Abstract
The aims of this study were to (1) compare the immediate post-treatment effects of an instructional video versus a self-preferred program on the hip range of motion and a pressure pain threshold using two different density roller balls, and (2) compare the effects of the two roller balls on those variables. Forty adults were randomly allocated into four groups: (1) MB1-video, (2) MB1-self-preferred, (3) MBX-video, and (4) MBX-self-preferred. Participants followed a video or a self-preferred program using either a moderate (MB1) or a hard (MBX) density ball. Main outcomes were passive hip internal rotation, external rotation, and a pressure pain threshold. For MB1, the video produced greater outcomes than the self-program for external rotation (10◦ versus 2◦), internal rotation (7◦ versus 2◦), and the pain threshold (210 kPa versus 44 kPa). For MBX, the video produced greater outcomes than the self-program for external rotation (8◦ versus 1◦), internal rotation (5◦ versus 1◦), and the pain threshold (184 kPa versus 30 kPa). When comparing roller balls, the MB1 produced greater outcomes than the MBX for external rotation (10◦ versus 8◦), internal rotation (7◦ versus 5◦), and the pain threshold (210 kPa versus 184 kPa) with the video. For the self-preferred program, the MB1 produced greater outcomes for external rotation (2◦ versus 1◦), internal rotation (2◦ versus 1◦), and the pain threshold (44 kPa versus 30 kPa). The instructional video and a moderate density ball produced greater immediate post-treatment outcomes than the self-program and a hard density ball. Professionals should consider using the video to teach technique and match clients to a specific density-type roller ball.
Key words: foam, massage, myofascial, pain, release
Introduction
Over the past decade roller massage (RM) has become a commonly-utilized myofascial intervention in various clinical, health & wellness, and sports performance settings. RM has emerged as one of the top 20 fitness trends in the United States which highlights its growing popularity (Thompson, 2018).
This popularity has stimulated an increase in RM research; however, evidence is still emerging. Currently, researchers have found that RM may be used as a warm-up without negatively effecting performance and may enhance joint mobility and range of motion (ROM) at the shoulder (Fairall et al., 2017), lumbopelvis (Sullivan et al., 2013), hip (DeBruyne et al., 2017), knee (Cheatham et al., 2017), and ankle (Kelly and Beardsley, 2016). Researchers have also found that RM may reduce post exercise decrements in muscle performance (Macdonald et al., 2014), increase posttreatment pressure pain thresholds (PPT) (Aboodarda et al., 2015; Cheatham and Kolber, 2018), and reduce the effects of delayed onset muscle soreness in healthy individuals (Macdonald et al., 2014). Several recent studies have also documented positive post-exercise effects of RM for different sports (Rey et al., 2017), occupations (Kalen et al., 2017), and fibromyalgia (Ceca et al., 2017). For rehabilitation, RM may have some benefits due to possible neurophysiological effects that occur to the target and surrounding tissues after treatment (Aboodarda et al., 2015; Monteiro et al., 2017). Researchers have shown that RM to the agonist target tissue may affect the muscle activity and pressure pain threshold of the ipsilateral antagonist through reciprocal inhibition and the contralateral agonist through a crossover effect (Cheatham and Kolber, 2018). This may have implications in the presence of injury since rolling on the target or agonist tissues could create a desired neurophysiological effect on the injured antagonist or contralateral muscles.
Despite the growing body of research, there are still many unanswered questions regarding the optimal type of a RM device, density, treatment time, cadence, technique, the amount of force, or instructional strategy (Cheatham et al., 2015). Of interest are the effects of RM using a roller ball, specifically, the effects of different instructional methods and the effects of different density type roller balls. To the researchers’ knowledge, no investigations have been published on this topic. Only one published study compared instructional methods (live, video, self-preferred) for foam rolling (Cheatham et al., 2017).
Understanding the efficacy of different instructional methods with different density-type roller balls may provide sports medicine professionals with the knowledge to more accurately prescribe/recommend a program and RM device for their clients. Therefore, the purpose of this investigation was to (1) compare the immediate post-treatment effects of an instructional roller ball video versus a self-preferred program on hip ROM and PPT using two different density roller balls, and (2) compare the immediate post-treatment effects of two different density type roller balls on hip ROM and PPT. It was hypothesized that the instructional video and a higher density roller ball would have a greater effect on ROM and PPT outcome measures than the self-preferred program and/or a moderate density roller ball.
Methods
Participants
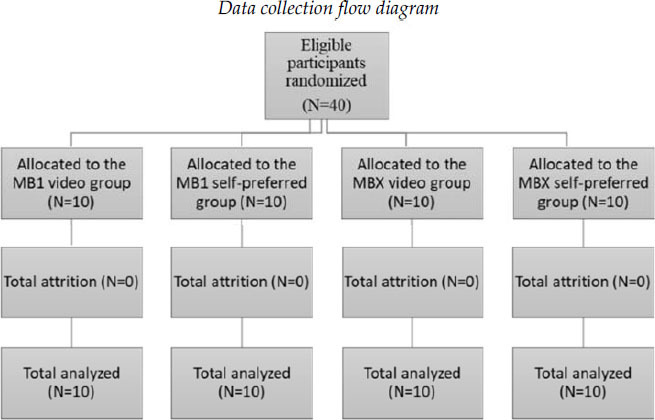
Forty healthy, recreationally active adults were recruited via convenience sampling (e.g. flyers) and randomly allocated into four groups of 10 participants: (1) MB1-video, (2) MB1-self-preferred, (3) MBX-video, (4) MBX-self-preferred (Table 1). Recruited participants reported taking part in recreational fitness activities (e.g. jogging) and no prior experience using a roller ball within the last year. Exclusion criteria included the presence of any neurosensory, musculoskeletal, systemic, or metabolic disease that would affect lower extremity joint ROM, tolerance to PPT testing, or the inability to avoid medications that may affect testing. Descriptive demographic information is provided in Table 2.
Table 1.
Data collection flow diagram
|
Table 2.
Participants’ demographics (N=40)
| Characteristics |
Age (years) |
Height (cm) |
Mass (kg) |
BMI (kg/m2) |
| MB1 (Video) (N=10) | 25.60 ± 2.67 | 172.17 ± 12.81 | 73.76 ± 12.72 | 24.75 ± 2.33 |
| MB1 (Self-program) (N=10) | 25.50 ± 3.89 | 172.13 ± 10.23 | 70.62 ± 11.23 | 23.68 ± 2.63 |
| MBX (Video) (N=10) | 23.40 ± 2.01 | 166.78 ± 11.43 | 63.09 ± 10.16 | 22.84 ± 3.92 |
| MBX (Self-program) (N=10) | 26.20 ± 4.54 | 169.08 ± 9.66 | 69.10 ± 13.00 | 24.28 ± 4.75 |
Data reported as mean ± SD; cm = centimeters; BMI = body mass index; kg/m2 = kilograms-meter squared; Exp = experimental, Con = control, MB1 = moderate density ball, MBX = hard density ball
Design
This pretest, posttest randomized controlled trial was approved by the Institutional Review Board at the California State University Dominguez Hills. Data collection was conducted at the kinesiology laboratory.
Instruments
Two instruments were used in this investigation to measure ROM and PPT. For passive hip ROM, the Halo digital laser goniometer (HALO, model HG1, HALO Medical Devices, Australia) was used to measure supine passive hip internal (IR) and external (ER) rotation. The manufacturer reports accuracy of ± 1.0 degree (Correll et al., 2018). This device has been shown to be valid and reliable for measuring ROM (Correll et al., 2018). The Wagner (Midvale, UT) FDX algometer was used to measure the pressure pain threshold. The manufacturer reports accuracy error of < ±0.3% for this technology (Wagner). Algometry is a valid and reliable tool for measuring pressure pain thresholds (Nussbaum and Downes, 1998) and it has been used in prior foam roll research (Cheatham and Kolber, 2018).
Instructional Video and Roller Balls
A commercial internet-based instructional video and roller balls were used in this investigation (TriggerPoint, a division of Implus, LLC, 5321 Industrial Oaks Blvd., Austin, Texas 78735, USA). The 2-min roller ball instructional video demonstrated the use of the roller ball on the left hip external rotator muscles. The video used the piriformis muscles as the main target tissue. RM video interventions have been used in prior research (Cheatham et al., 2019). The MB1 is a moderate density solid foam core roller ball (height: 6.6 cm, weight: 0.040 kg) with an EVA foam outer texture, while the MBX is a high density solid foam core roller ball (height: 6.6 cm, weight: 0.040 kg) with an EVA foam outer texture. Both roller balls were the same size and had the same surface texture (Figure 1).
Figure 1a.

MB1 (Moderate Density) Roller Ball
Measures
Two outcome measures were used for the pretest and posttest measures for each group. For passive hip IR and ER ROM, participants lied supine on a plinth with the digital goniometer attached just below the tibial tuberosity with a velcro strap. The examiner grasped the left hip and brought it up to 90◦ of hip flexion with the knee also flexed to 90◦. The goniometer was then calibrated, and the measurements were taken. The examiner passively moved the participant’s hip into IR, keeping the leg in neutral, to the end of the available range until an “unyielding” end-feel was experienced and then took the measurement. Afterwards, the examiner passively moved the participant’s hip into ER using the same procedure (Shimamura et al., 2015). Two measurements were taken for each motion. The examiner provided verbal cues if the participant compensated in any way to ensure no substitute movements occurred during testing (Shimamura et al., 2015).
For PPT, the left piriformis was tested with the participant in the relaxed prone position (2 measurements) (Cheatham et al., 2019). The 1.0-cm2 probe of the algometer was placed perpendicularly to the midline of the piriformis midway between the sacrum and greater trochanter of the left hip. The graded force was applied at a constant rate of 50-60 kilopascals per second (kPa/sec) until the participant verbally reported the presence of pain (Cheatham et al., 2019).
Pilot Study
Prior to data collection, two-session pilot training was conducted to establish intra-rater reliability. The primary investigator took all the measurements. The primary investigator was a licensed physical therapist with over 13 years of experience and board certified in orthopaedics. Ten independent participants were recruited and tested for this portion of the study. The intra-rater reliability was calculated using the Intraclass Correlation Coefficient (ICC model 3, k) (Portney and Watkins, 2009). There was good intra-rater reliability for both passive IR (ICC = 0.91) and ER (ICC = 0.92) ROM. These coefficients were in accordance with the minimum threshold of ≥ 0.90 for ICC values postulated to be acceptable for clinical decision making (Portney and Watkins, 2009).
Procedures
All eligible participants were given an IRB approved consent form to read and sign before testing. Participants then completed a questionnaire to provide demographic information. All participants were blinded from the results and other participants enrolled in the study. The primary investigator took all pre and posttest measures and was blinded from the testing procedures. Testing was conducted between 10 am and 2 pm and participants were instructed to refrain from any strenuous activity 5 hours prior to testing and from taking any medication that would interfere with testing. All participants underwent one session of testing that included: pretest measures, followed by the intervention, then immediate posttest measures.
Prior to testing, the primary investigator took baseline measures then left the testing area. A second investigator was present and explained the procedures to each participant based upon their group allocation and answered any questions. Then each participant was given their assigned roller ball (e.g. MB1 or MBX) and either followed the video or did their self-preferred program.
The instructional video demonstrated the use of the roller ball on the left hip external rotators using the piriformis as the primary target tissue. Participants followed the video with no feedback from the observing investigator. The instructor in the video provided a brief introduction and then discussed the rolling technique. The instructor described the left piriformis region as zone one: the middle of the muscle between the sacrum and greater trochanter. The model in the video was instructed to get into the long sitting position, bend the right hip and knee and place foot on the floor. The model then placed the roller ball under the left hip in the middle of zone one and shifted their weight over the ball with the left hip and knee straight. The model then performed three movements. First, the model performed four knee to chest leg lifts with the left leg. Second, the model bent the left hip and knee to place the foot on the floor and perform two ER movements. Third, the model performed one clockwise and one counterclockwise pivot motion over the roller ball. Both hips and knees were bent and feet on the floor with the second and third motions. This sequence was performed two consecutive times. The total intervention time was 2 minutes.
For the self-preferred program (control), the second examiner first demonstrated the starting position participants would assume during testing. Participants then positioned themselves on the floor in the long sitting position, bent the right hip and knee with foot placed on the floor, and then placed the ball under their left hip with the knee straight for the intervention. This was the same starting position as for the video group. The participants then (with the ball under the left hip) began their own self-preferred roller massage technique for 2 minutes. The observing examiner provided no feedback during the intervention and notified the participant to stop at 2 minutes.
Statistical Analysis
Statistical analysis was performed using SPSS version 25.0 (IBM SPSS, Armonk, New York, USA). Participant descriptive data were calculated and reported as the mean and standard deviation (SD) for age, body height, body mass, and body mass index (BMI) (Table 2). Group demographic differences were calculated using the ANOVA statistic for continuous level data and the Kruskal Wallis statistic for ordinal level data. Between group differences were calculated using the ANCOVA statistic. For the ANCOVA, the independent variable was the group, the dependent variable was posttest scores, and pretest scores was the covariate. Within group comparisons were calculated using the paired t test. Effect size (ES) was calculated (d = M1 - M2 / σpooled) for each group. Effect size of > .70 was considered strong, .41 to .70 moderate, and < .40 weak (Cohen, 1992). All statistical assumptions were met for the ANOVA, ANCOVA and paired t test statistics. Statistical significance was considered p < .05 using a conservative two-tailed test.
Results
All 40 participants completed the study (M = 24, F = 16; mean age = 25.17 ± 3.28 years, body height = 170.04 ± 11.03 cm, body mass = 69.14 ± 11.78 kg, BMI = 23.88 ± 3.40) (Figure 1). There was no statistically significant difference between groups for age (p = 0.30), body height (p = 0.65), body mass (p = 0.25), or a body mass index (p = 0.66). There were no adverse events reported or participant attrition during data collection. Group demographic data are presented in Table 2.
MB1 (Video versus Self-Preferred)
Between group comparisons were calculated. For passive hip ROM, there was a significant difference between the video and self-preferred group for ER (F 1,17 = 170.80, p ≤ 0.001, η2p = 0.909) and IR (F 1,17 = 259.65, p < 0.001, η2p = 0.939)]. For PPT, there was a significant difference between the video and self-preferred group (F 1,17 = 108.46, p ≤ 0.001, η2p = .865).
The within group analysis was calculated. For passive hip ER ROM, a posttest increase of approximate 10° (p < 0.001, ES = 1.13) for the video versus 2° (p < 0.001, ES = .016) for the self-preferred group was observed. For passive hip IR ROM, a posttest increase of approximate 7° (p < 0.001, ES = 0.77) for the video versus 2° (p < 0.012, ES = 0.25) for the self-preferred group was noted. For PPT, a posttest increase of 210 kPa (p < .001, ES = 1.09) was found for the video versus 44 kPa (p = 0.009, ES = 0.27) for the self-preferred group.
MBX (Video versus Self-Preferred)
Between group comparisons were calculated. For passive hip ROM, there was a significant difference between the video and the self-preferred group for ER (F 1,17 = 254.03, p ≤ 0.001, η2p = 0.937) and IR (F 1,17 = 160.30, p < 0.001, η2p = 0.904). For PPT, there was a significant difference between the video and the self-preferred group (F 1,17 = 132.32, p = 0.001, η2p = 0.886).
The within group analysis was conducted. For passive hip ER ROM, a posttest increase of approximate 8° (p < 0.001, ES = 0.99) for the video versus 1° (p = 0.017, ES = 0.11) for the self-preferred group was observed. For passive hip IR ROM, a posttest increase of approximate 5° (p < 0.001, ES = 0.50) for the video versus 1° (p = 0.15, ES = 0.16) for the self-preferred group was noted. For PPT, a posttest increase of 184 kPa (p < .001, ES = 0.73) was found for the video versus 30 kPa (p = 0.019, ES = 0.15) for the self-preferred group.
MB1 Ball versus MBX Ball (Video)
Between group comparisons were carried out for the video intervention. There was a significant difference between both devices for ER (F 1,17 = 154.13, p ≤ 0.001, η2p = 0.901) and IR (F 1,17 = 183.71, p < 0.001, η2p = .915). For PPT, there was a significant difference between both devices (F 1,17 = 77.76, p ≤ 0.001, η2p = 0.821). The within group analysis was performed. For passive hip ER ROM, a post-treatment increase of approximate 10° (p < 0.001, ES = 1.13) for the MB1 versus 8° (p < 0.001, ES = 0.99) for the MBX was observed. For passive hip IR ROM, the within group analysis revealed a post-treatment increase of approximate 7° (p < 0.001, ES = 0.77) for the MB1 versus 5° (p <0.001, ES = 0.50) for the MBX ball. For PPT, a post-treatment increase of 210 kPa (p < .001, ES = 1.09) for the MB1 versus 184 kPa (p < .001, ES = 0.73) for the MBX was found.
MB1 Ball versus MBX Ball (Self-Preferred)
Between group comparisons were performed for the self-preferred (control) program. There was a significant difference between both devices for ER (F 1,17 = 403.89, p = < 0.001, η2p = 0.960) and IR (F 1,17 = 223.91, p < 0.001, η2p = 0.929). For PPT, there was a significant difference between both devices (F 1,17 = 785.68, p ≤ 0.001, η2p = 0.980).
The within group analysis was conducted. For passive hip ER ROM, a post-treatment increase of approximate 2° (p < 0.001, ES = .016) for the MB1 versus 1° (p = .017, ES = 0.11) for the MBX group was noted. For passive hip IR ROM, a post-treatment increase of approximate 2° (p < 0.012, ES = 0.25) for the MB1 versus 1° (p = 0.15, ES = 0.16) for the MBX group was observed. For PPT, a post-treatment increase of 44 kPa (p = 0.009, ES = 0.27) for the MB1 versus 30 kPa (p = 0.019, ES = 0.15) for the MBX was found.
Figure 1b.
MBX (Hard Density) Roller Ball
Table 3.
Pretest, posttest descriptive results
| Pretest | Posttest | Change | p | |
| MB1 Ball (Video) (N=10) | ||||
| Hip ER ROM (degrees) | 31.61 ± 8.15 | 41.61 ± 9.43 | 10.00 ± 1.28 | *<0.001 |
| Hip IR ROM (degrees) | 24.10 ± 8.68 | 31.10 ± 9.49 | 7.00 ± 0.81 | *<0.001 |
| Pressure Pain Threshold (kPa) | 1100.20 ± 204.17 | 1310.00 ± 181.25 | 210.00 ± 22.92 | *<0.001 |
| MB1 Ball (Self-program) (N=10) | ||||
| Hip ER ROM (degrees) | 30.30 ± 10.21 | 31.90 ± 9.63 | 1.60 ± 0.57 | *0.016 |
| Hip IR ROM (degrees) | 26.80 ± 9.55 | 29.30 ± 10.40 | 2.50 ± 0.85 | *0.012 |
| Pressure Pain Threshold (kPa) | 902.80 ± 156.02 | 947.00 ± 171.82 | 44.20 ± 15.8 | *0.009 |
| MBX Ball (Video) (N=10) | ||||
| Hip ER ROM (degrees) | 32.40 ± 7.69 | 41.00 ± 9.61 | 8.40 ± 1.92 | *<0.001 |
| Hip IR ROM (degrees) | 24.45 ± 8.80 | 29.30 ± 10.60 | 4.85 ± 1.80 | *<0.001 |
| Pressure Pain Threshold (kPa) | 1055.80 ± 245.40 | 1240.00 ± 257.82 | 184.20 ± 12.42 | *<0.001 |
| MBX Ball (Self-program) (N=10) | ||||
| Hip ER ROM (degrees) | 32.41 ± 10.08 | 33.50 ± 9.87 | 1.10 ± 8.16 | 0.17 |
| Hip IR ROM (degrees) | 21.50 ± 7.21 | 22.70 ± 7.66 | 1.20 ± 0.45 | 0.15 |
| Pressure Pain Threshold (kPa) | 937.00 ± 195.60 | 967.20 ± 198.27 | 30.20 ± 2.67 | *0.019 |
*IR: inter Data reported as mean ± SD, kPa = kilopascals; *statistical significance = p < .05; Exp = experimental, Con = control ER = external rotation, IR = internal rotation, MB1 = moderate density ball, MBX = hard density ball
Discussion
The aim of this investigation was to (1) compare the immediate post-treatment effects of an instructional roller ball video versus a self-preferred program on hip ROM and PPT using two different density roller balls, and (2) compare the immediate post-treatment effects of two different density type roller balls on hip ROM and PPT. This study was unique because a control group was used for each roller ball and intervention. Very few RM studies have utilized a comparison control group (Cheatham et al., 2017; Cheatham et al., 2019).
For the MB1 ball (moderate density), the results of this investigation suggest that an instructional video produced greater immediate post-treatment outcomes when compared to a self-preferred program (control) for hip ER (10◦ versus 2◦), hip IR (7◦ versus 2◦), and PPT (210 kPa versus 44 kPa). For the MBX ball (hard density), similar findings were observed for the instructional video compared to the self-preferred program for hip ER (8◦ versus 1◦), hip IR (5◦ versus 1◦), and PPT (184 kPa versus 30 kPa). To the researchers’ knowledge, only one other published study compared the difference between an instructional RM foam rolling video to other methods. Cheatham et al. (2017) compared the therapeutic effects of three types of RM interventions with a foam roller: live instruction, video, and a self-preferred program. The outcome measures were passive knee flexion ROM and PPT of the quadriceps muscles. The researchers found no statistical difference between the three types of instructional interventions (Cheatham et al., 2017). This investigation used different methods (e.g. body region, variables, devices, and video) than the aforementioned study which may explain the different results and thus this makes it difficult for a direct comparison.
When comparing the post-treatment effects of the MB1 and MBX roller balls, the results suggest the MB1 ball produced greater outcomes when compared to the MBX ball for hip ER (10◦ versus 8◦), hip IR (7◦ versus 5◦), and PPT (210 kPa versus 184 kPa). Similar findings were observed for the self-preferred program. The MB1 produced greater post-treatment outcomes when compared to the MBX for hip ER (2◦ versus 1◦), hip IR (2◦ versus 1◦), and PPT (44 kPa versus 30 kPa). To the researcher’s knowledge, this is the first investigation to measure the post-treatment differences of two different density-type roller balls with the same core and surface texture. There have been some past studies that measured the therapeutic effects of roller balls (e.g. tennis ball), but have not compared different density-type roller balls with the same architectural properties (Grabow et al., 2017). Furthermore, the only prior research examining the therapeutic effects of different densities has been with foam rollers (Cheatham and Stull, 2018). The greater outcomes with the MB1 roller ball (moderate density) may be due to the subject’s pain perception during the intervention which could affect their post-treatment outcomes. Recent research suggests that harder density RM devices may produce higher levels of compression to the myofascia resulting in an elevated level of perceived discomfort (Cheatham et al., 2018). Thus, the MBX (high density) may have produced a higher level of perceived discomfort than the MB1 roller ball. Further research is needed to validate these clinical findings.
The existing body of research provides several hypotheses regarding how the body responds to RM interventions. Researchers believe the direct myofascial compression of RM devices may produce a local mechanical and global neurophysiological response that influences tissue relaxation and pain in the local and surrounding tissues through afferent central nervous system (CNS) pathways (Aboodarda et al., 2015; Grabow et al., 2018). For the mechanical effect, the direct roller compression may change the viscoelastic properties of the local myofascia by mechanisms such as reducing myofascial restriction, fluid changes, and cellular responses (Kelly and Beardsley, 2016). Researchers have also found that rolling reduces local arterial stiffness (Okamoto et al., 2014), increases arterial tissue perfusion (Hotfiel et al., 2017), and improves vascular endothelial function (Okamoto et al., 2014) which are all related to local physiological changes. For the neurophysiological effect, the direct roller compression may influence tissue relaxation and pain in the local and surrounding tissues. For tissue relaxation, the roller compression may induce greater myofascial relaxation or “stretch tolerance” through CNS afferent input from the Golgi tendon reflex and mechanoreceptors (Cavanaugh et al., 2017; Kelly and Beardsley, 2016; Monteiro et al., 2017). For pain, researchers have postulated that roller compression may modulate pain through stimulation of cutaneous receptors (e.g. C-tactile fibers) (Aboodarda et al., 2015), mechanoreceptors (Young et al., 2018), afferent central nociceptive pathways (gate theory of pain) (Cavanaugh et al., 2017), and descending anti-nociceptive pathways (diffuse noxious inhibitory control) (Aboodarda et al., 2015). These postulated responses are often seen clinically by posttest changes in joint ROM and pain perception which lends evidence to the sensitivity of the myofascia to external forces (Grabow et al., 2018).
Limitations
There are limitations to the investigation that need to be discussed. First, this investigation tested healthy subjects which limits the generalizability of the results to this population. Second, the two different density-type roller balls had the same surface architecture and diameter. Other roller balls with different surface patterns, diameters, densities, and material may have produced different results. Third, while the immediate effects of each intervention were studied, the longer-term effects of each intervention cannot be determined. Last, the instructional video used in the intervention only demonstrated one roller ball technique for the left hip external rotators (piriformis muscle). Other rolling techniques as well as testing other ranges of motion and muscle groups may have produced different results.
Future Research
Professionals should consider the results of this study as preliminary since no other investigations have been conducted. Future studies are needed to further validate the results and to develop a consensus on the optimal surface and density type roller ball for specific individuals. Furthermore, research should attempt to determine the longer-term effects of different types of roller balls based upon surface patterns, density, a diameter, and material using similar research methods. The current RM research is variable with different methodology which prevents a direct comparison among studies (Cheatham et al., 2015).
Practical Implications
Sports medicine professionals may prefer to initially provide live prescriptive instruction to their clients for the specific RM technique (Cheatham et al., 2017). The 1:1 instruction allows for the professional to teach, correct, and readily answer any questions. The professional may also want to use an instructional video to reinforce the RM techniques that were taught to the client. Instructional video may also be good for larger groups. For example, the video may help to standardize the RM session with a sports team since all individuals would undergo the same exercise prescription. For RM intervention time, the research suggests that short bouts (e.g. ≤ 2 minutes) of RM may enhance the warm-up and longer bouts (e.g. ≥ 2 minutes) may enhance the cool down. The post-treatment effects of RM seem to only last up to 20-30 minutes (Cheatham et al., 2015). The 2-minute prescriptive video used in this investigation utilized active movement through different ranges of motion which may have produced greater outcomes due to the influence of agonistic muscle activity during active motion. This activity may modulate activity of the antagonist muscle through reciprocal inhibition and other neural pathways (Cheatham et al., 2019). Sports medicine professionals should consider these variables before implementing an RM intervention to their clients and sports teams.
Sports medicine professionals should consider when to use a specific RM device with their clients or sports teams. For larger areas of the body, a foam roll may provide myofascial compression to a broader region which may be more efficient than a small device that compresses a smaller area. For certain areas of the body such as the shoulder or hip, a smaller RM device (such as a roller ball) may be better due to the surrounding bones. The roller ball may be able to compress the smaller soft-tissue areas better than a larger foam roll. This study measured the effects of two different density-type roller balls on the hip region. The results suggest that the MB1 (moderate density) produced statistically greater post-treatment gains than the MBX (hard density). However, those difference may not be clinically meaningful in many settings. Progressing the client through the different roller ball densities based upon their pain perception may be a viable alternative. Using the numerical pain rating scale (NPRS) (0-10) may be a way to documents a client’s pain level during and after RM and progress treatment (Cheatham and Stull, 2018). Professionals may want to have a variety of rollers (e.g. different shapes and densities) available to their clients and use a subjective scale such as the NPRS to help guide treatment.
Conclusion
This was the first investigation to measure the immediate post-treatment effects of an instructional roller ball video versus a self-preferred program and the differences between two density-type roller balls with the same surface architecture and diameter. The instructional video appears to produce a greater post-treatment effect on hip ROM and PPT which may be from the addition of active movement through different ranges of motion. The moderate density-type roller ball seems to produce greater immediate post-treatment outcomes than the hard density-type roller ball. Professionals should consider using video to reinforce technique after live instruction and match clients to a specific density-type roller ball.
Acknowledgements
We would like to thank Trigger Point Technologies for providing permission to use the instructional video and associated roller balls and images.
References
- Aboodarda SJ, Spence AJ, Button DC. Pain pressure threshold of a muscle tender spot increases following local and non-local rolling massage. BMC Musculoskelet Disord. 2015;16:265. doi: 10.1186/s12891-015-0729-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanaugh MT, Doweling A, Young JD, Quigley PJ, Hodgson DD, Whitten JH, Reid JC, Aboodarda SJ, Behm DG. An acute session of roller massage prolongs voluntary torque development and diminishes evoked pain. Eur J Appl Physiol. 2017;117:109–117. doi: 10.1007/s00421-016-3503-y. [DOI] [PubMed] [Google Scholar]
- Ceca D, Elvira L, Guzman JF, Pablos A. Benefits of a self-myofascial release program on health-related quality of life in people with fibromyalgia: a randomized controlled trial. J Sports Med Phys Fitness. 2017;57:993–1002. doi: 10.23736/S0022-4707.17.07025-6. [DOI] [PubMed] [Google Scholar]
- Cheatham SW, Kolber MJ. Does roller massage with a foam roll change pressure pain threshold of the ipsilateral lower extremity antagonist and contralateral muscle groups? an exploratory study. J Sport Rehabil. 2018;27:165–169. doi: 10.1123/jsr.2016-0196. [DOI] [PubMed] [Google Scholar]
- Cheatham SW, Kolber MJ, Cain M. Comparison of video-guided, live instructed, and self-guided foam roll interventions on knee joint range of motion and pressure pain threshold: a randomized controlled trial. Int J Sports Phys Ther. 2017;12:242–249. [PMC free article] [PubMed] [Google Scholar]
- Cheatham SW, Kolber MJ, Cain M, Lee M. The effects of self-myofascial release using a foam roll or roller massager on joint range of motion, muscle recovery, and performance: a systematic review. Int J Sports Phys Ther. 2015;10:827–838. [PMC free article] [PubMed] [Google Scholar]
- Cheatham SW, Stull KR. Comparison of three different density type foam rollers on knee range of motion and pressure pain threshold: a randomized controlled trial. Int J Sports Phys Ther. 2018;13:474–482. [PMC free article] [PubMed] [Google Scholar]
- Cheatham SW, Stull KR, Kolber MJ. Comparison of a vibrating foam roller and a non-vibrating foam roller intervention on knee range of motion and pressure pain threshold: a randomized controlled trial. J Sport Rehabil. 2019;28:39–45. doi: 10.1123/jsr.2017-0164. [DOI] [PubMed] [Google Scholar]
- Cheatham SW, Stull KR, Kolber MJ. Roller massage: is the numeric pain rating scale a reliable measurement and can it direct individuals with no experience to a specific roller density? J Can Chiropr Assoc. 2018;62:161–169. [PMC free article] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychol Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Correll S, Field J, Hutchinson H, Mickevicius G, Fitzsimmons A, Smoot B. Reliability and validity of the halo digital goniometer for shoulder range of motion in healthy subjects. Int J Sports Phys Ther. 2018;13:707–714. [PMC free article] [PubMed] [Google Scholar]
- DeBruyne DM, Dewhurst MM, Fischer KM, Wojtanowski MS, Durall C. Self-mobilization using a foam roller versus a roller massager: which is more effective for increasing hamstrings flexibility? J Sport Rehabil. 2017;26:94–100. doi: 10.1123/jsr.2015-0035. [DOI] [PubMed] [Google Scholar]
- Fairall RR, Cabell L, Boergers RJ, Battaglia F. Acute effects of self-myofascial release and stretching in overhead athletes with GIRD. J Bodyw Mov Ther. 2017;21:648–652. doi: 10.1016/j.jbmt.2017.04.001. [DOI] [PubMed] [Google Scholar]
- Grabow L, Young JD, Alcock LR, Quigley PJ, Byrne JM, Granacher U, Skarabot J, Behm DG. Higher quadriceps roller massage forces do not amplify range-of-motion increases nor impair strength and jump performance. J Strength Cond Res. 2018;32:3059–3069. doi: 10.1519/JSC.0000000000001906. [DOI] [PubMed] [Google Scholar]
- Grabow L, Young JD, Byrne JM, Granacher U, Behm DG. Unilateral rolling of the foot did not affect nonlocal range of motion or balance. J Sports Sci Med. 2017;16:209–218. [PMC free article] [PubMed] [Google Scholar]
- Hotfiel T, Swoboda B, Krinner S, Grim C, Engelhardt M, Uder M, Heiss RU. Acute effects of lateral thigh foam rolling on arterial tissue perfusion determined by spectral doppler and power doppler ultrasound. J Strength Cond Res. 2017;31:893–900. doi: 10.1519/JSC.0000000000001641. [DOI] [PubMed] [Google Scholar]
- Kalen A, Perez-Ferreiros A, Barcala-Furelos R, Fernandez-Mendez M, Padron-Cabo A, Prieto JA, Rios-Ave A, Abelairas-Gomez C. How can lifeguards recover better? A cross-over study comparing resting, running, and foam rolling. Am J Emerg Med. 2017;35(12):1887–1891. doi: 10.1016/j.ajem.2017.06.028. [DOI] [PubMed] [Google Scholar]
- Kelly S, Beardsley C. Specific and cross-over effects of foam rolling on ankle dorsiflexion range of motion. Int J Sports Phys Ther. 2016;11:544–551. [PMC free article] [PubMed] [Google Scholar]
- Macdonald GZ, Button DC, Drinkwater EJ, Behm DG. Foam rolling as a recovery tool after an intense bout of physical activity. Med Sci Sports Exerc. 2014;46:131–142. doi: 10.1249/MSS.0b013e3182a123db. [DOI] [PubMed] [Google Scholar]
- Monteiro ER, Skarabot J, Vigotsky AD, Brown AF, Gomes TM, Novaes JD. Acute effects of different self-massage volumes on the fms overhead deep squat performance. Int J Sports Phys Ther. 2017;12:94–104. [PMC free article] [PubMed] [Google Scholar]
- Nussbaum EL, Downes L. Reliability of clinical pressure-pain algometric measurements obtained on consecutive days. Phys Ther. 1998;78:160–169. doi: 10.1093/ptj/78.2.160. [DOI] [PubMed] [Google Scholar]
- Okamoto T, Masuhara M, Ikuta K. Acute effects of self-myofascial release using a foam roller on arterial function. J Strength Cond Res. 2014;28:69–73. doi: 10.1519/JSC.0b013e31829480f5. [DOI] [PubMed] [Google Scholar]
- Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. New Jersey: Pearson/Prentice Hall; 2009. [Google Scholar]
- Rey E, Padron-Cabo A, Costa PB, Barcala-Furelos R. The effects of foam rolling as a recovery tool in professional soccer players. J Strength Cond Res. 2017. [Epub ahead of print] [DOI] [PubMed]
- Shimamura KK, Cheatham S, Chung W, Farwell D, De la Cruz F, Goetz J, Lindblom K, Powers D. Regional interdependence of the hip and lumbo-pelvic region in divison ii collegiate level baseball pitchers: a preliminary study. Int J Sports Phys Ther. 2015;10:1–12. [PMC free article] [PubMed] [Google Scholar]
- Sullivan KM, Silvey DB, Button DC, Behm DG. Roller-massager application to the hamstrings increases sit-and-reach range of motion within five to ten seconds without performance impairments. Int J Sports Phys Ther. 2013;8:228–236. [PMC free article] [PubMed] [Google Scholar]
- Thompson WR. Worldwide survey of fitness trends for 2019. ACSM's Health Fit J. 2018;22:10–17. [Google Scholar]
- Wagner I. Wagner FDX Algometer Specification Page. http://www.wagnerinstruments.com/products/force-gages/digital/fdx Available at. Accessed 5/12/18.
- Young JD, Spence AJ, Behm DG. Roller massage decreases spinal excitability to the soleus. J Appl Physiol 1985. 2018;124(4):950–959. doi: 10.1152/japplphysiol.00732.2017. [DOI] [PubMed] [Google Scholar]