Abstract
Endometrial cancer is the most common gynecologic malignancy in developed countries. The antibody–drug conjugate (ADC) sacituzumab govitecan (SG) targets trophoblast cell‐surface antigen‐2 (Trop‐2) – a cell‐surface glycoprotein highly expressed in many epithelial tumors – and delivers the active metabolite of irinotecan SN‐38 to Trop‐2‐positive tumor cells. We evaluated Trop‐2 expression in endometrial endometrioid carcinoma (EC) tissues and the activity of SG against primary poorly differentiated EC cell lines and xenografts. Trop‐2 expression was assessed in 143 formalin‐fixed–paraffin‐embedded tumors and seven primary tumor cell lines by immunohistochemistry and flow cytometry, respectively. Cell viability of primary tumor cell lines was assessed following exposure to SG, or control antibodies. Antibody‐dependent cell cytotoxicity (ADCC) against Trop‐2‐positive and Trop‐2‐negative EC cell lines was measured in vitro using 4‐h chromium release assays. A Trop‐2‐positive EC xenograft model was used to determine the in vivo activity of SG. Moderate‐to‐strong staining was detected in 84% (120/143) of EC samples, whereas 43% (3/7) of the primary EC cell lines tested overexpressed Trop‐2. EC cell lines overexpressing Trop‐2 were significantly more sensitive to SG compared to control ADC (P = 0.014 and P = 0.005). Both SG and the unconjugated parental antibody hRS7 mediated high ADCC against Trop‐2‐positive cell lines. Moreover, SG induced significant bystander killing of Trop‐2‐negative tumors cocultured with Trop‐2‐positive tumors. In the xenograft model, intravenous administration of SG twice weekly for three weeks was well tolerated and demonstrated impressive tumor growth inhibition against poorly differentiated, chemotherapy‐resistant EC xenografts (P = 0.011). In summary, SG is a novel ADC with remarkable preclinical activity against poorly differentiated EC cell lines overexpressing Trop‐2. These findings warrant future clinical trials.
Keywords: antibody–drug conjugate, endometrial carcinoma, IMMU‐132, sacituzumab govitecan, uterine cancer
TROP‐1 is overexpressed in the majority of endometrial cancers. Sacituzumab Gavitecan (SG) is highly effective, both in vitro as well as in vivo, against primary endometrial cancer cell lines and xenografts overexpressing TROP‐2. Clinical studies with SG in patients with recurrent, chemotherapy‐resistant endometrial cancer overexpressing TROP‐2 are warranted.
![]()
Abbreviations
- ADC
antibody–drug conjugate
- ADCC
antibody‐dependent cellular cytotoxicity
- control ADC
nontargeting control antibody–drug conjugate
- DAR
drug‐to‐antibody ratio
- EC
endometrial endometrioid carcinoma
- hRS7
unconjugated monoclonal antibody
- PBLs
peripheral blood lymphocytes
- SG
sacituzumab govitecan
- SCID
severe combined immunodeficiency
- TMA
tissue microarray
- Trop‐2
trophoblast cell‐surface antigen‐2
1. Introduction
Endometrial endometrioid carcinoma (EC) is the most prevalent gynecologic malignancy in the United States, with approximately 61 880 newly diagnosed cases and 12 160 deaths in 2019. Unlike ovarian and cervical cancer, the incidence and mortality rates from EC are globally increasing. If current trends continue, the incidence of EC in the United States will double by 2030 (Siegel et al., 2019).
Traditionally, histologic classification has been used to counsel patients regarding prognosis and to guide decision‐making regarding the necessity for adjuvant treatment. Women diagnosed with early‐stage well‐differentiated endometrioid endometrial cancers have a 5‐year overall survival rate of over 90% after surgery with or without adjuvant radiation (Felix et al., 2010). However, up to 35% of EC patients are diagnosed with a more aggressive histopathology, such as poorly differentiated endometrioid, and serous or clear cell carcinoma (Bokhman, 1983; Rose et al., 2017). These patients account for the majority who present with stage III or IV disease that are typically nonresponsive to the gold standard chemotherapy treatment involving carboplatin plus paclitaxel, which portends a poor prognosis (Creutzberg et al., 2004; Rose et al., 2017; Young et al., 2015). The identification of novel treatment modalities for patients diagnosed with biologically aggressive EC remains an unmet medical need.
Antibody–drug conjugates (ADCs) precisely target tumor cells as they are composed of a monoclonal antibody specific to surface antigens present on particular tumor cells and then kill these tumor cells with a highly potent chemical linker. ADCs may therefore optimize tumor targeting in vivo while potentially minimizing the side effects of highly toxic chemotherapy agents (Tsimberidou, 2015). Many ADCs are currently in late‐stage development, while others are either in clinical trials or have recently been approved for clinical use by the Food and Drugs Administration (FDA). For example, T‐DM1 (Kadcyla; Genentech/Roche, South San Francisco, CA, USA) is currently approved by the European Medical Agency (EMA) and FDA for patients with HER2‐positive metastatic breast cancer. Additionally, IMGN853 (Immunogen, Waltham, MA, USA) has already demonstrated high preclinical activity against type II endometrial cancer and other solid tumors (Ab et al., 2015; Altwerger et al., 2018; English et al., 2014; Nicoletti et al., 2015).
Human trophoblast cell‐surface antigen 2 (Trop‐2) is a 45 kDa transmembrane glycoprotein encoded by the TACSTD2 gene on chromosome 1p32, which is differentially expressed in a variety of epithelial tumors (Cardillo et al., 2015). Trop‐2 overexpression has been previously demonstrated to represent an independent marker for poor prognosis in multiple human tumors including endometrial endometrioid adenocarcinomas by promoting increased invasion and metastases (Bignotti et al., 2012; Trerotola et al., 2013). Importantly, the differential expression in tumor cells when compared to normal tissues renders Trop‐2 an attractive target for cancer immunotherapy.
Sacituzumab govitecan or IMMU‐132 (SG) is a novel ADC combining the humanized RS7 antibody targeting Trop‐2 coupled to a hydrolyzable linker that allows for a time‐dependent release of the payload, SN‐38, the active metabolite of irinotecan (7‐ethyl‐10‐hydroxycamptothecin) to the tumor tissue (Goldenberg et al., 2015). SN‐38 has a 100‐ to 1000‐fold higher potency than irinotecan (Goldenberg et al., 2015; Liu et al., 2009; Mathijssen et al., 2001). SG is characterized by a conjugation of drug to monoclonal antibody at a high ratio (8 : 1) without affecting antibody targeting and pharmacokinetics. Importantly, the pH‐sensitive hydrolyzable linker of SG allows for a strong, time‐released bystander effect against nearby Trop‐2‐negative tumor cells within the tumor microenvironment (Goldenberg et al., 2015). Currently, no reports exist in the literature on the potential clinical activity of SG in EC patients. However, encouraging clinical activity of SG has recently been reported in a phase I/II IMMU‐132‐01 basket study of small‐cell lung cancer and non‐small‐cell lung cancer as well as in studies of triple‐negative breast cancer, HR+/HER2‐ breast cancer, and urothelial cancer (Bardia et al., 2019; Faltas et al., 2016; Gray et al., 2017; Heist et al., 2017).
The initial objective of this study was to determine the expression of Trop‐2 in EC tissue samples and primary established EC cell lines. Thereafter, we aimed to examine the preclinical antitumor activity of SG against multiple primary EC cell lines and xenograft models.
2. Materials and methods
2.1. Establishment of EC cell lines
The Institutional Review Board (IRB) approved this study, and patient consent was obtained per institutional guidelines prior to tissue collection. The EC cell lines were established from fresh tumor biopsy samples and de‐identified as described previously from our group (El‐Sahwi et al., 2010; Roque et al., 2014; Zhao et al., 2013). As this study involves work performed with human samples, all the study methodologies conformed to the standards set by the Declaration of Helsinki (World Medical Association, 2001).
2.2. Tissue microarray
A retrospective cohort of stage I‐IV endometrioid EC tissue microarray (TMA) format samples were used in this study (n = 143). Representative areas from primary EC were selected in hematoxylin/eosin‐stained preparations by a trained gynecologic surgical pathologist, and 0.6 mm cores were obtained and arrayed in a recipient block. In order to increase representation and capture possible marker heterogeneity, two cores were obtained from different areas of each tumor were included in the TMA samples. Sections of the resultant TMA samples were cut at 5 μm and then transferred to glass slides for further histologic staining and processing. The tissue samples were collected with either specific consent or a waiver of consent under an approved Yale Human Investigation Committee protocol. Next, purified goat polyclonal antibody against the recombinant human Trop‐2 extracellular domain (R&D Systems, Inc., Minneapolis, MN, USA; diluted 1 : 100) was applied for 1 h. After that, a secondary biotinylated anti‐goat antibody (Vector Laboratories, Burlingame, CA, USA; diluted 1 : 250) and the streptavidin–biotin complex (StreptABComplex/HRP; Dako, Carpinteria, CA, USA) were applied. Subsequently, 303‐diaminobenzidine (Dako) was used as a chromogen and the sections were counterstained by hematoxylin (Dako). For all of the above, appropriate positive and negative controls were used. The percentage of tumor cells with membranous Trop‐2 immunoreactivity was estimated, and the staining intensity was measured semiquantitatively using the following scale: 0 for no staining; 1+ for weak; 2+ for moderate; and 3+ for strong staining. In order to obtain the final immunoreactivity score, staining intensity (1+, 2+, 3+) was multiplied by the percentage of positive tumor cells. The final immunoreactivity score was then classified into four ordinal categories: 0–9 negative (score 0), 10–99 weak (score 1), 100–199 moderate (score 2), and 200–300 strong (score 3).
2.3. Determination of Trop‐2 expression in primary EC cell lines
Flow cytometry to determine Trop‐2 expression was performed on primary poorly differentiated EC cell lines that were cultured in vitro for up to 50 passages. EC cell lines were incubated with 2.5 μg·mL−1 of unconjugated antibody hRS7 IgG for 120 min at 4 °C, and then stained with a fluorescein isothiocyanate‐conjugated goat anti‐human F(ab’)2 immunoglobulin (FITC) that was used as a secondary reagent (BioSource International, Camarillo, CA, USA). The data were acquired using cell quest software (BD Biosciences, San Diego, CA, USA). Mean fluorescence intensity (MFI) was evaluated using cell quest and prism 8. Cell lines with MFI greater than 100 were determined to have 3+ expression of Trop‐2 and with MFI of 51–100 2+, 21–50 1+, and 20 or less were considered negative for Trop‐2 expression.
2.4. Drugs
Sacituzumab govitecan (hRS7‐CL2A‐SN‐38), a nontargeting control ADC (h679‐CL2A‐SN‐38), and unconjugated monoclonal antibody hRS7 IgG were obtained from Immunomedics, Inc. (Morris Plains, NJ, USA). Lyophilized SG and control ADC were dissolved in sterile 0.9% sodium chloride as a 2 μm stock solution for the in vitro experiments. Drug‐to‐antibody ratio (DAR) of SG and control ADC was 6.78 and 6.84, respectively. For the in vitro experiments, the dosage of the drug was adjusted according to the DAR, in order to expose cells treated with SG and control ADC to equivalent quantities of SN‐38. For in vivo experiments, SG and the control ADC were reconstituted in sterile 0.9% sodium chloride as a 5 mg·mL−1 solution. hRS7 IgG (molecular weight: 150 kDa) was obtained in liquid form from Immunomedics, Inc., as a 10 mg·mL−1 solution.
2.5. Antibody‐dependent cellular cytotoxicity (ADCC)
Standard 4‐h chromium (51Cr) release assays were performed in order to measure the cytotoxic reactivity of Ficoll–Hypaque‐separated peripheral blood lymphocytes (PBLs), in combination with the drug SG, the control ADC, and the hRS7 IgG against the EC cell lines at an effector to target ratio (E : T) of 5 : 1 and 10 : 1. The release of 51Cr from target cells was measured as evidence of tumor cell lysis after exposure of the tumor cells to a concentration of 2.5 µg·mL−1 of SG, the control ADC, or hRS7 IgG. Negative controls for this experiment included tumor cells incubated with PBLs and no ADCs. The positive control condition included 1% SDS to achieve complete lysis of target cells. Chimeric anti‐CD20 mAb rituxan (2.5 μg·mL−1) was used in all bioassays as a negative control for hRS7 IgG. The release of 51Cr by cytolysis from the target cells was counted in a gamma radiation counter (2470 WIZARD2 Automatic Gamma Counter; PerkinElmer, Waltham, MA, USA). The percentage cytotoxicity of SG, the control ADC, or hRS7 IgG was calculated by the following formula: % cytotoxicity = 100 × (E − S)/(T − S), where E is the experimental release, S is the spontaneous release by target cells, and T is the maximum release by target cells lysed with 0.1% SDS. The results were reported as mean ± SEM.
2.6. Flow cytometry‐based cytotoxicity
Each of the EC cell lines tested was plated at a density of 30 000–80 000 cells/well in six‐well tissue culture plates with RPMI 1640 media supplemented with 10% FBS, 1% amphotericin, and 1% penicillin/streptomycin. Cells were incubated at 37 °C and 5% CO2 for 24 h after which they were treated with SG, the control ADC, and hRS7 IgG at the following concentrations of 0.2, 0.5, 1, 2, 4 nm. The concentration of the control ADC was adjusted based upon its DAR to assure the EC cells were treated with an equal amount of SN‐38. Cells were exposed to the drugs for 10 h before being washed with culture medium to remove any unbound ADC or unconjugated mAb. Then, the six‐well plates were incubated for an additional 72 h after which the cells were harvested, centrifuged, and stained with propidium iodide (2 µL of 500 µg·mL−1 stock solution in PBS). The viable cells were then quantified using a flow cytometry‐based assay that has been previously characterized (Roque et al., 2014). A minimum of three independent experiments per cell line were performed in order to determine the IC50’s of SG, the control ADC, and hRS7 IgG in EC cell lines.
2.7. Bystander effect
ARK4, a Trop‐2‐negative uterine serous cell line stably transfected with a green fluorescence protein (GFP) plasmid (pCDH‐CMV‐MCSEF1‐copGFP, a gift from Simona Colla, MDACC) was plated (80 000 cells/well) alone in a 6‐well plate (2 mL per well). A 1 : 1 ratio of this ARK4 cell line stably transfected with GFP was admixed with END(K)265, a 3+ Trop‐2 expressing EC cell line, and then plated in a 6‐well plate (2 mL per well). After overnight incubation, cells were treated with either SG or the control ADC at a concentration of 1 nm for 10 h. Cells were then washed to remove unbound conjugate, and after additional 72 h, cells were collected, centrifuged, and stained with propidium iodide (2 µL of 500 µg·mL−1 stock solution in PBS) to identify the percentage of live versus dead cells that were present in each well. The bystander effect was assessed by comparing the percentage of live Trop‐2‐negative cells (GFP‐ARK4) when they were cocultured with Trop‐2‐positive cells (ARK2) and treated with either SG versus the control ADC.
2.8. In vivo testing
The in vivo antitumor activity of SG, the control ADC, and hRS7 IgG was tested in xenograft models using the Trop‐2 + END(K)265 cell line, a grade 3 EC with mixed endometrioid and clear cell histology. Each mouse (female, of age 5–8 weeks old with severe combined immunodeficiency (SCID); ENVIGO, Indianapolis, IN, USA) received a subcutaneous injection of 14 million END(K)265 cells suspended in 300 µL of a 1 : 1 solution of sterile PBS containing cells and Matrigel® (BD Biosciences). When a tumor volume of 0.3 cm3 was obtained, the mice were then randomized into four groups (six mice/group): saline control, SG, control ADC, and hRS7 IgG. SG, the control ADC, and hRS7 IgG were given at a dose of 500 μg in 100 μL IV twice per week for three weeks by retro‐orbital and/or tail vein injection. Tumor volume was measured twice weekly using Vernier calipers. Determination of tumor volume was obtained using the formula (A 2 × B)/2, where B represented the largest tumor diameter size and A was the smallest perpendicular tumor diameter. The mice were subsequently euthanized when the group's average tumor volume reached 1.5 cm3. All animal care and euthanasia were carried out according to the regulations and rules established by the Institutional Animal Care and Use Committee (IACUC), which are in accordance with National Institutes of Health Guide for the Care and Use of Laboratory Animals.
2.9. Statistical analysis
Statistical analysis and IC50 extrapolations were performed using graphpad prism 8 (GraphPad Software, Inc. San Diego, CA, USA). Five drug concentration points were used for the calculation of IC50 in agreement with the previous literature (Turner and Charlton, 2005). The differences in the inhibition of proliferation in the EC cell lines as a result of exposure to the various treatments were evaluated using two‐tailed unpaired Student's t‐test. The differences in tumor volumes at specific time points were compared using an unpaired t‐test. Overall survival data were analyzed using the Kaplan–Meier method, and survival curves were compared using the log‐rank test. A two‐sided P‐value < 0.05 was considered to be statistically significant.
3. Results
3.1. Determination of Trop‐2 expression in EC patient samples by TMA
Semiquantitative analysis of Trop‐2 expression by immunohistochemistry (IHC) was performed using a TMA containing 143 EC patient samples. Moderate‐to‐strong (score 2–3) Trop‐2 expression was found in 84% (120/143) of these tumors (Fig. 1A and Table 1). In Fig. 1B, representative IHC images are presented.
Figure 1.
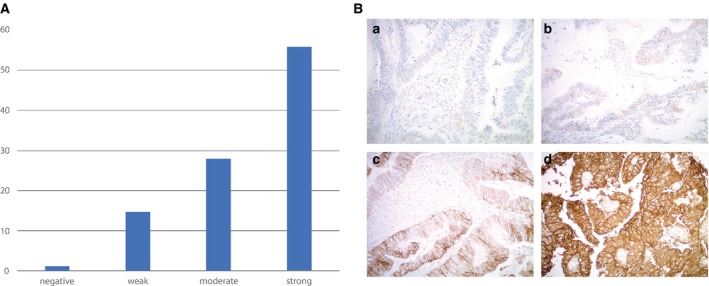
(A) Tissue microarray of 143 endometrioid EC samples. (B) Representative IHC images from the tissue microarray: (A) no Trop‐2 immunostaining (score 0), (B) weak focal (score 1), (C) moderate focal (score 2), and (D) strong diffuse (score 3) Trop‐2 expression. All images at 200× original magnification.
Table 1.
Semi‐quantitative analysis of Trop‐2 expression by IHC.
| TROP‐2 expression | Count | % |
|---|---|---|
| Negative | 2 | 1.3 |
| Weak | 21 | 14.7 |
| Moderate | 40 | 28 |
| Strong | 80 | 56 |
| total | 143 | 100.0 |
3.2. Determination of Trop‐2 expression in primary EC cell lines by flow cytometry
The expression of Trop‐2 was evaluated in seven primary EC cell lines. Table 2 demonstrates the clinicopathologic data of the patients from which these primary EC cell lines were established, which includes the cancer histology, stage, and grade clinic–pathologic and primary site of the tumors. With the use of flow cytometric analysis, three out of seven (43%) of the EC cell lines were found to have 3+ Trop‐2 expression (Table 2). Figure 2 demonstrates the flow cytometric analysis of the seven primary EC cell lines comparing those cell lines with 3+ Trop‐2 expression (i.e., END(K)254, END(K) 82, END(K)265 cell lines) versus those with 0 Trop‐2 expression (i.e., END(K)283, END(K)361, END(K)181, and END(K)23).
Table 2.
Endometrial cancer cell lines with demographics, stage, histologic grade, primary site of tumor, MFI, and score for Trop‐2. MFI 0–20 = flow cytometry score 0; MFI 21–50 = flow cytometry score 1+; MFI 51–100 = flow cytometry score 2+; MFI > 100 = flow cytometry score 3+. International Federation of Gynecology and Obstetrics (FIGO) staging and grading.
| Endometrioid endometrial cancer cell lines | Flow cytometry score | ||||||
|---|---|---|---|---|---|---|---|
| Cell line | Age | Ethnicity | FIGO stage | Primary site | Histology | ∆TROP2 MFI | |
| END(K)23 | 66 | Black | IIIA | Endometrium | Endometrioid G3 | 0.0 | 0 |
| END(K)254 | 65 | White | IIIC | Endometrium | Endometrioid G3 | 1208.9 | 3+ |
| END(K)181 | 88 | White | II | Endometrium | Endometrioid G3 | 0.0 | 0 |
| END(K)82 | 58 | White | IIIC | Endometrium | Endometrioid G2\G3 | 450.2 | 3+ |
| END(K)283 | 70 | White | IIIC | Endometrium | Endometrioid G3 | 2.06 | 0 |
| END(K)265 | 50 | White | IIIA | Endometrium | Endometrioid G3\CC | 186.2 | 3+ |
| END(K)361 | 65 | white | Xa | Endometrium | Endometrioid G3 | 1.6 | 0 |
Tumor collected from surgical specimen after neoadjuvant chemotherapy treatment.
Figure 2.
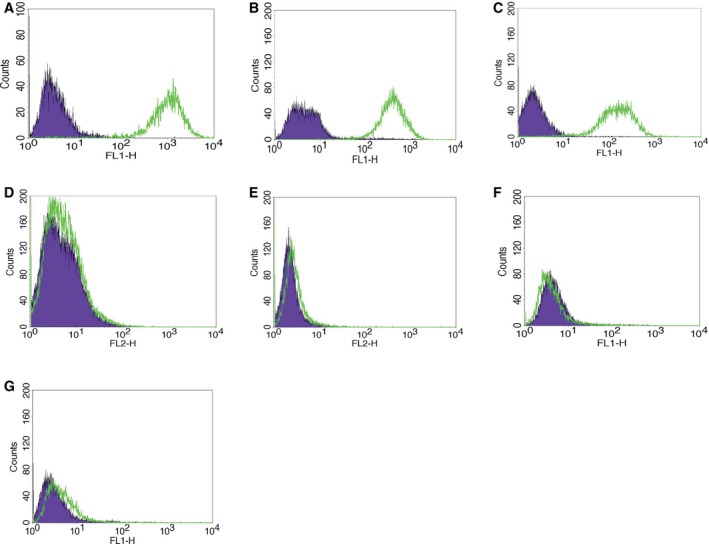
Representative flow cytometry histograms of the seven primary EC cell lines. (A) END(K)254, (B) END(K) 82, (C) END(K)265 cell lines demonstrating 3+ Trop‐2 expression and (D) END(K)283, (E) END(K)361, (F) END(K)181, and (G) END(K)23 cell lines demonstrating 0 Trop‐2 expression.
3.3. SG and hRS7 IgG mediate strong ADCC against Trop‐2‐positive primary EC
A Trop‐2‐positive cell line (i.e., END(K)265) and Trop‐2‐negative cell line (i.e., END(K)361) were both tested for their potential sensitivity to PBL‐mediated cytotoxicity using standard 4‐h 51Cr release assays. It was found that when both EC cell lines were combined with isotype control antibody (rituxan) (2 μg·mL−1) at E:T ratios of 5 : 1 and 10 : 1, they were resistant to PBL‐mediated cytotoxicity (Fig. 3). However, treatment with equivalent concentrations (2 μg·mL−1) of hRS7 IgG, SG, and the control ADC revealed that hRS7 IgG and SG were highly effective in inducing ADCC against primary EC cell lines expressing Trop‐2 at high levels (i.e., in the END(K)265 cell line) but the control ADC did not. As shown in Fig. 3A, at E:T ratios of 5 : 1 and 10 : 1, a mean cytotoxicity ± SEM = 12.3 ± 3.1% for SG and 19.7 ± 5.4% for hRS7‐IgG was determined, respectively, while low/negligible killing (i.e., 0.5 ± 0.03%) was induced by control ADC (P < 0.001 at 5 : 1 and 10 : 1 ratio, Fig. 3A). In contrast, there was no significant ADCC against the Trop‐2‐negative cell line END(K)361 after treatment with hRS7 IgG, SG, and the control ADC (Fig. 3B).
Figure 3.
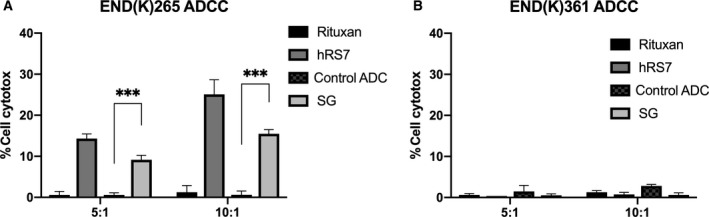
Antibody‐dependent cellular cytotoxicity results (mean ± SEM) of SG, control ADC, hRS7 IgG, and rituximab (anti‐CD20) in two representative EC cell lines [i.e., (A) END(K)265 3+ Trop‐2 cell line vs (B) END(K)361 Trop‐2‐ cell line] in the presence of PBL. Significant ADCC was detectable only against the Trop‐2 + tumors (P < 0.001).
3.4. In vitro viability assays with SG, the control ADC, and hRS7 IgG in primary EC cell lines
Subsequently, three primary EC cell lines (two were Trop‐2‐positive and one was Trop‐2‐negative) were treated with scalar concentrations of SG, the control ADC, and hRS7 IgG. There was a significant increase in cell cytotoxicity induced against Trop‐2‐positive EC cell lines treated with SG (i.e., a 2.7‐fold, 4.9‐fold increase against END(K)265 and END(K)254, respectively) than that of those treated by the control ADC (P = 0.014 and P = 0.005, respectively) (Fig. 4A,B). In contrast, no differences were found in Trop‐2‐negative END(K)361 EC cell lines (P = 0.3) (Fig. 4C). In the absence of PBL, the IC50 of hRS7 IgG was extrapolated using the statistical software of graphpad prism 8 to be greater than 40‐fold higher than IC50 of SG for all cell lines (data not shown).
Figure 4.
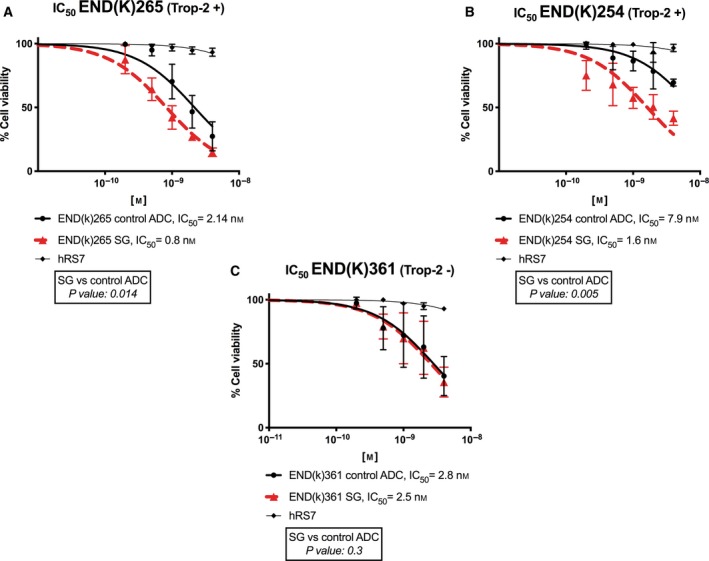
Determination of SG, control ADC, and hRS7 IgG IC50 (mean ± SEM) in primary EC cell lines. (A, B) EC cell lines with high Trop‐2 expression (3+) (i.e., END(K)265, END(K)254) demonstrated significantly lower IC50 when compared to control ADC (P < 0.05). (C) EC cell line with low/negligible Trop‐2 expression (i.e., END(K)361) showed no difference in the IC50s of SG and control ADC. hRS7 IgG antibody was inactive against all cell line tested. A minimum of three experiments for each cell line were performed.
3.5. Bystander effect in vitro
In order to evaluate the potential of SG to mediate a bystander killing effect toward EC cell lines with heterogeneous Trop‐2 expression, we admixed cells with high Trop‐2 expression (i.e., END(K)265 cells) and those with low or negligible Trop‐2 expression (i.e., GFP‐ARK4 cells) for 72 h. As shown in Fig. 5, there was a significant increase in the cytotoxicity of ARK4 cells when ARK4 and END(K)265 were cultured together and treated with SG when compared to ADC control‐treated cocultures (Fig. 5, P = 0.001).
Figure 5.
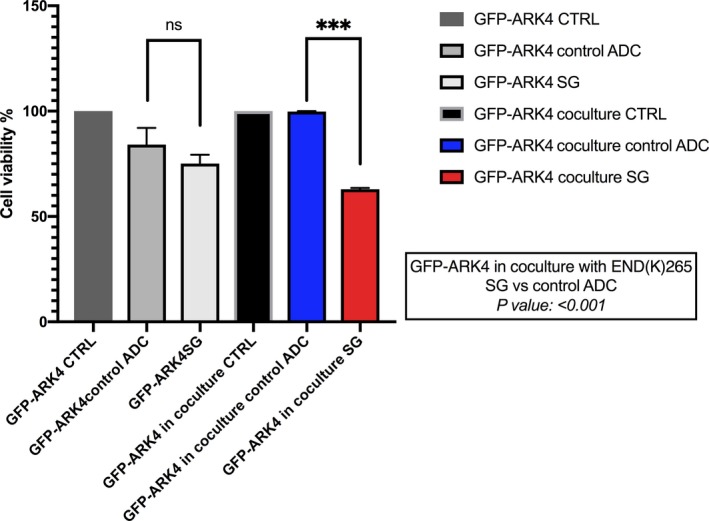
Bystander assay. Black bar: low/negative Trop‐2 expressing ARK4 cells (GFP‐ARK4 cells), cocultured with END(K)265 (i.e., 3+ Trop‐2) without treatment. Blue bar: low Trop‐2 expressing cells (GFP‐ARK4) cocultured with high Trop‐2 expressing cells (END(K)265) and treated with control ADC at 1 nm concentration. Red bar: low Trop‐2 expressing cells (GFP‐ARK4) cocultured with high Trop‐2 expressing cells (END(K)265) and treated with SG at 1 nm concentration. Significant increase in GFP‐ARK4 cell cytotoxicity was detected at the time of the co‐incubation with END(K)265 cells, when they were treated with SG (P < 0.05). Error bars indicate standard deviation (SD) throughout figure.
3.6. Antitumor activity of SG in the xenograft model
Due to the high Trop‐2 expression as well as the consistent engraftment of primary END(K)265 tumor cells in SCID mice, these xenograft models were chosen for the in vivo experiments comparing the potential antitumor activity of SG, the control ADC, hRS7 IgG, and saline. Within 4 days of therapy initiation (i.e., after only one injection), SG demonstrated a significant antitumor effect in these chemotherapy‐resistant tumors compared to all controls, including nonspecific ADC (Fig. 6A; P = 0.011). This SG‐mediated inhibition of tumor growth was evident at all subsequent time points up to day 15 when the control ADC animals were euthanized secondary to progression of disease, which was defined as a tumor volume greater than 1.5 cm3 (P < 0.01). This antitumor effect translated into a significant survival benefit for SG‐treated animals in comparison with all the controls (Fig. 6B; P < 0.05). Median survival for the SG group was 40 days versus 15 days for the control ADC, and 11 days for hRS7 IgG and saline (Fig. 6B). Overall, the mice tolerated the treatment well and there was no significant difference in the weight of the mice among all four groups (Fig. 6C).
Figure 6.
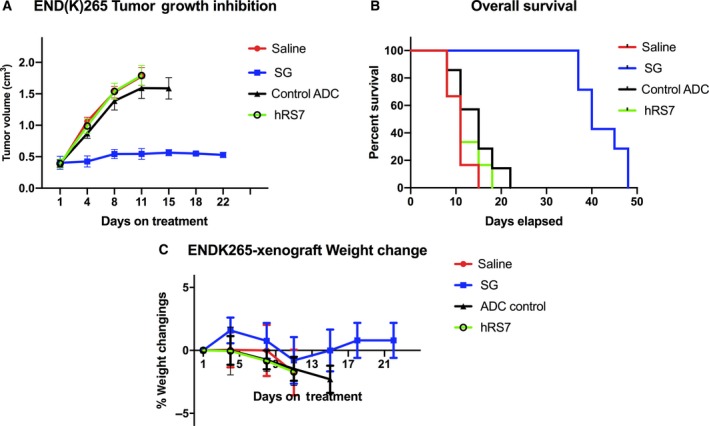
In vivo efficacy of SG: (A) antitumor activity and (B) overall survival of SG were compared to controls including control ADC, unconjugated mAb (hRS7 IgG), and saline, in EC xenograft models (i.e., END(K)265, 3+ Trop‐2‐positive). (C) Mice weight change during treatment. Mice were treated intravenously with twice‐weekly doses for 3 weeks as described in Methods. (A) A significant difference in tumor growth inhibition was detected beginning on day 4 (P < 0.05) in the SG‐treated group when compared to the other control groups. (B) Median survival for the SG group was 40 days, compared to 15 days for control ADC and 11 days for hRS7 and saline. Error bars indicate standard deviation (SD) in both (A) and (C).
4. Discussion
High expression of Trop‐2 has been discovered in a variety of human epithelial tumors including cervical, uterine, and ovarian cancers and confers tumor cells with an increased ability to proliferate and migrate (Bignotti et al., 2012; Liu et al., 2013; Santin et al., 2004; Varughese et al., 2011b; Xu et al., 2017). Importantly, as a result of its differential overexpression in tumor cells when compared to normal cells, Trop‐2 may represent an excellent target for targeted therapeutics such as ADCs.
Accordingly, in this study, we evaluated the level of Trop‐2 expression in 143 ECs and evaluated the potential cytotoxicity that treatment with SG may induce against multiple primary EC cell lines with different degrees of Trop‐2 expression. Moderate‐to‐strong Trop‐2 expression was found in 84% (120/143) of the EC samples evaluated by IHC and 43% of the primary EC cell lines assessed by flow cytometry. Importantly, we have shown Trop‐2‐positive EC cell lines to be highly sensitive to treatment with SG when compared to treatment with the control ADC and hRS7 IgG. In contrast, no differences were found in Trop‐2‐negative cell lines. These results demonstrate the need for Trop‐2 receptor expression on tumor cells for the induction of SG cytotoxic activity against EC.
Furthermore, we demonstrated that the mechanism by which SG induces tumor cell killing is not only due to the internalization of the ADC and the consequent intracellular release of the toxic payload SN‐38 but it may also be potentially mediated by immune system cells (i.e., NK cells). Indeed, both SG and hRS7 IgG demonstrated significant induction of ADCC toward Trop‐2‐positive EC cell lines in the presence of PBL, while the control ADC generated only a low level of cytotoxicity. The killing activity was Trop‐2‐specific as demonstrated by the negligible ADCC induced by SG against Trop‐2‐negative tumors. These findings support previous results from our group evaluating the activity of the unconjugated humanized anti‐Trop‐2 monoclonal antibody hRS7 in ovarian cancer (Bignotti et al., 2012; Trerotola et al., 2013; Varughese et al., 2011a).
EC is a heterogeneous disease, and accordingly, expression of Trop‐2, similarly to other surface markers, may not be uniformly expressed. Importantly, due to the cleavable hydrolyzable linker of SG the toxic payload, SN‐38 may be released in tumors both intracellularly and extracellularly in the tumor microenvironment. Therefore, this ultimately permits the delivery of a therapeutic concentration of the drug to surrounding cells, which were not the initial target of the ADC (Goldenberg et al., 2015). Consistent with this view, SG may kill Trop‐2‐positive tumor cells by intracellular intake of SN‐38, while neighboring cells (i.e., Trop‐2‐negative tumor and/or endothelial/stromal cells) may be killed by the extracellular release of SN‐38 (Goldenberg et al., 2015). To validate this hypothesis, we performed in vitro experiments admixing Trop‐2‐positive with Trop‐2‐negative tumor cells before exposing them to SG. We consistently found SG to induce killing against Trop‐2‐negative tumor cells but only when they were admixed with Trop‐2 overexpressing tumor cells. Overall, these results strongly support the fact that SG may also be effective in the treatment of patients with recurrent EC whose tumors often possess varying degrees of Trop‐2 expression.
Nonetheless, the in vivo experiments with Trop‐2‐positive EC xenografts established from a patient with a biologically aggressive tumor (i.e., mixed clear cell and G3 endometrioid histology) demonstrated that a few injections of SG were highly effective in inducing regression of EC xenografts. Indeed, twice‐weekly administration of SG demonstrated a statistically significant difference in tumor growth inhibition of END(K)265 when compared to administration of the control ADC. It was considered that a possible limitation in the use of SG in the clinical setting is its potential toxicity. Thus, it is important to note that there was no evidence of acute or chronic toxicity detected in the animals treated with SG for the entire duration of the study. These results are the first to demonstrate the efficacy and safety profile of the in vivo activity of SG against biologically aggressive and poorly differentiated EC. These findings warrant the support of the use of SG in clinic trials.
Consistent with our preclinical in vitro and in vivo results in biologically aggressive endometrial cancer, results from a phase I/II clinical study reported acceptable toxicity and encouraging therapeutic activity of SG against multiple recurrent human epithelial cancers including urothelial cancers and lung cancers (Bardia et al., 2019; Faltas et al., 2016; Gray et al., 2017; Heist et al., 2017; Starodub et al., 2015). Moreover, our group has recently reported an impressive clinical response to SG in a 74‐year‐old woman with recurrent/chemotherapy‐resistant endometrial serous tumor overexpressing Trop‐2 (66% reduction of target lesions by RECIST 1.1 criteria for over 10 months of follow‐up) (Han et al., 2018). Furthermore, other encouraging results of treatment with SG were previously described in a cohort of 108 heavily pretreated metastatic triple‐negative breast cancers. These patients had an objective response rate of 33.3%, median response duration of 7.7 months, and a clinical benefit rate of 45.4% (Bardia et al., 2019). As a result of these encouraging clinical findings in breast cancer patients, SG has received breakthrough therapy designation from the FDA for the treatment of TNBC patients with metastatic disease who have failed at least two prior therapies.
5. Conclusions
Trop‐2 overexpression is found in over 80% of EC, and our in vitro studies demonstrate that SG proves to be highly cytotoxic to these primary EC cell lines. Furthermore, SG induces significant ADCC against Trop‐2‐positive EC cells in the presence of effector cells (NK cells) but more uniquely SG demonstrates a significant bystander killing effect, which may aid in the treatment of tumors with heterogeneous antigen expression. Nonetheless, EC xenografts overexpressing Trop‐2 were found to be highly sensitive to treatment with SG. Our results combined with recent phase II data demonstrating significant clinical responses in tumors resistant to standard chemotherapy regimens support the implementation of clinical trials for patients with recurrent and poorly differentiated EC that harbor Trop‐2‐positive tumor expression.
Conflict of interest
All authors fulfill the conditions required for authorship. ADS declares research funding support to Institution from ImmunoMedics. AM declares that she receives research funding support from Spanish Medical Oncology Society.
Author contributions
ADS designed research; EP, SL, BZ, SB, AB, LZ, AM, EB, PM, NB, GA, CH, GM, ER, D‐AS, MA, JTR performed research; PES, GS contributed new reagents/analytic tools, ADS and EP wrote the paper.
References
- Ab O, Whiteman KR, Bartle LM, Sun X, Singh R, Tavares D, LaBelle A, Payne G, Lutz RJ, Pinkas J et al (2015) IMGN853, a folate receptor‐alpha (FRalpha)‐targeting antibody‐drug conjugate, exhibits potent targeted antitumor activity against FRalpha‐expressing tumors. Mol Cancer Ther 14, 1605–1613. [DOI] [PubMed] [Google Scholar]
- Altwerger G, Bonazzoli E, Bellone S, Egawa‐Takata T, Menderes G, Pettinella F, Bianchi A, Riccio F, Feinberg J, Zammataro L et al (2018) In vitro and in vivo activity of IMGN853, an antibody‐drug conjugate targeting folate receptor alpha linked to DM4, in biologically aggressive endometrial cancers. Mol Cancer Ther 17, 1003–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardia A, Mayer IA, Vahdat LT, Tolaney SM, Isakoff SJ, Diamond JR, O'Shaughnessy J, Moroose RL, Santin AD, Abramson VG et al (2019) Sacituzumab govitecan‐hziy in refractory metastatic triple‐negative breast cancer. N Engl J Med 380, 741–751. [DOI] [PubMed] [Google Scholar]
- Bignotti E, Zanotti L, Calza S, Falchetti M, Lonardi S, Ravaggi A, Romani C, Todeschini P, Bandiera E, Tassi RA et al (2012) Trop‐2 protein overexpression is an independent marker for predicting disease recurrence in endometrioid endometrial carcinoma. BMC Clin Pathol 12, 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bokhman JV (1983) Two pathogenetic types of endometrial carcinoma. Gynecol Oncol 15, 10–17. [DOI] [PubMed] [Google Scholar]
- Cardillo TM, Govindan SV, Sharkey RM, Trisal P, Arrojo R, Liu D, Rossi EA, Chang CH and Goldenberg DM (2015) Sacituzumab govitecan (IMMU‐132), an anti‐Trop‐2/SN‐38 antibody‐drug conjugate: characterization and efficacy in pancreatic, gastric, and other cancers. Bioconjug Chem 26, 919–931. [DOI] [PubMed] [Google Scholar]
- Creutzberg CL, van Putten WL, Warlam‐Rodenhuis CC, van den Bergh AC, de Winter KA, Koper PC, Lybeert ML, Slot A, Lutgens LC, Stenfert Kroese MC et al (2004) Outcome of high‐risk stage IC, grade 3, compared with stage I endometrial carcinoma patients: the postoperative radiation therapy in endometrial carcinoma trial. J Clin Oncol 22, 1234–1241. [DOI] [PubMed] [Google Scholar]
- El‐Sahwi K, Bellone S, Cocco E, Cargnelutti M, Casagrande F, Bellone M, Abu‐Khalaf M, Buza N, Tavassoli FA, Hui P et al (2010) In vitro activity of pertuzumab in combination with trastuzumab in uterine serous papillary adenocarcinoma. Br J Cancer 102, 134–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- English DP, Bellone S, Schwab CL, Bortolomai I, Bonazzoli E, Cocco E, Buza N, Hui P, Lopez S, Ratner E et al (2014) T‐DM1, a novel antibody‐drug conjugate, is highly effective against primary HER2 overexpressing uterine serous carcinoma in vitro and in vivo. Cancer Med 3, 1256–1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faltas B, Goldenberg DM, Ocean AJ, Govindan SV, Wilhelm F, Sharkey RM, Hajdenberg J, Hodes G, Nanus DM and Tagawa ST (2016) Sacituzumab govitecan, a novel antibody‐drug conjugate, in patients with metastatic platinum‐resistant urothelial carcinoma. Clin Genitourin Cancer 14, e75–e79. [DOI] [PubMed] [Google Scholar]
- Felix AS, Weissfeld JL, Stone RA, Bowser R, Chivukula M, Edwards RP and Linkov F (2010) Factors associated with type I and type II endometrial cancer. Cancer Causes Control 21, 1851–1856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldenberg DM, Cardillo TM, Govindan SV, Rossi EA and Sharkey RM (2015) Trop‐2 is a novel target for solid cancer therapy with sacituzumab govitecan (IMMU‐132), an antibody‐drug conjugate (ADC). Oncotarget 6, 22496–22512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray JE, Heist RS, Starodub AN, Camidge DR, Kio EA, Masters GA, Purcell WT, Guarino MJ, Misleh J, Schneider CJ et al (2017) Therapy of small cell lung cancer (SCLC) with a topoisomerase‐I‐inhibiting antibody‐drug conjugate (ADC) targeting trop‐2, sacituzumab govitecan. Clin Cancer Res 23, 5711–5719. [DOI] [PubMed] [Google Scholar]
- Han C, Bellone S, Schwartz PE, Govindan SV, Sharkey RM, Goldenberg DM and Santin AD (2018) Sacituzumab govitecan (IMMU‐132) in treatment‐resistant uterine serous carcinoma: a case report. Gynecol Oncol Rep 25, 37–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heist RS, Guarino MJ, Masters G, Purcell WT, Starodub AN, Horn L, Scheff RJ, Bardia A, Messersmith WA, Berlin J et al (2017) Therapy of advanced non‐small‐cell lung cancer with an SN‐38‐anti‐trop‐2 drug conjugate, sacituzumab govitecan. J Clin Oncol 35, 2790–2797. [DOI] [PubMed] [Google Scholar]
- Liu T, Liu Y, Bao X, Tian J, Liu Y and Yang X (2013) Overexpression of TROP2 predicts poor prognosis of patients with cervical cancer and promotes the proliferation and invasion of cervical cancer cells by regulating ERK signaling pathway. PLoS ONE 8, e75864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Xing H, Weng D, Song X, Qin X, Xia X, Weng Y, Liang F, Chen G, Han X et al (2009) Inhibition of Akt signaling by SN‐38 induces apoptosis in cervical cancer. Cancer Lett 274, 47–53. [DOI] [PubMed] [Google Scholar]
- Mathijssen RH, van Alphen RJ, Verweij J, Loos WJ, Nooter K, Stoter G and Sparreboom A (2001) Clinical pharmacokinetics and metabolism of irinotecan (CPT‐11). Clin Cancer Res 7, 2182–2194. [PubMed] [Google Scholar]
- Nicoletti R, Lopez S, Bellone S, Cocco E, Schwab CL, Black JD, Centritto F, Zhu L, Bonazzoli E, Buza N et al (2015) T‐DM1, a novel antibody‐drug conjugate, is highly effective against uterine and ovarian carcinosarcomas overexpressing HER2. Clin Exp Metastasis 32, 29–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roque DM, Buza N, Glasgow M, Bellone S, Bortolomai I, Gasparrini S, Cocco E, Ratner E, Silasi DA, Azodi M et al (2014) Class III beta‐tubulin overexpression within the tumor microenvironment is a prognostic biomarker for poor overall survival in ovarian cancer patients treated with neoadjuvant carboplatin/paclitaxel. Clin Exp Metastasis 31, 101–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose PG, Ali S, Moslemi‐Kebria M and Simpkins F (2017) Paclitaxel, carboplatin, and bevacizumab in advanced and recurrent endometrial carcinoma. Int J Gynecol Cancer 27, 452–458. [DOI] [PubMed] [Google Scholar]
- Santin AD, Zhan F, Bellone S, Palmieri M, Cane S, Bignotti E, Anfossi S, Gokden M, Dunn D, Roman JJ et al (2004) Gene expression profiles in primary ovarian serous papillary tumors and normal ovarian epithelium: identification of candidate molecular markers for ovarian cancer diagnosis and therapy. Int J Cancer 112, 14–25. [DOI] [PubMed] [Google Scholar]
- Siegel RL, Miller KD and Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin 69, 7–34. [DOI] [PubMed] [Google Scholar]
- Starodub AN, Ocean AJ, Shah MA, Guarino MJ, Picozzi VJ Jr, Vahdat LT, Thomas SS, Govindan SV, Maliakal PP, Wegener WA et al (2015) First‐in‐human trial of a novel anti‐trop‐2 antibody‐SN‐38 conjugate, sacituzumab govitecan, for the treatment of diverse metastatic solid tumors. Clin Cancer Res 21, 3870–3878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trerotola M, Cantanelli P, Guerra E, Tripaldi R, Aloisi AL, Bonasera V, Lattanzio R, de Lange R, Weidle UH, Piantelli M and et al (2013) Upregulation of Trop‐2 quantitatively stimulates human cancer growth. Oncogene 32, 222–233. [DOI] [PubMed] [Google Scholar]
- Tsimberidou AM (2015) Targeted therapy in cancer. Cancer Chemother Pharmacol 76, 1113–1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner RJ and Charlton SJ (2005) Assessing the minimum number of data points required for accurate IC50 determination. Assay Drug Dev Technol 3, 525–31. [DOI] [PubMed] [Google Scholar]
- Varughese J, Cocco E, Bellone S, Bellone M, Todeschini P, Carrara L, Schwartz PE, Rutherford TJ, Pecorelli S and Santin AD (2011a) High‐grade, chemotherapy‐resistant primary ovarian carcinoma cell lines overexpress human trophoblast cell‐surface marker (Trop‐2) and are highly sensitive to immunotherapy with hRS7, a humanized monoclonal anti‐Trop‐2 antibody. Gynecol Oncol 122, 171–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varughese J, Cocco E, Bellone S, Ratner E, Silasi DA, Azodi M, Schwartz PE, Rutherford TJ, Buza N, Pecorelli S and et al (2011b) Cervical carcinomas overexpress human trophoblast cell‐surface marker (Trop‐2) and are highly sensitive to immunotherapy with hRS7, a humanized monoclonal anti‐Trop‐2 antibody. Am J Obstet Gynecol 205, 567.e1–567.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Medical Association (2001) World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull World Health Org 79, 373–374. [PMC free article] [PubMed] [Google Scholar]
- Xu P, Zhao Y, Liu K, Lin S, Liu X, Wang M, Yang P, Tian T, Zhu YY and Dai Z (2017) Prognostic role and clinical significance of trophoblast cell surface antigen 2 in various carcinomas. Cancer Manag Res 9, 821–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young MR, Higgins SA, Ratner E, Yu JB, Mani S, Silasi DA, Azodi M, Rutherford T, Schwartz PE and Damast S (2015) Adjuvant carboplatin, paclitaxel, and vaginal cuff brachytherapy for stage III endometrial cancer: analysis of outcomes and patterns of recurrence based on pathologic characteristics. Int J Gynecol Cancer 25, 431–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao S, Choi M, Overton JD, Bellone S, Roque DM, Cocco E, Guzzo F, English DP, Varughese J, Gasparrini S et al (2013) Landscape of somatic single‐nucleotide and copy‐number mutations in uterine serous carcinoma. Proc Natl Acad Sci USA 110, 2916–2921. [DOI] [PMC free article] [PubMed] [Google Scholar]


