Abstract
Asthma is a disease characterized by chronic airway inflammation, leading to intermittent symptoms of wheeze, dyspnea, cough and chest tightness in combination with variable expiratory airway obstruction. Clinical diagnosis is usually established based on the presence of symptoms and documented variability in expiratory airflow limitation as measured by pulmonary function testing. Presently, asthma is a major chronic disease affecting approximately 334 million people worldwide. The epidemic spares no age group, race or ethnicity; however ethnicity and socioeconomic status do influence the prevalence, morbidity and mortality of asthma in the United States and various countries throughout the world. Moreover, asthma places a huge burden at the societal, financial and health-care levels of multiple nations.
Introduction
Asthma is a disease characterized by chronic airway inflammation, leading to intermittent symptoms of wheeze, dyspnea, cough and chest tightness in combination with variable expiratory airway obstruction [1]. Clinical diagnosis is usually established based on the presence of symptoms and documented variability in expiratory airflow limitation as measured by pulmonary function testing [2]. Presently, asthma is a major chronic disease affecting approximately 334 million people worldwide [3]. The epidemic spares no age group, race or ethnicity; however ethnicity and socioeconomic status do influence the prevalence, morbidity and mortality of asthma in the United States and various countries throughout the world [4]. Moreover, asthma places a huge burden at the societal, financial and health-care levels of multiple nations [2,5,6,7].
Asthma is more common in children and the leading cause of chronic airway disease; however, new onset disease can occur at any age [2,8,9]. With increasing age, it becomes more difficult to differentiate adult onset asthma from other diagnoses such as chronic obstructive pulmonary disease (COPD) or Asthma-COPD overlap syndrome (ACOS), leading to frequent under or misdiagnosis [2,7,10]. However, distinguishing between asthma, COPD and ACOS is important, not only to ensure appropriate treatment, but also for risk stratification as patients with ACOS have more exacerbations and worse prognosis [2].
Global Epidemiology of Asthma
Accurately estimating the incidence and prevalence of asthma on a global scale is challenging because the diagnosis is often based on survey responses to questions about relatively non-specific symptoms which are open to subjective interpretation [11,12,13]. A recent multicenter cohort study conducted in Canada that enrolled 701 randomly selected adults with physician-diagnosed asthma, showed that current asthma could not be confirmed in 33% of patients [14]. Moreover, there is no universally accepted definition nor is there a single test to definitively diagnose asthma [4]. Additionally, asthma has been increasingly recognized as a heterogeneous disease comprised of both allergic and non-allergic phenotypes, a feature not captured in prior surveys.
Despite these limitations, validated tools for asthma diagnosis are available. The International Study of Asthma and Allergy in Childhood validated questionnaire, which was used in 56 countries among children aged 6 to 14 years, is one of the frequently used tools for identifying asthma in children [13,15]. Similarly, a validated instrument for adults is based on the European Community Respiratory Health Survey questionnaire [11,13]. In the United States, the National Health Interview Survey (NHIS) conducted by the Centers for Disease Control and Prevention (CDC) routinely collects data about prevalence using self-reported symptoms (such as history of wheezing) using validated measures [16].
Prior studies have shown that the prevalence of asthma ranges from 15% to 20% in many countries, especially in the developed nations [12,13]. In the United States (US), the current prevalence of asthma among adults is approximately 7.6%, but rates vary dramatically among different ethnic groups. Prevalence is 9.1% among Black non-Hispanics and 13.6% among Puerto Ricans but only approximately 5% for Mexican and Asians [16,17]. Internationally, most data on ethnic-related differences in asthma prevalence come from the United Kingdom (UK) or Canada. Netuveli et al. reported similar rates of asthma, but increased risk for admissions, among black and South Asian populations in the UK [18,19]. Wang et al. found that Chinese children born in Canada had higher rates of asthma than those who were born in China [20].
The World Health Survey (WHS), a standardized questionnaire designed by the World Health Organization (WHO), collected data on the prevalence of several medical conditions in adults aged 18–45 years from multiple countries around the world (Figure 1). Countries with the highest prevalence of clinical asthma were Australia (21.5%), Sweden (20.2%), UK (18.2%), Netherlands (15.3%) and Brazil (13.0%); however, the US and Canada were excluded [21]. The lowest rates were observed in Vietnam (1.0%), Bosnia-Herzegovina (1.4%), and China (1.4%) [21]. The higher prevalence observed in more developed countries may be due to increased urbanization/westernized lifestyle, higher rates of obesity, and/or pollution.
Figure 1.
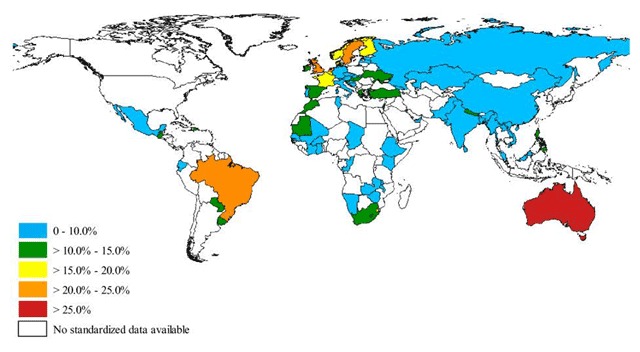
Prevalence of symptoms of asthma in the past 12 months among persons aged 18 to 45 years in 70 countries, Worlds Health Survey 2002–2003.
Source: To T, et al. BMC Public Health 2012.
The lower asthma prevalence rates in Asia and Africa, are thought to be more related to environmental and lifestyle causes than genetic differences [15]. Individuals who reside in developed countries have a higher asthma prevalence compared to their counterparts with similar genetic predispositions but who live in developing countries or immigrated at an older age [15]. Other hypotheses that could explain lower prevalence in developing countries like China, include the lower rates of atopy, more breastfeeding, larger household size and sometimes, rural residency during childhood [6]. The “hygiene hypothesis” which has been implicated in lowering the risk of asthma, suggests that exposure to microbes and higher rates of cross infection early in life can activate type 1 helper cells, thus offsetting inflammatory pathways associated with asthma development. Conversely, improved hygiene leads to higher rates of asthma by reducing early exposure to infections [6,22]. As documented by WHO’s Study on Ageing and Adult Health (SAGE), there is substantial under-diagnosis of asthma in some less developed countries like India and Mexico, a factor that may also potentially explain lower prevalence rates compared to more developed nations [23].
Trends suggest increasing asthma prevalence globally, with an anticipated 100 million new cases in the next decade [5,24,25,26]. According to the National Center for Health Statistics, the total prevalence of asthma in US adults increased from 7.3% to 8.4% from 2001 to 2010; similar patterns have been observed among children [27,28,29]. Multiracial individuals, women, children and people of low socioeconomic status are the groups at higher risk of asthma [13,27]. Notably, there was a wide racial disparity in incidence during 2001 to 2007, with Non-Hispanic black and Mexican-American children having significantly increased rates of asthma [29]. Fortunately, more recent data suggest possible changes in these trends with decreasing childhood asthma rates and a reduction in black-white racial disparities in asthma morbidity in the US [29].
Patterns of asthma prevalence in European countries have been mixed. In Italy, De Marco, et al. reported a 35% increase in asthma prevalence in adults aged 20–44 years [30]. A parental survey for Greek schoolchildren showed an increase in asthma from 1991 to 2003 with a subsequent plateau in 2003 to 2008 [31]. Similar patterns have been reported in the Netherlands and Norway [32,33]. Conversely, a study of the UK National Health database found that the incidence of asthma was decreasing, especially in children, while lifetime asthma rates for adults continued to increase [34]. Several studies have reported increasing rates of asthma in less developed countries in Asia and Africa. Factors such as smoking, urbanization and increasing population, ingestion of seafood, and presence of moist air with subsequent mold and mildew formation, have been proposed as mechanisms explaining these trends [35,36].
Morbidity and Mortality
Mortality from asthma is low compared to other chronic diseases and accounts for less than 1% of deaths globally. However, given the high prevalence worldwide, asthma is still responsible for 250,000 potentially preventable deaths annually [3,8,13,26]. In the US, mortality is highest among African Americans and Puerto Ricans and individuals of Cuban descent [37]. According to the WHO mortality database, South Africa had the highest age-standardized asthma mortality among the low and middle-income countries, while Netherlands had the lowest among the high-income countries [3,35] (Figure 2).
Figure 2.
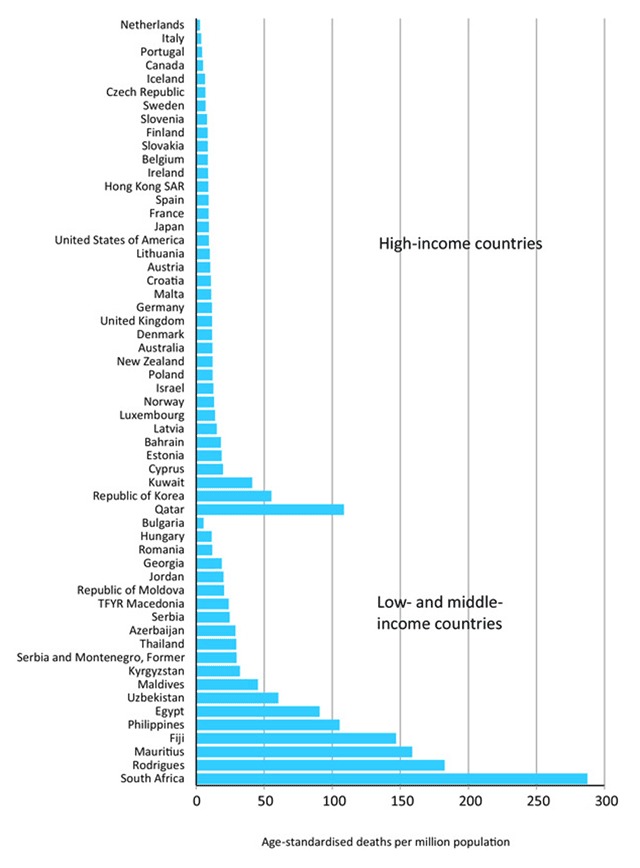
Age-standardised asthma mortality rates for all ages 2001–2010 from countries where asthma is separately coaded as a cause of death, ordered by mortality rate and country income group.*
Source: WHO Detailed Mortality Database, February 2014 update.
Though the mortality is low, asthma still leads to frequent acute healthcare resource utilization. Asthma is the 28th cause of loss of years in full health [11]. In the US alone, asthma exacerbations account for approximately two million emergency room visits each year [37]. Disease control plays a role in frequent emergency room visits as patients with severe persistent disease, while representing only 5% of the asthma population, consume over half of asthma-related resources [38,39]. Ironically, these patients only represent 5% of the asthma population [39]. Similar findings of increased healthcare utilization have been shown in Asia; in a survey-based study on over 3,000 adults and children, more than 40% of participants had at least one hospitalization or emergency room visit for asthma exacerbation. Both hospitalizations and emergency room visits were correlated with increasing level of severity [15]. Similarly, a Spanish study found that the 4% of patients with severe persistent asthma had considerable higher healthcare utilization than patients with a moderate disease [38]. On a global scale, better disease control would likely reduce associated economic costs since emergency room visits and hospitalizations account for most of the asthma-related expenses [15].
Asthma also accounts for the loss of over 15 million disability adjusted life years (DALY) annually and ranks among the highest causes of DALY for children [6,7,8]. Children aged 10–14 years, followed by elderly patients have the highest DALYs [3]. Conversely, adults aged 30–34 years have the least disability from the disease.
Morbidity due to asthma is underappreciated in the elderly. Asthma affects 7–9% of the US population older than 65 years, and causes substantial morbidity, as older adults are four times more likely to die from asthma [40,41,42]. Moreover, elderly patients have twice the risk of hospitalization and experience longer asthma-related hospital stays [43,44]. There is limited data on the prevalence of asthma in the elderly population worldwide due to lack of consensus on diagnostic criteria and diagnostic challenges due to comorbidities [3,10]. Thus, additional population-based studies are needed to better characterize the extent of this problem globally.
Cost of Asthma Care
Among chronic diseases, asthma is one of the main contributors to increased health care expenditures (Table 1) [39,45]. The costs of asthma care can be direct monetary or indirect [45,46]. Office visits, hospitalizations, emergency room visits, cost of tests and medications all contribute to direct costs [45]. In the US, an estimated $1,500 is spent per emergency room visit [47], and over $3,000 is spent per year per patient on medical expenses alone [48]. This is in contrast to PLN$251 (approximately US$63) spent on medications in Poland in 2012 [49,50]. Conversely, Canadian patients with mild to moderate asthma are estimated to spend CAD$134 per three months (approximately US$103) on asthma care, mostly on outpatient treatment [50,51]. Indirect costs include missed work days, waiting times and productivity loss [45,46,52,53]. Ojeda et al. estimated that adults had 1.5 missed days per month due to asthma symptoms and 4.9 days per month of reduced productivity [52]. Uncontrolled asthma causes more lost productivity compared to patients with well-controlled symptoms, with a loss of approximately CAD$286 (US$219) per week [50,54]. In Spain, approximately 285 Euros (US$315) were attributed to lost workdays per patient each month [50,52].
Table 1.
Annual Direct Costs of Asthma Care in US$ and by Severity of Illness.
| Category | Mild disease (n = 140) | Moderate disease (n = 116) | Severe disease (n = 77) | Total (n = 333) | |
|---|---|---|---|---|---|
| Drugs | 253 ± 276 | * | 473 ± 310 | 559 ± 340 | 400 ± 329 |
| General Practitioner Visits | 18 ± 23 | 26 ± 27 | 39 ± 34 | 26 ± 29 | |
| Specialist Visits | 60 ± 56 | 81 ± 142 | 82 ± 119 | 72 ± 107 | |
| Hospitalization | 119 ± 501 | * | 366 ± 927 | 480 ± 1247 | 289 ± 884 |
| Emergency Room Visits | 35 ± 75 | 58 ± 95 | 75 ± 119 | 52 ± 95 | |
| Diagnostic Tests | 48 ± 74 | 46 ± 74 | 42 ± 77 | 46 ± 76 | |
| Total | 533 ± 833 | * | 1050 ± 1323 | 1277 ± 1703 | 885 ± 813 |
Data are mean +/– SD. *p < 0.05 for differences according to severity of disease.
Adapted from Serra-Battles J, et al. Eur Resp J. 1998; 12: 1322–1326.
Many countries do not collect data on costs of asthma, especially low- and middle-income nations whose focus is primarily on infectious disease surveillance [55]. In 2009, a systematic review on the economic burden of asthma assessed 68 studies including data from the US, Canada, Europe, and Asia. Hospitalization and medication costs accounted for most of direct costs while work and school loss comprised the majority of the indirect costs [45]. However, the most recent Global Strategy for Asthma Management and Prevention (GINA) report describe that on a global scale, medication cost is the main contributor to asthma expenditures [56].
Some patient-related factors that have been implicated in higher asthma care costs include level of literacy, knowledge, beliefs, increased disease severity, poor asthma control, presence of multiple comorbidities and female sex [45]. Institutional factors that can contribute to higher asthma costs include admission to teaching or referral hospitals and intensive care unit use [45]. These findings can be due to the fact that these institutions provide care for more ill, complex patients which could lead to longer hospital days and higher need for expensive medications resulting in higher charges [45].
Strategies to Reduce Asthma Burden
Strategies have been implemented globally to reduce asthma burden [3]. In 2013, approximately 25% of countries worldwide reported having some form of national plan for adults and/or children suffering from asthma [3]. Implementation of a national plan seems to be beneficial as demonstrated by Finland, a country estimated to have saved 300-600 million Euros a year after instituting a national initiative for asthma control [3]. This 10-year program involved a multidisciplinary approach including physicians, nurses and pharmacists [57]. It focused on educating primary care providers on asthma being an inflammatory disease, thus requiring early appropriate treatment [57]. The adoption led to practice changes among healthcare providers including routine use of peak flow monitoring, early identification and treatment and pharmacist’s education on proper inhalation technique [57]. These measures led to a decreased emergency room visits by 24%, a 54% reduction in hospital days and 76% drop in asthma-related disability [57]. Other successful results have been documented in Poland, Brazil, and Portugal [3].
In an effort to improve lung health, the Global Alliance against Chronic Respiratory Diseases (GARD) has set up guidelines to address asthma and other chronic respiratory diseases which include: determining disease burden, increasing awareness, formulating simple, affordable, and feasible policies, as well as identifying evidence-based strategies that can be easily disseminated [25]. The strategies developed by the Global Initiative for Asthma also include updating the diagnosis and treatment of asthma and modifying guideline recommendations to the local needs [2]. It is important to focus on attainable goals, frequently reviewing and modifying them to fit the problems for the particular country of interest [2,3]. Limited knowledge by both providers and patients, clinician’s busy schedules and unwillingness to adopt new measures, inadequate resources, and patient’s cultural beliefs are a few potential barriers that can prevent implementation of these strategies [2,3]. Creating work groups that includes various stake holders, including patients and providers, may help address knowledge gaps [2].
Conclusions
Asthma is still a highly prevalent chronic disease that contributes to preventable healthcare resource utilization throughout the world. Prevalence remains high especially in developed countries and may be increasing in some low and middle-income countries. However, as many countries do not report prevalence or do not have accurate statistics, the true global burden of asthma is difficult to determine. Thankfully, mortality due to asthma is low; however, morbidity is a major problem. The most severe asthma patients account for the greatest expenditures including hospitalizations and emergency room visits. Global health organizations have identified strategies to lower asthma burden, but barriers to implementation, such as providers’ insufficient knowledge of recommendations, inertia, and lack of time and resources, remain a challenge.
Competing Interests
The authors have no competing interests to declare.
References
- 1.Reddel HK, Bateman ED, Becker A, et al. A summary of the new GINA strategy: A roadmap to asthma control. Eur Respir J. 2015; 46(3): 622–639. DOI: 10.1183/13993003.00853-2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GINA. From the global strategy for asthma management and prevention, Global initiative for asthma (GINA) 2015; http://www.ginasthma.org/ Updated 2015. Accessed December 12, 2015.
- 3.Global Asthma Report. The global asthma report 2014. 2014; 1–96. [Google Scholar]
- 4.Lugogo N and Kraft M. Epidemiology of Asthma. Clinics in Chest Medicine. 2006; 27(1): 1–15. DOI: 10.1016/j.ccm.2005.10.006 [DOI] [PubMed] [Google Scholar]
- 5.Ferkol T and Schraufnagel D. The global burden of respiratory disease. Ann Am Thorac Soc. 2014; 11(3): 404–406. DOI: 10.1513/AnnalsATS.201311-405PS [DOI] [PubMed] [Google Scholar]
- 6.Wang D, Xiao W, Ma D, et al. Cross-sectional epidemiological survey of asthma in jinan, china. Respirology. 2013; 18(2): 313–322. DOI: 10.1111/resp.12005 [DOI] [PubMed] [Google Scholar]
- 7.Postma DS and Rabe KF. The asthma-COPD overlap syndrome. N Engl J Med. 2015; 373(13): 1241–1249. DOI: 10.1056/NEJMra1411863 [DOI] [PubMed] [Google Scholar]
- 8.Asher I and Pearce N. Global burden of asthma among children. Int J Tuberc Lung Dis. 2014; 18(11): 1269–1278. DOI: 10.5588/ijtld.14.0170 [DOI] [PubMed] [Google Scholar]
- 9.Alith MB, Gazzotti MR, Montealegre F, Fish J, Nascimento OA and Jardim JR. Negative impact of asthma on patients in different age groups. J Bras Pneumol. 2015; 41(1): 16–22. DOI: 10.1590/S1806-37132015000100003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scichilone N, Pedone C, Battaglia S, Sorino C and Bellia V. Diagnosis and management of asthma in the elderly. Eur J Intern Med. 2014; 25(4): 336–342. DOI: 10.1016/j.ejim.2014.01.004 [DOI] [PubMed] [Google Scholar]
- 11.Burney P, Jarvis D and Perez-Padilla R. The global burden of chronic respiratory disease in adults. Int J Tuberc Lung Dis. 2015; 19(1): 10–20. DOI: 10.5588/ijtld.14.0446 [DOI] [PubMed] [Google Scholar]
- 12.Sears MR. Trends in the prevalence of asthma. Chest. 2014; 145(2): 219–225. DOI: 10.1378/chest.13-2059 [DOI] [PubMed] [Google Scholar]
- 13.Baiz N and Annesi-Maesano I. Is the asthma epidemic still ascending? Clin Chest Med. 2012; 33(3): 419–429. DOI: 10.1016/j.ccm.2012.06.001 [DOI] [PubMed] [Google Scholar]
- 14.Aaron SD, Vandemheen KL, Boulet LP, et al. Overdiagnosis of asthma in obese and nonobese adults. CMAJ. 2008; 179(11): 1121–1131. DOI: 10.1503/cmaj.081332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wong GW, Leung TF and Ko FW. Changing prevalence of allergic diseases in the Asia-Pacific region. Allergy Asthma Immunol Res. 2013; 5(5): 251–257. DOI: 10.4168/aair.2013.5.5.251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.CDC. Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. National Health Interview Survey (NHIS) data. https://www.cdc.gov/asthma/nhis/2015/table4-1.htm Updated 2015. Accessed April 11, 2017.
- 17.National Health Statistics Reports Number 32. January 12, 2011, CDC. https://www.cdc.gov/nchs/data/nhsr/nhsr032.pdf. Accessed July 28, 2017.
- 18.Netuveli G, Hurwitz B, et al. Ethnic variations in UK asthma frequency, morbidity, and health-service use: A systematic review and meta-analysis. Lancet. 2005; 365(9456): 312–317. DOI: 10.1016/S0140-6736(05)70195-1 [DOI] [PubMed] [Google Scholar]
- 19.Sheikh A, Steiner MFC, et al. Ethnic variations in asthma hospital admission, readmission and death: A retrospective, national cohort study of 4.62 million people in Scotland. BMC Medicine. 2016; 14: 3 DOI: 10.1186/s12916-015-0546-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang H, Wong GWK, et al. Prevalence of asthma among Chinese adolescents living in Canada and in China. CMAJ. 2008; 179(11): 1133–1142. DOI: 10.1503/cmaj.071797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.To T, Stanojevic S, Moores G, et al. Global asthma prevalence in adults: Findings from the cross-sectional world health survey. BMC Public Health. 2012; 12: 204 DOI: 10.1186/1471-2458-12-204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khan AA, Tanzil S, Jamali T, et al. Burden of asthma among children in a developing megacity: Childhood asthma study, Pakistan. J Asthma. 2014; 51(9): 891–899. DOI: 10.3109/02770903.2014.930882 [DOI] [PubMed] [Google Scholar]
- 23.Arokiasamy P, et al. Chronic noncommunicable diseases in 6 low- and middle-income countries: Findings from wave 1 of the World Health Organization’s study on global ageing and adult health (SAGE). Am J of Epidemiology. 2017; 185(6): 414–428. DOI: 10.1093/aje/kww125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chuchalin AG, Khaltaev N, Antonov NS, et al. Chronic respiratory diseases and risk factors in 12 regions of the Russian federation. Int J Chron Obstruct Pulmon Dis. 2014; 9: 963–974. DOI: 10.2147/COPD.S67283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.WHO. Global surveillance, prevention and control of chronic respiratory diseases: A comprehensive approach; 2007. Available at: who.int/respiratory/publications/global_surveillance/en. Accessed 5 May 2017.
- 26.Schluger NW and Koppaka R. Lung disease in a global context. A call for public health action. Ann Am Thorac Soc. 2014; 11(3): 407–416. DOI: 10.1513/AnnalsATS.201312-420PS [DOI] [PubMed] [Google Scholar]
- 27.Akinbami LJ, Moorman JE, Bailey C, et al. Trends in asthma prevalence, health care use, and mortality in the united states, 2001–2010. NCHS Data Brief. 2012; 94: 1–8. [PubMed] [Google Scholar]
- 28.Moorman JE, Akinbami LJ, Bailey CM, et al. National surveillance of asthma: United States, 2001–2010. Vital Health Stat 3. 2012; 35: 1–58. [PubMed] [Google Scholar]
- 29.Akinbami LJ, Simon AE and Rossen LM. Changing trends in asthma prevalence among children. Pediatrics. 2016; 137(1): 1–7. DOI: 10.1542/peds.2015-2354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.de Marco R, Cappa V, Accordini S, et al. Trends in the prevalence of asthma and allergic rhinitis in Italy between 1991 and 2010. Eur Respir J. 2012; 39(4): 883–892. DOI: 10.1183/09031936.00061611 [DOI] [PubMed] [Google Scholar]
- 31.Anthracopoulos MB, Fouzas S, et al. Prevalence trends of rhinoconjunctivitis, eczema, and atopic asthma in Greek schoolchildren: Four surveys during 1991–2008. Allergy Asthma Proc. 2011; 32(6): 56–62. DOI: 10.2500/aap.2011.32.3504 [DOI] [PubMed] [Google Scholar]
- 32.de Korte-de Boer D, Mommers M, et al. Stabilizing prevalence trends of eczema, asthma and rhinoconjunctivitis in Dutch schoolchildren (2001–2010). Allergy. 2015; 70(12): 1669–1673. DOI: 10.1111/all.12728 [DOI] [PubMed] [Google Scholar]
- 33.Hansen TE, Evjenth B and Holt J. Increasing prevalence of asthma, allergic rhinoconjunctivitis and eczema among schoolchildren: Three surveys during the period 1985–2008. Acta Paediatrica. 2013; 102(1): 47–52. DOI: 10.1111/apa.12030 [DOI] [PubMed] [Google Scholar]
- 34.Sheikh A and Simpson CR. Trends in the epidemiology of asthma in England: A national study of 333,294 patients. Journal of the Royal Society of Medicine. 2010; 103(3): 98–106. DOI: 10.1258/jrsm.2009.090348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Adeloye D, Chan KY, Rudan I and Campbell H. An estimate of asthma prevalence in Africa: A systematic analysis. Croat Med J. 2013; 54(6): 519–531. DOI: 10.3325/cmj.2013.54.519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lin R, Guan R, Liu X, Zhao B, Guan J and Lu L. Significant rise of the prevalence and clinical features of childhood asthma in Qingdao China: Cluster sampling investigation of 10,082 children. BMC Public Health. 2014; 14: 1002 DOI: 10.1186/1471-2458-14-1002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kenyon N, Zeki AA, Albertson TE and Louie S. Definition of critical asthma syndromes. Clin Rev Allergy Immunol. 2015; 48(1): 1–6. DOI: 10.1007/s12016-013-8395-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Quirce S, Plaza V, Picado C, Vennera M and Casafont J. Prevalence of uncontrolled severe persistent asthma in pneumology and allergy hospital units in Spain. J Investig Allergol Clin Immunol. 2011; 21(6): 466–471. [PubMed] [Google Scholar]
- 39.Al Efraij K and FitzGerald JM. Current and emerging treatments for severe asthma. Journal of Thoracic Disease. 2015; 7(11): E522–E525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.ALA. Trends in asthma morbidity and mortality. September 2012. Available at: http://www.lung.org/assets/documents/research/asthma-trend-report.pdf. Accessed 5 May 2017.
- 41.Moorman JE and Mannino DM. Increasing U.S. asthma mortality rates: Who is really dying? J Asthma. 2001; 38(1): 65–71. DOI: 10.1081/JAS-100000023 [DOI] [PubMed] [Google Scholar]
- 42.Moorman JE, Rudd RA, et al. National surveillance for asthma—United States—1980–2004. October 19, 2007; 56(SS08): 1–14, 18–54. [PubMed] [Google Scholar]
- 43.Hartert TV, Speroff T, Togias A, et al. Risk factors for recurrent asthma hospital visits and death among a population of indigent older adults with asthma. Ann Allergy Asthma Immunol. 2002; 89(5): 467–473. DOI: 10.1016/S1081-1206(10)62083-2 [DOI] [PubMed] [Google Scholar]
- 44.Cydulka RK, McFadden ER, Emerman CL, Jr., Sivinski LD, Pisanelli W and Rimm AA. Patterns of hospitalization in elderly patients with asthma and chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1997; 156(6): 1807–1812. DOI: 10.1164/ajrccm.156.6.9611008 [DOI] [PubMed] [Google Scholar]
- 45.Bahadori K and Doyle-Waters M. Economic burden of asthma: A systematic review. BMC Pulm Med. 2009; 9: 24 BMC Pulmonary Medicine BMC series. DOI: 10.1186/1471-2466-9-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Maslan J and Mims JW. What is asthma? Pathophysiology, demographics, and health care costs. Otolaryngol Clin North Am. 2014; 47(1): 13–22. DOI: 10.1016/j.otc.2013.09.010 [DOI] [PubMed] [Google Scholar]
- 47.Wang T, Srebotnjak T, Brownell J and Hsia RY. Emergency department charges for asthma-related outpatient visits by insurance status. J Health Care Poor Underserved. 2014; 25(1): 396–405. DOI: 10.1353/hpu.2014.0051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.CDC. Asthma in the US. http://www.cdc.gov/vitalsigns/asthma/ Updated 2011. Accessed April 1, 2016.
- 49.Jahnz-Rozyk K, Kucharczyk A, Warchol M, Radziwilska-Muc A, Wladysiuk M and Plisko R. The costs of asthma in Poland in 2012. Pol Merkur Lekarski. 2015; 39(230): 91–95. [PubMed] [Google Scholar]
- 50.Fx Currency Exchange. Foreign currency exchange rates and currency converter calculator. http://www.fx-exchange.com/ Updated 2016. Accessed April 1, 2016.
- 51.Sadatsafavi M, Chen W, Tavakoli H, et al. Saving in medical costs by achieving guideline-based asthma symptom control: A population-based study. Allergy. 2016; 71(3): 371–377. DOI: 10.1111/all.12803 [DOI] [PubMed] [Google Scholar]
- 52.Ojeda P, Sanz de Burgoa V, Coste Asma Study. Costs associated with workdays lost and utilization of health care resources because of asthma in daily clinical practice in Spain. J Investig Allergol Clin Immunol. 2013; 23(4): 234–241. [PubMed] [Google Scholar]
- 53.Pearce N, Asher I, Billo N, et al. Asthma in the global NCD agenda: A neglected epidemic. Lancet Respir Med. 2013; 1(2): 96–98. DOI: 10.1016/S2213-2600(13)70023-7 [DOI] [PubMed] [Google Scholar]
- 54.Moullec G, FitzGerald JM, Rousseau R, Chen W, Sadatsafavi M and Economic Burden of Asthma (EBA) study team. Interaction effect of psychological distress and asthma control on productivity loss? Eur Respir J. 2015; 45(6): 1557–1565. DOI: 10.1183/09031936.00141614 [DOI] [PubMed] [Google Scholar]
- 55.Nunes C, Pereira AM and Morais-Almeida M. Asthma costs and social impact. Asthma Research and Practice. 2017. January 6; 3: 1 DOI: 10.1186/s40733-016-0029-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.2017 GINA Report. Global Strategy for Asthma Management and Prevention available at: ginasthma.org/2017-gina-report-global-strategy-for-asthma-management-and-prevention. Accessed May 5, 2017.
- 57.Haahtela T, Tuomisto LE, Pietinalho A, et al. A 10-year asthma programme in Finland: Major change for the better. Thorax. 2006; 61(8): 663–670. DOI: 10.1136/thx.2005.055699 [DOI] [PMC free article] [PubMed] [Google Scholar]


