Implant Versus First Metatarsophalangeal Arthrodesis in Advanced Hallux Rigidus Foot Ankle Int 20163705457–469. [DOI] [PubMed] [Google Scholar]
- 19.Donegan R J, Blume P A. Functional Results and Patient Satisfaction of First Metatarsophalangeal Joint Arthrodesis Using Dual Crossed Screw Fixation. J Foot Ankle Surg. 2017;56(02):291–297. doi: 10.1053/j.jfas.2016.10.021. [DOI] [PubMed] [Google Scholar]
- 20.Horisberger M, Haeni D, Henninger H B, Valderrabano V, Barg A. Total Arthroplasty of the Metatarsophalangeal Joint of the Hallux. Foot Ankle Int. 2016;37(07):755–765. doi: 10.1177/1071100716637901. [DOI] [PubMed] [Google Scholar]
- 21.Karlock L G, Berry L, Craft S T, Petrozzi R, Grahn A G, Casteel M L. First Metatarsophalangeal Joint Fusion With Use of Crossed Kirschner Wires and Intramedullary Steinmann Pin. J Foot Ankle Surg. 2017;56(06):1139–1142. doi: 10.1053/j.jfas.2017.05.012. [DOI] [PubMed] [Google Scholar]
- 22.Mirmiran R, Wilde B, Nielsen M. Retrospective analysis of the rate and interval to union for joint arthrodesis of the foot and ankle. J Foot Ankle Surg. 2014;53(04):420–425. doi: 10.1053/j.jfas.2013.12.022. [DOI] [PubMed] [Google Scholar]
- 23.Raikin S M, Ahmad J, Pour A E, Abidi N. Comparison of arthrodesis and metallic hemiarthroplasty of the hallux metatarsophalangeal joint. J Bone Joint Surg Am. 2007;89(09):1979–1985. doi: 10.2106/JBJS.F.01385. [DOI] [PubMed] [Google Scholar]
- 24.Erkocak O F, Senaran H, Altan E, Aydin B K, Acar M A. Short-term functional outcomes of first metatarsophalangeal total joint replacement for hallux rigidus. Foot Ankle Int. 2013;34(11):1569–1579. doi: 10.1177/1071100713496770. [DOI] [PubMed] [Google Scholar]
- 25.Gibson J N, Thomson C E. Arthrodesis or total replacement arthroplasty for hallux rigidus: a randomized controlled trial. Foot Ankle Int. 2005;26(09):680–690. doi: 10.1177/107110070502600904. [DOI] [PubMed] [Google Scholar]
- 26.Pulavarti R S, McVie J L, Tulloch C J. First metatarsophalangeal joint replacement using the bio-action great toe implant: intermediate results. Foot Ankle Int. 2005;26(12):1033–1037. doi: 10.1177/107110070502601206. [DOI] [PubMed] [Google Scholar]
- 27.Stevens J, de Bot R TAL, Hermus J PS, van Rhijn L W, Witlox A M. Clinical Outcome Following Total Joint Replacement and Arthrodesis for Hallux Rigidus: A Systematic Review. JBJS Rev. 2017;5(11):e2. doi: 10.2106/JBJS.RVW.17.00032. [DOI] [PubMed] [Google Scholar]
- 28.Stone O D, Ray R, Thomson C E, Gibson J N. Long-Term Follow-up of Arthrodesis vs Total Joint Arthroplasty for Hallux Rigidus. Foot Ankle Int. 2017;38(04):375–380. doi: 10.1177/1071100716682994. [DOI] [PubMed] [Google Scholar]
- 29.Kim P J, Hatch D, Didomenico L A, Lee M S, Kaczander B, Count G, Kravette M. A multicenter retrospective review of outcomes for arthrodesis, hemi-metallic joint implant, and resectional arthroplasty in the surgical treatment of end-stage hallux rigidus. J Foot Ankle Surg. 2012;51(01):50–56. doi: 10.1053/j.jfas.2011.08.009. [DOI] [PubMed] [Google Scholar]