Abstract
Study Objectives:
To assess the effects of a yoga versus educational film (EF) program on restless legs syndrome (RLS) symptoms and related outcomes in adults with RLS.
Methods:
Forty-one community-dwelling, ambulatory nonpregnant adults with moderate to severe RLS were randomized to a 12-week yoga (n = 19) or EF program (n = 22). In addition to attending classes, all participants completed practice/treatment logs. Yoga group participants were asked to practice at home 30 minutes per day on nonclass days; EF participants were instructed to record any RLS treatments used on their daily logs. Core outcomes assessed pretreatment and posttreatment were RLS symptoms and symptom severity (International RLS Study Group Scale (IRLS) and RLS ordinal scale), sleep quality, mood, perceived stress, and quality of life (QOL).
Results:
Thirty adults (13 yoga, 17 EF), aged 24 to 73 (mean = 50.4 ± 2.4 years), completed the 12-week study (78% female, 80.5% white). Post-intervention, both groups showed significant improvement in RLS symptoms and severity, perceived stress, mood, and QOL-mental health (P ≤ .04). Relative to the EF group, yoga participants demonstrated significantly greater reductions in RLS symptoms and symptom severity (P ≤ .01), and greater improvements in perceived stress and mood (P ≤ .04), as well as sleep quality (P = .09); RLS symptoms decreased to minimal/mild in 77% of yoga group participants, with none scoring in the severe range by week 12, versus 24% and 12%, respectively, in EF participants. In the yoga group, IRLS and RLS severity scores declined with increasing minutes of homework practice (r = .7, P = .009 and r = .6, P = .03, respectively), suggesting a possible dose-response relationship.
Conclusions:
Findings of this exploratory RCT suggest that yoga may be effective in reducing RLS symptoms and symptom severity, decreasing perceived stress, and improving mood and sleep in adults with RLS.
Clinical Trial Registration:
Registry: Clinicaltrials.gov; Title: Yoga vs. Education for Restless Legs: a Feasibility Study; Identifier: NCT03570515; URL: https://clinicaltrials.gov/ct2/show/NCT03570515
Citation:
Innes KE, Selfe TK, Montgomery C, et al. Effects of a 12-week yoga versus a 12-week educational film intervention on symptoms of restless legs syndrome and related outcomes: an exploratory randomized controlled trial. J Clin Sleep Med. 2020;16(1):107–119.
Keywords: education, exercise therapy, mental health, mind-body, quality of life, restless legs syndrome, sleep disorders, yoga
BRIEF SUMMARY
Current Knowledge/Study Rationale: Relaxation and other nonpharmacologic therapies are often recommended for management of restless legs syndrome (RLS), a common and burdensome sleep and sensorimotor disorder. However, rigorous supporting research remains sparse. This exploratory randomized controlled trial assessed the effects of a yoga versus educational film program on RLS symptoms and related outcomes in adults with moderate to severe RLS.
Study Impact: Findings of this study suggest that yoga may offer a safe, viable, and effective therapy for reducing RLS symptoms and symptom severity, decreasing perceived stress, and improving sleep and mood in adults with RLS, with effects that were comparable to those of RLS medications.
INTRODUCTION
Restless legs syndrome (RLS) is a burdensome sleep and sensorimotor disorder affecting up to 29% of US and European adults, with estimated prevalence rates averaging 12% in the general population and 19.5% in primary care patients.1 RLS is characterized by a compelling urge to move the legs that is usually accompanied by unpleasant, often painful sensations in the legs, begins or worsens during periods of inactivity, is worse at night, and is at least partially alleviated by movement.2 Up to 65% of those affected by RLS experience moderate to severe symptoms.1 Associated with significant economic and societal burden,3,4 RLS can lead to reductions in quality of life (QOL) and declines in productivity that are comparable to or greater than those reported in other serious chronic disorders, including diabetes, depression, Parkinson disease, and stroke.1,4 A major cause of chronic sleep loss,5 RLS is also associated with significant deterioration in mood,6,7 which can further exacerbate sleep deficits.8,9
Although RLS is increasingly recognized as a disorder of significant clinical and economic importance,1,3,4,10 RLS etiology remains incompletely understood.4,11 Currently, the primary underlying causes of RLS are thought to be dopaminergic dysfunction, genetic predisposition, and deficiencies in iron metabolism,11–13 although these factors have to date offered only a partial explanation.9 A growing body of evidence also suggests that autonomic and hypothalamic–pituitary-adrenal axis dysregulation may also play an important role in RLS pathogenesis and progression.1,9,14 Recent studies suggest that RLS may also be linked, in a bidirectional manner, to cardiovascular disease, stroke, and key components of the metabolic syndrome,9 associations that may be in part mediated by RLS’s adverse effects on sleep and mood.15,16
Unfortunately, there is no cure for RLS, with current treatments aimed at symptom management. Pharmaceutical agents, specifically dopaminergic agents and antiseizure medications (α2δ ligands), remain first-line treatments for RLS, with opioids and less commonly, benzodiazepines, employed as second-line therapies.17,18 Regrettably, all medications used in the management of RLS carry risk of serious side effects (affecting 6% to 80% of patients, depending on the medication and treatment duration).15,17 Among the most problematic is augmentation of symptoms, a serious clinical sequelae reported for all dopaminergic drugs and certain opioids, with risk increasing with longer treatment duration.15,17 Other common side effects include somnolence and general toxicity (all RLS medications); impulse control disorders (dopamine receptor agonists); nausea and vomiting (dopaminergic agents, opioids); mood disturbances (α2δ ligands, opioids, benzodiazepines); weight gain (α2δ ligands); addiction (opioids, benzodiazepines); dizziness; unsteadiness; increased risk for falls (α2δ ligands, opioids, benzodiazepines); and other adverse side effects.15,17,19–21 In addition, these sequelae can be a particularly serious for older adults,22,23 who are also disproportionately affected by RLS.20,24 In addition, the efficacy of all RLS medications often diminishes with time,17,25 leaving patients with few treatment options.
Given the drawbacks of medications currently prescribed for RLS, investigation of safe, sustainable nonpharmacologic therapies that are suitable for long-term use and that may not only alleviate RLS symptoms but address associated declines in psychosocial status and QOL is clearly warranted. Although clinical guidelines often recommend lifestyle and other nonpharmacologic approaches for patients with RLS,17,26,27 recommendations are generally nonspecific and rigorous supportive research remains sparse.8,28 One nonpharmacological approach that may hold particular promise for adults with RLS is yoga, an ancient mind-body practice that is increasingly used as a therapeutic modality.29,30 Numerous studies have shown yoga to improve QOL, enhance well-being, and decrease pain,31–37 outcomes of clear relevance to those with RLS. In addition, our recent proof-of-concept studies suggest that yoga may attenuate RLS symptoms, improve sleep, enhance mood, and decrease stress in adults with RLS.14,38 However, although findings of these trials suggest that yoga may be beneficial for those with RLS, interpretation is hindered by design and other methodological limitations, including lack of a control group,38 restriction to women,14,38 and lack of RLS-specific measures.14 Designed to help address these limitations, this pilot randomized controlled trial (RCT) investigated the effects of a gentle yoga versus an educational film (EF) program on RLS symptoms and symptom severity, and on the associated outcomes of sleep, mood, perceived stress, and QOL in adults with moderate to severe RLS.
METHODS
Study participants and methods for this exploratory RCT are described in the next paragraphs and in the literature.8 The study was approved by the West Virginia University (WVU) Institutional Review Board (IRB), The Ohio State University (OSU) IRB, and the National Center for Complementary and Integrative Health/National Institutes of Health Office of Clinical and Regulatory Affairs.
Study participants
Eligible participants were community-dwelling, ambulatory adults aged 18 years or older with moderate to severe RLS defined as follows: (1) symptoms that meet all five of the International Restless Legs Syndrome Study Group Rating Scale (IRLS) essential diagnostic criteria for RLS2,39 (an urge to move the legs, often associated with discomfort or disagreeable sensations in the legs, that begins or worsens during periods of rest or inactivity, is partially or totally relieved by movement, is worse or only occurs in the evening or night, and is not solely accounted for by another condition [eg, positional discomfort, leg cramps, habitual foot tapping]); (2) RLS symptoms at least once a week in the past 3 months; (3) a score of at least 2 points (moderate) on IRLS question 6: “How severe was your RLS as a whole?”40,41; and (4) confirmation of RLS diagnosis and study eligibility by a physician trained in sleep medicine. These criteria helped to ensure exclusion of mimics (such as positional discomfort, leg cramps, arthritis pain.).5,42 We excluded those who screened positive for anemia (hemoglobin [Hb] levels < 12 g/dL for women,<13 g/dL for men); had practiced yoga within the past year; were currently on antipsychotic medication or had changed dosage of dopaminergic or any other central nervous system agents (eg, opiates, sedative hypnotics, anticonvulsants, adrenolytic agents, benzodiazepines) within the past 3 months; had any orthopedic, neurologic or other concomitant condition that could prevent safe completion of a 12-week yoga program or confound assessments (eg, neuropathy; Parkinson disease; stroke; rheumatoid arthritis; renal or heart failure; sleep apnea; myocardial infarction within the past 6 months; cancer (except nonmelanoma skin cancer); had evidence of anemia; or were pregnant or within 6 months postpartum. These exclusion criteria are consistent with those commonly used in trials of RLS drugs and other RLS interventions.43–48
Recruitment and screening
Participants were recruited from the Morgantown, West Virginia metropolitan area (WVU site) and Columbus, Ohio (OSU site) via a combination of print and electronic advertisements, flyers, and brochures posted in public places such as community bulletin boards (physical and electronic); health center waiting areas, work place settings, churches, the Intranet, and other venues. In the WVU site, recruitment letters were sent to all adults visiting a local WVU Medicine clinic who had received a diagnosis of RLS (ICD-9 code: 333.94, 333.99) within the past 5 years. Eligibility criteria were reviewed with all potential participants via telephone, along with the study protocol, timing, and class schedules.
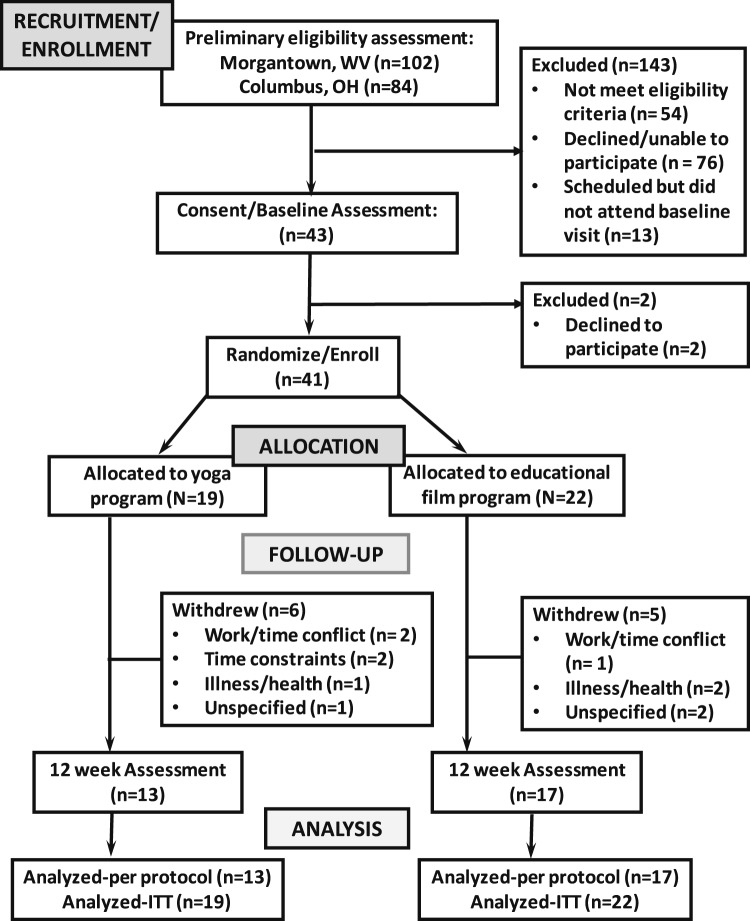
At visit 1, following informed consent each consented adult still interested in participating was formally screened for trial eligibility using a standard screening checklist,8 with RLS confirmed via consultation with the study physician. Hb levels were also measured using a simple, hand-held pulse oximetry Hb monitor (Masimo Pronto); any individuals with evidence of anemia (Hb levels < 12 g/dL for women, < 13 g/dL for men) were excluded (n = 1). Participants meeting all eligibility criteria then underwent a comprehensive baseline assessment and treatment randomization. Of a total of 186 potential participants who made initial inquiries, (102 WVU, 84 OSU), 56 indicated that they were eligible, willing, and available to participate and were scheduled for a consent visit, full eligibility screen, and baseline assessment. Of these, 41 were ultimately enrolled in the study (Figure 1).
Figure 1. Study flow diagram.
Treatment allocation and randomization
Following confirmation of eligibility and baseline assessment, randomization was performed by a team member who had no advance knowledge of treatment allocation; uniquely numbered, sealed, opaque envelopes containing information regarding the participant’s assigned intervention were given to each participant in sequence; as in previous studies, participants were instructed to open their envelopes upon exiting the building. Enrolled participants were randomized to one of the two treatment groups described in the next paragraphs, in a 1:1 ratio, based on the allocation sequence generated by the study statistician using a permuted block design.8 The statistician, who had no contact with participants, generated the randomized assignment master list and provided the sequentially numbered opaque envelopes containing the group assignment and corresponding study forms. The list linking participant numbers with personally identifiable information was maintained by the study coordinator.
Baseline and outcome assessments
Participants underwent an assessment at baseline and following the 12-week intervention period. All assessments and data entry were performed by trained study personnel blinded to participant treatment assignment. Detailed baseline information was gathered on medical and reproductive history, demographic characteristics, body mass index (BMI, kg/m2), and lifestyle factors. The primary outcome for this study was RLS symptomatology, measured using the IRLS, a 10-item scale that includes questions related to frequency, intensity, and impact.40 The IRLS is considered the gold standard for measuring RLS symptoms,49 and is recommended for use in RLS clinical trials by the European RLS Study Group50 and other RLS experts51; this instrument is widely used both in the United States and internationally.1,9 We also evaluated the effects of yoga on RLS symptom severity using the IRLS severity subscale52 (considered relatively robust to placebo effects50), and the single-item RLS ordinal scale.48,53
Secondary outcomes included sleep quality, mood, perceived stress, and health-related QOL, endpoints recommended for inclusion in all clinical trials of RLS.15,50 These outcomes were assessed via a short battery of self-report instruments commonly used in pharmaceutical trials of patients with RLS.54–57 Sleep quality was assessed using the 9-item Pittsburgh Sleep Quality Index58; mood was evaluated using the 65-item Profile of Mood States59 and 10-item Perceived Stress Scale60; and health-related QOL) was measured using the 36-item Medical Outcomes Study Short Form-36 (SF-36).61 These self-report instruments are well-established scales that have been shown to be sensitive to short-term behavioral interventions, and have been validated in a wide range of populations, including patients with RLS.14,59,62–69 Blood pressure and heart rate were also measured in a seated position following a 5-minute rest period, with measurements taken three times using an automatic blood pressure monitor (OMRON HEM-780) and averaged for a final score.
To assess possible change in social support and physical activity (other than yoga) potential confounding factors, participants also completed the 11-item Duke Social Support Index70 and 10-item Physical Activity Scale for Elderly71 at each visit. In addition, information on BMI,2 caffeine and alcohol consumption, smoking, and use of non-RLS medications was gathered at each assessment. To assess expectation of benefit, the Credibility/ Expectancy Questionnaire72 was collected from participants after their first class. Participants were also asked to record use of other RLS treatments on their weekly logs (see next paragraphs). In addition, all participants were asked to complete a short, anonymous exit questionnaire, modeled after that used in our previous trials.73
Interventions
Yoga program (active intervention)
Participants randomized to the yoga group completed a 12-week gentle Iyengar yoga program based on that developed and successfully implemented in our two pilot studies14,38 and finalized following detailed review and input from an Iyengar Master Trainer. Participants attended two 75-minute classes per week for the first 4 weeks, then one 75-minute class for the remaining 8 weeks and were asked to complete a 30-minute homework routine 5 days a week on nonclass days. Yoga classes were held at two yoga studios in close proximity to the WVU Health Sciences Center campus (WVU site) and OSU Center for Integrative Health and Wellness (OSU site), respectively. As in our prior trials,14,38 each yoga class began with simple yogic centering and breathing exercises, followed by a sequence of active and restorative poses (asanas), and ending with a 10-minute guided supine relaxation practice. The yoga routines, including a collective total of 25 commonly used asanas, were tailored for sedentary adults naïve to yoga, designed to increase gradually in difficulty as participants progress. Pose modifications and props (eg, chairs, blankets, and straps) were used as needed to allow all participants to perform the poses safely and easily. In addition, each class was restricted to a maximum of 12 participants to allow for personalized attention if needed. All study yoga instructors were certified in Iyengar yoga (≥ 500 hours), with a minimum of 5 years’ experience teaching adults with a range of chronic health conditions; all were specifically trained in the final RLS yoga protocol by lead study yoga teacher, Dr. Kimberly Williams. To facilitate home practice, all participants received yoga mats and straps, along with a yoga DVD and a comprehensive, indexed training manual illustrating the homework routines.8
Educational film program (comparator)
Participants assigned to the film group attended one 75-minute class per week for 12 weeks, and were asked to complete, as their study homework assignments, a daily log at home recording any RLS or sleep treatments they tried. Class sizes were equivalent to those in the yoga group to facilitate personal interaction with the instructor. At the first class, film group participants received a comprehensive set of lay educational materials regarding RLS symptoms, causes, and epidemiology and detailing recommended nonpharmacologic approaches to RLS management based on current national guidelines. Classes were held in an easily accessible private seminar room on the WVU or OSU campus, and were administered by health educators familiar with sleep disorders and common nonpharmacologic treatments and specifically trained for this purpose. Each class began with a brief meet-and-greet period, followed by a 60-minute instructional film segment, and a 10- to 15-minute group discussion.
As described in detail elsewhere,8 course content for this standardized film education program included a total of 11 films providing information on: RLS symptoms, epidemiology, and management, including sleep hygiene practices; other sleep disorders and associated comorbidities; and on mind-body and other complementary therapies likely to be of interest to those participating in a yoga and sleep education study. The film selection procedure was similar to that used in our earlier studies.8,14,73
Upon study completion, yoga group participants were given access to all EF group materials and films; the film group participants received all yoga homework materials, as well as a half- day workshop in yoga for RLS. All participants were given modest compensation for their time and travel expenses.
Adherence and adverse events
Yoga and film class attendance was recorded by the instructor on standardized check sheets. Yoga participants also completed a daily log after each home practice session, indicating the number of minutes practiced, as well as any comments regarding the session; as noted previously, film group participants documented any RLS treatments used on their daily log, along with any comments or perceptions. Daily logs were turned in to the participant’s respective instructor at the first group class each week. Logs and attendance records were collected weekly.
Adverse events were tracked via weekly review of participant logs. At the beginning of each class, the instructor also queried participants discretely regarding any potential problems; these were likewise recorded. A trained study team member also followed up with all participants within the first 10 days following the onset of the intervention, and periodically thereafter to address any potential issues or questions. In addition, participants were encouraged to contact study investigators and/or staff if they had any questions or concerns.
Fidelity
Program fidelity was assessed at least twice for each cohort and intervention. A trained study team member recorded adherence to the intervention protocol using a standardized check list tailored for this study. The study coordinator and principal investigator were notified of any protocol deviations, and these were immediately discussed with the instructor(s) and corrective action, if necessary, taken.
Statistical analysis
Data analysis was performed using SPSS, Version 25 (IBM Corp, Armonk, New York, United States). Baseline differences between the intervention groups, between participants at the two sites, and between dropouts and nondropouts were assessed using chi-square (for categorical variables), independent samples t tests (for normally distributed continuous variables), or Mann-Whitney U tests (for ordinal or continuous variables with evidence of skewing). Potential differences between treatment groups were analyzed using chi-square for retention, and one-way analysis of variance for treatment expectancies and adherence. In preliminary assessments, within-group changes over time at 3 months were assessed using analysis of covariance with baseline scores and site as covariates; site-adjusted between-group differences in treatment outcomes were assessed using repeated-measures analysis of variance. Distributions of dependent variables were examined to ensure the assumptions of normality and sphericity were met and variables transformed as necessary. In our intention-to-treat analyses, we used the SPSS multiple imputation function (10 iterations) to handle missing data.74 As this was a pilot feasibility study, alpha was set at 0.05. Effect sizes were calculated using Cohen d. Bivariate correlations were performed using Pearson r. To assess the potential influence of RLS medication use and medication change, we conducted additional analyses, both adjusting for these factors statistically and excluding those reporting use or change in RLS medication.
RESULTS
Baseline characteristics
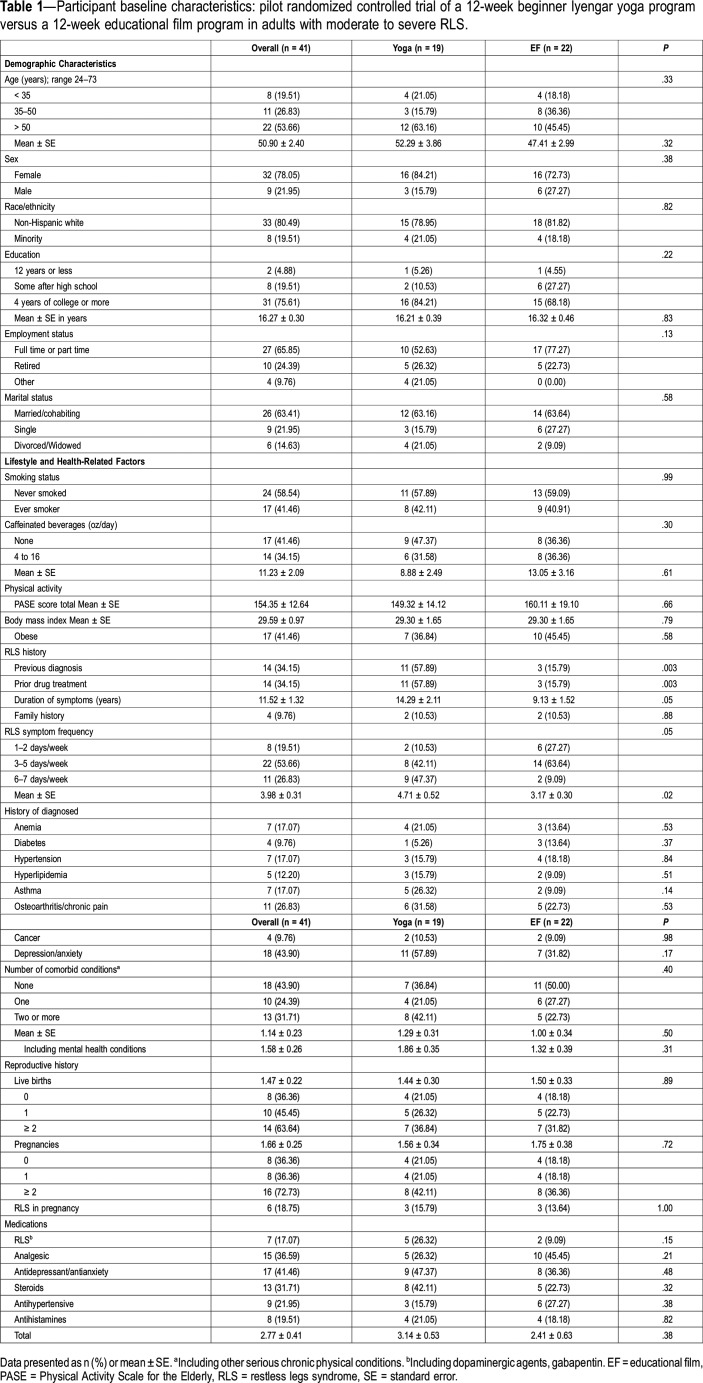
A total of 41 eligible adults with moderate to severe RLS were enrolled in the final study (15 from the WVU site, 26 from the OSU site). Participant characteristics, stratified by treatment group, are given in Table 1. Participant age ranged from 24 to 73 years (mean ± standard error [SE] = 50.9 ± 2.4 years). Most participants were female (78%) and non-Hispanic white (80.5%), college educated (75.6%), married or cohabiting (63.4%), and employed full time (65.9%) or part time (24.4%). Most consumed caffeinated beverages (58.5%), had never smoked (58.5%), and had received a diagnosis of at least one chronic comorbid condition (56.1%), with 43.9% reporting a history of depression or anxiety disorder (Table 1). Over 40% of participants were obese (mean BMI = 29.6 ± 1.0 kg/m2); 41.5% were taking at least three medications. Most (80.5%) reported RLS symptoms at least 3 days a week, with 56.1% scoring in the severe to very severe range, and 17.1% indicating they currently were on RLS medications.
Table 1.
Participant baseline characteristics: pilot randomized controlled trial of a 12-week beginner Iyengar yoga program versus a 12-week educational film program in adults with moderate to severe RLS.
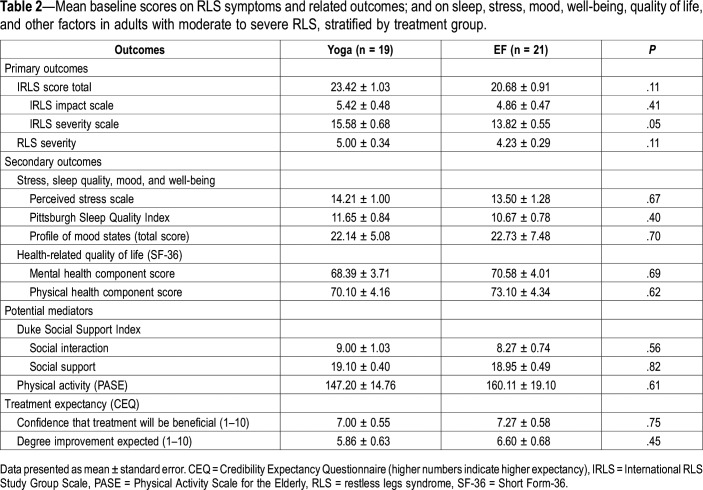
Between-group differences at baseline
The yoga and EF group did not differ significantly in baseline demographics, in lifestyle characteristics, or in reproductive or medical history (P > .1, Table 1) Although 7 participants (17%) indicated a prior history of anemia, no participants had evidence of anemia or were undergoing treatment for this condition. However, yoga group participants were more likely to have a previous diagnosis of RLS and to have more frequent RLS symptoms (P ≤ .05, Table 1). As detailed in Table 2, yoga group participants also scored significantly higher on the IRLS severity subscale, but did not differ significantly in other measures of RLS symptom frequency, severity, or impact (P > .1), or in measures of stress, sleep quality, mood, QOL, social support or physical activity (P ≥ .3). Likewise, the two groups indicated similar expectations regarding treatment benefit (P ≥ .45).
Table 2.
Mean baseline scores on RLS symptoms and related outcomes; and on sleep, stress, mood, well-being, quality of life, and other factors in adults with moderate to severe RLS, stratified by treatment group.
OSU participants reported significantly lower frequency and severity of RLS symptoms than did those from the WVU site (P < .05) and were more likely to indicate full-time or part-time employment (P = .04), but did not differ significantly in other baseline characteristics or scores or in treatment expectations.
Retention and adherence
Of the original 41 participants, 30 (73%) completed the 12-week study and follow-up assessment (13 yoga, 17 EF). Reasons for dropout included: change in work schedule (n = 3), unexpected health issues unrelated to the study (n = 3), time constraints (n = 2), and unspecified (n = 3). Attrition rates did not differ between groups or sites (P > .4). Dropouts reported significantly shorter duration of RLS than did those completing the study (7.3 ± 1.5 versus 13.3 ± 1.6 years, P < .01) but did not otherwise differ in any demographic or lifestyle factors, medical history, BMI, or other health-related factors, treatment expectations, or baseline scores on any measure (P ≥ .4).
Among those who completed the study, adherence exceeded our target goals for the study,8 with participants in the yoga and EF group attending an average of 13.0 ± 0.84 (81%) and 10.3 ± 0.3 classes (85%), respectively. Yoga group participants completed an average of 45.5 ± 3.8 (81%) homework sessions and 1.9 ± 0.6 breathing exercises/nonclass day. Adherence did not differ significantly by site or by treatment assignment (class attendance).
Change over time
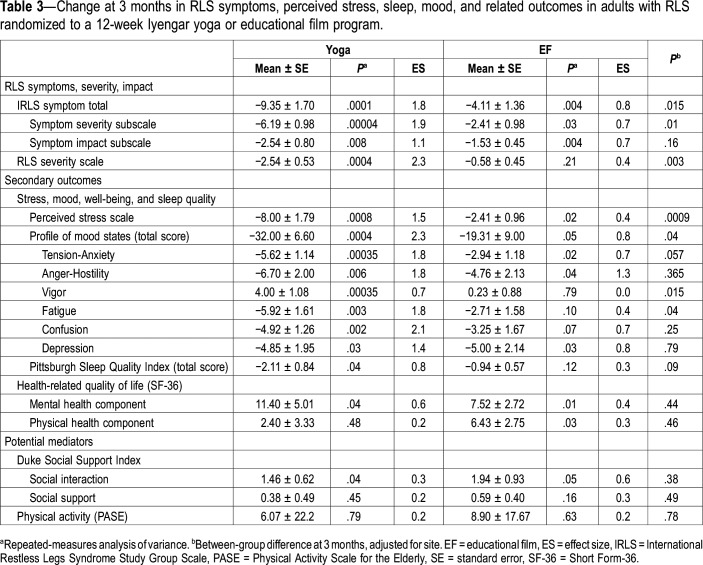
As detailed in Table 3, both the yoga and EF groups improved significantly over time in their IRLS symptom scores, overall and in both subscales (P ≤ .03), although only yoga group participants showed significant reductions in the RLS Severity Scale (P = .0004). Likewise, both groups showed significant improvements in perceived stress, mood (overall and several subscales, ie, tension-anxiety, anger-hostility, depression), and QOL-mental health (P < .05). Yoga group participants also showed significant improvements in other mood domains (vigor, fatigue, confusion, Ps ≤ .003) and in sleep quality (P = .04), whereas the EF group participants indicated significant gains in QOL-physical health (P = .04).
Table 3.
Change at 3 months in RLS symptoms, perceived stress, sleep, mood, and related outcomes in adults with RLS randomized to a 12-week Iyengar yoga or educational film program.
Relative to the EF group, the yoga group demonstrated significantly greater improvement in RLS symptom burden as measured by the IRLS total and severity subscale (P ≤ .015) and the RLS Severity Scale (P = .003) (Table 3). Although a higher percentage of yoga than EF group participants tested in the severe to very severe range at baseline (61.5 versus 47.1%), 77% of yoga group participants tested in the minimal range at 12 weeks, with no participants scoring in the severe range, versus 23.4% and 12%, respectively in the education group (P < .05). Yoga group participants also showed significantly greater improvements in perceived stress (P = .0009), marginally significant reductions in sleep impairment (P < .09), as well as greater improvements in mood, both overall (P = .04) and in certain individual domains, including vigor (P = .015), fatigue (P = .04), and tension-anxiety (P = .057). Improvements in QOL did not differ by treatment group, nor did changes in either social support or physical activity. Repeated intention-to-treat analyses yielded similar results. Additional adjustment for medication change, prior history of anemia, report of previous RLS diagnosis or drug treatment, RLS duration, or treatment expectations did not appreciably alter the findings. Exclusion of those on dopaminergic medications (n = 3 yoga, 2 EF group participants) in the analyses slightly strengthened the between-group differences in sleep quality (mean differences in the yoga versus film (P = .056) but did not substantively alter other findings.
In the yoga group, class attendance was significantly and positively associated with improvement in RLS symptom burden in the yoga group (r for IRLS and RLS severity scale = .4 and .5, respectively, P ≤ .05), as were the number of home practice sessions (r for IRLS and RLS severity scale = .6 and .7, respectively, P ≤ .03). Likewise, home practice sessions were significantly correlated with improvements in perceived stress (r = .5), several domains of mood (overall, depression, fatigue, and vigor, r = .45–.6), and QOL-mental health (r = .6) (P ≤ .05).
In contrast, EF participants showed no significant relationships between adherence (class attendance) and reduction in RLS symptom burden (r's = .1–.2, P's > .2) or improvement in any measure of stress, mood, or QOL. Sixteen EF group participants (94%) reported regular use of nonpharmacologic RLS management strategies recommended in the films and readings, often in combination. For example, 82% used relaxation practices, including hot showers/baths (60%), stretching and progressive muscle relaxation (59%), and breathing exercises, visualization, and/or yoga/meditation (59%). Eight EF participants (41%) used exercise to help reduce their symptoms, and several employed sleep hygiene practices (n = 4), sought care from an alternative/allied health care provider (n = 4), and/or used other measures (n = 13).
Treatment expectations were unrelated to change in any outcome in either group. No adverse events were observed or reported.
DISCUSSION
To our knowledge, this preliminary investigation is the first RCT to assess the potential efficacy of yoga for reducing RLS symptoms and symptom severity, and the first RCT specifically designed to examine the potential benefits of this popular mind-body therapy for adults with RLS. Consistent with findings from our two pilot studies in women with RLS,38,75 findings of this preliminary RCT suggest that a gentle 12-week yoga program can significantly alleviate RLS symptoms and symptom severity, improve mood, and reduce perceived stress in adults with moderate to severe RLS. In this preliminary study, participants completing a 12-week yoga program showed significant improvements relative to those in the EF group in RLS symptoms and burden overall as measured by both the IRLS and the RLS Severity Scale. Effect sizes were moderate to large, and, in the yoga group, all but 3 adults (all in the severe to very severe range at baseline) tested in the minimal to mild RLS symptom range following the 12-week yoga program, indicating a robust response rate to this nonpharmacologic therapy.
Studies of yoga for RLS are limited to our two previous pilot trials in women, including a nested RCT of 20 sedentary older women at risk for cardiovascular disease that did not include RLS-specific measures,14 and a single arm study of 13 community-dwelling women with moderate to severe RLS.38 In agreement with findings from our prior research, participants assigned to the yoga program showed significant attenuation of RLS symptoms and symptom severity, with pre-post effect sizes ranging from 1.8 for IRLS total to 2.3 for RLS severity. The reductions in RLS symptoms and symptom severity observed in the current study are comparable to or greater than those documented in several previous controlled trials of exercise interventions in adults with RLS.48,76–81 In four RCTs of adults with RLS who were on hemodialysis (total n = 178), participants assigned to a 4-week76 to 6-month77 exercise program showed significant declines in RLS symptoms and symptom severity compared to those receiving a placebo medication77 or no intervention/usual care76,78,79; pre-post effect sizes for RLS symptoms overall ranged from an estimated 1.179 to 2.5576 (estimated weighted mean effect size = 1.85), with only one study, a 3-arm, 4-week study of 90 Iranian adults with severe RLS demonstrating an effect size greater than 1.6.
Similarly, an RCT of 23 community-dwelling adults reported significant declines in RLS symptoms and symptom severity in those assigned to a 12-week exercise program relative to those receiving usual care,48 with pre-post effect sizes of 1.4 and 0.9 for IRLS total and RLS severity, respectively. In contrast, a recent 6-week, 3-arm RCT of exercise versus discussion/waitlist in 18 Australian adults81 showed no differences between groups in RLS symptoms or symptom severity; as in our study, both the active and control groups in this study showed significant improvements, although estimated effect sizes for the active (exercise) intervention were more modest (1.1 IRLS total, 0.55 for RLS severity) than those observed in our trial. By contrast, in all other studies of exercise and RLS, participants assigned to the control group demonstrated either no change or nonsignificant deterioration in symptoms.48,76–79 This discrepancy may be due in part to the choice of control group. Whereas the latter studies used a usual care/no intervention control, we, like Harrison et al,81 used a more active comparator designed, at minimum, to control for time, attention, and setting. Moreover, almost all participants in the EF group engaged in RLS management strategies recommended in the films and readings, perhaps helping to explain the improvements observed in this group.
Likewise, the improvements in sleep, mood and perceived stress observed in this exploratory RCT are consistent with those demonstrated in our recent pilot trials regarding the effects of yoga in women with RLS.14,38 However, the three studies assessing the effects of exercise on psychosocial outcomes in adults with RLS (two RCTs77,81 and one non-RCT80 in adults with77,80 and without end-stage renal disease14,81) have yielded mixed findings. One study, a small community-based RCT, reported significant reductions in sleep impairment, global stress, and depressive symptoms in both the exercise and control groups, but no between-group differences in any outcome.81 In a small three-arm RCT of patients on hemodialysis, participants completing the 6-month exercise program showed no change in measures of sleep quality (effect sizes 0.0–0.1), but a significant improvement in depressive symptoms relative to those in the placebo group (with the latter demonstrating significant deterioration).77 In contrast, a non-RCT in 14 hemodialysis patients indicated significant improvement in sleep quality (one measure) but not depression following a 16 week exercise program, although between-group differences were not reported.80 In agreement with the two RCTs in patients with RLS on hemodialysis,77,79 we found no evidence for between-group differences in QOL, although both the yoga and the EF groups showed significant within group improvements in QOL-mental health.
Although the mechanisms underlying the improvements observed following completion of the yoga program in this study remain unknown, yoga may benefit those experiencing RLS via several possible interrelated pathways.8,14,38 For example, yoga may reduce RLS symptoms and symptom burden by decreasing sympathoadrenal and hypothalamic–pituitary-adrenal axis activation, restoring parasympathetic/sympathetic balance, and improving cardiometabolic function, factors linked to RLS etiology and progression, and bidirectionally associated with sleep impairment, mood disturbance, stress, and poor QOL.9,82 In addition, findings from neurophysiological and neuroimaging studies83–86 suggest that yogic practices may, by selectively activating specific neurochemical systems implicated in RLS, also promote beneficial changes in autonomic, neuroendocrine, and metabolic function, and in sleep, mood, and pain processing, changes which may, in turn, lead to reduced RLS symptoms and symptom burden.8,14,38 Yoga may also lower motor cortex excitability and promote muscle relaxation, factors implicated in RLS pathophysiology.14,87
Notably, improvements in RLS symptoms, sleep, and mood observed following our 12-week yoga program were comparable or superior to those reported in recent meta-analytic reviews of RLS medication trials.21,88 In addition, no adverse events were reported, retention was acceptable, and compliance very good overall. Together, these findings suggest that yoga may offer a safe and viable complement or alternative to pharmacologic treatment for patients with this burdensome disorder. Given the promising findings of this exploratory RCT, larger, longer term RCTs are warranted to further evaluate the efficacy of yoga for the management of RLS.
Strengths and limitations
Strengths of this study are several, including the community-based design, recruitment of participants from two sites, randomization of participants and between-group similarity in most baseline characteristics, acceptable participant retention, overall excellent adherence, and a comparison condition designed to help control for time, attention, and social interaction. The study population comprised a diverse sample of adults characterized by broad variation in demographic, lifestyle, and health-related characteristics. All participants tested in the moderate to severe range, with symptom scores comparable to those of participants in other RLS intervention trials.48,77–79,81,88 In addition to change in RLS symptoms and symptom severity, we also assessed change in sleep quality, mood, and QOL, recommended endpoints for clinical trials of RLS.15 To account for the potential placebo effects, we also measured treatment expectations after the first class, as well as change in social support/interaction to account for the potential influence of these factors.
This pilot RCT also has several limitations. Sample sizes were small, limiting power and generalizability. However, we observed significant improvement in the yoga versus control group in RLS symptoms and symptom severity, as well as in several other clinically important parameters, again arguing for a potential beneficial effect of the yoga program. Although the EF program was designed to help control for staff attention, setting, and time, class time requirements were higher in the yoga group and EF participants did not receive formal home practice assignments. However, EF group instructions to complete daily treatment logs were specifically framed as homework, and all but one EF participant reported regular engagement in nonpharmacologic approaches recommended in the educational films and reading materials. Nonetheless, because we did not require EF participants to record the time expended on these treatments, we cannot directly compare time expenditures on these home-based activities with those of the yoga group home practice, and thus cannot rule out the potential influence of differential time expenditure on the observed improvements in the yoga versus EF group. In addition, although assessors were blinded to participant treatment status, participants could not be masked. However, treatment expectancies did not differ between-groups, expectations were unrelated to change in outcomes, and adjustment for treatment expectancies did not substantively alter findings, suggesting that placebo effects did not explain the observed findings. Moreover, observed effect sizes were substantially larger than would be expected with placebo,89 and significantly greater than those observed in control groups for RLS symptoms, symptom severity, and other clinically important outcomes. Yoga group participants reported longer duration of RLS symptoms at baseline, and were more likely to report a prior RLS diagnosis. However, adjustment for neither symptom duration nor previous diagnosis appreciably altered findings, suggesting that these factors did not account for the observed between-group differences and that yoga may offer a viable therapeutic option even in patients with long-standing RLS. Finally, the study population was drawn from only two sites and was predominantly female and well educated, potentially limiting generalizability to other populations and geographic regions. Participants may also have been particularly receptive to yoga and other nonpharmacologic therapies (as reflected in the comparator group’s active participation in the latter), again raising the possibility of selection bias and potentially limiting generalizability to adults less receptive to nonpharmaceutical treatment of RLS. Finally, outcomes were assessed only before and after the 12-week intervention period, precluding determination of potential longer term effects of the yoga program on RLS symptom burden or other clinically important endpoints.
CONCLUSIONS
Findings of this exploratory RCT suggest that yoga may offer a safe, viable, and effective intervention for reducing RLS symptoms and symptom severity, sleep and mood disturbance, and perceived stress in adults with moderate to severe RLS. Larger RCTs are needed to confirm these benefits in this and other adult populations with RLS, to assess the long-term effects of yoga in patients with RLS, and to evaluate potential underlying mechanisms.
DISCLOSURE STATEMENT
All authors have read and approved the manuscript. Work for this study was performed at West Virginia University and The Ohio State University. This work was supported by the National Center for Complementary and Integrative Health (grant numbers 1 R15 AT008606-01A1 and 3 R15 AT008606-01A1S1). The contents are solely the responsibility of the authors and do not represent the official views of West Virginia University, The Ohio State University, or the National Institutes of Health. The authors report no conflicts of interest.
ACKNOWLEDGMENTS
The authors thank Drs. Kimberly Williams, lead study yoga teacher, and Lois Steinberg for their valuable contributions to the development of the RLS yoga program, to Raquel Graham for her work as a study instructor, and to Christine Junk and Madelaine Flick for their assistance with data collection.
ABBREVIATIONS
- BMI
Body mass index
- CEQ
Credibility Expectancy Questionnaire
- EF
Educational film
- ES
Effect size
- dL
Deciliter
- g
Gram
- Hg
Hemoglobin
- ICD-9
International Classification of Diseases, 9th Revision
- IRB
Institutional Review Board
- IRLS
International Restless Legs Syndrome Study Group Rating Scale
- ITT
Intent to treat
- kg
Kilogram
- OSU
The Ohio State University
- m
Meter
- PASE
Physical Activity Scale for the Elderly
- QOL
Quality of life
- RCT
Randomized controlled trial
- RLS
Restless Legs Syndrome
- SE
Standard error
- SF-36
Medical Outcomes Study Short Form-36
- SPSS
Statistical Package for the Social Sciences
- WVU
West Virginia University
REFERENCES
- 1.Innes KE, Selfe TK, Agarwal P. Prevalence of restless legs syndrome in North American and Western European populations: a systematic review. Sleep Med. 2011;12(7):623–634. doi: 10.1016/j.sleep.2010.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allen RP, Picchietti D, Hening WA, et al. Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med. 2003;4(2):101–119. doi: 10.1016/s1389-9457(03)00010-8. [DOI] [PubMed] [Google Scholar]
- 3.Durgin T, Witt EA, Fishman J. The humanistic and economic burden of restless legs syndrome. PLoS One. 2015;10(10):e0140632. doi: 10.1371/journal.pone.0140632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salas RE, Kwan AB. The real burden of restless legs syndrome: clinical and economic outcomes. Am J Manag Care. 2012;18(9, Suppl):S207–S212. [PubMed] [Google Scholar]
- 5.Garcia-Borreguero D, Stillman P, Benes H, et al. Algorithms for the diagnosis and treatment of restless legs syndrome in primary care. BMC Neurol. 2011;11(1):28. doi: 10.1186/1471-2377-11-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hornyak M. Depressive disorders in restless legs syndrome: epidemiology, pathophysiology and management. CNS Drugs. 2010;24(2):89–98. doi: 10.2165/11317500-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 7.Hening WA, Allen RP, Chaudhuri KR, et al. Clinical significance of RLS. Mov Disord. 2007;22(S18):S395–S400. doi: 10.1002/mds.21665. [DOI] [PubMed] [Google Scholar]
- 8.Selfe TK, Wen S, Sherman K, Klatt M, Innes KE. Acceptability and feasibility of a 12-week yoga vs. educational film program for the management of restless legs syndrome (RLS): study protocol for a randomized controlled trial. Trials. 2019;20(1):134. doi: 10.1186/s13063-019-3217-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Innes KE, Selfe TK, Agarwal P. Restless legs syndrome and conditions associated with metabolic dysregulation, sympathoadrenal dysfunction, and cardiovascular disease risk: a systematic review. Sleep Med. Rev. 2012;16(4):309–339. doi: 10.1016/j.smrv.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 10.Allen RP, Bharmal M, Calloway M. Prevalence and disease burden of primary restless legs syndrome: results of a general population survey in the United States. Mov Disord. 2011;26(1):114–120. doi: 10.1002/mds.23430. [DOI] [PubMed] [Google Scholar]
- 11.Khan FH, Ahlberg CD, Chow CA, Shah DR, Koo BB. Iron, dopamine, genetics, and hormones in the pathophysiology of restless legs syndrome. J Neurol. 2017;264(8):1634–1641. doi: 10.1007/s00415-017-8431-1. [DOI] [PubMed] [Google Scholar]
- 12.Garcia Borreguero DG, Winkelmann J, Allen RP. Introduction: towards a better understanding of the science of RLS/WED. Sleep Med. 2017;31:1–2. doi: 10.1016/j.sleep.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 13.Leschziner GD. Restless Legs Syndrome. In: Selsick H, ed. Sleep Disorders in Psychiatric Patients. London: Springer; 2018:175-188. [Google Scholar]
- 14.Innes KE, Selfe TK. The effects of a gentle yoga program on sleep, mood, and blood pressure in older women with restless legs syndrome (RLS): a preliminary randomized controlled trial. Evid Based Complement. Alternat Med. 2012;2012(294058):1–14. doi: 10.1155/2012/294058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Earley CJ, Silber MH. Restless legs syndrome: understanding its consequences and the need for better treatment. Sleep Med. 2010;11(9):807–815. doi: 10.1016/j.sleep.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 16.Allen RP, Stillman P, Myers AJ. Physician-diagnosed restless legs syndrome in a large sample of primary medical care patients in western Europe: prevalence and characteristics. Sleep Med. 2010;11(1):31–37. doi: 10.1016/j.sleep.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 17.Garcia-Borreguero D, Kohnen R, Silber MH, et al. The long-term treatment of restless legs syndrome/Willis-Ekbom disease: evidence-based guidelines and clinical consensus best practice guidance: a report from the International Restless Legs Syndrome Study Group. Sleep Med. 2013;14(7):675–684. doi: 10.1016/j.sleep.2013.05.016. [DOI] [PubMed] [Google Scholar]
- 18.Trenkwalder C, Winkelmann J, Inoue Y, Paulus W. Restless legs syndrome-current therapies and management of augmentation. Nat Rev Neurol. 2015;11(8):434–445. doi: 10.1038/nrneurol.2015.122. [DOI] [PubMed] [Google Scholar]
- 19.Buckner AC. The use of dopamine agonist in the treatment of restless legs syndrome: caution for practitioners and bipolar patients. South Med J. 2008;101(8):785. doi: 10.1097/SMJ.0b013e31817c6bb4. [DOI] [PubMed] [Google Scholar]
- 20.Spiegelhalder K, Hornyak M. Restless legs syndrome in older adults. Clin Geriatr Med. 2008;24(1):167–180. doi: 10.1016/j.cger.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 21.Wilt TJ, Macdonald R, Ouellette J, et al. Pharmacologic therapy for primary restless legs syndrome: a systematic review and meta-analysis. JAMA Intern Med. 2013;173(7):496–505. doi: 10.1001/jamainternmed.2013.3733. [DOI] [PubMed] [Google Scholar]
- 22.Milligan SA, Chesson AL. Restless legs syndrome in the older adult: diagnosis and management. Drugs Aging. 2002;19(10):741–751. doi: 10.2165/00002512-200219100-00003. [DOI] [PubMed] [Google Scholar]
- 23.Wolkove N, Elkholy O, Baltzan M, Palayew M. Sleep and aging: 2. Management of sleep disorders in older people. CMAJ. 2007;176(10):1449–1454. doi: 10.1503/cmaj.070335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cochen V, Arbus C, Soto ME, et al. Sleep disorders and their impacts on healthy, dependent, and frail older adults. J Nutr Health Aging. 2009;13(4):322–329. doi: 10.1007/s12603-009-0030-0. [DOI] [PubMed] [Google Scholar]
- 25.Garcia-Borreguero D, Allen R, Kohnen R, et al. Loss of response during long-term treatment of restless legs syndrome: Guidelines approved by the International Restless Legs Syndrome Study Group for use in clinical trials. Sleep Med. 2010;11(9):956–957. doi: 10.1016/j.sleep.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 26.Bozorg AM. Restless Legs Syndrome Treatment & Management. https://emedicine.medscape.com/article/1188327-treatment. Updated February 22, 2017. Accessed November 19, 2019.
- 27. Restless Legs Syndrome Foundation. Restless Legs Syndrome: Causes, Diagnosis and Treatment. Austin, TX: Restless Legs Syndrome Foundation; 2018.
- 28.Harrison EG, Keating JL, Morgan PE. Non-pharmacological interventions for restless legs syndrome: a systematic review of randomised controlled trials. Disabil Rehabil. 2019;41(17):2006–2014. doi: 10.1080/09638288.2018.1453875. [DOI] [PubMed] [Google Scholar]
- 29.Saper R, Eisenberg D, Davis R, Culpepper L, Phillips R. Prevalence and patterns of adult yoga use in the United States: results of a national survey. Altern Ther Health Med. 2004;10(2):44–49. [PubMed] [Google Scholar]
- 30.Barnes PM, Bloom B. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Rep. 2008;12:1–24. [PubMed] [Google Scholar]
- 31.Patel NK, Newstead AH, Ferrer RL. The effects of yoga on physical functioning and health related quality of life in older adults: a systematic review and meta-analysis. J Altern Complement Med. 2012;18(10):902–917. doi: 10.1089/acm.2011.0473. [DOI] [PubMed] [Google Scholar]
- 32.Lin K-Y, Hu Y-T, Chang K-J, Lin H-F, Tsauo J-Y. Effects of yoga on psychological health, quality of life, and physical health of patients with cancer: a meta-analysis. eCAM. 2011;2011:659876. doi: 10.1155/2011/659876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sharma M. Yoga as an alternative and complementary approach for stress management: a systematic review. J Evid Based Complementary Altern Med. 2014;19(1):59–67. doi: 10.1177/2156587213503344. [DOI] [PubMed] [Google Scholar]
- 34.Field T. Yoga research review. Complement Ther Clin Pract. 2016;24:145–161. doi: 10.1016/j.ctcp.2016.06.005. [DOI] [PubMed] [Google Scholar]
- 35.Uebelacker LA, Broughton MK. Yoga for depression and anxiety: a review of published research and implications for healthcare providers. R I Med J (2013) 2016;99(3):20–22. [PubMed] [Google Scholar]
- 36.Büssing A, Ostermann T, Ludtke R, Michalsen A. Effects of yoga interventions on pain and pain-associated disability: a meta-analysis. J Pain. 2012;13(1):1–9. doi: 10.1016/j.jpain.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 37.Posadzki P, Ernst E, Terry R, Lee MS. Is yoga effective for pain? A systematic review of randomized clinical trials. Complement Ther Med. 2011;19(5):281–287. doi: 10.1016/j.ctim.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 38.Innes KE, Selfe TK, Agarwal P, Williams K, Flack KL. Efficacy of an 8-week yoga intervention on symptoms of restless legs syndrome (RLS): a pilot study. J Altern Complement Med. 2013;19(3):139–146. doi: 10.1089/acm.2012.0330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Uzun S, Kozumplik O, Jakovljevic M, Sedic B. Side effects of treatment with benzodiazepines. Psychiatr. Danub. 2010;22(1):90–93. [PubMed] [Google Scholar]
- 40.Walters AS, LeBrocq C, Dhar A, et al. Validation of the International Restless Legs Syndrome Study Group rating scale for restless legs syndrome. Sleep Med. 2003;4(2):121–132. doi: 10.1016/s1389-9457(02)00258-7. [DOI] [PubMed] [Google Scholar]
- 41.Hening WA, Allen RP. Restless legs syndrome (RLS): the continuing development of diagnostic standards and severity measures. Sleep Med. 2003;4(2):95–97. doi: 10.1016/s1389-9457(03)00009-1. [DOI] [PubMed] [Google Scholar]
- 42.Benes H, Walters AS, Allen RP, Hening WA, Kohnen R. Definition of restless legs syndrome, how to diagnose it, and how to differentiate it from RLS mimics. Mov Disord. 2007;;22(Suppl 18):S401–S408. doi: 10.1002/mds.21604. [DOI] [PubMed] [Google Scholar]
- 43.Inoue Y, Kuroda K, Hirata K, Uchimura N, Kagimura T, Shimizu T. Efficacy, safety and dose-response of pramipexole in Japanese patients with primary restless legs syndrome: randomized trial. Neuropsychobiology. 2011;63(1):35–42. doi: 10.1159/000322289. [DOI] [PubMed] [Google Scholar]
- 44.Oertel WH, Stiasny-Kolster K, Bergtholdt B, et al. Efficacy of pramipexole in restless legs syndrome: a six-week, multicenter, randomized, double-blind study (effect-RLS study) Mov Disord. 2007;22(2):213–219. doi: 10.1002/mds.21261. [DOI] [PubMed] [Google Scholar]
- 45.Partinen M, Hirvonen K, Jama L, et al. Efficacy and safety of pramipexole in idiopathic restless legs syndrome: a polysomnographic dose-finding study–the PRELUDE study. Sleep Med. 2006;7(5):407–417. doi: 10.1016/j.sleep.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 46.Trenkwalder C, Benes H, Poewe W, et al. Efficacy of rotigotine for treatment of moderate-to-severe restless legs syndrome: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2008;7(7):595–604. doi: 10.1016/S1474-4422(08)70112-1. [DOI] [PubMed] [Google Scholar]
- 47.Winkelman JW, Sethi KD, Kushida CA, et al. Efficacy and safety of pramipexole in restless legs syndrome. Neurology. 2006;67(6):1034–1039. doi: 10.1212/01.wnl.0000231513.23919.a1. [DOI] [PubMed] [Google Scholar]
- 48.Aukerman MM, Aukerman D, Bayard M, Tudiver F, Thorp L, Bailey B. Exercise and restless legs syndrome: a randomized controlled trial. J Am Board Fam Med. 2006;19(5):487–493. doi: 10.3122/jabfm.19.5.487. [DOI] [PubMed] [Google Scholar]
- 49.Kohnen R, Allen RP, Benes H, et al. Assessment of restless legs syndrome–methodological approaches for use in practice and clinical trials. Mov Disord. 2007;;22(Suppl 18):S485–S494. doi: 10.1002/mds.21588. [DOI] [PubMed] [Google Scholar]
- 50.Trenkwalder C, Kohnen R, Allen RP, et al. Clinical trials in restless legs syndrome–recommendations of the European RLS Study Group (EURLSSG) Mov Disord. 2007;22(Suppl 18):S495–S504. doi: 10.1002/mds.21538. [DOI] [PubMed] [Google Scholar]
- 51.Ekbom K, Ulfberg J. Restless legs syndrome. J Intern Med. 2009;266(5):419–431. doi: 10.1111/j.1365-2796.2009.02159.x. [DOI] [PubMed] [Google Scholar]
- 52.Allen RP, Kushida CA, Atkinson MJ. Factor analysis of the International Restless Legs Syndrome Study Group’s scale for restless legs severity. Sleep Med. 2003;4(2):133–135. doi: 10.1016/s1389-9457(02)00193-4. [DOI] [PubMed] [Google Scholar]
- 53.Collado-Seidel V, Winkelmann J, Trenkwalder C. Aetiology and treatment of restless legs syndrome. CNS Drugs. 1999;12(1):9–20. [Google Scholar]
- 54.Conti CF, de Oliveira MM, Andriolo RB, et al. Levodopa for idiopathic restless legs syndrome: evidence-based review. Mov Disord. 2007;22(13):1943–1951. doi: 10.1002/mds.21662. [DOI] [PubMed] [Google Scholar]
- 55.Conti CF, Oliveira MM, Valbuza JS, Prado LBF, Carvalho LB, Prado GF. Anticonvulsants to treat idiopathic restless legs syndrome: systematic review. Arq Neuropsiquiatr. 2008;66(2B):431–435. doi: 10.1590/s0004-282x2008000300034. [DOI] [PubMed] [Google Scholar]
- 56.Montagna P, Hornyak M, Ulfberg J, et al. Randomized trial of pramipexole for patients with restless legs syndrome (RLS) and RLS-related impairment of mood. Sleep Med. 2011;12(1):34–40. doi: 10.1016/j.sleep.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 57.Kushida CA. Ropinirole for the treatment of restless legs syndrome. Neuropsychiatr Dis Treat. 2006;2(4):407–419. doi: 10.2147/nedt.2006.2.4.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 59.Berger BG, Motl RW. Exercise and mood: a selective review and synthesis of research employing the Profile of Mood States. J Appl Sport Psychol. 2000;12(1):69–92. [Google Scholar]
- 60.Cohen S, Kamararck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 61.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 62.Nyenhuis DL, Yamamoto C, Luchetta T, Terrien A, Parmentier A. Adult and geriatric normative data and validation of the profile of mood states. J Clin Psychol. 1999;55(1):79–86. doi: 10.1002/(sici)1097-4679(199901)55:1<79::aid-jclp8>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 63.Cole JC, Dubois D, Kosinski M. Use of patient-reported sleep measures in clinical trials of pain treatment: a literature review and synthesis of current sleep measures and a conceptual model of sleep disturbance in pain. Clin Ther. 2007;29(11, Suppl):2580–2588. doi: 10.1016/j.clinthera.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 64.Lane JD, Seskevich JE, Pieper CF. Brief meditation training can improve perceived stress and negative mood. Altern Ther Health Med. 2007;13(1):38–44. [PubMed] [Google Scholar]
- 65.Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosom. Med. 2003;65(4):571–581. doi: 10.1097/01.psy.0000074003.35911.41. [DOI] [PubMed] [Google Scholar]
- 66.Johnson SK, Frederick J, Kaufman M, Mountjoy B. A controlled investigation of bodywork in multiple sclerosis. J Altern Complement Med. 1999;5(3):237–243. doi: 10.1089/acm.1999.5.237. [DOI] [PubMed] [Google Scholar]
- 67.McHorney CA, Ware JE, Jr, Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32(1):40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 68.Beusterien KM, Steinwald B, Ware JE., Jr Usefulness of the SF-36 Health Survey in measuring health outcomes in the depressed elderly. J Geriatr Psychiatry Neurol. 1996;9(1):13–21. doi: 10.1177/089198879600900103. [DOI] [PubMed] [Google Scholar]
- 69.Fuhs A, Bentama D, Antkowiak R, Mathis J, Trenkwalder C, Berger K. Effects of short- and long-term variations in RLS severity on perceived health status - the COR-study. PLoS One. 2014;9(4):e94821. doi: 10.1371/journal.pone.0094821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Koenig HG, Westlund RE, George LK, Hughes DC, Blazer DG, Hybels C. Abbreviating the Duke Social Support Index for use in chronically ill elderly individuals. Psychosomatics. 1993;34(1):61–69. doi: 10.1016/S0033-3182(93)71928-3. [DOI] [PubMed] [Google Scholar]
- 71.Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46(2):153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 72.Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry. 2000;31(2):73–86. doi: 10.1016/s0005-7916(00)00012-4. [DOI] [PubMed] [Google Scholar]
- 73.Innes KE, Selfe TK, Alexander GK, Taylor AG. A new educational film control for use in studies of active mind-body therapies: acceptability and feasibility. J Altern Complement Med. 2011;17(5):453–458. doi: 10.1089/acm.2010.0401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.van Ginkel JR, Kroonenberg PM. Analysis of variance of multiply imputed data. Multivariate Behav Res. 2014;49(1):78–91. doi: 10.1080/00273171.2013.855890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Innes K, Selfe T, Leeming K, et al. P02.156. Effects of a gentle yoga program on Restless Legs Syndrome (RLS) symptoms and related outcomes in women with RLS: a pilot study. BMC Complement Altern Med. 2012;12:P212. [Google Scholar]
- 76.Shahgholian N, Jazi SK, Karimian J, Valiani M. The effects of two methods of reflexology and stretching exercises on the severity of restless leg syndrome among hemodialysis patients. Iran J Nurs Midwifery Res. 2016;21(3):219–224. doi: 10.4103/1735-9066.180381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Giannaki CD, Sakkas GK, Karatzaferi C, et al. Effect of exercise training and dopamine agonists in patients with uremic restless legs syndrome: a six-month randomized, partially double-blind, placebo-controlled comparative study. BMC Nephrol. 2013;14(1):194. doi: 10.1186/1471-2369-14-194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Aliasgharpour M, Abbasi Z, Pedram Razi S, Kazemnezhad A. The effect of stretching exercises on severity of restless legs syndrome in patients on hemodialysis. Asian J Sports Med. 2016;7(2):e31001. doi: 10.5812/asjsm.31001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Mortazavi M, Vahdatpour B, Ghasempour A, et al. Aerobic exercise improves signs of restless leg syndrome in end stage renal disease patients suffering chronic hemodialysis. ScientificWorldJournal. 2013;2013:628142. doi: 10.1155/2013/628142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sakkas GK, Hadjigeorgiou GM, Karatzaferi C, et al. Intradialytic aerobic exercise training ameliorates symptoms of restless legs syndrome and improves functional capacity in patients on hemodialysis: a pilot study. ASAIO J. 2008;54(2):185–190. doi: 10.1097/MAT.0b013e3181641b07. [DOI] [PubMed] [Google Scholar]
- 81.Harrison EG, Keating JL, Morgan P. Novel exercises for restless legs syndrome: a randomized, controlled trial. J Am Board Fam Med. 2018;31(5):783–794. doi: 10.3122/jabfm.2018.05.180065. [DOI] [PubMed] [Google Scholar]
- 82.Innes KE, Vincent HK, Taylor AG. Chronic stress and insulin resistance-related indices of cardiovascular disease risk, part I: neurophysiological responses and pathological sequelae. Altern Ther Health Med. 2007;13(4):46–52. [PubMed] [Google Scholar]
- 83.Cohen DL, Wintering N, Tolles V, et al. Cerebral blood flow effects of yoga training: preliminary evaluation of 4 cases. J Altern Complement Med. 2009;15(1):9–14. doi: 10.1089/acm.2008.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Streeter CC, Jensen JE, Perlmutter RM, et al. Yoga Asana sessions increase brain GABA levels: a pilot study. J Altern Complement Med. 2007;13(4):419–426. doi: 10.1089/acm.2007.6338. [DOI] [PubMed] [Google Scholar]
- 85.Brown RP, Gerbarg PL. Sudarshan Kriya yogic breathing in the treatment of stress, anxiety, and depression: part I-neurophysiologic model. J Altern Complement Med. 2005;11(1):189–201. doi: 10.1089/acm.2005.11.189. [DOI] [PubMed] [Google Scholar]
- 86.Streeter C, Whitfield T, Owen L, et al. Effects of yoga versus walking on mood, anxiety, and brain GABA levels: a randomized controlled MRS study. J Altern Complement Med. 2010;16(11):1145–1152. doi: 10.1089/acm.2010.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Scalise A, Pittaro-Cadore I, Janes F, Marinig R, Gigli GL. Changes of cortical excitability after dopaminergic treatment in restless legs syndrome. Sleep Med. 2010;11(1):75–81. doi: 10.1016/j.sleep.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 88.Hornyak M, Scholz H, Kohnen R, Bengel J, Kassubek J, Trenkwalder C. What treatment works best for restless legs syndrome? Meta-analyses of dopaminergic and non-dopaminergic medications. Sleep Med Rev. 2014;18(2):153–164. doi: 10.1016/j.smrv.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 89.Fulda S, Wetter TC. Where dopamine meets opioids: a meta-analysis of the placebo effect in restless legs syndrome treatment studies. Brain. 2008;131(Pt 4):902–917. doi: 10.1093/brain/awm244. [DOI] [PubMed] [Google Scholar]