INTRODUCTION
Over two decades ago, an association between mast cell degranulation, histamine release, and bladder nerve hypersensitivity was first identified by researchers trying to determine the cause of a persistent urinary bladder dysfunction now known as interstitial cystitis/bladder pain syndrome (IC/BPS) (8, 14). Further studies determined that the association between histamine and bladder dysfunction was not limited to IC/BPS. Stress, allergies, peripheral neuropathy, and genetic abnormalities caused an increase in histamine concentration and mast cell number in plasma, urine, and tissue that associated with symptoms of overactive bladder (2, 4, 7, 12). Researchers and clinicians used this association to probe for a possible mechanism under the holistic lens of “neurogenic inflammation,” which encompassed a variety of complicated and confounding pathways by which histamine could potentially act to release neuropeptides and bidirectionally activate mast cells within the bladder (1, 5, 6, 9–11). Recent publications have identified differential expression of histamine receptors in the urinary bladder in patients with IC/BPS (13), again suggesting an important role for histamine signaling in bladder function but still without identifying a testable mechanism.
HISTAMINE AND THE REGULATION OF BLADDER FUNCTION AND SENSATION
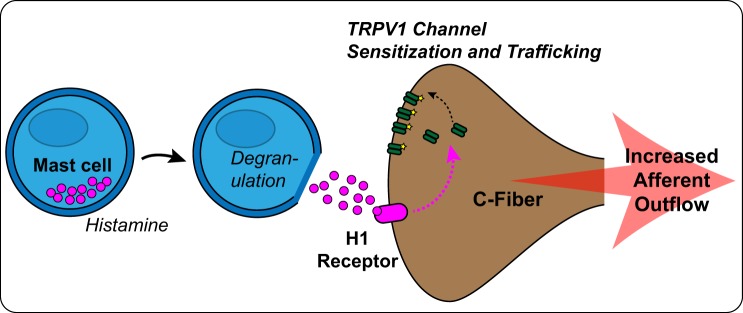
It is well known that histamine’s actions in terms of allergic responses are multifaceted, but little is known about its roles in the context of regulating bladder function and sensation. In an article recently published in the American Journal of Physiology-Renal Physiology, Grundy et al. (3) finally cracked the code, elegantly identifying a direct mechanism of action by which histamine leads to sensory nerve hypersensitivity during bladder distension (Fig. 1). They determined that specific populations of sensory nerves within the bladder can be directly sensitized or recruited by histamine to augment mechanosensation during bladder filling. This happens through the direct activation of histamine H1 receptors, which sensitizes transient receptor potential vanilloid type 1 (TRPV1) channels and recruits them to the membrane of sensory nerve endings in the bladder wall. This study also determined the localization and expression of histamine receptor subtypes within various locations of the urinary bladder (urothelium, detrusor, and afferent nerves), to better understand the neuroregulatory regions and network activation pathways involved in histamine-induced bladder sensitization. Most surprising and exciting was their discovery that a significant amount of nerve fibers initially identified as “silent” (unresponsive to distention) became mechanosensitive after exposure to histamine (3). Importantly, histamine also enhanced activation of sensory nerve cell bodies within the dorsal root ganglia, which strongly suggests that these changes in sensory nerve activity in the bladder alter central sensation of fullness. Further investigation of these pathways concluded that both histamine H1 receptors and TRPV1 channels have dominant roles in regulating sensory nerve signaling.
Fig. 1.
Cartoon showing the pathway proposed by Grundy et al. (3) by which histamine release changes sensory outflow from the urinary bladder during filling. TRPV1, transient receptor potential vanilloid type 1 channel.
CONCLUSIONS
In summary, Grundy et al. were able to apply their knowledge of histamine-dependent mechanisms that regulate mechanosensory innervation in other organs (e.g., the gastrointestinal tract) to elucidate a sound and logical mechanism of action by which histamine could directly cause the onset of symptoms similar to those seen in IC/BPS. This work has indeed established an innovative link between the central and peripheral roles of TRPV1 channels, histamine, and histamine receptors to induce bladder dysfunction through alterations in the sensation of bladder fullness. It also highlights and further supports the need to investigate histaminergic signaling as more than the result of inflammation-driven mast cell degranulation but as a potential direct cause of bladder dysfunction.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
AUTHOR CONTRIBUTIONS
N.R.T. prepared figures; B.M.J. drafted manuscript; B.M.J. and N.R.T. edited and revised manuscript; B.M.J. and N.R.T. approved final version of manuscript.
REFERENCES
- 1.Geppetti P, Nassini R, Materazzi S, Benemei S. The concept of neurogenic inflammation. BJU Int 101, Suppl 3: 2–6, 2008. doi: 10.1111/j.1464-410X.2008.07493.x. [DOI] [PubMed] [Google Scholar]
- 2.Grundy L, Caldwell A, Brierley SM. Mechanisms underlying overactive bladder and interstitial cystitis/painful bladder syndrome. Front Neurosci 12: 931, 2018. doi: 10.3389/fnins.2018.00931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grundy L, Caldwell A, Garcia Caraballo S, Erickson A, Schober G, Castro J, Harrington AM, Brierley SM. Histamine induces peripheral and central hypersensitivity to bladder distension via the histamine H1 receptor and TRPV1. Am J Physiol Renal Physiol 318: F298–F314, 2020. doi: 10.1152/ajprenal.00435.2019. [DOI] [PubMed] [Google Scholar]
- 4.Grundy L, Harrington AM, Castro J, Garcia-Caraballo S, Deiteren A, Maddern J, Rychkov GY, Ge P, Peters S, Feil R, Miller P, Ghetti A, Hannig G, Kurtz CB, Silos-Santiago I, Brierley SM. Chronic linaclotide treatment reduces colitis-induced neuroplasticity and reverses persistent bladder dysfunction. JCI Insight 3: e121841, 2018. doi: 10.1172/jci.insight.121841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jasmin L, Janni G. Experimental neurogenic cystitis. Adv Exp Med Biol 539: 319–335, 2003. [DOI] [PubMed] [Google Scholar]
- 6.Lv J, Huang Y, Zhu S, Yang G, Zhang Y, Leng J, Bo J, Liu D. MCP-1-induced histamine release from mast cells is associated with development of interstitial cystitis/bladder pain syndrome in rat models. Mediators Inflamm 2012: 358184, 2012. doi: 10.1155/2012/358184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mingin GC, Peterson A, Erickson CS, Nelson MT, Vizzard MA. Social stress induces changes in urinary bladder function, bladder NGF content, and generalized bladder inflammation in mice. Am J Physiol Regul Integr Comp Physiol 307: R893–R900, 2014. doi: 10.1152/ajpregu.00500.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parsons JK, Parsons CL. The historical origins of interstitial cystitis. J Urol 171: 20–22, 2004. doi: 10.1097/01.ju.0000099890.35040.8d. [DOI] [PubMed] [Google Scholar]
- 9.Rosa AC, Fantozzi R. The role of histamine in neurogenic inflammation. Br J Pharmacol 170: 38–45, 2013. doi: 10.1111/bph.12266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rudick CN, Bryce PJ, Guichelaar LA, Berry RE, Klumpp DJ. Mast cell-derived histamine mediates cystitis pain. PLoS One 3: e2096, 2008. doi: 10.1371/journal.pone.0002096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rudick CN, Pavlov VI, Chen MC, Klumpp DJ. Gender specific pelvic pain severity in neurogenic cystitis. J Urol 187: 715–724, 2012. doi: 10.1016/j.juro.2011.10.048. [DOI] [PubMed] [Google Scholar]
- 12.Schemann M, Kugler EM, Buhner S, Eastwood C, Donovan J, Jiang W, Grundy D. The mast cell degranulator compound 48/80 directly activates neurons. PLoS One 7: e52104, 2012. doi: 10.1371/journal.pone.0052104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shan H, Zhang EW, Zhang P, Zhang XD, Zhang N, Du P, Yang Y. Differential expression of histamine receptors in the bladder wall tissues of patients with bladder pain syndrome/interstitial cystitis−significance in the responsiveness to antihistamine treatment and disease symptoms. BMC Urol 19: 115, 2019. doi: 10.1186/s12894-019-0548-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Theoharides TC, Sant GR, el-Mansoury M, Letourneau R, Ucci AA Jr, Meares EM Jr. Activation of bladder mast cells in interstitial cystitis: a light and electron microscopic study. J Urol 153: 629–636, 1995. doi: 10.1016/S0022-5347(01)67669-9. [DOI] [PubMed] [Google Scholar]