Abstract
Background
In China, lack of evidence remains a significant challenge for the national initiative to promote physical activity (PA). We aimed to quantify the beneficial effects of meeting or maintaining the recommended PA level [150 minutes per week (min/wk) of moderate PA or 75 min/wk of vigorous PA or an equivalent combination] on incident cardiovascular disease (CVD) among Chinese population.
Methods
We included 100,560 participants without history of CVD from three cohorts in the Prediction for Atherosclerotic Cardiovascular Disease Risk in China (China-PAR) project. Cox proportional hazards models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for CVD events and its subtypes, including stroke, coronary heart disease, heart failure, and CVD death.
Results
During a median follow-up of 7.3 years (range: 6–15 years), 777,163 person-years and 4693 incident CVD events were observed. Compared with participants who were inactive at baseline, the multivariable adjusted HR (95% CI) of developing CVD was 0.74 (0.69–0.79) for those who met recommended moderate to vigorous physical activity (MVPA) level at baseline. Furthermore, the risk of CVD incidence was reduced with increment of MVPA (Ptrend < 0.001), and the HR (95% CI) of highly-active versus inactive category was 0.62 (0.56–0.68). Compared with individuals who were inactive both at the baseline and follow-up, those keeping active over the period of follow-up had a substantial lower risk of incident CVD with the HR (95% CI) of 0.57 (0.43–0.77).
Conclusions
The findings demonstrated that meeting and maintaining the recommended MVPA level could reduce the cardiovascular risk. Wider adoption of the PA recommendations would have considerable health impacts to the Chinese population.
Keywords: Cardiovascular disease, China, Cohort study, Physical activity
1. Introduction
Cardiovascular disease (CVD) has been the leading cause of mortality and morbidity worldwide,[1] and over 75% of the CVD death occurred in low-income and middle-income countries, such as China.[2] Guidelines from the World Health Organization (WHO) and several countries recommend at least 150 minutes per week (min/wk) of moderate physical activity (MPA) or 75 min/wk of vigorous physical activity (VPA) or an equivalent combination.[3],[4]
Cumulative evidence showed an inverse association between meeting recommended physical activity (PA) and cardiovascular risk,[5]–[7] and several studies also found that increases in PA over time were associated with lower risk of CVD.[8]–[10] However, most of them were from high-income countries and focused on leisure-time physical activity (LTPA). The pattern and level of PA in developing countries differed substantially from high-income countries.[6],[11] In China, over 30% of the population failed to meet the recommended level,[11] moreover, there showed a steady decreasing trend in PA due to rapid economic development and urbanization.[12] To date, evidence for the benefits associated with recommended PA level was scarce in China.[13]
Most of studies from China were limited to participants with specific cardiovascular risk factors,[14] covering a limited region,[5],[15] or only considering LTPA, a minimal domain of the overall PA among Chinese population.[5],[15] Furthermore, the effects of PA changes over time on CVD risk have never been reported before in China. Thus, this study aimed to determine the cardiovascular effects associated with baseline moderate to vigorous physical activity (MVPA) levels and change in MVPA among 100,560 participants from three large cohorts in the Prediction for Atherosclerotic Cardiovascular Disease Risk in China (China-PAR) project.
2. Methods
2.1. Study population
The study participants were derived from three cohorts in the China-PAR project, including the China Multi-Center Collaborative Study of Cardiovascular Epidemiology 1998 (China MUCA-1998), the International Collaborative Study of Cardiovascular disease in Asia (InterASIA), and the Community Intervention of Metabolic Syndrome in China & Chinese Family Health Study (CIMIC). China MUCA-1998 and InterASIA had their baseline examinations conducted in 1998 and 2000 to 2001, respectively. Both had their two follow-up surveys performed during 2007–2008 and 2012–2015. The CIMIC study, established from 2007 to 2008, was only followed up once from 2012 to 2015. Detailed information for the cohorts has been published elsewhere.[16] The China-PAR project was approved by the Institutional Review Board at Fuwai Hospital in Beijing (No.2012-399). Written informed consents were obtained from all study participants before data collection.
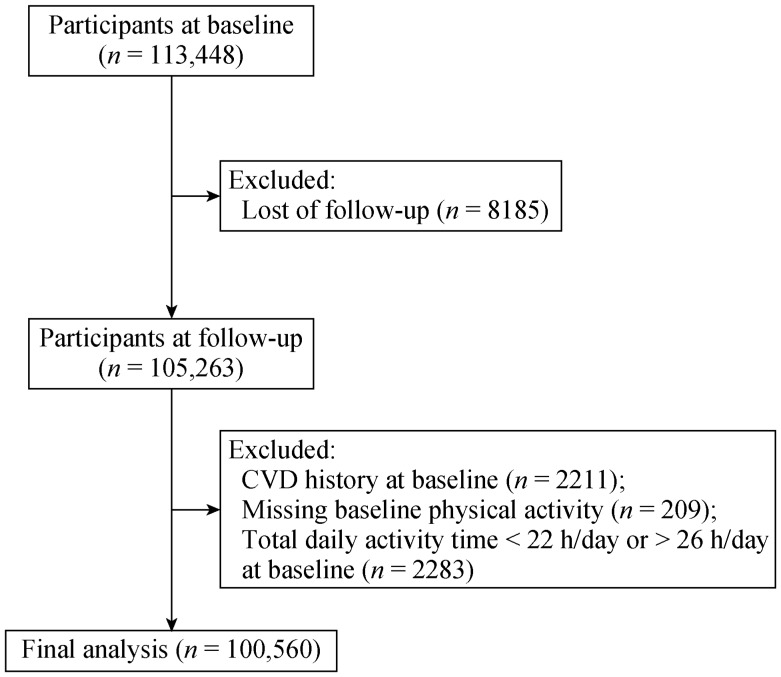
In total, 113,448 participants were enrolled in the three cohorts, of which 105,263 participants (92.79%) completed the follow-up survey at least once. For the analyses of baseline MVPA level with CVD outcomes, we excluded those with a history of CVD (n = 2211) or missing PA information (n = 209) at baseline. Furthermore, participants who reported spending more than 26 h or less than 22 h of activity per day were treated as invalid data and excluded (n = 2283), leaving 100,560 participants remained for the analyses (Figure 1). Using InterASIA and China MUCA-1998 cohorts, we examined the associations between changes in PA and CVD outcomes in 15,219 participants who were free from CVD and had complete information on PA at the first two examinations. We also used 68,065 individuals reporting participation in MVPA to investigate the relationship between the proportion of MVPA achieved by VPA and incident CVD.
Figure 1. Work flow of exclusion criteria for the analyzed subjects.
CVD: cardiovascular disease.
2.2. Assessment of PA
PA information for baseline examinations of InterASIA and CIMIC cohorts and all follow-up surveys was derived from the same question “During the previous year, how many hours per day did you usually spend on the following activities on weekdays and on weekends, respectively”. Daily activities included vigorous [defined as activities ≥ 6.0 metabolic equivalents (METs), i.e., running, heavy farming work], moderate (activities between 3.0 METs and 5.9 METs, i.e., brisk walking, yard work), light (activities between 1.5 METs and 2.9 METs, i.e., walking slowly, standing work) physical activity, sedentary behavior (activities < 1.5 METs, i.e., watching television, reading) or reclining/sleeping activity. Baseline questionnaire for China MUCA-1998 covered relevant questions for more detailed activity information, including the average time spent on specific types of PA in occupation, household, transportation, and leisure-time domains, sedentary behavior and sleeping on working days and off days during the previous year. The intensity of each PA type was determined according to 2011 Compendium of Physical Activities.[17]
For all three cohorts, VPA were weighted by two to be converted into equivalent MPA,[3] and then weighted VPA and MPA were summed up to calculate total MVPA level. We assessed the levels of MVPA in hours per week instead of METs for easier understanding and translation of the study findings. Subjects were classified into physically inactive and physically active groups by 2.5 hours/week (h/wk) of total MVPA according to the guideline recommendations.[3],[4] The physically active group was further categorized into low-active (2.5–37.4 h/wk), moderately-active (37.5–74.9 h/wk), and highly-active (≥ 75 h/wk) to analyze the dose-response relationship of MVPA with CVD outcomes, the cut points of which were selected according to the distribution of MVPA. To investigate relative effect of VPA versus MPA, individuals were divided into three groups according to the proportion of total MVPA level achieved by VPA: “0% VPA”, “0%–50% VPA”, and “≥ 50% VPA”. Regarding changes in PA, individuals were categorized into four groups: those physically inactive at both baseline and follow-up; those physically inactive at baseline and active at follow-up; those physically active at baseline and inactive at follow-up; and those physically active at both visits.
2.3. Assessment of covariates
Information on demographics, lifestyle information, and medical history was collected by trained staff with standardized questionnaires. Family history of CVD was defined as at least a parent or a sibling with coronary heart disease (CHD) or stroke. Smoker was defined as someone who smoked at least 20 packs (or 500 g of dry tobacco) during their lifetime. Current smoking was self-reported to be smoker currently at the time of baseline survey. Alcohol consumption was defined as drinking alcohol at least 12 times in the past year. Body weight and height were measured with the subject wearing light indoor clothes without shoes, and body mass index (BMI) was calculated as kilograms per meters squared. Blood pressure (BP) was measured three times after 5-minute rest in a sitting position according to a standard protocol, and the average of three BP was used. Blood samples were drawn after at least 10 h fasting and centrifuged immediately to measure serum glucose and lipids levels. Hypertension was defined as systolic BP ≥ 140 mmHg or diastolic BP ≥ 90 mmHg or antihypertensive medication use within previous two weeks. Dyslipidemia was defined as cholesterol-lowering medication use or high-density lipoprotein cholesterol < 40 mg/dL, or low-density lipoprotein cholesterol ≥ 160 mg/dL, or triglycerides ≥ 200 mg/dL, or total cholesterol ≥ 240 mg/dL. We defined prevalent diabetes mellitus as a fasting glucose level ≥ 126 mg/dL, or current treatment for diabetes.
2.4. Outcomes
For this study, CVD was defined as the first diagnosis of stroke, angina, non-fatal acute myocardial infarction, heart failure, or death with a cardiovascular event. We further classified the CVD events into four types, including stroke (fatal or non-fatal stroke events, ICD-10 I60 to I69), CHD (fatal or non-fatal CHD events, ICD-10 I20 to I25), heart failure (fatal or non-fatal heart failure events, ICD-10 I50), and CVD death (ICD-10 I00 to I99). Information regarding CVD outcomes was collected through interviewing study participants or their proxies and then checking hospital records and/or death certificates to validate the diagnosis according to ICD-10 codes. An expert committee at Fuwai Hospital reviewed and adjudicated the final end-point events by reviewing all incidence and death records.
2.5. Statistical analyses
Poisson regression model was employed to calculate the age- and sex-adjusted incidence of each outcome per 1000 person-years.[18] Cox proportional hazards model was used to estimate the hazard ratios (HRs) and corresponding 95% confidence intervals (CIs) for risk of incident CVD and subtype outcomes associated with PA levels. In Model 1, we adjusted age and sex. In Model 2, we further adjusted for geographic region (north, east, north eastern, south, central, south western, and north western), education level (below high school, high school or above), family history of CVD (yes or no), urbanization (urban or rural), alcohol consumption (yes or no), current smoking status (yes or no), levels of light physical activity (LPA), and cohort sources. Model 3 included variables in the Model 2 plus potential mediators on the causal pathway, such as BMI categories (< 18.5 kg/m2, 18.5–23.9 kg/m2, 24.0–27.9 kg/m2, ≥ 28.0 kg/m2), hypertension, diabetes, and dyslipidemia. In this study, findings from Model 2 were used as the main results to avoid over-adjustment. For the analyses of baseline MVPA, person-years of follow-up for each outcome were calculated from the date of baseline examination to the date of the occurrence of events, death, or the last follow-up interview, whichever came first. For the analyses of changes in PA levels, person-years of follow-up were calculated from the first follow-up survey, and all the covariates for Model 2 were derived from the follow-up visit.
Trend tests were conducted using median values for MVPA categories as continuous variables in the Cox models. Dose-response relationships were assessed by restricted cubic spline analyses with four knots placed at the 5th, 35th, 65th, and 95th percentiles of MVPA.[19],[20] Nonlinear associations were checked first with the likelihood ratio test. If tests for nonlinearity were significant, spline models were used to describe the overall association, otherwise, linear models were used. Stratified analyses were used to assess whether the associations were modified by selected characteristics and tests for interaction were performed by including cross-product terms in models. We conducted sensitivity analyses by excluding 1335 participants who developed CVD within the first two years of follow-up. Furthermore, we estimated the gained disease-free years associated with meeting recommended MVPA by applying the trapezium rule in intervals of 0.5 years, from the baseline age to age 95.[21]
Statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, North Carolina, USA). All statistical tests were two-sided, with P-value < 0.05 considered significant.
3. Results
The baseline characteristics of study participants were shown in Table 1. The mean age was 51.5 ± 12.2 years and 40.1% of the subjects were male. Participants with higher MVPA were more likely to be male, to have lower education level, higher prevalence of smoking and alcohol consumption, and were less likely to live in urban areas and participate in LPA. Higher MVPA was also associated with lower BMI, lower prevalence of hypertension, diabetes mellitus, and dyslipidemia.
Table 1. Characteristics according to moderate to vigorous physical activity levels at baseline.
| Characteristics | All | Inactive (< 2.5 h/wk) | Meeting guideline recommended MVPA |
||
| Low-active (2.5–37.4 h/wk) | Moderately-active (37.5–74.9 h/wk) | Highly-active (≥ 75 h/wk) | |||
| Number of participants | 100,560 | 32,887 | 15,224 | 22,737 | 29,712 |
| Age, yrs | 51.5 ± 12.2 | 52.8 ± 13.7 | 51.2 ± 12.2 | 50.3 ± 11.7 | 51.3 ± 10.7 |
| Male | 40,367 (40.1%) | 11,853 (36.0%) | 5930 (39.0%) | 9435 (41.5%) | 13,149 (44.3%) |
| Urban | 9546 (9.5%) | 6191 (18.8%) | 2446 (16.1%) | 735 (3.2%) | 174 (0.6%) |
| Education level ≥ high school | 14,080 (14.1%) | 6491 (19.7%) | 3312 (21.8%) | 2317 (10.2%) | 1960 (6.6%) |
| Current smoker | 22,104 (22.1%) | 6206 (18.9%) | 3238 (21.3%) | 5452 (24.0%) | 7208 (24.3%) |
| Alcohol drinker | 18,597 (18.5%) | 5013 (15.2%) | 2661 (17.5%) | 4464 (19.6%) | 6459 (21.7%) |
| Family history of CVD | 10,010 (10.0%) | 2988 (9.1%) | 2270 (14.9%) | 2127 (9.4%) | 2625 (8.8%) |
| VPA#, h/wk | 0.0 (0.0–35.0) | 0.0 (0.0–0.0) | 0.0 (0.0–7.0) | 14.0 (0.0–22.7) | 50.0 (42.0–56.0) |
| MPA#, h/wk | 0.0 (0.0–21.0) | 0.0 (0.0–0.0) | 14.0 (4.9–21.0) | 35.0 (0.0–56.0) | 0.0 (0.0–21.0) |
| LPA#, h/wk | 21.0 (7.0–42.0) | 46.0 (25.5–63.0) | 30.0 (21.0–47.0) | 14.0 (7.0–28.0) | 10.5 (0.0–14.0) |
| Body mass index, kg/m2 | 23.8 ± 3.6 | 23.8 ± 3.7 | 24.0 ± 3.7 | 23.7 ± 3.6 | 23.6 ± 3.5 |
| Hypertension | 33,594 (33.4%) | 12,801 (38.9%) | 5093 (33.5%) | 6894 (30.3%) | 8806 (29.6%) |
| Diabetes mellitus | 5571 (5.9%) | 2299 (7.0%) | 1011 (6.6%) | 1060 (4.7%) | 1201 (4.0%) |
| Dyslipidemia | 30,078 (31.4%) | 10,588 (32.2%) | 5170 (34.0%) | 6651 (29.3%) | 7669 (25.8%) |
Data are presented as means ± SD or n (%). #Presented as median (25th–75th). h/wk refers to hours per week. CVD: cardiovascular disease; LPA: light physical activity; MPA: moderate physical activity; MVPA: moderate to vigorous physical activity; VPA: vigorous physical activity.
During 777,163 person-years, a median follow-up of 7.3 years, there were 4693 CVD events, including 2850 stroke, 1218 CHD, 497 heart failure and 1915 CVD deaths, with the mean follow-up duration of 15 years, 13 years and 6 years for the China MUCA-1998, InterASIA, and CIMIC, respectively. After adjustment for potential confounders, meeting recommended MVPA level was related to lower risk of incident CVD and each subtype outcome (Table 2). In comparison with physically inactive individuals, those who met recommended MVPA had 26%, 10%, 41%, 50%, and 35% risk reduction of CVD, stroke, CHD, heart failure, and CVD death, respectively (Model 2). After additional adjustment for potential mediators, including BMI, diabetes, hypertension, and dyslipidemia, the associations between MVPA and CVD, CHD, heart failure, and CVD death were modestly attenuated but remained significant, whereas the association was not significant for stroke (Model 3).
Table 2. Hazard ratios for cardiovascular disease outcomes according to baseline moderate to vigorous physical activity categories.
| Variable | Inactive | Meeting recommended MVPA |
Ptrend-value# | |||
| All | Low-active | Moderately-active | Highly-active | |||
| CVD | ||||||
| Number of cases | 1964 | 2729 | 866 | 835 | 1028 | |
| Adjusted incidence* (95% CI) | 7.14 (6.74–7.57) | 6.16 (5.88–6.45) | 6.74 (6.28–7.24) | 6.21 (5.77–6.68) | 5.73 (5.36–6.13) | |
| Model 1: HR (95% CI) | 1.00 (ref.) | 0.88 (0.83–0.94) | 1.02 (0.94–1.10) | 0.85 (0.78–0.92) | 0.81 (0.75–0.87) | < 0.001 |
| Model 2: HR (95% CI) | 1.00 (ref.) | 0.74 (0.69–0.79) | 0.90 (0.83–0.98) | 0.68 (0.63–0.75) | 0.62 (0.56–0.68) | < 0.001 |
| Model 3: HR (95% CI) | 1.00 (ref.) | 0.82 (0.77–0.88) | 0.93(0.85–1.01) | 0.77 (0.70–0.84) | 0.73 (0.67–0.81) | < 0.001 |
| Stroke | ||||||
| Number of cases | 1048 | 1802 | 537 | 563 | 702 | |
| Adjusted incidence* (95% CI) | 4.06 (3.76–4.39) | 3.85 (3.64–4.08) | 4.11 (3.75–4.50) | 3.86 (3.53–4.22) | 3.68 (3.39–3.99) | |
| Model 1: HR (95% CI) | 1.00 (ref.) | 1.06 (0.98–1.55) | 1.16 (1.05–1.29) | 1.05 (0.94–1.16) | 1.00 (0.91–1.10) | 0.561 |
| Model 2: HR (95% CI) | 1.00 (ref.) | 0.90 (0.83–0.99) | 1.01 (0.91–1.13) | 0.86 (0.77–0.97) | 0.81 (0.72–0.91) | < 0.001 |
| Model 3: HR (95% CI) | 1.00 (ref.) | 1.01 (0.92–1.11) | 1.06 (0.95–1.18) | 0.98 (0.88–1.11) | 0.97 (0.86–1.11) | 0.516 |
| CHD | ||||||
| Number of cases | 596 | 622 | 221 | 183 | 218 | |
| Adjusted incidence* (95% CI) | 2.03 (1.84–2.25) | 1.49 (1.36–1.63) | 1.67 (1.46–1.91) | 1.53 (1.32–1.78) | 1.33 (1.16–1.53) | |
| Model 1: HR (95% CI) | 1.00 (ref.) | 0.68 (0.61–0.77) | 0.83 (0.71–0.97) | 0.64 (0.54–0.76) | 0.60 (0.51–0.71) | < 0.001 |
| Model 2: HR (95% CI) | 1.00 (ref.) | 0.59 (0.51–0.67) | 0.73 (0.62–0.86) | 0.53 (0.44–0.64) | 0.47 (0.39–0.56) | < 0.001 |
| Model 3: HR (95% CI) | 1.00 (ref.) | 0.66 (0.58–0.75) | 0.77 (0.65–0.91) | 0.59 (0.49–0.71) | 0.58 (0.48–0.70) | < 0.001 |
| Heart failure | ||||||
| Number of cases | 246 | 251 | 78 | 78 | 95 | |
| Adjusted incidence* (95% CI) | 0.78 (0.64–0.95) | 0.63 (0.53–0.75) | 0.66 (0.51–0.86) | 0.68 (0.53–0.87) | 0.57 (0.45–0.72) | |
| Model 1: HR (95% CI) | 1.00 (ref.) | 0.70 (0.58–0.83) | 0.79 (0.61–1.02) | 0.67 (0.52–0.87) | 0.64 (0.51–0.82) | < 0.001 |
| Model 2: HR (95% CI) | 1.00 (ref.) | 0.50 (0.40–0.61) | 0.77 (0.59–1.01) | 0.45 (0.34–0.59) | 0.35 (0.26–0.46) | < 0.001 |
| Model 3: HR (95% CI) | 1.00 (ref.) | 0.55 (0.45–0.69) | 0.80 (0.61–1.05) | 0.49 (0.37–0.66) | 0.41 (0.31–0.55) | < 0.001 |
| CVD death | ||||||
| Number of cases | 903 | 1012 | 323 | 301 | 388 | |
| Adjusted incidence* (95% CI) | 2.91 (2.63–3.23) | 2.47 (2.27–2.69) | 2.74 (2.42–3.10) | 2.41 (2.12–2.73) | 2.34 (2.09–2.62) | |
| Model 1: HR (95% CI) | 1.00 (ref.) | 0.79 (0.72–0.87) | 0.92 (0.81–1.04) | 0.73 (0.64–0.84) | 0.75 (0.66–0.84) | < 0.001 |
| Model 2: HR (95% CI) | 1.00 (ref.) | 0.65 (0.59–0.72) | 0.83 (0.72–0.94) | 0.57 (0.50–0.66) | 0.55 (0.47–0.63) | < 0.001 |
| Model 3: HR (95% CI) | 1.00 (ref.) | 0.71 (0.63–0.79) | 0.84 (0.73–0.96) | 0.63 (0.54–0.73) | 0.63 (0.54–0.73) | < 0.001 |
Model 1: adjusted for age and sex. Model 2: adjusted for variables in model 1 plus geographic region, urbanization, education, family history of CVD, current smoking status, alcohol consumption, light physical activity, and cohort sources. Model 3: adjusted for variables in model 2 plus baseline BMI categories (< 18.5 kg/m2, 18.5–23.9 kg/m2, 24.0–27.9 kg/m2, ≥ 28.0 kg/m2), diabetes, hypertension, and dyslipidemia. *Refers to all adjusted incidence rates were per 1000 person-years and adjusted for age and sex by Poisson regression model. #Refers to P-value for linear trend across inactive, low-active, moderately-active, and highly-active categories. BMI: body mass index; CHD: coronary heart disease; CI: confidence interval; CVD: cardiovascular disease; HR: hazard ratio; MVPA: moderate to vigorous physical activity.
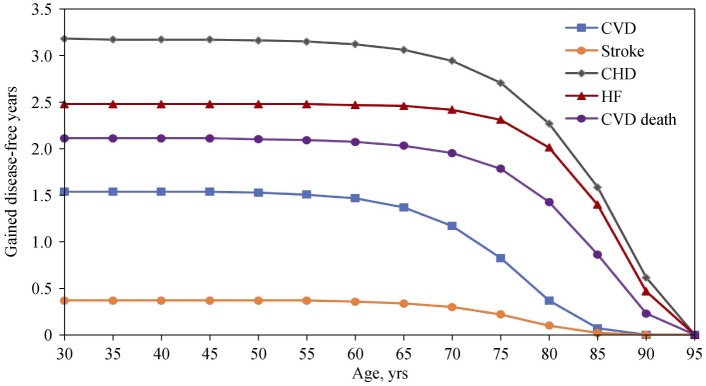
The inverse associations between meeting recommended MVPA and the risk of each CVD outcome were consistent across subgroups by age, sex, urbanization, or health conditions (Pinteraction > 0.05), although the association did not reach significance among urban participants (Figure 2). In addition, meeting recommended MVPA level postponed the occurrence of CVD (Figure 3). Compared with those meeting recommended MVPA levels, inactive subjects at the range of index age from 30 years old to 65 years old would develop CVD approximately 1.5 years earlier. When comparing the relative benefits associated with VPA versus MPA, the proportion of MVPA achieved by VPA was not related to risk of CVD after multivariable adjustment (Ptrend > 0.05), regardless of age, sex, and comorbidities (Table 3).
Figure 2. Hazard ratios for CVD associated with meeting recommended MVPA levels across subgroups.
Models were adjusted for age, sex, geographic region, urbanization, education, family history of CVD, current smoking status, alcohol consumption, light physical activity, and cohort sources. The reference in each subgroup was participants who did not meet the recommended MVPA level. BMI: body mass index; CI: confidence interval; CVD: cardiovascular disease; MVPA: moderate to vigorous physical activity.
Figure 3. Gained disease-free years up to 95 years of age associated with meeting recommended MVPA levels.
CHD: coronary heart disease; CVD: cardiovascular disease; HF: heart failure; MVPA: moderate to vigorous physical activity.
Table 3. Hazard ratios for CVD associated with proportion of MVPA achieved by VPA stratified by baseline characteristics among participants who reported participation in MVPA.
| Variable | Proportion of MVPA by VPA |
Ptrend-value | |||
| Number of participants | 0 | > 0 to < 50% | ≥ 50% | ||
| All | 68,065 | 1.00 (ref.) | 0.97 (0.82–1.15) | 1.02 (0.92–1.14) | 0.584 |
| Age, yrs | |||||
| 16–44 | 23,091 | 1.00 (ref.) | 0.97 (0.54–1.73) | 1.18 (0.82–1.68) | 0.346 |
| 45–59 | 29,857 | 1.00 (ref.) | 1.04 (0.79–1.35) | 1.05 (0.89–1.25) | 0.549 |
| ≥ 60 | 15,117 | 1.00 (ref.) | 0.87 (0.68–1.11) | 0.90 (0.77–1.05) | 0.238 |
| Sex | |||||
| Male | 28,722 | 1.00 (ref.) | 0.77 (0.60–1.00) | 1.02 (0.88–1.18) | 0.560 |
| Female | 39,343 | 1.00 (ref.) | 1.21 (0.96–1.52) | 1.06 (0.90–1.24) | 0.652 |
| BMI, kg/m2 | |||||
| < 24 | 38,254 | 1.00 (ref.) | 0.96 (0.75–1.22) | 1.10 (0.95–1.28) | 0.145 |
| ≥ 24 | 29,766 | 1.00 (ref.) | 0.98 (0.77–1.25) | 0.94 (0.81–1.10) | 0.463 |
| Hypertension | |||||
| No | 47,158 | 1.00 (ref.) | 1.01 (0.78–1.31) | 1.04 (0.88–1.23) | 0.640 |
| Yes | 20,876 | 1.00 (ref.) | 1.00 (0.79–1.25) | 1.07 (0.93–1.23) | 0.348 |
| Diabetes | |||||
| No | 60,059 | 1.00 (ref.) | 0.97 (0.80–1.17) | 1.06 (0.95–1.19) | 0.244 |
| Yes | 3286 | 1.00 (ref.) | 1.28 (0.73–2.24) | 0.99 (0.69–1.43) | 0.847 |
| Dyslipidemia | |||||
| No | 44,800 | 1.00 (ref.) | 0.92 (0.73–1.15) | 1.07 (0.93–1.22) | 0.311 |
| Yes | 19,430 | 1.00 (ref.) | 1.12 (0.85–1.47) | 1.03 (0.86–1.24) | 0.726 |
Models were adjusted for age, sex, geographic region, urbanization, education, family history of CVD, current smoking status, alcohol consumption, light physical activity, total volume of MVPA, and cohort sources. BMI: body mass index; CVD: cardiovascular disease; MVPA: moderate to vigorous physical activity; VPA: vigorous physical activity.
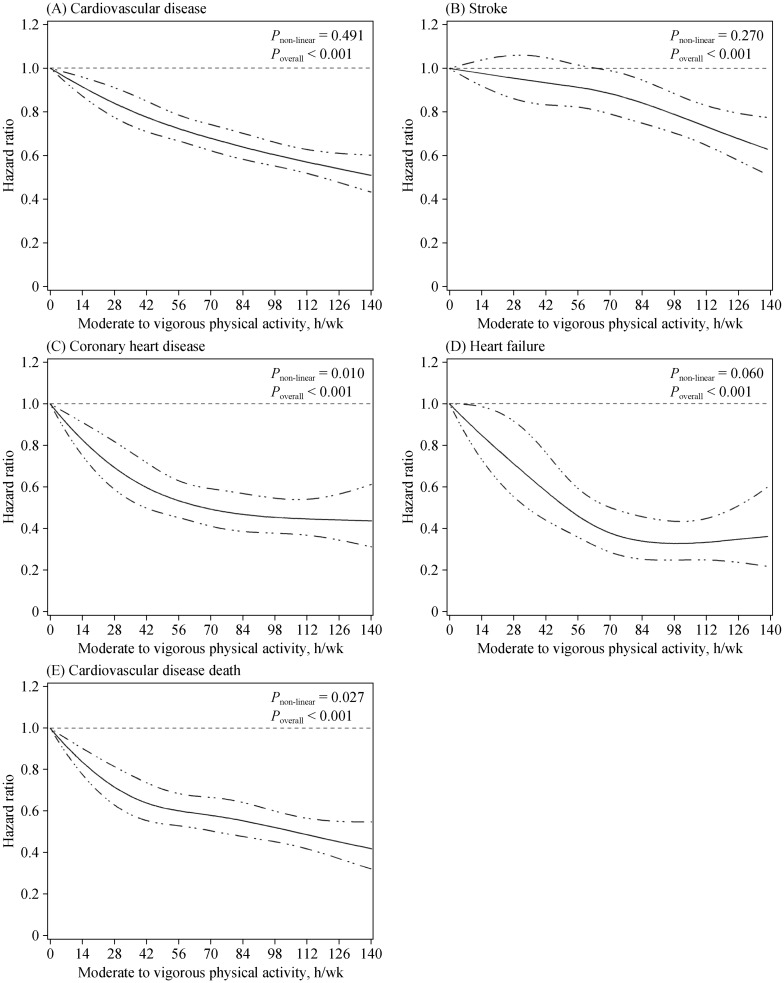
In the analyses further categorizing participants meeting recommendations by MVPA level, a graded inverse association between MVPA and the risk of CVD was observed (Ptrend < 0.001, Table 2). Compared with the inactive group, the risk reductions of CVD among the low-active, moderately-active, and highly-active categories were 10%, 32%, and 38%, respectively. Similarly, the incident risk of each CVD subtype outcome was lower with higher level of MVPA (Table 2). The exclusion of participants developing CVD events during the first two years of follow-up had little effect on the observed associations (supplemental material, Table 1S). In continuous analyses with restricted cubic splines, an inverse, linear dose-response relationship was observed between MVPA levels and CVD risk (Pnon-linear = 0.491) (Figure 4). However, there appeared to be a flattening of the inverse relationship at approximately 70 h/wk for CHD (Pnon-linear = 0.01) and heart failure (Pnon-linear = 0.06), despite of a borderline significance for heart failure possibly due to low number of cases. Moreover, risk reduction of CVD mortality was much slower at activity levels above around 42 h/wk than lower activity levels (Pnon-linear = 0.027).
Figure 4. Hazard ratios for cardiovascular events according to MVPA levels.
(A): Cardiovascular disease; (B): stroke; (C): coronary heart disease; (D): heart failure; and (E): cardiovascular disease death. Data were fitted by restricted cubic spline Cox proportional hazards models, with four knots placed at the 5th, 35th, 65th, and 95th percentiles of MVPA. Covariates were the same as Model 2 in the main analysis, including age, sex, geographic region, urbanization, drinking status, current smoking status, education level, family history of cardiovascular disease, light physical activity, and cohort sources. Results were reported as hazard ratios (solid line) and 95% confidence intervals (dashed line). MVPA: moderate to vigorous physical activity.
Among 15,219 individuals who received two examinations over a median interval of eight years, 4520 (29.7%) participants were continually inactive, 1942 (12.8%) became active, 3271(21.5%) became inactive, and 5496 (36.1%) were continually active. In comparison with participants who were inactive at both visits, subjects who were persistently active had the lowest risk for each CVD subtype after multivariate adjustment, with the HRs (95% CIs) of 0.57 (0.43–0.77) for CVD, 0.65 (0.44–0.96) for stroke, 0.53 (0.33–0.87) for CHD, 0.37 (0.10–1.36) for heart failure, and 0.52 (0.31–0.89) for CVD mortality, respectively. Increasing MVPA levels over the follow-up period was also related to reduced CVD risk of borderline significance (HR = 0.71, 95% CI: 0.50–1.00), while those reducing MVPA from physically active to physically inactive status had similar risk to those continually inactive (HR = 0.97, 95% CI: 0.74–1.26) (Table 4).
Table 4. Hazard ratios for CVD outcomes according to changes in MVPA levels from baseline to the first follow-up examination.
| Variable | Number of cases/Number at risk | Adjusted incidence (95% CI)* | HR (95% CI) |
| CVD | |||
| Continually inactive | 178/4520 | 9.51 (7.93–11.41) | 1.00 (ref.) |
| From inactive to active | 47/1942 | 6.81 (5.01–9.26) | 0.71 (0.50–1.00) |
| From active to inactive | 125/3271 | 6.39 (5.25–7.79) | 0.97 (0.74–1.26) |
| Continually active | 127/5496 | 5.10 (4.21–6.17) | 0.57 (0.43–0.77) |
| Stroke | |||
| Continually inactive | 93/4520 | 5.70 (4.45–7.29) | 1.00 (ref.) |
| From inactive to active | 27/1942 | 3.65 (2.43–5.49) | 0.78 (0.49–1.25) |
| From active to inactive | 77/3271 | 3.86 (2.96–5.04) | 1.07 (0.75–1.52) |
| Continually active | 85/5496 | 2.96 (2.32–3.78) | 0.65 (0.44–0.96) |
| CHD | |||
| Continually inactive | 73/4520 | 3.40 (2.55–4.54) | 1.00 (ref.) |
| From inactive to active | 15/1942 | 2.43 (1.43–4.11) | 0.59 (0.32–1.06) |
| From active to inactive | 41/3271 | 2.04 (1.50–2.77) | 1.02 (0.67–1.56) |
| Continually active | 38/5496 | 1.76 (1.26–2.47) | 0.53 (0.33–0.87) |
| Heart failure | |||
| Continually inactive | 20/4520 | 0.60 (0.31–1.15) | 1.00 (ref.) |
| From inactive to active | 3/1942 | 1.09 (0.25–4.64) | 0.44 (0.10–2.02) |
| From active to inactive | 12/3271 | 0.37 (0.17–0.84) | 0.75 (0.27–2.11) |
| Continually active | 4/5496 | 0.45 (0.15–1.34) | 0.37 (0.10–1.36) |
| CVD death | |||
| Continually inactive | 55/4520 | 2.62 (1.79–3.85) | 1.00 (ref.) |
| From inactive to active | 15/1942 | 2.42 (1.43–4.12) | 0.89 (0.50–1.60) |
| From active to inactive | 42/3271 | 2.06 (1.44–2.94) | 1.24 (0.80–1.93) |
| Continually active | 37/5496 | 1.64 (1.16–2.32) | 0.52 (0.31–0.89) |
Models were adjusted for covariates derived from first follow-up survey, including age, sex, geographic region, urbanization, education, family history of CVD, cohort sources, current smoking status, alcohol consumption, and light physical activity. *Refers to all adjusted incidence rates were per 1000 person-years and adjusted for age and sex by Poisson regression model. CHD: coronary heart disease; CI: confidence interval; CVD: cardiovascular disease; HR: hazard ratio; MVPA: moderate to vigorous physical activity.
4. Discussion
With the large longitudinal data from the Chinese cohort, this study demonstrated that meeting the MVPA level recommended by international guidelines was associated with cardiovascular benefits among Chinese adults. In addition, maintaining the recommended MVPA level substantially reduced the incident CVD risk up to 43%. When adjusted for the MVPA level, higher proportion of VPA did not convey additional cardiovascular benefits or harms. Our findings provided timely evidence for Healthy China Initiative, as well as for other countries that intend to achieve a PA goal.
Conclusions from previous studies remained unclear whether excessive PA resulted in additional benefits.[7],[22]–[24] A cohort of 88,140 US adults reported that the risk of CVD mortality was higher when comparing high versus medium dose of PA.[7] In a prospective study from Japan that involved 3345 CVD events, CVD risk decreased steeply from the lowest PA to 50th percentile of the PA distribution and then reached a plateau.[24] In a Chinese cohort of 487,334 individuals with 7.5 years of follow-up, there was a log-linear inverse relationship between total PA and major CVD risk, suggesting PA at very high level could also reduce CVD risk.[25] Similarly, our study, with a much broader range of PA levels, also found a progressively reduced risk of CVD when MVPA was far exceeding the recommended levels (≥ 150 min/wk MPA or ≥ 75 min/wk VPA or combination).
Consistent with evidence from western countries, keeping physically active over eight years could convey substantial benefits, while those initially active and subsequently decreased PA showed no risk difference from individuals who remained inactive at both visits.[26] It emphasized the great importance of persistence in regards to PA. In our study, 21.5% of participants were active at baseline and became inactive, while only 12.8% were inactive at baseline and became active over eight years. This was consistent with studies demonstrating a decline in PA among Chinese adults, largely driven by occupational PA reductions.[12],[27],[28] Given the importance of keeping active, health policies are needed to encourage LTPA as a substitution for the diminishing occupational activity. Moreover, compared with “continually inactive” group, “from inactive to active” tended to have reduced cardiovascular risk, supporting the adoption of a physically active lifestyle by previously inactive individuals.
Although PA guidelines recommend that one minute of VPA is equivalent to two minutes of MPA,[3],[4] previous studies from western countries on the relative cardiovascular benefits of VPA versus MPA was inconsistent, with some studies showing advantages of VPA over MPA[5] and others reporting no significant difference.[29] We found that the proportion of VPA was not related to CVD risk after adjustment for total MVPA time, which concurred with the guidelines. Thus, individuals with less available time for exercise could turn to high-intensity activity to get comparable benefits within limited time.
4.1. Strengths and limitations
This study extended previous cohort studies in several important ways. Firstly, this was the first cohort study in China to quantify the association between total PA meeting international recommended levels and incident CVD, and to demonstrate the relationship between changes in PA and cardiovascular outcomes. Moreover, this study was based on a large sample size, high rate of follow-up (92.79%), and stringent quality control procedures as well. Furthermore, unlike previous studies mainly focused on leisure time activity,[5] we quantified total PA. Nevertheless, the present study also had several limitations. Firstly, PA was assessed with questionnaire other than objective measurement, which might lead to measurement error. Secondly, although the average level of PA during the past year before each survey was collected as the baseline level, we cannot exclude that PA actually fluctuated from time to time, which might lead to misclassification bias. The findings still need further validation by future independent cohort studies among Chinese adults. Last but not least, despite of adjustment for multiple covariates, residual confounding may still exist because of unknown or suboptimal measured factors.
4.2. Conclusions
In conclusion, moderate or vigorous physical activity above international guideline recommended level were associated with cardiovascular benefits among Chinese adults, regardless of the composition of MVPA. The more physically active, the less risk of cardiovascular diseases.
Acknowledgments
This study was supported by the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (2017-I2M-1-004 & 2019-I2M-2-003), the National Key Research and Development Program of China (2017 YFC0211703 & 2018YFE0115300 & 2018YFC1311703 & 2017YFC0908401), and the National Natural Science Foundation of China (91643208). All authors had no conflicts of interest to disclose. The authors acknowledge the staff and participants of the China-PAR (Prediction for Atherosclerotic Cardiovascular Disease Risk in China) project for their important participation and contribution.
References
- 1.Naghavi M, Abajobir AA, Abbafati C, et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1151–1210. doi: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. About cardiovascular diseases, 2020. World Health Organization of cardiovascular diseases Web site. [(accessed on Feb 11, 2020)]. https://www.who.int/cardiovascular_diseases/about_cvd/en/
- 3.Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA. 2018;320:2020–2028. doi: 10.1001/jama.2018.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Global recommendations on physical activity for health. Geneva, Switzerland: World Health Organization; 2010. [PubMed] [Google Scholar]
- 5.Wen CP, Wai JP, Tsai MK, et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet. 2011;378:1244–1253. doi: 10.1016/S0140-6736(11)60749-6. [DOI] [PubMed] [Google Scholar]
- 6.Lear SA, Hu W, Rangarajan S, et al. The effect of physical activity on mortality and cardiovascular disease in 130,000 people from 17 high-income, middle-income, and low-income countries: the PURE study. Lancet. 2017;390:2643–2654. doi: 10.1016/S0140-6736(17)31634-3. [DOI] [PubMed] [Google Scholar]
- 7.Zhao M, Veeranki SP, Li S, et al. Beneficial associations of low and large doses of leisure time physical activity with all-cause, cardiovascular disease and cancer mortality: a national cohort study of 88,140 US adults. Br J Sports Med. 2019;53:1405–1411. doi: 10.1136/bjsports-2018-099254. [DOI] [PubMed] [Google Scholar]
- 8.Florido R, Kwak L, Lazo M, et al. Six-year changes in physical activity and the risk of incident heart failure: ARIC study. Circulation. 2018;137:2142–2151. doi: 10.1161/CIRCULATIONAHA.117.030226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim K, Choi S, Hwang SE, et al. Changes in exercise frequency and cardiovascular outcomes in older adults. Eur Heart J. doi: 10.1093/eurheartj/ehz768. Published Online First: 8 November 2019. [DOI] [PubMed] [Google Scholar]
- 10.Mok A, Khaw KT, Luben R, et al. Physical activity trajectories and mortality: population based cohort study. BMJ. 2019;365:l2323. doi: 10.1136/bmj.l2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hallal PC, Andersen LB, Bull FC, et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380:247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- 12.Ng SW, Howard AG, Wang HJ, et al. The physical activity transition among adults in China: 1991–2011. Obes Rev. 2014;15(Suppl 1):27–36. doi: 10.1111/obr.12127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Milton K, Macniven R, Bauman A. Review of the epidemiological evidence for physical activity and health from low- and middle-income countries. Glob Public Health. 2014;9:369–381. doi: 10.1080/17441692.2014.894548. [DOI] [PubMed] [Google Scholar]
- 14.Fan M, Yu C, Guo Y, et al. Effect of total, domain-specific, and intensity-specific physical activity on all-cause and cardiovascular mortality among hypertensive adults in China. J Hypertens. 2018;36:793–800. doi: 10.1097/HJH.0000000000001601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu Y, Wen W, Gao YT, et al. Level of moderate-intensity leisure-time physical activity and reduced mortality in middle-aged and elderly Chinese. J Epidemiol Community Health. 2018;72:13–20. doi: 10.1136/jech-2017-209903. [DOI] [PubMed] [Google Scholar]
- 16.Yang X, Li J, Hu D, et al. Predicting the 10-year risks of atherosclerotic cardiovascular disease in Chinese population: the China-PAR project (prediction for ASCVD risk in China) Circulation. 2016;134:1430–1440. doi: 10.1161/CIRCULATIONAHA.116.022367. [DOI] [PubMed] [Google Scholar]
- 17.Ainsworth BE, Haskell WL, Herrmann SD, et al. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43:1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 18.Zhao D. Poisson regression adjustment of event rates and its macro procedure ADJ_POIS. SAS Users Group 24th International Annual Conference; Florida, USA. 1999. [Google Scholar]
- 19.Desquilbet L, Mariotti F. Dose-response analyses using restricted cubic spline functions in public health research. Stat Med. 2010;29:1037–1057. doi: 10.1002/sim.3841. [DOI] [PubMed] [Google Scholar]
- 20.Li R, Hertzmark E, Louie M, et al. The SAS LGTPHCURV9 Macro. Boston: Channing Laboratory; 2011. [Google Scholar]
- 21.Liu F, Li J, Chen J, et al. Predicting lifetime risk for developing atherosclerotic cardiovascular disease in Chinese population: the China-PAR project. Sci Bull. 2018;63:779–787. doi: 10.1016/j.scib.2018.05.020. [DOI] [PubMed] [Google Scholar]
- 22.Armstrong ME, Green J, Reeves GK, et al. Frequent physical activity may not reduce vascular disease risk as much as moderate activity: large prospective study of women in the United Kingdom. Circulation. 2015;131:721–729. doi: 10.1161/CIRCULATIONAHA.114.010296. [DOI] [PubMed] [Google Scholar]
- 23.Schnohr P, O'Keefe JH, Marott JL, et al. Dose of jogging and long-term mortality: the Copenhagen City Heart Study. J Am Coll Cardiol. 2015;65:411–419. doi: 10.1016/j.jacc.2014.11.023. [DOI] [PubMed] [Google Scholar]
- 24.Kubota Y, Iso H, Yamagishi K, et al. Daily total physical activity and incident cardiovascular disease in Japanese men and women: Japan Public Health Center-Based Prospective Study. Circulation. 2017;135:1471–1473. doi: 10.1161/CIRCULATIONAHA.116.026557. [DOI] [PubMed] [Google Scholar]
- 25.Bennett DA, Du H, Clarke R, et al. Association of physical activity with risk of major cardiovascular diseases in Chinese men and women. JAMA Cardiol. 2017;2:1349–1358. doi: 10.1001/jamacardio.2017.4069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gregg EW, Cauley JA, Stone K, et al. Relationship of changes in physical activity and mortality among older women. JAMA. 2003;289:2379–2386. doi: 10.1001/jama.289.18.2379. [DOI] [PubMed] [Google Scholar]
- 27.Ng SW, Norton EC, Popkin BM. Why have physical activity levels declined among Chinese adults? Findings from the 1991–2006 China Health and Nutrition Surveys. Soc Sci Med. 2009;68:1305–1314. doi: 10.1016/j.socscimed.2009.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Attard SM, Howard AG, Herring AH, et al. Differential associations of urbanicity and income with physical activity in adults in urbanizing China: findings from the population-based China Health and Nutrition Survey 1991–2009. Int J Behav Nutr Phys Act. 2015;12:152. doi: 10.1186/s12966-015-0321-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shiroma EJ, Sesso HD, Moorthy MV, et al. Do moderate-intensity and vigorous-intensity physical activities reduce mortality rates to the same extent? J Am Heart Assoc. 2014;3:e000802. doi: 10.1161/JAHA.114.000802. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.