Abstract
Study Objectives:
The modified Mallampati (MM) grade and Friedman tongue position (FTP) are commonly used scales that assess the oropharynx during evaluation for obstructive sleep apnea (OSA). Though used by many practitioners, there is controversy in the literature regarding their practical utility. The goal of this review will be to review the history of how the MM and FTP were developed, to discuss current evidence for their usefulness in the workup of OSA, and to provide future direction to better understand their utility in the workup of OSA.
Methods:
We searched the literature (PubMed) for the terms “modified Mallampati” and “Friedman tongue position.” Articles were selected based on our study objectives emphasizing articles discussing the utility of MM and FTP in managing OSA.
Conclusions:
MM and FTP have the potential to be useful assessment tools in the evaluation of OSA. When performing this examination, it is important for physicians and other medical providers to understand the pitfalls of the MM and FTP including the potential difficulty in performing the exam and the lack of consistency between examiners in both the terminology and execution of this physical exam finding. Better methods to standardize the assessment are necessary to ensure consistent evaluation among individual examiners while at the same time keeping the method simple and convenient for wide use as a clinical screening tool.
Citation:
Yu JL, Rosen I. Utility of the modified Mallampati grade and Friedman tongue position in the assessment of obstructive sleep apnea. J Clin Sleep Med. 2020;16(2):303–308.
Keywords: modified Mallampati, Friedman tongue position, obstructive sleep apnea, OSA
INTRODUCTION
Obstructive sleep apnea (OSA) is a major health epidemic in the United States with an estimated 22 million people having the disorder.1 Diagnosis is confirmed by polysomnography in the laboratory, or more commonly by using a portable home sleep apnea testing (HSAT) device.2,3 However, in-laboratory polysomnography is expensive to perform and often considered burdensome by patients. HSAT is a more convenient and inexpensive alternative for the evaluation of OSA, but ultimately, evaluation and testing, even with HSAT, is still a limited resource. Ultimately, physicians and other medical providers rely on a variety of clinical history and physical examination findings to determine whether to obtain these tests.
Examination of the oral cavity and oropharyngeal crowding is one such physical examination finding that is commonly evaluated in determining risk for OSA. The modified Mallampati (MM) grade and Friedman tongue position (FTP) are commonly used to describe how crowded the pharynx is during assessment for OSA. However, despite its widespread use as part of the physical examination during initial sleep disorder evaluations, there is debate as to whether this examination finding is useful in helping determine the risk for OSA and whether the findings change management. The goal of this review will be to review the history of how the MM and FTP were developed, to discuss current evidence for its usefulness in the workup of OSA, and to provide future direction to better understand its utility in the workup of OSA.
Modified Mallampati grade
The Mallampati grade was first developed by Seshagiri Mallamapati in 1985.4 He was an anesthesiologist who sought to predict the risk of difficult intubation based on mouth opening. In a time period without modern-day fiberoptic laryngoscopes, the ability to predict difficult intubations was of significant importance in anesthesia as failure to do so could lead to life- threatening airway emergencies. To perform the examination, patients were asked to sit with their head in neutral position and to open their mouths fully while sticking out their tongues maximally. Using a simple three-grade classification based on whether Mallampati could visualize the tonsillar pillars, uvula, and soft palate, he showed correlation between Mallampati grade and view of the airway on direct laryngoscopy.
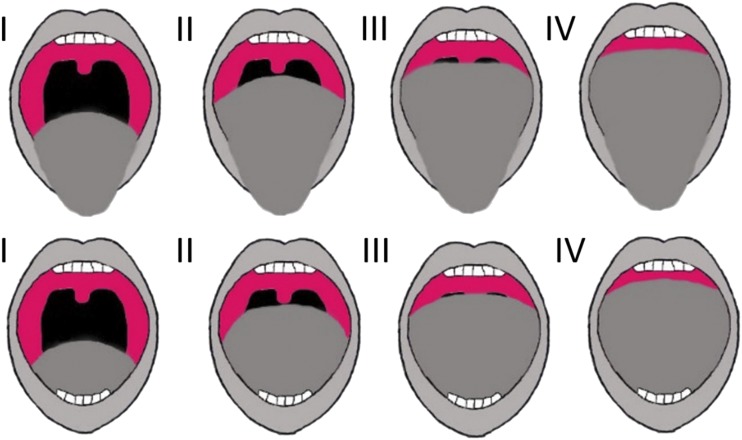
Samsoon and Young5 reported a modification of the Mallampati grade when they retrospectively reviewed a cohort of difficult intubations at their institution. They noted that in some patients even the soft palate was difficult to visualize and they added an additional classification, grade 4, where only the hard palate was able to be visualized.5 This was the first modification to the original Mallampati grade (Figure 1).
Figure 1. Diagram of modified Mallampai (upper row) and Friedman tongue position (lower row) grades.
Friedman tongue position
Friedman et al6 performed a prospective study of 172 patients who were being evaluated for OSA. He performed a further modified version of the Mallampati examination where he asked the patient sit upright with their head in neutral position and had them open their mouth without sticking their tongue out (Figure 1). He initially called this a “modified Mallampati” grade but later changed the term to “Friedman tongue position.” He found a statistically significant correlation between his FTP grade and the apnea-hypopnea index (AHI) severity (r = .340, P < 001).6
Confusion of nomenclature
It is worth noting that there is confusion within the literature regarding the descriptions of MM and FTP. MM was originally coined by Samsoon and Young when they described the addition of grade 4 to the original scale that Mallampati developed in assessing for difficult intubation risk.5 This technique, as previously mentioned, includes having patients stick their tongues out maximally. However, in his initial description of his methods for assessing OSA risk, Friedman also used the term “modified Mallampati” to describe a physical examination where the patient’s mouth is open but the tongue is left in the oral cavity.6 On subsequent publications, Friedman had changed the name of his method to “Friedman palate position,” then to “Friedman tongue position” to further emphasize that it was the tongue that played an important role in assessing OSA risk.7 It is unclear whether this was also done to partially clarify the confusion between his method and the MM that Samsoon and Young already described. Regardless, MM is still being used to describe both examinations with the tongue either protruded or in neutral position in the mouth. The literature continues to mix the use of the terms, and it is important for one who is reviewing the literature to check the methods described in order to know which technique was used, specifically whether the tongue is kept in or out of the mouth during the examination. For the purposes of this review, we will continue describing MM as an examination with the tongue protruded and the FTP as an examination with the tongue in neutral position within the mouth regardless of what each primary source called it.
USE OF MM/FTP IN ASSESSING OSA RISK
The first use of MM in the assessment of OSA was performed by Hiremath et al.8 Comparing 15 patients with documented difficult intubations to 15 healthy control patients, they found a statistically significant difference in the incidence of OSA among the patients who were difficult to intubate. The authors concluded that OSA was a risk factor for difficult intubation. When comparing physical examination findings, higher MM grades were associated with both increased risk of difficult intubation and OSA.
Since that time, several studies have shown an association between both MM and FTP to OSA risk. Nuckton et al9 assessed 137 patients with suspected OSA and performed multivariate analysis to evaluate for independent risk factors for OSA. They found MM grade to be an independent risk factor for OSA with an odds ratio of 2.5 for every 1 point increase in MM.9 Dahlqvist et al10 showed that MM grade 3 or above was an independent risk factor for an AHI > 15 events/h, which was statistically significant in men (odds ratio [OR] 1.7, 95% confidence interval [95% CI] 1.07–2.69) but not significant in women (OR 2.09, 95% CI 0.79–5.46).10 Ramachandran et al11 used numerous independently associated risk factors to develop an OSA risk scoring system for which MM grade 3 and above was noted to be a statistically significant risk factor (β coefficient = .367, P < .001).11 Friedman et al7 performed a meta-analysis of 8 separate studies with a total of 1,358 patients looking at both MM and FTP in assessing AHI and OSA. The results of the meta-analysis found statistically significant correlations between AHI severity and both MM (.184, P = .006) and FTP (.388, P = .026). Schwab et al12 compared digital morphometrics along with conventional physical examination findings including FTP in 542 patients with a diagnosis of OSA. They found that higher FTP grades were associated with both increased risk for OSA as well as AHI severity.12
MM or FTP can also be incorporated into scoring systems to better screen for OSA risk. Avincsal et al reported on a scoring system that included both MM and the STOP-BANG questionnaire, a validated screening questionnaire with a high sensitivity but low specificity.13,14 In their scoring system a MM grade of 3 or greater was assigned a value of 1, which was added to the STOP-BANG score. They found that MM grades of 3 and 4 in combination with the STOP-BANG score increased the specificity of detecting an AHI > 15 events/h from 10.6% to 26%.13 Lin et al15 used FTP and several other parameters to develop a linear regression model that output an OSA score. With this model, they determined at an OSA score of 6.25 had a sensitivity of 84% and specificity of 58% in predicting OSA with an AHI > 5 events/h.15
The limited utility of MM/FTP
Although several sources in the literature suggest an association between MM/FTP and OSA risk, there is still debate about its practical applicability. Bins et al16 performed a systematic review of eight studies that reported on MM and OSA. They showed that when patients were stratified based on MM grading, those with grades 1–2 had a 1% to 13% decrease in the probability of having OSA, whereas grades 3–4 had a zero to 11% increase in the probability of having OSA.16 These were not considered statistically significant. The authors concluded that MM provides no practical value in predicting OSA and likely would not change management.
Returning to Friedman’s initial study and subsequent meta-analysis of FTP in predicting OSA severity, he notes a statistically significant correlation between FTP and AHI.6,7,17 The average correlation coefficient from the studies was .388 (P = .026), which is not a strong correlation. In fact, Friedman notes that with linear regression modeling, FTP only contributed to 12% of the variance in AHI seen in OSA. Although this was statistically significant, P = .026, it does call into question its utility in a clinical setting given such a small contribution to the effects on predicting OSA and AHI severity.
Although the use of MM/FTP may have limited utility in predicting the severity of OSA, it may be useful in ruling out OSA. Screening to rule out OSA with MM/FTP values of 1 or 2 could be beneficial in the clinical setting. Hukins18 performed a retrospective study looking at 953 patients being evaluated for OSA by PSG and analyzed the ability of MM to both predict severe OSA with high grades and to rule out OSA with low grades.18 Like Friedman, Hukins found a statistically significant but weak correlation between MM and AHI (r = .13, P < .001) that in their study translated into MM only explaining 1.7% of the variability in AHI. When they looked at using MM grade 1 to rule out OSA as defined by them as an AHI < 5 events/h, they had a sensitivity of 13% and a specificity of 92%. The investigators converted the sensitivity and specificity to likelihood ratios, a validated metric for assessing diagnostic accuracy.19 A MM grade 1 has a positive likelihood ratio of 1.63 for predicting an AHI < 5 events/h. A likelihood ratio between 1 and 2 is considered to have a negligible effect (< 15%) in modifying the pretest probability of the outcome of interest and their conclusion was that MM grade 1 was not clinical useful in ruling out OSA.
The prevalence of the disease and pretest probability of the likelihood of having OSA is also important when determining the utility of screening tools. Hukins18 comment that their study population was selected from a sleep clinic where patients were already referred for concern of OSA. Therefore, there is likely a higher prevalence and a higher pretest probability of having OSA among these patients compared to the general population. As prevalence increases, the negative predictive value of a test decreases and so use of a MM grade 1 to rule out OSA may generate a high false-negative rate. This does not mean that use of the MM/FTP as a screening tool would be less useful in the general population, but further studies are needed to make this determination.
The interexaminer reliability of MM/FTP
It is interesting to note that in the meta-analysis performed by Friedman et al, one study had an R coefficient of .88, which suggests a very strong correlation that was larger than any of the other seven studies.7 This study compared multiple physical examination findings and AHI severity among 300 patients.20 The average age, body mass index, and AHI were not significantly different from the other studies included in the meta-analysis. One possible explanation for the strong correlation is that in this study, the FTP was evaluated by a single otolaryngologist. Referring back to Nuckton et al, 9 this study also relied on a single physician to perform the physical examination when determining that MM was an independent risk factor for OSA. These studies relied on a single examiner for their grading schemes and a critique of both MM and FTP is that there is poor interexaminer agreement that can affect their predictive value.
Physical examination findings can be subjective in nature and the assessment of visualization of various landmarks may be difficult to standardize, which gives rise to poor interexaminer reliability and agreement. There continues to be debate regarding the interobserver reliability of these tests in both the anesthesia literature and in the sleep apnea literature. Only a handful of studies have looked into the interexaminer reliability of MM and FTP.
Within the anesthesia literature, Karkouti et al21 compared 10 screening tools for assessment of difficult intubation, including MM. In this prospective study of 59 patients undergoing elective surgery, they found that for MM the interrater reliability kappa coefficient (κ) was .31, which is considered poorly correlated.21 When discussing the poor correlation, the investigators noted that the original instructions for MM staging were somewhat vague and “prone to classification errors.”21 Rosenstock et al22 performed a prospective study of 120 patients undergoing elective study comparing 6 tools for assessment of difficult intubation including Mallampati grading and had an interrater reliability (κ) of .8 among experienced anesthesiologists.22 However, the grading system used consisted of only grades 1-3 as originally described by Mallampati. In their discussion, the investigators elaborated their decision not to include the Samsoon and Young modification because they found that this grading system was prone to significant variation in interrater reliability.
In the OSA literature, Friedman et al23 performed a study to assess the interexaminer reliability of the FTP classification in evaluating for OSA. They showed a κ coefficient of .82, suggesting strong agreement among raters with his staging method.23 However, several aspects of the study were idealized. In this study, 126 otolaryngologists were asked to examine several video recordings of oral cavity examinations. By design, videos were optimized examples of patient oral cavities; those with poor quality examinations were excluded. Examiners were also allowed to view the videos as many times as they needed before making their decision.
Sundman et al24 addressed this concern by having FTP examinations performed on actual volunteers. A total of 15 otolaryngologists volunteered to perform FTP examinations among each other and the interrater reliability κ coefficient was .36. A follow-up study where 14 otolaryngologists were asked to evaluate 12 patients with a known diagnosis of OSA produced a similar κ coefficient of .32.25 They concluded that FTP findings varied widely among examiners, making it an unreliable physical examination finding.
Challenges when performing MM/FTP examinations
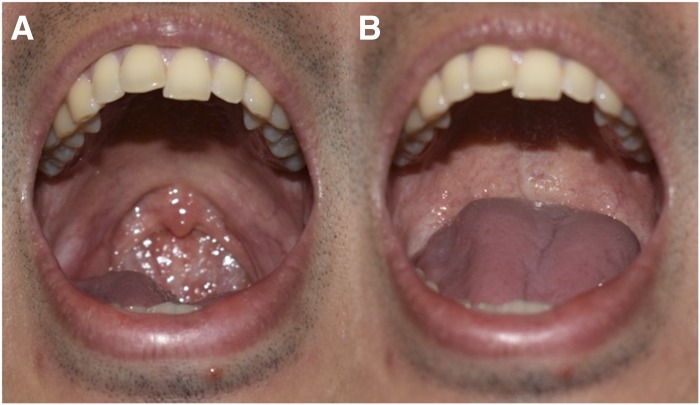
Changes are needed to improve reliability in the use of MM and FTP among physicians and other medical providers. One major issue is that the initial descriptions of the examinations are actually quite vague when it relates to the dynamic changes that may occur due to a patients breathing. In Mallampati and Friedman’s respective original studies, there is no instruction on the patient’s breathing pattern.4,6 This is important as the position of the soft palate will vary depending on whether a patient is breathing through his mouth or nose. When breathing through the nose with the mouth open, the soft palate descends to occlude the oral cavity to allow the nasal passages to be the path of least resistance into the airway.26 With this in mind, if the examination is performed with the patient breathing from the mouth, the soft palate would elevate to close off the nasopharynx and give the appearance of a MM/FTP grade 1 or 2. If asked to breathe nasally, the soft palate will descend against the base of tongue and that very same patient may become a MM/FTP grade 3 or 4 (Figure 2). Friedman et al27 attempted to address the issue with an update of how to perform the FTP with the following instruction27:
“To evaluate FTP, the clinician should ask the patient to open his/her mouth widely, a minimum of 5 times. This allows the observer to assign the most consistent position of the tongue. The patient should also be instructed to breathe normally while leaving the tongue in its natural position.”
It is apparent that an individual’s oral cavity examination may vary requiring at least the average of 5 separate evaluations prior to confirming the grade. Even in Mallampati’s original description of this examination, patients performed the examination a minimum of two times in order to decrease inconsistency.4 Such instructions render both the MM and FTP assessments impractical as medical providers are unlikely to reattempt oral cavity examinations several times in the clinical setting. Moreover, the term “breathe normally” is vague and does not address the concern of palatal positioning based on either nasal or mouth breathing. Physicians and other medical providers should be aware of the challenges in terms of the definition of proper technique when they are performing their examination. In this reviewer’s experience, given the variation of soft palate and tongue position, patients should be instructed to slowly breathe through the mouth as this provides a clear and easily understandable instruction to allow consistency to the examination and will not cause artificial lowering of the soft palate in nasal breathing nor artificial elevation of the palate that can occur with heavy breathing. However, further clarification and standardization of the examination methods is required in order to allow for accurate reporting of findings and improve the predictive value of either the MM or the FTP.
Figure 2. Soft palate and tongue position.
During oral breathing (A), the soft palate is elevated to close off the oropharynx from the nasopharynx giving a Friedman tongue position grade 1 appearance. During nasal breathing (B), the soft palate lowers and there is elevation of the base of tongue which can give the appearance of Friedman tongue position grade 3 in the same patient.
FUTURE DIRECTIONS
Improvements to standardize the MM and FTP evaluations can include strategies such as using standardized equipment to position and open a patient’s mouth for evaluation, taking multiple photographs to control for the dynamic variability of pharyngeal movement, or use of machine learning algorithms to improve accuracy of grading. As noted earlier, Schwab et al12 performed FTP examinations along with other oropharyngeal measurements by using a digital camera and a laser ruler to obtain precise objective measurements of the oropharyngeal airway. One appeal of using MM/FTP during the clinical evaluation is that these assessments are relatively quick and easy examinations that require only a penlight to perform. Addition of other equipment or complicated instructions may affect a clinician’s workflow in the office, thereby making the examination more difficult to perform which may, in turn, influence its utility in the clinical setting.
It is important for medical providers to recognize as OSA a complex disorder that is a culmination of multiple physiologic factors and cannot be fully described by a single physical examination finding. Studies looking into how demographics and other medical comorbidities influence the predictive value of MM/FTP have been limited. Only one study in our search in the literature compared MM/FTP among different demographics. As previously noted, Dahlqvist et al10 showed that higher MM grades were associated with increased odds of having OSA among men but not among women. This suggests the value of MM/FTP may differ based on sex. Further studies looking at differences in MM/FTP when compared to age, race, or other demographic factors are needed to better to determine if MM/FTP may be a more or less valuable examination finding under specific circumstances.
The definition of OSA itself has also evolved over time and will likely continue to evolve into the future. Obstructive apneas were defined as a total cessation of airflow of greater than 10 seconds in all referenced studies. However, the definitions for obstructive hypopneas varied among the studies. Whether different definitions of obstructive hypopneas could influence the diagnostic utility of MM/FTP is beyond the scope of this review, but as our understanding of OSA continues to develop, and our definitions for the diagnosis of OSA continue to evolve, we may find that the predictive value of MM/FTP may also change.
CONCLUSIONS
Given the body of literature, it may seem that both the MM and FTP are difficult subjective assessments with little significance correlating the risk of OSA. However, there is also evidence that MM and FTP can be useful tools in assessment of risk for OSA and potentially severity. Although it may have limited predictive value as an independent risk factor, it may still play a role when incorporated into the overall clinical picture of an individual patient and still has the potential to play a role in screening for OSA. When performing this examination, it is important for physicians and other medical providers to understand the limitations of the MM and FTP including the potential difficulty in performing the examination and the lack of consistency between examiners in both the terminology and execution of this physical examination finding. Better methods to standardize the assessment are necessary to ensure consistent evaluation among individual examiners while at the same time keeping the method simple and convenient for wide use as a clinical screening tool. Further study of MM/FTP among subgroups of the OSA population, particularly among those patients with different demographic characteristics, may also help us better determine when MM/FTP may be more or less important. Ultimately, a better understanding of the MM and FTP, their strengths and weaknesses in evaluating OSA, and the future potential to improve these examinations will serve to better inform physicians and other medical providers in their medical decision making.
DISCLOSURE STATEMENT
All authors have reviewed and approved this manuscript. Work for this study was performed at the Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA. The authors report no conflicts of interest.
ABBREVIATIONS
- AHI
apnea-hypopnea index
- FTP
Friedman tongue position
- MM
modified Mallampati
- OSA
obstructive sleep apnea
REFERENCES
- 1.Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006–1014. doi: 10.1093/aje/kws342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iber C, Ancoli-Israel S, Chesson AL, Jr, Quan SF. for the American Academy of Sleep Medicine . The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. 1st ed. Westchester, IL: American Academy of Sleep Medicine; 2007; [Google Scholar]
- 3.Kapur VK, Auckley DH, Chowdhuri S, et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13(3):479–504. doi: 10.5664/jcsm.6506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mallampati SR, Gatt SP, Gugino LD, et al. A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaesth Soc J. 1985;32(4):429–434. doi: 10.1007/BF03011357. [DOI] [PubMed] [Google Scholar]
- 5.Samsoon GL, Young JR. Difficult tracheal intubation: a retrospective study. Anaesthesia. 1987;42(5):487–490. doi: 10.1111/j.1365-2044.1987.tb04039.x. [DOI] [PubMed] [Google Scholar]
- 6.Friedman M, Tanyeri H, La Rosa M, et al. Clinical predictors of obstructive sleep apnea. Laryngoscope. 1999;109(12):1901–1907. doi: 10.1097/00005537-199912000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Friedman M, Hamilton C, Samuelson CG, Lundgren ME, Pott T. Diagnostic value of the Friedman tongue position and Mallampati classification for obstructive sleep apnea: a meta-analysis. Otolaryngol Head Neck Surg. 2013;148(4):540–547. doi: 10.1177/0194599812473413. [DOI] [PubMed] [Google Scholar]
- 8.Hiremath AS, Hillman DR, James AL, Noffsinger WJ, Platt PR, Singer SL. Relationship between difficult tracheal intubation and obstructive sleep apnoea. Br J Anaesth. 1998;80(5):606–611. doi: 10.1093/bja/80.5.606. [DOI] [PubMed] [Google Scholar]
- 9.Nuckton TJ, Glidden DV, Browner WS, Claman DM. Physical examination: Mallampati score as an independent predictor of obstructive sleep apnea. Sleep. 2006;29(7):903–908. doi: 10.1093/sleep/29.7.903. [DOI] [PubMed] [Google Scholar]
- 10.Dahlqvist J, Dahlqvist A, Marklund M, Berggren D, Stenlund H, Franklin KA. Physical findings in the upper airways related to obstructive sleep apnea in men and women. Acta Otolaryngol. 2007;127(6):623–630. doi: 10.1080/00016480600987842. [DOI] [PubMed] [Google Scholar]
- 11.Ramachandran SK, Kheterpal S, Consens F, et al. Derivation and validation of a simple perioperative sleep apnea prediction score. Anesth Analg. 2010;110(4):1007–1015. doi: 10.1213/ANE.0b013e3181d489b0. [DOI] [PubMed] [Google Scholar]
- 12.Schwab RJ, Leinwand SE, Bearn CB, et al. Digital morphometrics: a new upper airway phenotyping paradigm in OSA. Chest. 2017;152(2):330–342. doi: 10.1016/j.chest.2017.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Avincsal MO, Dinc ME, Ulusoy S, Dalgic A, Ozdemir C, Develioglu ON. Modified Mallampati score improves specificity of STOP-BANG questionnaire for obstructive sleep apnea. J Craniofac Surg. 2017;28(4):904–908. doi: 10.1097/SCS.0000000000003513. [DOI] [PubMed] [Google Scholar]
- 14.Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108(5):812–821. doi: 10.1097/ALN.0b013e31816d83e4. [DOI] [PubMed] [Google Scholar]
- 15.Lin HC, Lai CC, Lin PW, et al. Clinical prediction model for obstructive sleep apnea among adult patients with habitual snoring. Otolaryngol Head Neck Surg. 2019;161(1):178–185. doi: 10.1177/0194599819839999. [DOI] [PubMed] [Google Scholar]
- 16.Bins S, Koster TD, de Heij AH, et al. No evidence for diagnostic value of Mallampati score in patients suspected of having obstructive sleep apnea syndrome. Otolaryngol Head Neck Surg. 2011;145(2):199–203. doi: 10.1177/0194599811409302. [DOI] [PubMed] [Google Scholar]
- 17.Friedman M, Ibrahim H, Joseph NJ. Staging of obstructive sleep apnea/hypopnea syndrome: a guide to appropriate treatment. Laryngoscope. 2004;114(3):454–459. doi: 10.1097/00005537-200403000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Hukins C. Mallampati class is not useful in the clinical assessment of sleep clinic patients. J Clin Sleep Med. 2010;6(6):545–549. [PMC free article] [PubMed] [Google Scholar]
- 19.McGee S. Simplifying likelihood ratios. J Gen Intern Med. 2002;17(8):647–649. doi: 10.1046/j.1525-1497.2002.10750.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barceló X, Mirapeix RM, Buges J, Cobos A, Domingo C. Oropharyngeal examination to predict sleep apnea severity. Arch Otolaryngol Head Neck Surg. 2011;137(10):990–996. doi: 10.1001/archoto.2011.176. [DOI] [PubMed] [Google Scholar]
- 21.Karkouti K, Rose DK, Ferris LE, Wigglesworth DF, Meisami-Fard T, Lee H. Inter-observer reliability of ten tests used for predicting difficult tracheal intubation. Can J Anaesth. 1996;43(6):554–559. doi: 10.1007/BF03011765. [DOI] [PubMed] [Google Scholar]
- 22.Rosenstock C, Gillesberg I, Gatke MR, Levin D, Kristensen MS, Rasmussen LS. Inter-observer agreement of tests used for prediction of difficult laryngoscopy/tracheal intubation. Acta Anaesthesiol Scand. 2005;49(8):1057–1062. doi: 10.1111/j.1399-6576.2005.00792.x. [DOI] [PubMed] [Google Scholar]
- 23.Friedman M, Soans R, Gurpinar B, Lin HC, Joseph NJ. Interexaminer agreement of Friedman tongue positions for staging of obstructive sleep apnea/hypopnea syndrome. Otolaryngol Head Neck Surg. 2008;139(3):372–377. doi: 10.1016/j.otohns.2008.06.017. [DOI] [PubMed] [Google Scholar]
- 24.Sundman J, Bring J, Friberg D. Poor interexaminer agreement on Friedman tongue position. Acta Otolaryngol. 2017;137(5):554–556. doi: 10.1080/00016489.2016.1255776. [DOI] [PubMed] [Google Scholar]
- 25.Sundman J, Fehrm J, Friberg D. Low inter-examiner agreement of the Friedman staging system indicating limited value in patient selection. Eur Arch Otorhinolaryngol. 2018;275(6):1541–1545. doi: 10.1007/s00405-018-4970-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rodenstein DO, Stanescu DC. Soft palate and oronasal breathing in humans. J Appl Physiol. 1984;57(3):651–657. doi: 10.1152/jappl.1984.57.3.651. [DOI] [PubMed] [Google Scholar]
- 27.Friedman M, Salapatas AM, Bonzelaar LB. Updated Friedman staging system for obstructive sleep apnea. Adv Otorhinolaryngol. 2017;80:41–48. doi: 10.1159/000470859. [DOI] [PubMed] [Google Scholar]