Abstract
Objective: To describe the feasibility and dye diffusion of selective perineural injection of the 7 and 8th cervical nerve (C7 and C8) ramus ventralis under ultrasonographic guidance in horses.
Study design: Prospective experimental pilot cadaver study.
Animals: Four equine cadavers of similar body weight (420–480 kg) and neck conformation.
Methods: Five C7 and five C8 rami were perineurally injected with a dye solution. Anatomic dissections including vertebral canal opening were conducted to confirm nerve dye staining and describe the extent of color diffusion.
Results: The ramus ventralis of the spinal cervical nerves was visualized in all cadavers. All the injections were successful in staining a portion of the nerve trunk. Eight rami had a uniform transversal staining of the nerve trunk that longitudinally covered a distance >2 cm. One C7 and one C8 nerve trunk showed incomplete transversal staining with a more concentrated color on its half cranial aspect and a longitudinal coverage of <2 cm. Five injections resulted in dye extending proximally and medially into the epidural space. Volume had no appreciable effect on the extent of nerve staining. A greater proportion of epidural diffusion was found with injections done within less than one cm distally to the articular processes. All injections were considered to be selective for the targeted nerve.
Conclusion and clinical relevance: Ultrasonography-guided perineural injection of C7 and C8 ramus ventralis is a feasible technique that may have multiple applications in multimodal analgesia in horses. Further clinical study will be necessary to determine the appropriate drug, dosage, and volume to inject and to confirm its usefulness.
Keywords: horse, ultrasonography, cervical, nerve roots, anesthesia, analgesia
Introduction
Arthropathy of the articular process joints of the caudal cervical spine has been associated with neck pain and stiffness as well as forelimb lameness in horses (1–3). Enlarged articular process joints with periarticular bony proliferation and associated capsule effusion have been documented to reduce intraforaminal space resulting in possible nerve root impingement (1, 4–6). Compressive neuropathy of the 7th cervical nerve root has been evidenced histologically on post-mortem specimens in horses (1, 2).
Cervical radiculopathy is considered to be a debilitating disease in humans with variable clinical signs that range from pain, numbness, and/or tingling in the upper extremity to electric shock type pain and muscle weakness (7). In dogs, the pathognomonic clinical presentation is the nerve root-signature sign, which is similar to the signs seen in horses. Dogs adopt a non-weight bearing posture on the affected side, holding their forelimb in a semi-flexed position. They may also show some signs of neck pain (8).
Magnetic resonance imaging (MRI) and contrast-enhanced computed tomography (CT) are the imaging techniques of choice to identify articular process enlargement, intervertebral foramen size reduction, and nerve root impingement (6, 7, 9, 10). In horses, despite recently improving technology, these imaging techniques are still of limited clinical applicability to the equine caudal cervical region due to technical constraint imposed by the relative size of the equine neck/chest/shoulders compared to the instrument bore.
Selective cervical nerve root injections have been used in humans and dogs mainly for therapeutic purposes and, less commonly, to confirm the site of pain (8, 11–16). Periradicular injection techniques have been developed under fluoroscopic guidance but more recently ultrasonography-guided injections have been shown to be as effective and possibly safer in humans (11, 14, 16, 17). More precisely, transforaminal injections around the cervical nerve root are classically performed using the fluoroscopic techniques while ultrasonographic guidance has allowed for more distal injections around the ramus ventralis of the spinal nerve (16). Scientific reports on both techniques typically use the term “nerve root” for both parts of the spinal nerve. According to the Nomina Anatomica Veterinaria (2012), the nerve segment considered in this paper is the ramus ventralis.
Ultrasonography (US) is commonly used in horses for perineural/periarticular/intraarticular blocks and therapeutic infiltrations (18–21). Periarticular and intraarticular corticosteroid injections of the articular process joints have been reported to possibly improve clinical signs related to articular process arthropathy (19). Due to its clinical availability, applicability, and safety while also taking into consideration imaging techniques used in humans and their possible applicability in horses, US should constitute the guidance of choice to perform a selective caudal cervical nerve root injection in horses (16, 19, 22).
The ramus ventralis of the 7 and 8th cervical spinal nerve (C7, C8) with the 1st thoracic (T1) provides the largest roots to the equine brachial plexus with a minor contribution of the C6 and T2 nerves (23). The aim of this pilot study on cadavers was to describe the feasibility and the dye diffusion of selective perineural injection of C7 and C8 ramus ventralis under ultrasonographic guidance in horses.
Materials and Methods
The experimental protocol was reviewed and approved by the Ethical Committee for Animal Research of the ANSES/ENVA/Paris-Est Créteil University (authorization number COMETH 16-025). Four cadavers of recently euthanized horses for reasons unrelated to the study were used (storage <36 h at 4°C). They were 3 to 5 year old, 420 to 480 kg French Trotters with a similar lean neck conformation. A radiographic screening including the cervical region was available in each individual medical file. No abnormalities were found on the lateral radiographic view of their caudal cervical region (5th cervical to 1st thoracic vertebrae, C5-T1).
Ultrasonographic Technique and Landmarks
The cadavers were positioned in lateral recumbency with the side to be injected up and the uppermost forelimb retracted caudally. The cervical vertebrae C6 and C7 were located using manual palpation of the transverse process of C1 and counting segments of the width of the hand in a caudal direction as described by Mattoon et al. (18). After adequate skin preparation (hair clipping and surgical skin disinfection), a micro-convex 5–8 MHz ultrasound probe (C11x, SonoSite Edge portable ultrasound machine, FUJIFILM SonoSite France SARL) was applied to the most caudal segment to identify the C7-T1 articular process joint. The probe was oriented perpendicularly to the vertebral axis to obtain a reference image of the 2 articular processes and the joint space (22). Then to visualize a longitudinal section of C8 ramus ventralis, the probe was glided ventro-caudally with an approximate 20° angle from its initial position by orienting the uppermost edge of the probe cranially and ventrally (counter-clockwise rotation on the left side of the neck) (Figure 1). The probe was then glided along the nerve course over the vertebral body between the articular process and the transverse process to identify the best ramus ventralis longitudinal section image possible that would allow for easy needle placement and product injection monitoring on the US screen (Figure 2). A 88 mm 20G spinal needle (Spinocan, BBraun France SA) was inserted ~2 cm caudo-ventrally to the transducer and advanced “in plane” until the needle tip was <5 mm adjacent to the nerve surface. The injection of the syringe content was monitored on the US screen. The same technique was repeated one segment cranially on the C7 ramus ventralis. Localizing the best injection window by US was conditional on individual horse neck conformation and ability to optimize the cadaver neck to forelimb and shoulder position. As a result the point of injection along the ramus ventralis course was not standardized as a set distance from the articular processes. Therefore, the distance between the articular process ventral border and the needle tip was recorded. The injection was qualified as proximal if the distance was <1 cm or distal if it was within 1 to 2 cm.
Figure 1.
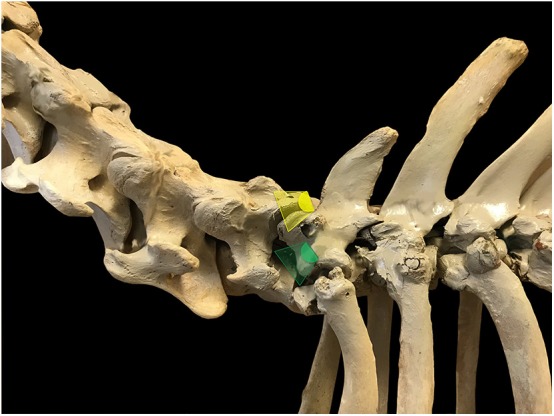
Ultrasound probe positioning and orientation to visualize C8 ramus ventralis in a longitudinal section in horses. The probe is initially oriented perpendicular to the vertebral axis to obtain a reference image of the 2 articular processes and the joint space (yellow scan field) then glided ventro-caudally with an approximate 20° angle from its initial position (counter-clockwise rotation on the left side of the neck, green scan field).
Figure 2.
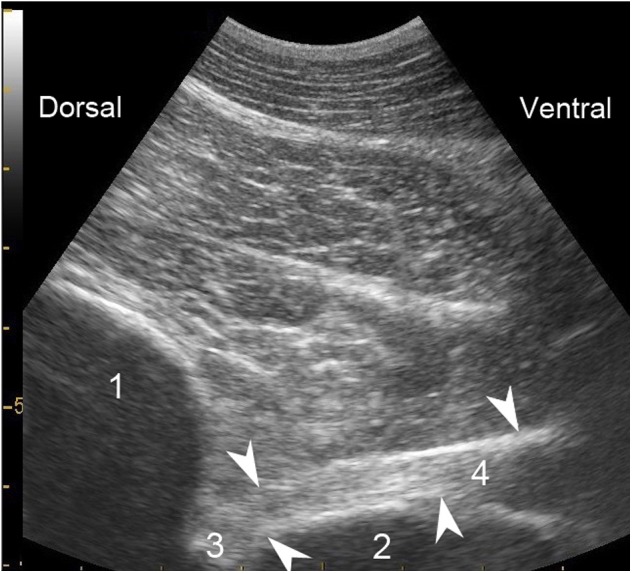
Representative longitudinal ultrasonographic section of C8 ramus ventralis in an equine cadaver. Ventrally to T1 cranial articular process, the nerve trunk (arrows) shows echogenic longitudinal fasciculi bordered by a more echogenic sheath. 1- Cranial articular process of T1; 2- Vertebral body (margin of the fossa) of C7; 3- Intervertebral foramen; 4- Ramus ventralis of C8.
Dyes and Dye Solution
Methylene blue powder (Bleu de méthylène, RAL Diagnostics, France) was used in the first three horses and reconstituted as a 0.12% solution. Following the analysis of the first results with methylene blue staining and recent scientific information on dye nerve staining (24, 25), an additional cadaver was injected with multiple color permanent marking tissue dyes (Davison Marking System; Bradley Products, Inc., MN, USA) at a 1:50 dilution (1 ml of dye in 50 ml of carrier solution).
For both dyes, the solution carriers were chosen to reproduce as much as possible an in vivo situation and a foreseen clinical study (25, 26). The solution consisted of one part iohexol (Omnipaque 300 mg/ml, GE Healthcare SAS, France) for 2.5 parts lidocaine 2% (Lidocaïne sans conservateur 20 mg/ml, Laboratoire Aguettant, France). Carrier agent respective proportions were extrapolated from similar studies (16, 26).
Dye Injection Volume and Allocation
The initial objectives of perineural injections with methylene blue solution were to observe tissue dye staining and test the injection selectivity for the ramus ventralis considering possible diffusion to the adjacent cranial and/or caudal ispilateral ramus in addition to diffusion to the epidural space across midline. Three equine cadavers stored for <36 h at 4°C were used after being at room temperature for 3 h. They received unilateral perineural ramus ventralis injections of C7 and C8 with the methylene blue solution (6 injections in toto). The use of a single dye color limited the number of injection possibilities and testing conditions. As a result and to facilitate cadaver handling and dissection, it was decided to test 2 volume conditions on the same side of the neck. While considering the ramus ventralis size difference (width of C8 1.5 to 2 times larger than C7), the two conditions tested were C7–7 ml/C8–14 ml on two horses (horse 1 and 3) and C7–7 ml/C8–7 ml on horse 2. Perineural injection volumes selected (7 and 14 ml) were extrapolated from similar studies using an allometric scale (12, 16, 26). Left and right neck injections and condition assignment for the 3 cadavers were randomly selected using a closed envelope technique.
Following the results on the 3 methylene blue cadavers and to confirm the findings, an additional cadaver received, four injections with a solution of permanent marking tissue dye within 30 min from euthanasia. The use of 4 different colors allowed to perform bilateral injections without compromising the evaluation of individual injection selectivity for each ramus ventralis. Opposite randomized conditions were tested: C7–7 ml/C8–14 ml on the left and C7–14 ml/C8–7 ml on the right.
Dissection and Nerve Staining Evaluation
The injections in the 3 methylene blue cadavers were performed one cadaver after the other on the same morning and followed by the dissection respecting the cadaver injection sequence within 1 to 3 h after the injections. Horse 4 was dissected within the same time frame, respecting the injection side order (right then left). After removing the ipsilateral forelimb and the cervical muscles attached to it, the C7 and C8 ramus ventralis were isolated from the surrounding muscles along their course from the articular processes to the brachial plexus. The vertebral canal was opened in situ on horse 1, 2, and 4. On horse 3 (C7–7 ml/C8–14 ml) in an attempt to better visualize possible dye spread to the vertebral canal, the C5 to T2 vertebral segment was isolated as one block for frozen transverse sections.
The distribution and extent of nerve staining were evaluated cranio-caudally for partial or complete transversal coloration across the nerve trunk and longitudinally, considering a staining length greater than 2 cm to be indicative of what would be a clinically effective nerve blockade (27). For horse 1, 2, and 4, epidural/subarachnoid diffusion was assessed upon opening the vertebral canal looking at the ventral and dorsal spinal nerve roots as well as the meninges around the spinal cord. The meninges were then transected longitudinally on their dorsal sagittal aspect and reclined to inspect for presence or absence of dye on the spinal cord, the spinal nerve rootlets and the arachnoid membrane. The assessment on horse 3 was done through observation of 1 cm thick transverse sections of the vertebras from C5 to T2.
Results
The ramus ventralis could be identified by US in all cadavers. Cervical segment identification was erroneous on one methylene blue cadaver (horse 1), leading to C6 and C7 ramus ventralis injections instead of C7 and C8. The 10 performed injections corresponded to 1 C6–7 ml, 3 C7–7 ml, 2 C7–14 ml, 2 C8–7 ml, and 2 C8–14 ml. Results of individual cadaver perineural ramus ventralis injections are presented in Table 1. The probe positioning adjustment to obtain an optimized ramus ventralis visualization for the injection resulted in 5 injections that were qualified as proximal and 5 as distal. All the injections were successful in staining a portion of the nerve trunk and were identified as selective for the ramus concerning their distal diffusion toward the brachial plexus. Eight ramus ventralis had a uniform complete transversal staining of the nerve trunk that longitudinally covered a distance >2 cm, of which three ramus (2 C7–7 ml, horse 2 and 4; 1 C8–14 ml, horse 3) were colored from the articular processes to the limit of the brachial plexus (Figure 3A). One C7–14 ml and one C8–7 ml ramus ventralis (horse 4 and 2 respectively) showed incomplete transverse staining with a more concentrated color on their cranial half and a longitudinal coverage of <2 cm.
Table 1.
Caudal cervical ramus ventralis perineural injections on 4 equine cadavers: injection condition allocation (neck side and injection volume), injection site along the nerve course, dye choice, and extent of diffusion.
| Cadavers |
Ramus Ventralis Left (L) or right (R) side Volume injected |
Injection site | Length of nerve staining | Epidural diffusion |
|---|---|---|---|---|
| Methylene blue dye | ||||
| Horse 1 | C6 L 7 ml | Distal | >2 cm* | No |
| Horse 1 | C7 L 14 ml | Proximal | >2 cm | Yes(+ sub-arachnoid) |
| Horse 2 | C7 L 7 ml | Distal | >2 cm* | No |
| Horse 2 | C8 L 7 ml | Proximal | <2 cm** | Yes |
| Horse 3 | C7 R 7 ml | Proximal | >2 cm | Yes (frozen sections) |
| Horse 3 | C8 R 14 ml | Distal | >2 cm* | Yes (frozen sections) |
| Permament marking tissue dye | ||||
| Horse 4 | C7 R 14 ml | Proximal | <2 cm** | No |
| Horse 4 | C8 R 7 ml | Distal | >2 cm | No |
| Horse 4 | C7 L 7 ml | Proximal | >2 cm* | Yes |
| Horse 4 | C8 L 14 ml | Distal | >2 cm | No |
Longitudinal staining of the ramus ventralis from the ventral border of the articular processes to the limit of the brachial plexus.
Incomplete transversal staining with more concentrated color on cranial half of the nerve trunk.
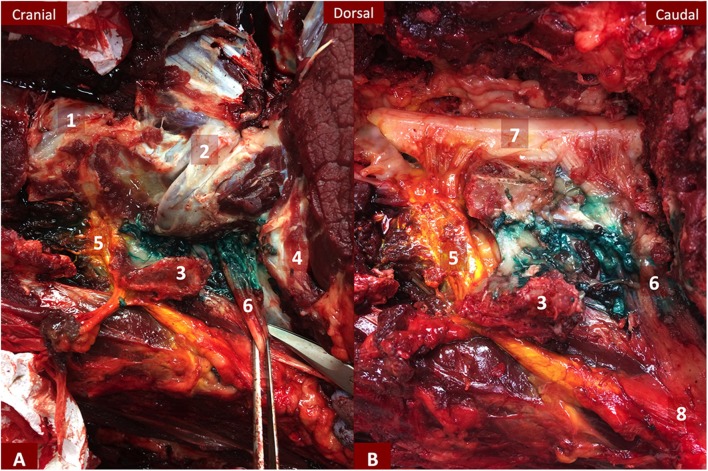
Figure 3.
(A,B) Dissection of the left C7 and C8 ramus ventralis of horse 4 after removal of the neck muscles (A) and after opening of the vertebral canal (B). C7 has an extensive yellow staining reaching the epidural space and the meninges and spreading to the limit of the brachial plexus. C8 green dye spread is delimited to the ventral aspect of the articular processes with dye diffusing dorsally to C7 transverse process. 1- Caudal articular process of C6 and cranial articular process of C7; 2- Caudal articular process of C7 and cranial articular process of T1; 3- Transverse process of C7; 4- First rib; 5- Ramus ventralis of C7; 6- Ramus ventralis of C8; 7- Spinal cord covered by the meninges; 8- Brachial plexus.
On horse 3, the ramus ventralis staining from the articular processes to the brachial plexus was evaluated in situ as with on the other cadavers but the potential epidural spread was investigated by transverse sections. Five days of freezing were required to obtain a completely frozen vertebral segment. Indeed, a first attempt at slicing the cranial edge of the isolated vertebral segment (C6 vertebra) on day three showed an incompletely frozen segment core preventing completion of the trans-section. The transverse sections presented an extensive methylene blue diffusion into the vertebral canal reaching proximal and distal vertebral segments (C6-T1) and crossing midline. Meninges, venous sinuses and surrounding vertebral bone were deeply colored. The extensive diffusion was attributed to the methylene blue propensity to diffuse in tissue over time associated with the slow freezing process (24). The evaluation technique was therefore not pursued but the data was included in the epidural spread evaluation as time would be clinically relevant.
Overall, the effect of volume was not clearly recognizable on nerve length staining nor on epidural spread likelihood. Four out of five proximal injections resulted in an epidural spread (Figure 3B), of which one showed a mixed epidural/subarachnoid diffusion, compared to only one out of five distal injections that happened to be evaluated by the frozen section. Apart from an epidural spread in the vertebral canal across midline and to the neighboring segments on the frozen sections, no dye stain was evidenced neither on the opposite side nerve nor on the proximal or distal nerve. Therefore, all injections were considered to be nerve selective regarding their proximal diffusion in the vertebral canal.
Discussion
This study evaluated the nerve coloration extent of ultrasonographically guided C7 and C8 ramus ventralis perineural injections in horses. The technique was effective in staining the entire width of the nerve trunk on a length >2 cm in eight out of ten injections.
Ultrasonographic visualization of the C7 and C8 ramus ventralis was easily achieved with a micro-convex 5–8 Mz US probe and allowed for adequate needle positioning. Some degree of rigor mortis may have precluded from ideal neck/foreleg positioning on horse 1 and, associated with the cervical segment identification method, resulted in injections of C6-C7 rami instead of C7-C8 rami. More precise methods have been described such as the use of external radio-opaque markers for cervical radiographs before US or US identification of the deep cervical artery passing caudo-dorsally to C7-T1 articular process joints (3). These methods were not applicable to the experiment settings but would be easily undertaken on standing horses in a clinical setting.
The injection site was selected individually for each nerve upon obtaining the best US visualization of the nerve trunk. As a result, needle tip positioning over the nerve trunk was close to the articular processes in five of the total ten injections, of which four out of five were C7 injections. The anatomic conformation of the C6 vertebral transverse process with a marked dorsal tubercle prevented C7 ramus ventralis distal portion visualization and may have contributed to the proximal injections. Due to its large size and width, C8 ramus ventralis was the easiest to identify in longitudinal section for an in plane US-guided injection (23). It resulted predominantly in distal injections.
The length of nerve staining >2 cm was compatible with a clinically effective blockade of nerve conduction for eight injections, of which 50% resulted in staining of the complete nerve trunk length from the articular processes to the brachial plexus (27). The absence of an identifiable volume effect has to be linked to the small sample size and the study design, main limitations of this pilot study. Interestingly, Anderberg et al. (26), while testing 3 different volumes of injection in human cadavers, found that the length of nerve staining was not correlated to the volume.
The change in epidural spreading assessment from in situ dissection to evaluation on frozen transverse sections may appear as a lack of protocol standardization. It was initially thought to be more adapted to visualize the entire vertebral canal and spinal cord compared to an in situ canal opening by a lateral window. Unexpectedly, the intense vertebral canal tissue coloration up to cortical bone, its extent across midline and to the cranial and caudal vertebrae rendered necessary to evaluate the choice of methylene blue as a dye and the effect of time on its diffusion ability in tissue.
Methylene blue has been used for nerve staining to identify nerve structures during surgery or for neurohistology as well as to document perineural injection techniques in animal cadaveric studies (16, 23, 27). Even though it is rarely mentioned in cadaveric studies, time has an effect on its extent of diffusion; this was evidenced in organ pharmacokinetics studies in rodents (24). The compound is a water-soluble cation but, at physiologic pH, it is present in tissue mostly in its reduced non-ionized lipid-soluble colorless form that has all the physical properties for extensive diffusion across tissue and cellular membrane. Moreover, exposure of dye impregnated tissue sections to air results in appearance of the blue color by oxidation. These facts may bring some explanation to the present study results, especially to the extended diffusion into the vertebral canal identified on the delayed frozen sections. The anatomic piece took more than 3 days to freeze at −20°C. It is possible to postulate that a faster freezing process may have limited this effect. It was also witnessed during the immediate cadaver dissection that the blue color spreading had a tendency to increase over time, was easily transferable to gloves and surrounding tissues if careful tissue manipulation was not applied. Similarly, the assessment of the saw sliced frozen vertebral segments allowed seeing very minimal methylene blue “smudging” but manipulation of the sections over time showed dye spreading to surrounding tissues.
The impact of dye diffusion properties and dissection approach on the assessment of an injection technique has been discussed by Portela et al. (25). Taking into account their findings and the present study results with methylene blue, it was decided to perform four more injections with the dye used by the authors, a permanent marking tissue dye designed to permanently mark tissue in less than 5 min and orient tissue specimen for surgery or histology. Different colors are available and allowed testing for injection selectivity using a single cadaver that therefore received 4 ramus ventralis perineural injections (2 C7 and 2 C8). No further expansion of the dyes was appreciable during the dissection. Used in the present study setting, it is hypothesized that the permanent marking tissue dye more accurately tested for adequate needle placement and volume diffusion compared to methylene blue. Comparison of the dissection process and dye behaviors over time during tissue manipulation lead to the thought that, with the permanent marking tissue dye, the stained area was mainly the result of the needle placement, the volume/pressure of the injection and the tissue reaction. The intrinsic diffusing property of the dye was only linked to the dilution solution and not to the dye per se. It may however represent an underestimation of drug diffusion. Nonetheless, the results on the last cadaver confirmed methylene blue findings concerning staining extent of the nerve. The injection of 7 and 14 mL with both dye solutions resulted mostly in a greater than 2 cm length staining. To confirm the suitability of the permanent marking tissue dye, further dissections reproducing the study setting including frozen section assessment are needed as well as evalutating the impact of the freezing process duration.
Apart from the delayed epidural spread on the frozen section, all the injections were considered nerve selective but may not exactly reflect drug diffusion over time in living horses. On four injections, the dye reached the limit of the brachial plexus or diffused cranio-caudally over the transverse process nearly reaching the adjacent ramus ventralis (2 dyed with methylene blue and 2 with permanent marking dye). It can be hypothesized that, with more time between the injection and the dissection, nerve selectivity would have been lost. Even though the used dye carrier solution aimed at reproducing a clinical setting, it cannot be certain that drugs would not reach the contiguous ramus ventralis or would not spread as much due to systemic resorption by the lymphatic and venous system.
Of the 10 perineural injections performed all cervical nerves considered, five injections resulted in a transforaminal diffusion into the epidural space. Four of those 5 were C7 injections and were qualified as proximal. One reached the subarachnoid space and happened to be the injection done the closest to the articular process (less than 5 mm from the articular process ventral border). Similar findings have been reported by Yamauchi et al. (16) that advocate the advantage of ultrasonographic guidance to perform an extraforaminal perineural injection without epidural spreading. The safety of transforaminal injections in humans has been questioned following recognition of major complications after accidental intradural or intra-arterial injections (17, 26, 28, 29). The study was undertaken on equine cadavers so the risk of intravascular injection and arterial wall damage could not be fully tested. Recommendations to limit the risk of complications include injecting along the nerve root distally to the articular process with a dorsal approach to the nerve, the use of US to allow for the identification of vulnerable vessels, and the use of non-particulate steroids; the absence of epidural spread in US-guided perineural corticosteroid injections have not been linked to a decreased efficacy compared to transforaminal injections in human radicular pain (16, 17).
In conclusion, the perineural injection of C7 and C8 ramus ventralis using ultrasonographic guidance may represent a feasible technique for local perineural drug delivery in horses. The results of this study suggest that a proximal injection along the nerve may favor a transforaminal diffusion reaching the epidural space while a more distal injection may target the ramus ventralis on its course over the vertebral body. The volumes (7–14 ml) appear adequate but need to be confirmed in living horses. Clinical applicability and efficacy still have to be investigated.
Data Availability Statement
All datasets generated for this study are included in the article/supplementary material.
Ethics Statement
The study was reviewed and approved by the Ethical Committee for Animal Research of the ANSES/ENVA/Paris-Est Créteil University (authorization number COMETH 16-025).
Author Contributions
GT-J and J-MD conceived the study design. GT-J, J-MD, and AT participated in data collection and analysis. GT-J, J-MD, OGe and OGa contributed to the writing of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank Luis Campoy (Department of Clinical Sciences, College of Veterinary Medicine, Cornell University, Ithaca, NY, USA) for sharing his experience in nerve dye staining.
Footnotes
Funding. The authors would like to thank the regional government Pays-de-la-Loire for funding the study.
References
- 1.Ricardi G, Dyson SJ. Forelimb lameness associated with radiographic abnormalities of the cervical vertebrae. Equine Vet J. (1993) 25:422–6. 10.1111/j.2042-3306.1993.tb02984.x [DOI] [PubMed] [Google Scholar]
- 2.Dyson SJ. Lesions of the equine neck resulting in lameness or poor performance. Vet Clin Equine. (2011) 27:417–37. 10.1016/j.cveq.2011.08.005 [DOI] [PubMed] [Google Scholar]
- 3.Denoix JM. Ataxia is not the only clinical manifestation of neck injuries. In: Proceeding of the American College of veterinary Internal Medicine ACVIM Forum Scientific Sessions. National Harbour, MD (2017). p. 300–4. [Google Scholar]
- 4.Whitwell KJ, Dyson S. Interpreting radiographs. 8: equine cervical vertebrae. Equine Vet J. (1987) 19:8–14. 10.1111/j.2042-3306.1987.tb02568.x [DOI] [PubMed] [Google Scholar]
- 5.Down SS, Henson FM. Radiographic retrospective study of the caudal cervical articular process joints in the horse. Equine Vet J. (2009) 41:518–24. 10.2746/042516409X391015 [DOI] [PubMed] [Google Scholar]
- 6.Sleutjens J, Cooley AJ, Sampson SN, Wijnberg ID, Back W, van der Kolk JH, et al. The equine cervical spine: comparing MRI and contrast-enhanced CT images with anatomic slices in the sagittal, dorsal, and transverse plane. Vet Q. (2014) 34:74–84. 10.1080/01652176.2014.951129 [DOI] [PubMed] [Google Scholar]
- 7.Caridi JM, Pumberger M, Hughes AP. Cervical radiculopathy: a review. HSS J. (2011) 7:265–72. 10.1007/s11420-011-9218-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Giambuzzi S, Pancotto T, Ruth J. Perineural injection for treatment of root-signature signs associated with lateralized disk material in five dogs (2009–2013). Frontiers Vet Sci. (2016) 3:1. 10.3389/fvets.2016.00001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moore BR, Holbrook TC, Stefanacci JD, Reed SM, Tate LP, Menard MC. Contrast-enhanced computed tomography and myelography in six horses with cervical stenotic myelopathy. Equine Vet J. (1992) 24:197–202. 10.1111/j.2042-3306.1992.tb02814.x [DOI] [PubMed] [Google Scholar]
- 10.Marks D. Cervical nerve root impingement in a horse treated by epidural injection of corticosteroids. J Vet Equine Sci. (1999) 19:399–401. 10.1016/S0737-0806(99)80304-9 [DOI] [Google Scholar]
- 11.Anderberg L, Annertz M, Brandt L, Sävel H. Selective diagnostic cervical nerve root block–correlation with clinical symptoms and MRI-pathology. Acta Neurochir. (2004) 146:559–65. 10.1007/s00701-004-0241-4 [DOI] [PubMed] [Google Scholar]
- 12.Anderberg L, Annertz M, Rydholm U, Brandt L, Sävel H. Selective diagnostic nerve root block for the evaluation of radicular pain in the multilevel degenerated cervical spine. Eur Spine J. (2006) 15:794–801. 10.1007/s00586-005-0931-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anderberg L, Annertz M, Persson L, Brandt L, Sävel H. Transforaminal steroid injections for the treatment of cervical radiculopathy: a prospective and randomised study. Eur Spine J. (2007) 16:321–8. 10.1007/s00586-006-0142-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Slipman CW, Lipetz JS, Jackson HB, Plastaras CT, Vresilovic EJ. Outcomes of therapeutic selective nerve root blocks for whiplash induced cervical radicular pain. Pain Physician. (2001) 4:167–74. [PubMed] [Google Scholar]
- 15.Slipman CW, Lipetz JS, Jackson HB, Rogers DP, Vresilovic EJ. Therapeutic selective nerve root block in the nonsurgical treatment of atraumatic cervical spondylotic radicular pain: a retrospective analysis with independent clinical review. Arch Phys Med Rehabil. (2000) 81:741–6. 10.1016/S0003-9993(00)90104-7 [DOI] [PubMed] [Google Scholar]
- 16.Yamauchi M, Suzuki D, Niiya T, Honma H, Tachibana N, Watanabe A, et al. Ultrasound-guided cervical nerve root block: spread of solution and clinical effect. Pain Med. (2011) 12:1190–5. 10.1111/j.1526-4637.2011.01170.x [DOI] [PubMed] [Google Scholar]
- 17.Jee H, Lee JH, Kim J, Park KD, Lee WY, Park Y. Ultrasound-guided selective nerve root block versus fluoroscopy-guided transforaminal block for the treatment of radicular pain in the lower cervical spine: A randomized, blinded, controlled study. Skeletal Radiol. (2012) 42:69–78. 10.1007/s00256-012-1434-1 [DOI] [PubMed] [Google Scholar]
- 18.Mattoon JS, Drost WT, Grguric MR, Auld DM, Reed SM. Technique for equine cervical articular process joint injection. Vet Radiol Ultrasound. (2004) 45:238–40. 10.1111/j.1740-8261.2004.04042.x [DOI] [PubMed] [Google Scholar]
- 19.Birmingham SSW, Reed SM, Mattoon JS, Saville WJ. Qualitative assessment of corticosteroid cervical articular facet injection in symptomatic horses. Equine Vet Educ. (2010) 22 77–82. 10.2746/095777309X477852 [DOI] [Google Scholar]
- 20.Denoix JM, Jacquet S. Ultrasound-guided injections of the sacroiliac area in horses. Equine Vet Educ. (2008) 20:203–7. 10.2746/095777308X292128 [DOI] [Google Scholar]
- 21.Morath U, Luyet C, Spadavecchia C, Stoffel MH, Hatch GM. Ultrasound-guided retrobulbar nerve block in horses: a cadaveric study. Vet Anaesth Analg. (2013) 40:205–11. 10.1111/j.1467-2995.2012.00780.x [DOI] [PubMed] [Google Scholar]
- 22.Nielsen JV, Berg LC, Thoefner MB, Thomsen PD. Accuracy of ultrasound-guided intra-articular injection of cervical facet joints in horses: a cadaveric study. Equine Vet J. (2003) 35:657–61. 10.2746/042516403775696366 [DOI] [PubMed] [Google Scholar]
- 23.Barone R, Simoens S. Chapitre II: Nerfs Spinaux. In: Anatomie Comparée des Mammifères Domestiques, Tome 7 Neurologie II Système Nerveux Périphérique, Glandes Endocrines, Esthésiologie. Paris: Ed Vigot; (2010). p. 149–320. [Google Scholar]
- 24.Oz M, Lorke DE, Hasan M, Petroianu GA. Cellular and molecular actions of methylene blue in the nervous system. Med Res Rev. (2011) 31:93–117. 10.1002/med.20177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Portela DA, Campoy L, Otero PE, Martin-Flores M, Gleed RD. Ultrasound-guided thoracic paravertebral injection in dogs: a cadaveric study. Vet Anesth Analg. (2017) 40:205–11. 10.1016/j.vaa.2016.05.012 [DOI] [PubMed] [Google Scholar]
- 26.Anderberg L, Sävel H, Annertz M. Distribution patterns of transforaminal injections in the cervical spine evaluated by multi-slice computed tomography. Eur Spine J. (2006) 15:1465–71. 10.1007/s00586-005-0024-5 [DOI] [PubMed] [Google Scholar]
- 27.Campoy L, Martin-Flores M, Looney AL, Erb HN, Ludders JW, Stewart JE, et al. Distribution of a lidocaine-methylene blue solution staining in the brachial plexus, lumbar plexus and sciatic nerve blocks in dogs. Vet Anaesth Analg. (2008) 35:348–54. 10.1111/j.1467-2995.2007.00390.x [DOI] [PubMed] [Google Scholar]
- 28.Hodler J, Boos N, Schubert M. Must we discontinue selective cervical nerve root blocks? Report of two cases and review of the litterature. Eur Spine J. (2013) 22(Suppl. 3):S466–70. 10.1007/s00586-012-2642-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huston CW, Slipman CW, Garvin C. Complications and side effects of cervical and lumbosacral selective nerve root injections. Arch Phys Med Rehab. (2005) 86:277–83. 10.1016/j.apmr.2004.02.018 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All datasets generated for this study are included in the article/supplementary material.