Abstract
BACKGROUND AND OBJECTIVES:
Maternal drinking is associated with child emotional and behavior problems. There is, however, a lack of studies that properly account for confounding. Our objective was to estimate the association between at-risk drinking in mothers of young children and child emotional and behavior problems, taking into account the passive transmission of familial risk.
METHODS:
This population-based sample consists of 34 039 children nested within 21 911 nuclear families and 18 158 extended families from the Norwegian Mother, Father, and Child Cohort Study. Participants were recruited between 1999 and 2009 during routine ultrasound examinations. Data were collected during the 17th and 30th gestational week and when the children were 1.5, 3, and 5 years old. We applied a multilevel structural equation model that accounted for unobserved familial risks.
RESULTS:
Children of mothers with at-risk drinking had a higher likelihood of behavior problems (β = 3.53; 95% confidence interval [CI] 3.01 to 4.05) than children of mothers with low alcohol consumption. This association was reduced after adjusting for factors in the extended family (β = 1.93; 95% CI 1.16 to 2.71) and the nuclear family (β = 1.20; 95% CI 0.39 to 2.01). Maternal at-risk drinking had a smaller association with child emotional problems (β = 1.80; 95% CI 1.26 to 2.34). This association was reduced after adjusting for factors in the extended family (β = 0.67; 95% CI −0.12 to 1.46) and the nuclear family (β = 0.58; 95% CI −0.31 to 1.48).
CONCLUSIONS:
The results suggest an association between maternal at-risk drinking and child behavior problems. A reduction in maternal drinking may improve outcomes for children with such symptoms.
What’s Known on This Subject:
Although maternal drinking has been associated with child emotional and behavior problems, several factors may contribute to these outcomes, making it challenging to disentangle the true association of maternal drinking with child emotional and behavior problems.
What This Study Adds:
In this study, we estimate the association between at-risk drinking in mothers of young children and child emotional and behavior problems, taking into account the passive transmission of familial risk.
Maternal drinking is associated with several adverse child outcomes, including emotional and behavior problems, such as anxiety, depression, inattentiveness, and aggressive behavior.1–9 Several factors may contribute to child emotional and behavior problems, making it challenging to disentangle the true effect of maternal drinking. A better understanding of this association is needed. Here, we estimate the effect of maternal drinking on children’s emotional and behavior problems, taking into account both environmental and genetic risks.
Several plausible mechanisms may explain the association between maternal drinking and child emotional and behavior problems.10–12 A possible mechanism is that maternal drinking places children at increased risk of behavior problems because their mothers pass on genetic vulnerability to a range of behavior problems13 that are genetically linked to drinking.14 Thus, behavior problems may be an expression of familial vulnerability, not necessarily maternal drinking in itself.15,16 Some studies find that parental drinking also increases the risk of child emotional problems17; other studies do not.8 A recent study showed that although maternal drinking was initially associated with both emotional and behavior problems in toddlers, the associations disappeared after other variables were taken into account, suggesting that other maternal variables may be more important.18 Although the link between parental drinking and child emotional problems may not be as strong as that for alcohol consumption and behavior problems, alcohol problems are more prevalent among persons with emotional problems,19,20 and shared genetic risk between alcohol use and emotional problems21–23 suggests that maternal drinking also places children at risk for emotional problems.
Another plausible mechanism is that maternal drinking constitutes an environmental risk through compromising the mother’s ability to be supportive when interacting with her child.24,25 Although genetic risk influences the transmission of emotional problems, much of the variance remains unexplained,26 suggesting that environmental risks are more important risk factors for child emotional problems (eg, maternal drinking may compromise the mother’s connection with her child).27
To better understand the association between alcohol consumption among mothers of young children and associated child emotional and behavior problems, methodologically robust studies that take into account both environmental and genetic risks and can control for several types of potential biases are necessary. In a recent study, we found that maternal drinking during pregnancy was initially associated with behavior and emotional problems; but most associations were strongly reduced after controlling for transmission of familial risk factors.28 In the current study, we estimate the effect of maternal drinking when the children are 1.5, 3, and 5 years old on children’s emotional and behavior problems, taking into account both environmental and genetic risks. Confounding by familial risk can be estimated by comparing cousins, children of sisters whose alcohol use differs, or siblings who are discordant on exposure to maternal alcohol use. We combine these 2 family-study approaches (ie, extended family and nuclear family) in 1 model to estimate confounding. We estimate the associations of maternal drinking on child emotional and behavior problems while accounting for passive transmission of familial risk. Much of the literature focuses on how parental alcohol use disorder (AUD) or heavy drinking13,17,18,29 affects the risk of child emotional and behavior problems; how more normative types of maternal drinking are associated with such problems remains understudied and is the focus in the current study. There are more mothers with at-risk drinking than there are mothers with AUDs. If at-risk maternal drinking is also associated with increased risk for child emotional and behavior problems, then the number of children at risk is probably higher than previously assumed.
If the association between maternal drinking and child emotional and behavior outcomes remains after adequately accounting for confounding, this suggests that policies and interventions aimed at reducing parental drinking would be useful in reducing the risk of these child problems. If the associations are confounded, and maternal drinking is just a risk indicator, then such interventions or policies are less likely to be effective. This is important because strategies implemented on the basis of the currently limited knowledge base may be misguided and waste resources that would have had a better impact if applied elsewhere.30
Methods
Study Design, Participants, and Procedures
We use data from the Norwegian Mother, Father, and Child Cohort Study (MoBa). This prospective study has been described in detail elsewhere.31 Participants were recruited between 1999 and 2009 while attending routine ultrasound examinations offered to all pregnant women in Norway during gestational weeks 17 to 18. Of those eligible, 41% chose to participate in the study. The total MoBa sample includes >114 000 children, 95 000 mothers, and 75 000 fathers. The study sample for the current study comprised 34 039 children nested within 21 911 nuclear families (ie, children of the same mother) and 18 158 cousins sharing a maternal grandmother. We used data collected when the children were 1.5, 3, and 5 years old. To acquire information about children when they were the same age, questionnaires were sent according to the children’s birthdays. The study also includes information from the Norwegian Medical Birth Registry.32
Study participants provided written informed consent. The Norwegian Data Inspectorate granted the MoBa a license, and the Regional Committees for Medical and Health Research Ethics approved the current study.
Measures: Exposure to Maternal Drinking
Women self-reported how much alcohol they typically consumed on a weekday or weekend drinking occasion (ie, “How many alcohol units do you usually drink when you consume alcohol?”). We constructed an ordinal variable where 1 represented at-risk drinking. On this scale, the reported typical unit of alcohol consumption was coded as follows: “1 to 2” = 0, “3 to 4” = 0.5, “5 to 6” = 1, “7 to 9” = 2, and “>10” = 3 for weekends and “1 to 2” = 0, “3 to 4” = 1, “5 to 6” = 2, and “7 to 9” = 3 for weekdays. We used the average of weekends and weekdays. Abstaining (ie, <1 unit) was coded as missing, because it is a form of censored data; this is the recommended approach when you have auxiliary information in the data, other time points, or relatives.33 Our effect sizes therefore represent the increase in outcomes when going from 1 to 2 units (ie, 0) on a typical occasion to drinking both 3 or more units of alcohol on a typical occasion during weekdays and 5 or more units on weekends.1 For descriptive purposes, we have also included information about how often women reported that they consumed alcohol. In the MoBa, 1 unit of alcohol constitutes 1.5 cL (12.8 g) of pure alcohol.18 The women responded to these questions when the child was 1.5, 3, and 5 years old.
Outcomes: Child Emotional and Behavior Problems
We used items from the Child Behavior Checklist (CBCL) for preschool children (1.5–5 years old) to assess child behavior and emotional problems when the children were 1.5, 3, and 5 years old.34 The instrument consists of 99 items that describe how the child has behaved over the past 2 months. Mothers responded to these items using a scale ranging from “not true” (1) to “somewhat or sometimes true” (2), and “very true” or “often true” (3). The CBCL consists of subscales within emotional and behavior problems (Table 1). Item selection was necessary because of space restrictions in the MoBa questionnaires; choice of items was based on consensus among specialists in clinical and developmental psychology. Numerous publications based on MoBa data have used this short version of the CBCL.35–38
TABLE 1.
Items From the CBCL Included in the MoBa Questionnaires Completed When the Children Were 1.5, 3, and 5 Years Old
| Problems | 1.5-y Follow-up | 3-y Follow-up | 5-y Follow-up |
|---|---|---|---|
| Emotional | |||
| Somatic complaints | |||
| Does not eat well | X | X | X |
| Stomachaches or cramps without medical cause | — | X | X |
| Constipated, does not move bowels | — | X | |
| Vomiting, throwing up without medical cause | — | X | X |
| Anxious and/or depressed | |||
| Too fearful or anxious | X | X | X |
| Clings to adults or too dependent | X | X | X |
| Gets too upset when separated from parents | X | X | X |
| Nervous, high strung, or tense | — | — | X |
| Unhappy, sad, or depressed | — | — | X |
| Feelings are easily hurt | — | — | X |
| Self-conscious or easily embarrassed | — | — | X |
| Emotionally reactive | |||
| Disturbed by any change in routine | X | X | X |
| Sudden changes in moods or feelings | — | X | — |
| Behavior | |||
| Attention | |||
| Cannot concentrate, cannot pay attention for long | X | X | X |
| Quickly shifts from 1 activity to another | X | X | X |
| Cannot sit still, restless or overactive | X | X | X |
| Poorly coordinated or clumsy | — | X | X |
| Aggressive behavior | |||
| Gets in many fights | X | X | X |
| Hits others | X | X | X |
| Defiant | X | X | X |
| Does not seem to feel guilty after misbehaving | X | X | X |
| Punishment does not change his or her behavior | X | X | X |
| Cannot stand waiting, wants everything now | — | X | X |
| Demands must be met immediately | — | X | X |
—, not applicable.
Other Variables
To account for sibling-order associations, we adjusted for parity (ie, the number of previous births) centered within each mother. We also adjusted for offspring sex.
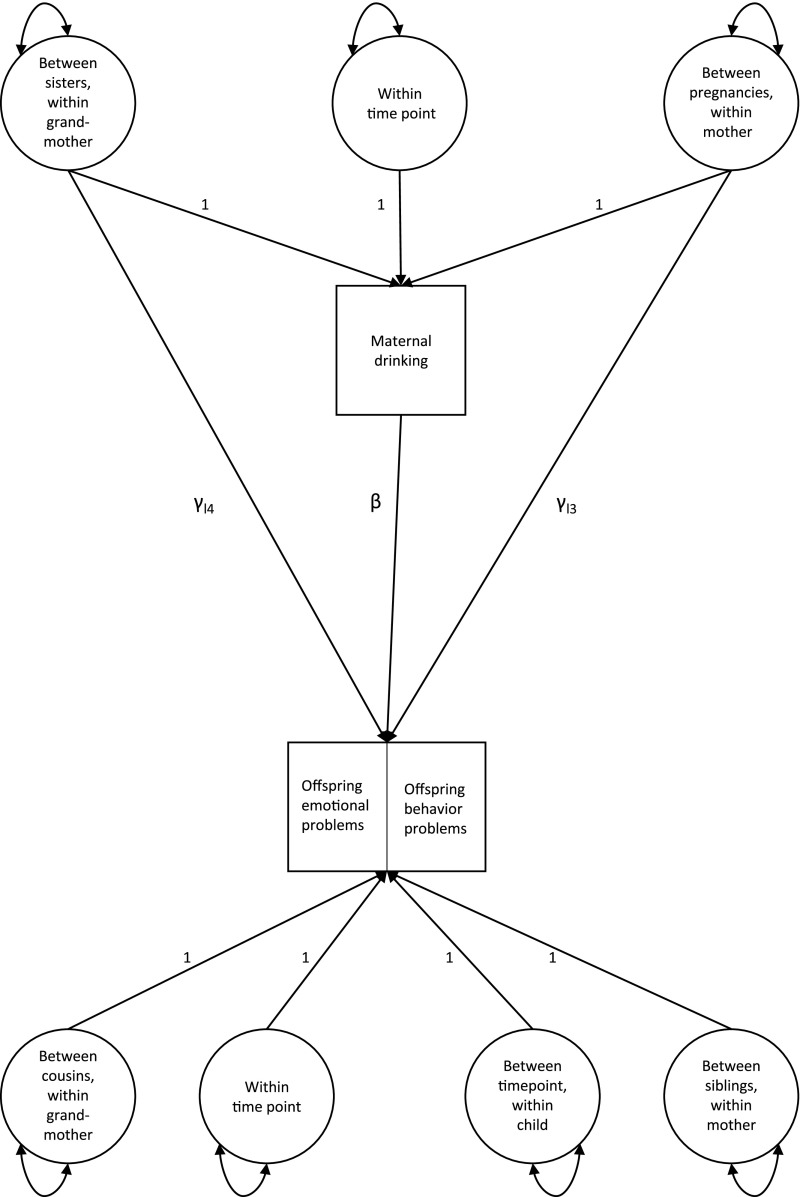
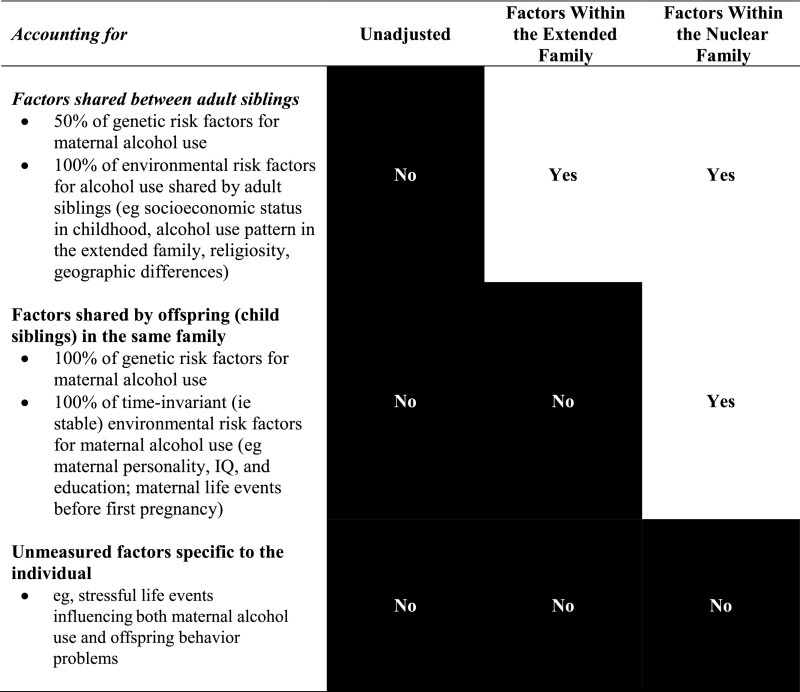
Statistical Analyses
To model the intergenerational transmission of risk, we applied a generalized structural equation model (Fig 1). Maternal alcohol use is influenced by (1) familial factors shared by adult sisters (ie, 50% of genetic effects and 100% of extended familial environmental effects), (2) factors that are stable within a woman not explained by a previous level (ie, between time points within mother; 50% of genetic effects and stable environmental effects not shared between adult sisters), and (3) time-varying environmental factors influencing alcohol consumption at a given time point. The first 2 factors can influence offspring behavior and emotional problems directly (γl4 and γl3) or can be indirectly mediated through maternal alcohol use, an example of “nature of nurture”(β).39 Moreover, maternal alcohol use can influence offspring behavior and emotional problems directly (β). Residual variance in offspring behavior and emotional problems is also divided into effects located at the 2 familial levels: factors shared by cousins (0.125 of genetic associations) and additional factors shared by siblings (remaining 0.375 of genetic associations and 100% of environmental associations shared by siblings) and associations that are not shared by siblings (remaining 0.50 of genetic associations and individual-specific environmental associations). Our primary aim was to render an unbiased estimate of the associations of maternal alcohol use (β). Therefore, we did not design the model to calculate biometric parameters such as heritability or familial environmental associations. Notably, to estimate such parameters without possible bias to β, the data should also have comprised monozygotic and dizygotic twins or adopted siblings. We did not assume any constrained model across time for the residual variance in the child outcomes and therefore let the residual variance correlate freely across time. We ran 3 models (Fig 2) for emotional problems and 3 models for behavior problems. Each of the levels leads to an incremental adjustment of potential confounding factors.
FIGURE 1.
Illustration of how maternal concurrent drinking is influenced by familial factors shared by sisters, factors that are stable within the woman across her children, and time-varying environmental factors that influence alcohol consumption at different time points.
FIGURE 2.
Representation of possible confounders adjusted for in unadjusted and extended and nuclear family designs.
After we estimated the crude association, we sequentially adjusted for familial confounding in 2 steps: first for unobserved risk factors in the extended family, then for unobserved risk factors within the nuclear family (Fig 2). In the first step, we adjust for all environmental factors of alcohol use shared by adult sisters (eg, upbringing environment and early social class) and 50% of passive genetic transmission. Because the mother acts as her own control across children and time points within children, the last step contains a full adjustment for passive genetic transmission from risk for maternal alcohol use to offspring behavior and emotional problems.40 Drinking and other risk factors during pregnancy, which is a type of risk factor between the measured time points for a given child, is included in the estimate for familial confounding. We calculated the effect of a 1-unit change in the alcohol use score on the CBCL T scores (mean = 50; SD = 10). To render our results interpretable in a clinical setting, we calculated the corresponding odds ratios (OR). We used the SD of the logistic response variable 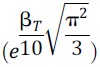 to rescale the effect sizes from T scores (βT) to ORs via logits.41
to rescale the effect sizes from T scores (βT) to ORs via logits.41
We handled missing data due to nonresponse by full-information maximum likelihood. This is according to the missing-at-random assumption accounting for bias due to observed variables from all levels of the family included in the model (eg, nonresponse and attrition associated with high alcohol consumption or child behavior problems).
Results
Descriptive Characteristics
Table 2 provides an overview of background characteristics for study participants. The mean age of the women was 30 years when they entered the study. Relatively few women reported consuming 5 or more units of alcohol during a weekend drinking occasion, with a range of 13.5% when their children were 1.5 years old to 8.7% when their children were 5 years old. Less than 1% at all time points consumed 3 or more alcohol units during a weekday drinking occasion.
TABLE 2.
Overview of Background Characteristics for Study Participants That Contributed to the 1.5-, 3-, and 5-Year Follow-up
| 1.5-y Follow-up (N = 31 410) | 3-y Follow-up (N = 24 844) | 5-y Follow-up (N = 17 030) | |
|---|---|---|---|
| Maternal age, y, when entering study, mean (SD) | 30.00 (4.2) | 30.01 (4.1) | 30.67 (4.1) |
| Parity, n (%) | |||
| 0 | 13 671 (43.5) | 10 858 (43.7) | 6252 (36.7) |
| 1 | 12 224 (38.9) | 9763 (39.3) | 7441 (43.7) |
| 2 | 4369 (13.9) | 3335 (13.4) | 2638 (15.5) |
| 3 | 870 (2.8) | 678 (2.7) | 538 (3.2) |
| ≥4 | 870 (2.8) | 210 (0.9) | 161 (1.0) |
| How often do you consume alcohol at present?a n (%) | |||
| Never | 8500 (27.4) | 6446 (26.6) | 1453 (14.4) |
| Less than once per month | 9108 (29.3) | 6897 (28.5) | 2695 (26.7) |
| Roughly 1–3 times per month | 7940 (25.6) | 6000 (24.8) | 2806 (27.8) |
| Roughly once per week | 3599 (11.6) | 2939 (12.2) | 1680 (16.6) |
| Roughly 2–3 times per week | 1664 (5.4) | 1640 (6.8) | 1269 (12.6) |
| Roughly 4–5 times per week | 223 (0.7) | 229 (0.9) | 173 (1.7) |
| Roughly 6–7 times per week | 40 (0.1) | 38 (0.2) | 31 (0.3) |
| How many units of alcohol do you usually drink when you consume alcohol on weekends?a,b n (%) | |||
| <1 | 3467 (12.8) | 3019 (13.9) | 910 (9.8) |
| 1–2 | 13 574 (50.1) | 11 163 (51.5) | 5326 (57.3) |
| 3–4 | 6396 (23.6) | 4936 (22.8) | 2263 (24.3) |
| 5–6 | 2706 (10.0) | 1856 (8.6) | 631 (6.8) |
| 7–9 | 785 (2.9) | 572 (2.6) | 154 (1.7) |
| ≥10 | 165 (0.6) | 124 (0.6) | 17 (0.2) |
| How many units of alcohol do you usually drink when you consume alcohol on weekdays?a,b n (%) | |||
| <1 | 14 847 (77.8) | 10 159 (75.8) | 4868 (71.9) |
| 1–2 | 4120 (21.6) | 3171 (23.7) | 1857 (27.4) |
| 3–4 | 93 (0.5) | 68 (0.5) | 44 (0.6) |
| 5–6 | 14 (0.1) | 9 (0.1) | 2 (0.0) |
| ≥7 | 1 (0.0) | 1 (0.0) | 1 (0.0) |
| At-risk drinkinga,b,c n (%) | |||
| 0 | 9455 (60.9) | 6690 (62.7) | 3964 (64.2) |
| 0.25–0.75 | 5541 (35.7) | 3638 (34.1) | 2082 (33.7) |
| ≥1 | 519 (3.3) | 337 (3.2) | 127 (2.1) |
| Child sex, n (%) | |||
| Male | 15 292 (48.7) | 12 028 (48.4) | 8294 (48.7) |
| Female | 16 118 (51.3) | 12 816 (51.6) | 8736 (51.3) |
Version A of the MoBa 5-y questionnaires did not include measures about alcohol.
Consumption of both 3 or more units of alcohol on a typical weekday drinking occasion and 5 or more units during a typical weekend drinking occasion were defined as at-risk drinking.
1 represents at-risk drinking. The reported typical unit of alcohol consumption was coded as follows: 1 to 2 = 0, 3 to 4 = 0.5, 5 to 6 = 1, 7 to 9 = 2, and >10 = 3 for weekends; 1 to 2 = 0, 3 to 4 = 1, 5 to 6 = 2, and 7 to 9 = 3 for weekdays. We used the average of weekends and weekdays.
Child Behavior and Emotional Outcome Models
Table 3 shows the unadjusted and adjusted associations of maternal alcohol use on offspring emotional and behavior problems. Children of mothers with at-risk drinking behaviors had a higher likelihood of behavior problems (β = 3.53; 95% confidence interval [CI] 3.01 to 4.05). When adjusting for factors in the extended family, this association was reduced with 45% (β = 1.93; 95% CI 1.16 to 2.71). Adjusting for factors in the nuclear family further reduced the association (β = 1.20; 95% CI 0.39 to 2.01; a 66% reduction in effect size).
TABLE 3.
Results From General Structural Equation Modeling of the Effect of Maternal Concurrent At-Risk Drinking on Child Behavior and Emotional Problems
| Problems | Unadjusted | Within Extended Family | Within Nuclear Family | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | β | 95% CI | OR | β | 95% CI | OR | β | 95% CI | |
| Behavior | 1.90 | 3.53 | 3.01 to 4.05 | 1.42 | 1.93 | 1.16 to 2.71 | 1.24 | 1.20 | 0.39 to 2.01 |
| Emotional | 1.39 | 1.80 | 1.26 to 2.34 | 1.13 | .67 | −0.12 to 1.46 | 1.11 | .58 | −0.31 to 1.48 |
Children of mothers with at-risk drinking behaviors were more likely to have emotional problems (β = 1.80; 95% CI 1.26 to 2.34). Adjusting for all common factors in the extended family reduced this association by 63% (β = 0.67; 95% CI −0.12 to 1.46). The association was further reduced when adjusting for factors in the nuclear family (β = 0.58; 95% CI −0.31 to 1.48; a 68% reduction of the unadjusted effect).
Factors shared by adult sisters accounted for 21% of the variation in maternal alcohol consumption, whereas factors not shared by adult sisters but that were stable within the mother accounted for 40%, and factors varying across time points accounted for 39%.
Discussion
Several factors may contribute to the association between maternal drinking and child emotional and behavior problems. To contribute to a better understanding, we investigated whether the link remained after taking into account passive transmission of familial risk. We found a considerable association between concurrent maternal alcohol use and offspring behavior problems in children aged 1.5 to 5 years. This association was reduced by 66% when adjusting for familial factors. Factors both in the extended and nuclear family appeared to confound the exposure-outcome association, but the association was still notable and significant. Also for emotional problems, there was initially an effect, but the effect was reduced and became insignificant after adjusting for familial factors.
Several studies have investigated the association between maternal drinking and child emotional and behavior problems,8,17 but the findings have been inconsistent. A possible explanation is that most studies use study designs that do not adequately account for confounding.18,42,43 Our findings are partly in line with findings from an Australian study that included the children-of-twins design.29 Results from our study indicate both environmental and familial transmission of risk for behavior problems; the Australian study indicated genetic transmission of risk for behavior problems but found no support for environmental associations.29
The extant literature suggests that the association between substance-related problems and behavior problems is stronger than between substance-related problems and emotional problems. It therefore seemed plausible that the association between maternal drinking and child emotional problems would be smaller than that between maternal drinking and child behavior problems.15,44 Indeed, this was the case for in the current study, and we found no environmental transmission. The Australian twin study did not suggest environmental transmission of risk from parental alcoholism in child emotional problems and was inconclusive regarding genetic transmission of risk.29 A possible reason for the difference in findings is that genetic risk for various behavior and emotional problems may vary at different ages23,45: children in our study were 1.5, 3, and 5 years old; the Australian study included participants between 7 and 24 years old.29 Another study assessed the association between maternal drinking and child mental health problems8 and found an association between maternal drinking and emotional and behavior problems among 8- to 11-year-old girls but not in younger girls or boys in any age groups,8 suggesting that it may be easier to identify symptoms as children grow older. Our results were inconclusive regarding the association of maternal at-risk drinking with child emotional problems. Methodologically robust studies should follow children over a more extended period to see if this link is more apparent as children become older.
Although maternal drinking is probably related to child behavior problems, more than half of the association was due to familial confounding. Nevertheless, the findings suggest that a reduction in maternal drinking is likely to contribute to fewer behavior problems; in particular, parents of children with such problems may see an improvement in these areas if mothers discontinue or reduce their drinking. Without improvement, the accumulation of adverse outcomes associated with behavior problems can be substantial, for the persons with these problems and society.46 The literature has focused on the effects of parental AUD and heavy drinking on child emotional and behavior problems13,17,18,29; the association between more normative drinking, maternal at-risk drinking, and child behavior problems found in the current study suggests that the number of children at risk is probably higher than previously assumed. The findings may be used as an argument for implementing and strengthening strategies aimed at reducing parental drinking.
Major strengths include that our sample is from a prospective population cohort study and has a large sample size, and with the methodologic robustness combining 2 levels, or generations, of sibling design (ie, adult and child siblings), we could assess the relative effect of confounding factors that are stable within a nuclear family (eg, parental education) but vary between extended families.
The following limitations should be considered when interpreting the results. The participation rate in the MoBa may have resulted in selection bias. Indeed, some groups are underrepresented (eg, pregnant women who live alone, women who are <25 years old, mothers with >2 previous births, and women who smoke).47 When comparing the MoBa population to that of the general pregnant population in Norway, the differences are small,47,48 and in this study, all exposed and unexposed children were, by design, balanced on stable factors leading to selection (eg, socioeconomic status). Only maternal drinking frequency and quantity were used to identify maternal at-risk drinking. This is because the full Alcohol Use Disorders Identification Test of consumption was not used in the MoBa in the time periods addressed in this study. Fortunately, all stable factors leading to underreporting or overreporting of maternal alcohol use were adjusted for by design. Although it would have been preferable to have information about child problems from sources other than the mother, a major strength of the sibling design is that by having several children per each mother, we adjust for all stable systematic maternal rating biases. As depicted in Fig 2, the major weakness of the current study is its inability to adjust for dynamic (time-variant) factors (eg, how marital conflicts or fluctuations in paternal drinking may influence maternal drinking).
Conclusions
Our findings suggest that after accounting for passive transmission of familial risk, there is an association between maternal drinking and child behavior problems. It therefore seems likely that a reduction in maternal alcohol consumption may improve outcomes for children with such symptoms.
Acknowledgments
We are grateful to all the families who participate in this ongoing study.
Glossary
- AUD
alcohol use disorder
- CBCL
Child Behavior Checklist
- CI
confidence interval
- MoBa
Norwegian Mother, Father, and Child Cohort Study
- OR
odds ratio
Footnotes
Dr Lund assisted in study conceptualization, study design, and analysis aspects, interpreted results, drafted the initial manuscript, and reviewed and revised the manuscript; Dr Ystrom conceptualized and designed the study, designed the data analysis strategy, conducted the data analysis, assisted in drafting the initial manuscript, and reviewed and revised the manuscript; Drs Moen Eilertsen and Gjerde assisted in the study conceptualization, data integrity, and analysis aspects and critically reviewed the manuscript for important intellectual content; Drs Ask Torvik, Røysamb, and Reichborn-Kjennerud assisted in the study conceptualization and critically reviewed the manuscript for important intellectual content; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by The Research Council of Norway (grants 262177 and 288083; grant 273659 to Dr Ask Torvik). The Norwegian Mother, Father, and Child Cohort Study is supported by the Norwegian Ministry of Education and Research and the Norwegian Ministry of Health and Care Services (NIH-NIEHS contract N01-ES-75558 and NIH-NINDA grants 1 UO1 NS 047537-01 and 2 Uo1 NS 047537-06A1).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose
References
- 1.Jacob T, Windle M, Seilhamer RA, Bost J. Adult children of alcoholics: drinking, psychiatric, and psychosocial status. Psychol Addict Behav. 1999;13(1):3 [Google Scholar]
- 2.Rossow I, Felix L, Keating P, McCambridge J. Parental drinking and adverse outcomes in children: a scoping review of cohort studies. Drug Alcohol Rev. 2016;35(4):397–405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Christoffersen MN, Soothill K. The long-term consequences of parental alcohol abuse: a cohort study of children in Denmark. J Subst Abuse Treat. 2003;25(2):107–116 [DOI] [PubMed] [Google Scholar]
- 4.Eiden RD, Molnar DS, Colder C, Edwards EP, Leonard KE. A conceptual model predicting internalizing problems in middle childhood among children of alcoholic and nonalcoholic fathers: the role of marital aggression. J Stud Alcohol Drugs. 2009;70(5):741–750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hussong AM, Huang W, Curran PJ, Chassin L, Zucker RA. Parent alcoholism impacts the severity and timing of children’s externalizing symptoms. J Abnorm Child Psychol. 2010;38(3):367–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Masten AS, Roisman GI, Long JD, et al. Developmental cascades: linking academic achievement and externalizing and internalizing symptoms over 20 years. Dev Psychol. 2005;41(5):733–746 [DOI] [PubMed] [Google Scholar]
- 7.Finan LJ, Schulz J, Gordon MS, Ohannessian CM. Parental problem drinking and adolescent externalizing behaviors: the mediating role of family functioning. J Adolesc. 2015;43:100–110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Husky MM, Keyes K, Hamilton A, et al. Maternal problem drinking and child mental health. Subst Use Misuse. 2017;52(14):1823–1831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith VC, Wilson CR; Committee on Substance Use and Prevention . Families affected by parental substance use. Pediatrics. 2016;138(2):e20161575. [DOI] [PubMed] [Google Scholar]
- 10.Gjone H, Stevenson J, Sundet JM, Eilertsen DE. Changes in heritability across increasing levels of behavior problems in young twins. Behav Genet. 1996;26(4):419–426 [DOI] [PubMed] [Google Scholar]
- 11.Chassin L, Haller M, Lee MR, Handley E, Bountress K, Beltran I. Familial Factors Influencing Offspring Substance Use and Dependence In: Sher KJ, ed. The Oxford Handbook of Substance Use and Substance Use Disorders, vol. Vol 1 New York, NY: Oxford University Press; 2016:449 [Google Scholar]
- 12.McAdams TA, Neiderhiser JM, Rijsdijk FV, Narusyte J, Lichtenstein P, Eley TC. Accounting for genetic and environmental confounds in associations between parent and child characteristics: a systematic review of children-of-twins studies. Psychol Bull. 2014;140(4):1138–1173 [DOI] [PubMed] [Google Scholar]
- 13.Bountress K, Chassin L. Risk for behavior problems in children of parents with substance use disorders. Am J Orthopsychiatry. 2015;85(3):275–286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kendler KS, Jacobson KC, Prescott CA, Neale MC. Specificity of genetic and environmental risk factors for use and abuse/dependence of cannabis, cocaine, hallucinogens, sedatives, stimulants, and opiates in male twins. Am J Psychiatry. 2003;160(4):687–695 [DOI] [PubMed] [Google Scholar]
- 15.Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003;60(9):929–937 [DOI] [PubMed] [Google Scholar]
- 16.Knopik VS, Heath AC, Jacob T, et al. Maternal alcohol use disorder and offspring ADHD: disentangling genetic and environmental effects using a children-of-twins design. Psychol Med. 2006;36(10):1461–1471 [DOI] [PubMed] [Google Scholar]
- 17.Ohannessian CM, Hesselbrock VM, Kramer J, et al. The relationship between parental alcoholism and adolescent psychopathology: a systematic examination of parental comorbid psychopathology. J Abnorm Child Psychol. 2004;32(5):519–533 [DOI] [PubMed] [Google Scholar]
- 18.Knudsen AK, Ystrom E, Skogen JC, Torgersen L. Maternal heavy alcohol use and toddler behavior problems: a fixed effects regression analysis. Eur Child Adolesc Psychiatry. 2015;24(10):1269–1277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kushner MG, Wall MM, Krueger RF, et al. Alcohol dependence is related to overall internalizing psychopathology load rather than to particular internalizing disorders: evidence from a national sample. Alcohol Clin Exp Res. 2012;36(2):325–331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry. 1997;54(4):313–321 [DOI] [PubMed] [Google Scholar]
- 21.Kendler KS, Aggen SH, Knudsen GP, Røysamb E, Neale MC, Reichborn-Kjennerud T. The structure of genetic and environmental risk factors for syndromal and subsyndromal common DSM-IV axis I and all axis II disorders. Am J Psychiatry. 2011;168(1):29–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lahey BB, Krueger RF, Rathouz PJ, Waldman ID, Zald DH. A hierarchical causal taxonomy of psychopathology across the life span. Psychol Bull. 2017;143(2):142–186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Torvik FA, Rosenström TH, Ystrom E, et al. Stability and change in etiological factors for alcohol use disorder and major depression. J Abnorm Psychol. 2017;126(6):812–822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mørland J. Biological mechanisms and some clinical effects of alcohol [in Norwegian]. Tidsskr Nor Laegeforen. 2003;123(2):180–184 [PubMed] [Google Scholar]
- 25.Hale WW III, Engels R, Meeus W. Adolescent’s perceptions of parenting behaviours and its relationship to adolescent generalized anxiety disorder symptoms. J Adolesc. 2006;29(3):407–417 [DOI] [PubMed] [Google Scholar]
- 26.Ehringer MA, Rhee SH, Young S, Corley R, Hewitt JK. Genetic and environmental contributions to common psychopathologies of childhood and adolescence: a study of twins and their siblings. J Abnorm Child Psychol. 2006;34(1):1–17 [DOI] [PubMed] [Google Scholar]
- 27.Hayward RA, Depanfilis D, Woodruff K. Parental methamphetamine use and implications for child welfare intervention: a review of the literature. J Public Child Welf. 2010;4:25–60 [Google Scholar]
- 28.Lund IO, Moen Eilertsen E, Gjerde LC, et al. Is the association between maternal alcohol consumption in pregnancy and pre-school child behavioural and emotional problems causal? Multiple approaches for controlling unmeasured confounding. Addiction. 2019;114(6):1004–1014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Waldron M, Martin NG, Heath AC. Parental alcoholism and offspring behavior problems: findings in Australian children of twins. Twin Res Hum Genet. 2009;12(5):433–440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ioannidis JPA, Greenland S, Hlatky MA, et al. Increasing value and reducing waste in research design, conduct, and analysis. Lancet. 2014;383(9912):166–175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Magnus P, Birke C, Vejrup K, et al. Cohort profile update: the Norwegian Mother and Child Cohort Study (MoBa). Int J Epidemiol. 2016;45(2):382–388 [DOI] [PubMed] [Google Scholar]
- 32.Irgens LM. The Medical Birth Registry of Norway. Epidemiological research and surveillance throughout 30 years. Acta Obstet Gynecol Scand. 2000;79(6):435–439 [PubMed] [Google Scholar]
- 33.Kendler KS, Neale MC, Sullivan P, Corey LA, Gardner CO, Prescott CA. A population-based twin study in women of smoking initiation and nicotine dependence. Psychol Med. 1999;29(2):299–308 [DOI] [PubMed] [Google Scholar]
- 34.Achenbach TM. Manual for the Child Behavior Checklist 2/3 Years. Burlington, VT: University of Vermont, Department of Psychiatry; 1992 [Google Scholar]
- 35.Gjerde LC, Eilertsen EM, Reichborn-Kjennerud T, et al. Maternal perinatal and concurrent depressive symptoms and child behavior problems: a sibling comparison study. J Child Psychol Psychiatry. 2017;58(7):779–786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brandlistuen RE, Ystrom E, Nulman I, Koren G, Nordeng H. Prenatal paracetamol exposure and child neurodevelopment: a sibling-controlled cohort study. Int J Epidemiol. 2013;42(6):1702–1713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sivertsen B, Harvey AG, Reichborn-Kjennerud T, Torgersen L, Ystrom E, Hysing M. Later emotional and behavioral problems associated with sleep problems in toddlers: a longitudinal study. JAMA Pediatr. 2015;169(6):575–582 [DOI] [PubMed] [Google Scholar]
- 38.Zachrisson HD, Dearing E, Lekhal R, Toppelberg CO. Little evidence that time in child care causes externalizing problems during early childhood in Norway. Child Dev. 2013;84(4):1152–1170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kong A, Thorleifsson G, Frigge ML, et al. The nature of nurture: effects of parental genotypes. Science. 2018;359(6374):424–428 [DOI] [PubMed] [Google Scholar]
- 40.Lahey BB, D’Onofrio BM. All in the family: comparing siblings to test causal hypotheses regarding environmental influences on behavior. Curr Dir Psychol Sci. 2010;19(5):319–323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Meta-Analysis Converting among Effect Sizes In: Introduction to Meta-Analysis. Chichester, United Kingdom: John Wiley & Sons, Ltd; 2009:1–5 [Google Scholar]
- 42.Mahedy L, Hammerton G, Teyhan A, et al. Parental alcohol use and risk of behavioral and emotional problems in offspring. PLoS One. 2017;12(6):e0178862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hafekost K, Lawrence D, O’Leary C, Bower C, Semmens J, Zubrick SR. Maternal alcohol use disorder and risk of child contact with the justice system in Western Australia: a population cohort record linkage study. Alcohol Clin Exp Res. 2017;41(8):1452–1460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Krueger RF, Markon KE. Reinterpreting comorbidity: a model-based approach to understanding and classifying psychopathology. Annu Rev Clin Psychol. 2006;2:111–133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kendler KS, Lönn SL, Maes HH, et al. A national Swedish longitudinal twin-sibling study of criminal convictions from adolescence through early adulthood. Twin Res Hum Genet. 2015;18(3):227–233 [DOI] [PubMed] [Google Scholar]
- 46.Caspi A, Houts RM, Belsky DW, et al. Childhood forecasting of a small segment of the population with large economic burden. Nat Hum Behav. 2016;1:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nilsen RM, Vollset SE, Gjessing HK, et al. Self-selection and bias in a large prospective pregnancy cohort in Norway. Paediatr Perinat Epidemiol. 2009;23(6):597–608 [DOI] [PubMed] [Google Scholar]
- 48.Magnus P, Irgens LM, Haug K, Nystad W, Skjaerven R, Stoltenberg C; MoBa Study Group . Cohort profile: the Norwegian mother and child cohort study (MoBa). Int J Epidemiol. 2006;35(5):1146–1150 [DOI] [PubMed] [Google Scholar]