Abstract
Parenting children with neurodevelopmental disabilities is often challenging. Biological mothers of children with Fragile X Syndrome (FXS) may be susceptible to increased risk of mental health problems. This study examined the longitudinal relationships between maternal mental health, child challenging behaviors, and mother-child relationship quality in children and adolescents with FXS. Fifty-five mother-child dyads were followed from childhood into adolescence. The findings suggest that child challenging behaviors, maternal mental health, and mother-child relationship quality were stable during that period. Additionally, elevated levels of child challenging behaviors negatively impacted maternal mental health. Finally, child challenging behaviors, in combination with maternal mental health, influenced mother-child relationship quality. Clinical implications are discussed.
Keywords: Fragile X, Mental Health, Challenging Behaviors, Relationship Quality
Parenting a child with a neurodevelopmental disorder, particularly one that is associated with challenging behavioral needs and cognitive impairments, can be difficult. The stresses of raising such a child can strain the mother’s mental well-being and the quality of the relationship between the mother and child. In this study we examined the longitudinal relationships between child challenging behaviors, maternal mental health, and mother-child relationship quality in children and adolescents with Fragile X Syndrome (FXS). This population is particularly interesting because both mother and child are affected by the disorder. Mothers of children with FXS may have a genetic predisposition towards poorer mental health (Franke et al., 1996; Hunter, Rohr, & Sherman, 2010), and many children with FXS demonstrate increased challenging behaviors (Hardiman & McGill, 2018; Hatton et al., 2002). These symptoms may compound one another and negatively affect the quality of the relationship between the mother and child.
FXS is a heritable neurodevelopmental disorder that causes a broad range of developmental delays and impairments. It is the most common inherited cause of intellectual disability and the most common single gene disorder associated with autism (Cohen et al., 2005). FXS is caused by an abnormally high number of CGG repeats on the first exon of the FMR1 gene (Verkerk et al., 1991). This elongated sequence is located on the X chromosome and results in hypermethylation of the coding region, which leads to loss or reduction of protein production (Darnell, Warren, & Darnell, 2004). Individuals with fewer than 55 CGG repeats are typically unaffected by the disorder, although recent findings suggest a grey zone between 41 and 54 repeats (Debrey et al., 2016). Individuals who have between 55 and 199 repeats are considered to carry the premutation, and those with 200 or more repeats carry the full mutation. Because this premutation can be highly unstable, many women who carry the premutation have children with the full mutation. Both disorders, pre- and full mutation FXS, display unique profiles of impairment.
Premutation Fragile X Phenotype
Women who carry the premutation (pmFXS) are genetically predisposed to a variety of health concerns (Wheeler et al., 2014). Specifically, they have increased risk for FXS-associated Primary Ovarian Insufficiency (FXPOI), FXS-associated Tremor and Ataxia Syndrome (FXTAS), impairments in executive function, and increased rates of depression, anxiety, and ADHD (R. J. Hagerman & Hagerman, 2013; Hunter et al., 2010; Sullivan et al., 2005; Wheeler et al., 2014). Mothers of children with FXS may experience increased rates of anxiety compared to mothers of children with autism and mothers from the general population (Franke et al., 1996). Similarly, women with pmFXS may also experience elevated rates of anxiety, with 13% of pmFXS women reporting a diagnosis of anxiety compared to 6.4% of controls (Hunter et al., 2010). Premutation carrier mothers may also have higher rates of affective disorders than controls, with Franke et al. (1996) stating that 44.8% of pmFXS mothers reported a lifetime diagnosis of an affective disorder compared to 13.3% of control mothers. Finally, this may also be the case for depressive symptoms, with 25% women with pmFXS receiving a diagnosis of depression, compared to 15% of non-FXS controls (Hunter et al., 2010).
However, as suggested by Hunter et al. (2010), demographic factors such as age, income, and ethnicity, may account for differences between pmFXS and non-FXS groups. Furthermore, while mothers with pmFXS may be susceptible to higher rates of depression and anxiety than mothers of typically developing children, they seem to experience similar levels of anxiety and depression to mothers of children with autism or Down syndrome (Lewis, Abbeduto, Murphy, Richmond, Giles, Bruno, Schroeder, et al., 2006). Thus, maternal mental health may be impacted by factors beyond genetic susceptibility such as parenting stress or difficult socioeconomic circumstances.
Fragile X Phenotype
Children with FXS, especially boys, typically have cognitive impairments and language delays (Abbeduto, Brady, & Kover, 2007; Lewis, Abbeduto, Murphy, Richmond, Giles, Bruno, & Schroeder, 2006). Because the disorder is X-linked, boys and girls present with different profiles of strengths and abilities. Many boys with FXS demonstrate poor adaptive functioning and challenging behaviors, and most have a moderate-to-severe intellectual disability (P. J. Hagerman & Hagerman, 2004). Many boys with FXS also demonstrate high ADHD symptomology (for a review see Rinehart, Cornish, & Tonge, 2010). Girls are more variable in their adaptive functioning and may not demonstrate as severe symptoms. Roughly half of girls with FXS qualify as having an intellectual disability (P. J. Hagerman & Hagerman, 2004) and some demonstrate elevated ADHD symptomology (Rinehart et al., 2010). Girls with FXS may also have increased social anxiety (Mazzocco, Kates, Baumgardner, Freund, & Reiss, 1997). Finally, there is a high rate of comorbidity between FXS and autism spectrum disorders (ASD), with estimates suggesting as many as 60% of males and 14% of females with FXS meet diagnostic criteria for ASD (Klusek, Martin, & Losh, 2014).
Child Challenging Behaviors in FXS.
Children with FXS have elevated rates of challenging behaviors (Hardiman & McGill, 2018; Hatton et al., 2002). Although highly variable, Hatton and colleagues (2002) reported that 26–57% of their sample of young boys with FXS had clinically elevated scores in thought, social, attention, and total problem scales on the Childhood Behavior Checklist (CBCL; Achenbach & Rescorla, 2001). As many as 44.6% of males with FXS demonstrate self-injurious behaviors and 40.2% display aggressive behaviors (Hardiman & McGill, 2018). Additionally, 36.2% engage in destructive behaviors (Hardiman & McGill, 2018). Comparatively, as many as 14.2% of females with FXS demonstrate self-injurious behaviors and 13.9% demonstrate aggressive behaviors (Hardiman & McGill, 2018). Autism symptomology may include increased challenging behaviors.
Effects of Child Challenging Behaviors
Because of the varying severity of behavioral symptoms demonstrated by children with FXS, it is important to consider the child’s behavioral profile and the effect it may have on maternal mental health and family functioning in families with FXS. Mothers of children with FXS who must cope with challenging child behaviors may experience higher levels of parenting stress leading to mental health disorders. Alternately, mothers of children with FXS may be at increased genetic susceptibility to psychiatric symptoms, which may in turn reduce their ability to parent children with the behavioral challenges associated with FXS. Reduced maternal mental health, in combination with elevated child challenging behaviors, may negatively influence the reciprocated closeness between the mother and child. This compromised relationship quality could negatively impact family dynamics and the nurturing relationships between a mother and her child.
Maternal mental health.
Parenting stress from child challenging behaviors.
There may be explanations beyond biological susceptibility for potentially higher rates of affective and anxiety-related disorders in women with pmFXS. Mothers of children with FXS may be more susceptible to parenting stress due to the nature of their children’s disabilities and challenging behaviors, thereby impacting their mental health. Child challenging behaviors is strongly associated with variability in maternal depression over time in mothers of children with or without intellectual disability (Zeedyk & Blacher, 2017). Increased parenting stress due to parent’s ability to manage the child’s behaviors is associated with higher levels of child challenging behaviors and parental psychological problems (Johnston et al., 2003). Finally, unpredictable maladaptive behaviors in adult children with intellectual disabilities are associated with higher rates of maternal depression (Seltzer, Greenberg, & Krauss, 1995).
Specific to families with FXS, there are significant positive associations between child behavior problems, as assessed by the CBCL, and maternal stress, depression, anxiety, anger, and quality of life (Bailey, Sideris, Roberts, & Hatton, 2008). However, mother’s susceptibility to psychological distress and her ability to positively adapt to her children’s behavior problems may be highly individualistic. The variability in responses to stress suggest that some mothers are seemingly unaffected by heightened stress while a subset of mothers experience psychological symptoms at or above diagnostic cut offs (Bailey et al., 2008). Furthermore, child challenging behavior and maternal mental health may not be significantly related over time in families with FXS (Hauser, Kover, & Abbeduto, 2014). In fact, one study suggested that maternal depression decreases over time for mothers whose children have high levels of challenging behaviors (Hauser et al., 2014). This may be due to mothers acclimating to the child’s challenging behaviors or accessing additional resources that may be available to families with particularly challenging children. Consequently, the basis for the relationship over time between maternal mental health and child challenging behaviors in FXS may be complex with several sources of potential variability.
Genetic predisposition.
Maternal well-being may also be impacted by the interaction between child challenging behaviors and increased genetic susceptibility to mental health disorders (Wheeler et al., 2014). If mothers with pmFXS are at increased risk of mental health disorders, then they may experience more negative effects of parenting stress than mothers of children with challenging behaviors who do not have a genetic predisposition. In fact, mothers of children with FXS report more pessimism about their children’s future than mothers of children with Down syndrome, but less pessimism than mothers of children with autism (Abbeduto et al., 2004). Given the differential relationships between these groups of mothers of children with neurodevelopmental disorders, it seems that the genetic liability in FXS may contribute to pessimism. Beyond these findings, the role of maternal genetic susceptibility towards mental health disorders is not understood in the context of parenting children with FXS.
Mother-child relationship quality.
Mother-child relationship quality is a measure of reciprocated trust, respect, understanding, affection, and fairness between mother and child. Reciprocated emotional closeness is an important factor in nurturing relationships within the family unit. Studies of relationship quality in families with FXS report mixed results. Mothers of sons with FXS report lower mother-child relationship quality than mothers of children with Down syndrome, but higher relationship quality than mothers of children with autism (Abbeduto et al., 2004). Additionally, mothers of sons with FXS and autism report lower relationship quality than mothers of sons with FXS-only, potentially implicating elevated autism symptoms in reduced relationship quality (Abbeduto et al., 2004; Lewis, Abbeduto, Murphy, Richmond, Giles, Bruno, Schroeder, et al., 2006). Over time, child challenging behavior and maternal depression may be significant predictors of maternal feelings of closeness in relationship quality in families with FXS (Hauser et al., 2014). In fact, child challenging behaviors may be associated with and predict change in mother-child relationship quality above and beyond the influence of maternal depressive symptoms (Hauser et al., 2014). However, this finding needs further investigation given the unclear relationship between maternal mental health and child challenging behaviors. The impact of child challenging behaviors on mother-child relationship quality could become particularly pronounced as children move into puberty and adolescence, necessitating longitudinal investigation of these variables.
Longitudinal studies of relationship quality.
Relatively little is known about the longitudinal associations between maternal mental health, child challenging behaviors, and mother-child relationship quality in families with FXS. However, there is an extensive line of research that has focused on family adaptation and maternal well-being in families with children who have autism (Orsmond, Seltzer, Greenberg, & Krauss, 2006; Smith, Greenberg, Seltzer, & Hong, 2008). Literature on these associations in autism can inform studies of FXS, as autism is closely related to FXS. Smith and colleagues (2008) used a cross-lagged model to demonstrate that higher levels of mother-child relationship quality were associated with fewer internalizing and externalizing behavior problems 18 months later in adolescents and adults with ASD. They further demonstrated that externalizing behaviors had a reciprocal effect on mother-child relationship quality, such that higher levels of earlier externalizing behaviors were associated with lower levels of later mother-child relationship quality. These findings suggest there may be a cumulative effect of child behavior problems on mother-child relationship quality over time in families with ASD.
The cumulative effect of child challenging behaviors on relationship quality has not been sufficiently studied in FXS. The only other study to examine these associations longitudinally, examined the relationships between child challenging behaviors, maternal mental health, and mother-child reciprocated closeness in families with adolescents with FXS over the span of one year (Hauser et al., 2014). However, they were limited by their small (n = 18) and unrepresentative sample. Their study used data from paternal reports, excluding single mother households, and suggesting a certain level of co-parenting by a father. Accordingly, there is a need for continued study of this relationship in families with FXS.
Motivation and Research Questions
In the current study, we aimed to provide longitudinal evidence for the association between mother-child relationship quality, child challenging behaviors, and maternal mental health. We also aimed to better understand the role of maternal genetic susceptibility to mental health disorders by including maternal CGG repeat length as a control. Finally, we hoped to determine how maternal mental health symptoms interact with child behavior problems to impact mother-child relationship quality over time.
We asked the following questions:
How stable are mother-child relationship quality, maternal mental health, and child challenging behaviors in FXS?
What is the longitudinal relationship between maternal mental health and child challenging behaviors in children and adolescents with FXS and their mothers, controlling for maternal CGG repeat length?
Finally, what is the longitudinal relationship between mother-child relationship quality and child challenging behaviors in children and adolescents with FXS and their mothers, and is this relationship moderated by maternal mental health?
We predicted that mother-child relationship quality, maternal mental health, and child challenging behaviors would remain relatively stable over time, as previously suggested (Zeedyk & Blacher, 2017). Next, we hypothesized that child challenging behaviors and maternal mental health would be highly associated. Specifically, we hypothesized that fluctuations in maternal mental health would be predicted by child challenging behaviors beyond maternal genetic susceptibility, such that mothers would report poorer mental health when their children were exhibiting higher levels of challenging behaviors. Finally, we expected that maternal mental health and child challenging behaviors would influence mother-child relationship quality both separately and together, such that maternal mental health may intensify the effect of child challenging behaviors on relationship quality.
Methods
Participants
Participants came from an ongoing longitudinal study at the University of Kansas (PIs: Steve Warren and Nancy Brady) examining the effects of parenting on development in children with FXS. Fifty-five children with full-mutation FXS (11 females) and their biological mothers were visited in their homes multiple times beginning in 2003 (see Warren, Brady, Sterling, Fleming, & Marquis, 2010). Data for this study come from three occasions. The first, Time 1, was the last childhood home-visit. Time 2 data was collected remotely through mail and occurred when the children were entering adolescence. Time 3 data come from the most recent home-visit, when the children were well into adolescence. At Time 1 children were on average 109.60 months old, ranging from 88 to 122 (+/− 9.39). At Time 2 the children were on average 163.34 months (range: 134–184, +/− 14.01), and at Time 3 they were on average 191.16 months (range: 160–216, +/− 12.23). See Table 1 for child characteristics. The participants were recruited from across the United States and represent a sample of convenience. The sample shows substantial variance on socioeconomic status, race, and maternal education, see Table 1.
Table 1:
Demographic Characteristics from Time 3 Visit
| Construct | Level | Percent |
|---|---|---|
| Child Race | ||
| Native Hawaiian or Other Pacific Islander | 2.22% | |
| Mother Race | ||
| Native Hawaiian or Other Pacific Islander | 2.22% | |
| Child Ethnicity | ||
| Hispanic | 6.67% | |
| Mother Ethnicity | ||
| Hispanic | 6.67% | |
| Mother Education | ||
| Professional or 2 Master’s Degree(s) | 9.09% | |
| Mother Marital Status | ||
| Engaged | 2.27% | |
| Household Income | ||
| > $100,000 | 59.09% |
Note. Mothers could indicate more than one category for Mother and Child race.
Mother Characteristics.
Maternal age at Time 1 ranged from 27 to 48 years, with a mean of 40.21 (+/− 4.72). At Time 2, they were between 33 and 53 years (mean = 45.54, S = 4.48), and at Time 3 they were between 36 and 55 years (mean = 46.94, SD = 4.33). Three mothers carried the full mutation, three had mosaicism for premutation and full mutation, and the remaining 49 mothers carried the premutation. Their carrier statuses were confirmed by genetic testing from blood collection. CGG repeat length from blood testing was our measure of genetic predisposition. We used the Wechsler Adult Intelligence Scale (Wechsler, 1997) to measure maternal cognitive ability. This measure was collected at the first visit upon entry into the study but was not repeatedly collected. At Time 3, twelve mothers were taking prescription anti-depressant and/or anti-anxiety medications. Maternal medication use was not collected at Times 1 and 2.
Procedure
At each home visit the child completed a battery of standardized assessments of language and cognition with a trained examiner while the mother completed questionnaires and interviews with another examiner. For Time 2, the remote data collection visit, all data were obtained from questionnaires and forms that were mailed to the family. All assessments were scored by trained examiners, and then double-scored to ensure accuracy.
Measures
Positive Affect Index (PAI; Bengtson & Schrader, 1982).
The PAI was our primary outcome measure. The PAI was developed as a measure of reciprocated closeness between parents and their adult children. This measure has been shown to be a reliable measure of mother-child relationship quality in a variety of populations, including adults and adolescents with ASD (Orsmond et al., 2006; Smith et al., 2008) and adults with schizophrenia, ASD, or Down syndrome (Greenberg, Seltzer, Krauss, Chou, & Hong, 2004). The PAI measures inter-generational relationship quality, also described as mother-child closeness, by assessing trust, affection, respect, fairness, and understanding between the mother and child. This 10-item survey includes five items that ask the mother how she feels towards her child and five items that ask the mother how she perceives her child feels towards her. Each item has a Likert-scale response space between 1 and 6, with 1 indicating lower levels of closeness and 6 indicating higher levels of closeness. The mothers each completed this questionnaire with respect to their feelings currently and in the past week.
Childhood Behavior Checklist (CBCL; Achenbach & Rescorla, 2001).
The CBCL was used to measure the level of child challenging behaviors. The mother completed this form at each time point, indicating the presence and frequency of challenging behaviors. The 112 items comprise several different subscales, including internalizing behaviors (anxious/depressed, withdrawn/depressed, thought, and social problems) and externalizing behaviors (hyperactivity, aggressive, rule-breaking behaviors). The mothers each completed this questionnaire with respect to their feelings currently and in the past week. The total raw score on this assessment represents the number of challenging behaviors that the child demonstrated as well as the frequency and intensity of these behaviors. Children whose raw scores are above 48 when they are younger than 12 years of age and adolescents whose raw scores are above 51 fall into the clinically significant range (Achenbach & Rescorla, 2001).
We used the total raw score rather than a standardized score because we were interested in how the children’s behavior problems varied over time. Using the standardized score does not allow for that level of detail, as it conflates raw score and age. Additionally, the total raw score indicates the day-to-day experiences of the mother while parenting her child and managing their behaviors. Because we were interested in the number of challenging behaviors, rather than the specific types, we did not examine internalizing versus externalizing behaviors, nor did we examine any subscales of the CBCL. Internal consistency for the total problems score on the CBCL is high, with alpha equal to 0.97 (Achenbach & Rescorla, 2001).
Center for Epidemiological Studies Depression Scale (CES-D; Radloff, 1977).
The CES-D was our measure of maternal depressive symptoms. This questionnaire required the mothers to rate how often they experienced certain depressive symptoms in the past week. The scale includes 20 items, each rated from 0 to 3. Lower scores indicate fewer depressive symptoms, and scores of 16 or higher suggest clinically significant symptoms of depression. Internal consistency is acceptable, with alpha equal to 0.82 (Lewinsohn, Seeley, Roberts, & Allen, 1997).
Profile of Mood States (POMS; McNair, Lorr, & Droppleman, 1971).
We used the Profile of Mood States Tension/Anxiety and Anger/Hostility forms to measure maternal anxiety and anger. This form requires the mothers to rate their feelings of anxiety or anger in the past week on a scale from 1 to 5, where 5 indicates higher feelings of anxiety or anger. Of the 21 items, 9 comprise the Tension/Anxiety scale and the remaining 12 form the Anger/Hostility scale. The internal consistency is adequate for the Tension/Anxiety scale, with alpha equal to 0.67, and high for Anger/Hostility, with alpha equal to 0.92 (Curran, Andrykowski, & Studts, 1995).
Analyses
Multilevel modeling was conducted using the PROC MIXED procedure in SAS software, version 9.4 of the SAS System for Windows (SAS Institute Inc., 2013) We used residual maximum likelihood estimation (REML). Significance tests of fixed effects were examined using multivariate Wald tests with Satterthwaite denominator degrees of freedom. As recommended by Hoffman (2015), the models were built based on the research questions and the consideration of control variables and predictors. Thus, control variables, namely maternal CGG repeat length, IQ, and medication use were entered first, followed by the predictors of interest (mental health measures and child challenging behaviors). The models predicting maternal mental health from child challenging behaviors first included maternal control variables, and then level-1 and level-2 child challenging behaviors. Finally, the models predicting mother-child relationship quality first included maternal control variables, then child challenging behaviors, maternal mental health, and moderation effects at each level.
Results
Descriptive and Correlational Information
Descriptive statistics for all variables are shown in Table 2. Mother-Child relationship quality score, measured from the PAI, ranged from 39 to 60 at Times 1 and 2, and from 36 to 60 at Time 3. Average reported relationship quality at all three occasions suggested high levels of endorsed mother-child reciprocated closeness. Maternal mental health measures, including the POMS tension/anxiety and anger/hostility scales and the CES-D demonstrated considerable variability. Although the overall averages were low, suggesting few symptoms of poor mental health, each measure had a wide range and relatively large standard deviations. Child challenging behaviors were also highly variable, with scores ranging from zero to 86, two to 92, and five to 82 at each occasion, respectively. The average levels of challenging behaviors suggest that children demonstrated moderate levels of these behaviors with relatively highly variability between children. A trend across all variables suggested declines in symptom severity except for mother-child relationship quality, which increased slightly at the Time 3.
Table 2:
Mother and Child Characteristics
| Variable | Time | N | Mean | Std Dev | Range |
|---|---|---|---|---|---|
| Mother Age (years) | |||||
| 3 | 44 | 46.94 | 4.33 | 36–55 | |
| Child Age (months) | |||||
| 3 | 44 | 191.16 | 12.23 | 160–216 | |
| CBCL Total Problems Raw Score | |||||
| 3 | 43 | 33.33 | 18.46 | 5–82 | |
| Relationship Quality (PAI) Total Score | |||||
| 3 | 38 | 52.57 | 5.54 | 36–60 | |
| POMS Anger/Hostility Score | |||||
| 3 | 43 | 4.38 | 4.22 | 0–18 | |
| POMS Tension/Anxiety Score | |||||
| 3 | 43 | 7.05 | 5.21 | 0–20 | |
| CES-D Depression Score | |||||
| 3 | 43 | 7.00 | 6.89 | 0–29 | |
| Maternal IQ | 55 | 107.75 | 14.01 | 55–130 |
Note. CBCL = Child Behavior Checklist; PAI = Positive Affect Index; POMS = Profile of Mood States; CES-D = Center for Epidemiological Studies Depression Scale.
Child challenging behaviors were significantly and positively correlated with all three maternal mental health measures (r = .41 to .48, p < 0.01), suggesting that higher levels of child challenging behaviors were associated with higher levels of maternal mental health problems. Child challenging behaviors were significantly and negatively correlated with mother-child relationship quality (r = −0.48, p < 0.01), suggesting that higher levels of these behaviors were associated with lower mother-child relationship quality. These relationships remained when controlling for maternal CGG repeat length, maternal IQ, child sex, and child age. Maternal CGG repeat length was significantly and negatively correlated with child challenging behaviors (r = −0.25, p < 0.01) and all three maternal mental health measures (r = −0.26 to −0.33, p < 0.01) and was significantly and positively correlated with mother-child relationship quality. This suggests that mothers with higher CGG repeat lengths experienced more depressive, anxious, and angry feelings, but that they also reported higher mother-child relationship quality. Correlations are provided in Table 3.
Table 3:
Correlations Between Variables
| CBCL | PAI | A/H | T/A | CES-D | IQ | CGG | Sex | |
|---|---|---|---|---|---|---|---|---|
| CBCL Total Problems | 1 | |||||||
| Positive Affect Index | −0.48* | 1 | ||||||
| POMS Anger/Hostility | 0.46* | −0.44* | 1 | |||||
| POMS Tension/Anxiety | 0.48* | −0.37* | 0.60* | 1 | ||||
| CES-D Depression | 0.41* | −0.43* | 0.57* | 0.63* | 1 | |||
| Maternal IQ | 0.06 | −0.04 | 0.10 | 0.09 | 0.07 | 1 | ||
| Maternal CGG Repeat Length | −0.25* | 0.24* | −0.26* | −0.33* | −0.27* | −0.31* | 1 | |
| Child Sex | −0.10 | 0.06 | −0.03 | −0.15 | −0.00 | 0.07 | 0.36* | 1 |
Note. CBCL = Child Behavior Checklist; PAI = Positive Affect Index; POMS = Profile of Mood States; CES-D = Center for Epidemiological Studies Depression Scale;
p < 0.01
Stability of Variables Over Time
We examined the relative stability of child challenging behaviors, mother-child relationship quality, and maternal mental health over time in multiple ways. First, we created and visually inspected observed growth trajectory plots, (see Figures 1 to 5). Then, we performed single regressions using time to predict each variable. We used child age in months as our metric of time. Finally, we conducted repeated-measures analysis of variances with post-hoc tests to determine the mean differences between occasions for each variable.
Fig. 1:
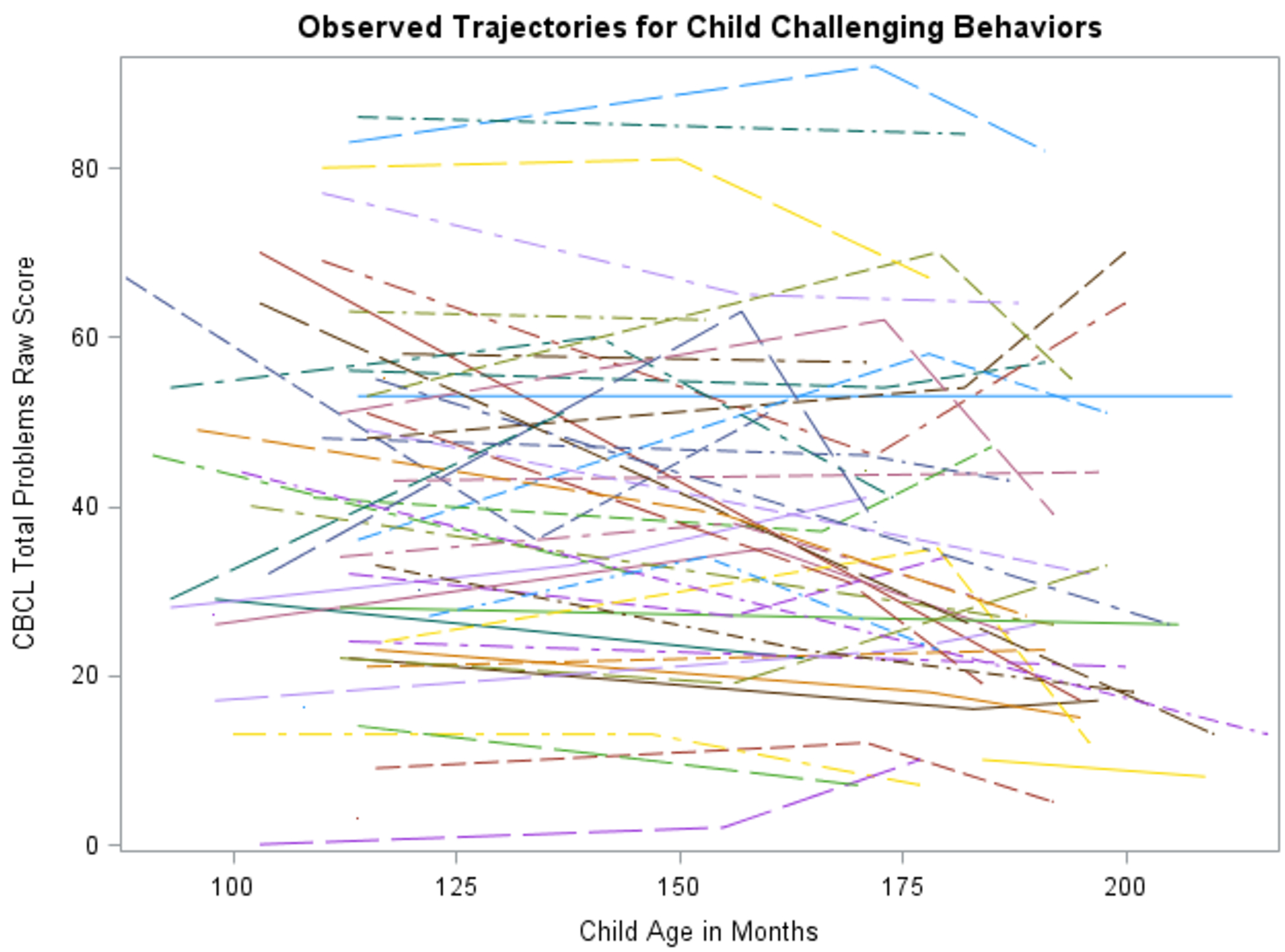
Observed Growth Trajectories for Child Challenging Behaviors
Fig. 5:
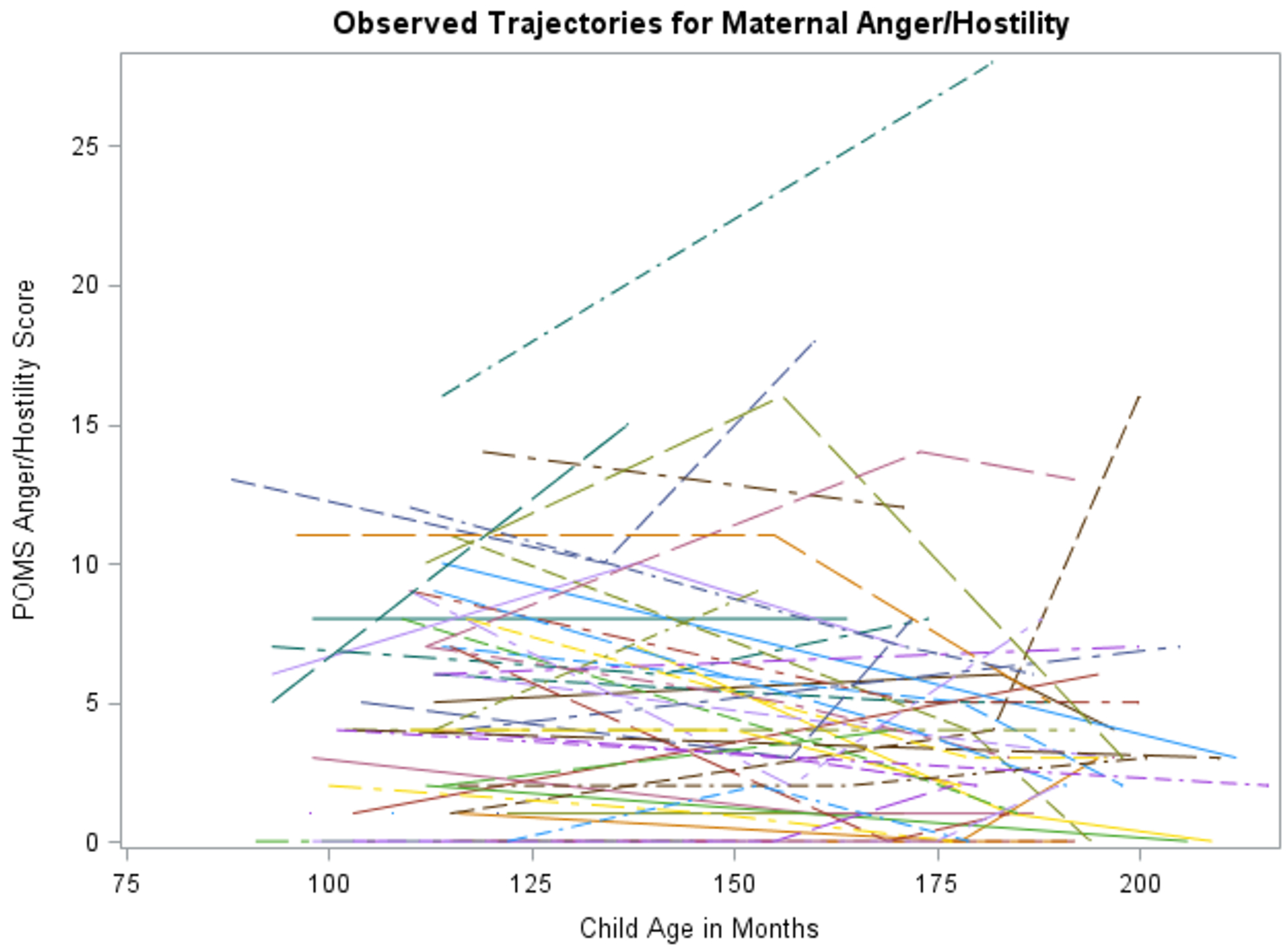
Observed Growth Trajectories for Maternal Anger/Hostility
Child challenging behaviors.
Visual inspection of child challenging behaviors suggested high levels of between-person variation and moderate within-person variation, see Figure 1. A regression predicting challenging behaviors from child age in months revealed a significant effect of time (t = −3.93, p < 0.01). Child challenging behaviors decreased by 0.07 points on average for every month the child aged. The repeated-measured ANOVA also revealed a significant effect of time, F(2,42) = 4.87, p = 0.01. Post-hoc tests revealed significant mean differences between Time 1 and 3 (t = 2.93, p = 0.01) and Time 2 and 3 (t = 2.62, p = 0.01), but not between Time 1 and 2 (t = 0.54, p = 0.59). Thus, child challenging behaviors decreased significantly over time.
Mother-child relationship quality.
Visual inspection of mother-child relationship quality suggested moderate levels of between-person variation and moderate within-person variation, see Figure 2. A regression predicting relationship quality from child age in months revealed no significant effect of time (t = 1.73, p = 0.09). The repeated-measured ANOVA also revealed no significant effect of time, F(2,42) = 1.96, p = 0.16. Post-hoc tests revealed a marginally significant mean difference between Time 1 and 3 (t = −1.95, p = 0.06). There was no significant mean difference between Time 2 and 3 (t = −1.47, p = 0.15), nor between Time 1 and 2 (t = −0.69, p = 0.50). Relationship quality appeared to be stable over time.
Fig. 2:
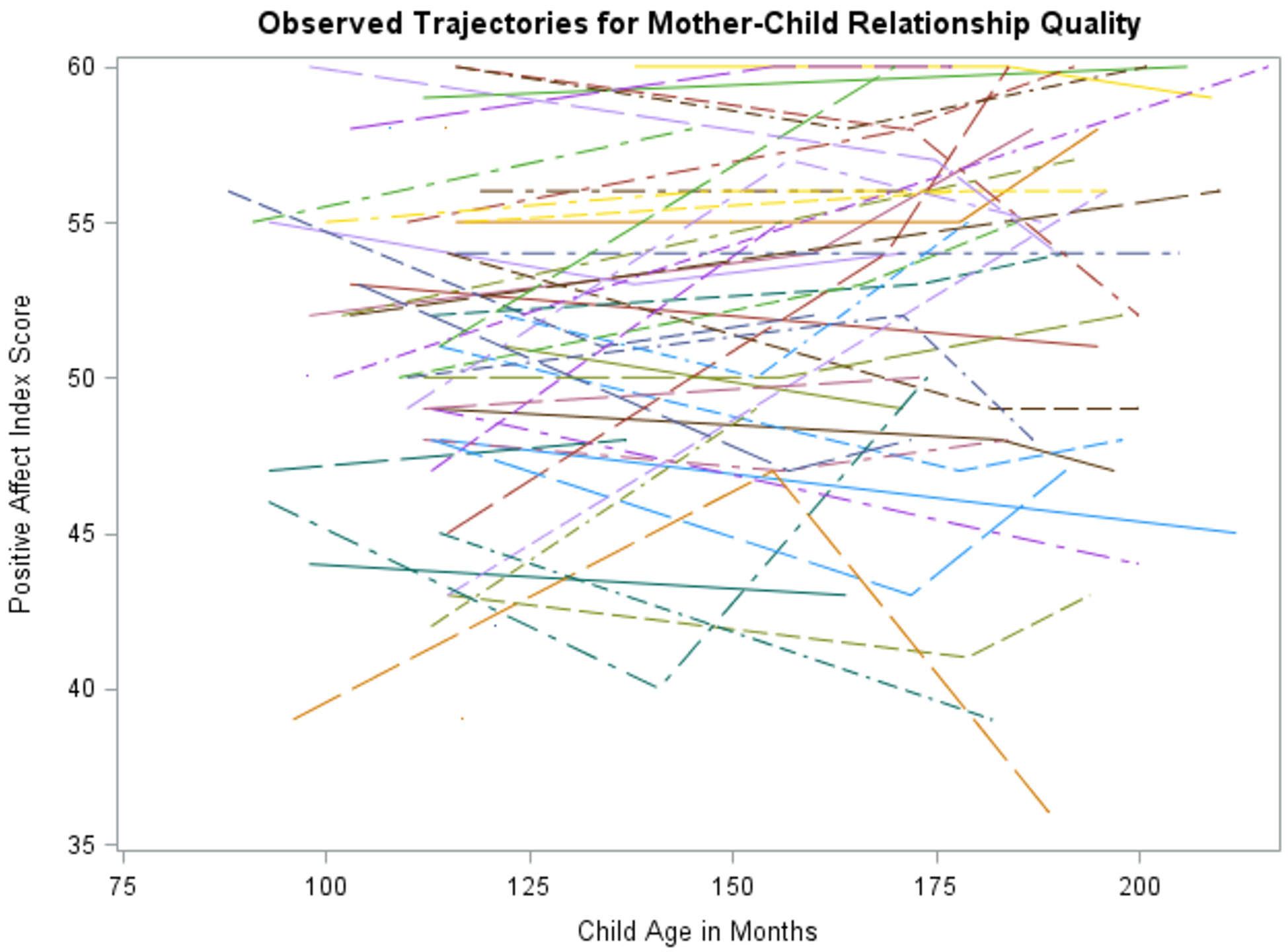
Observed Growth Trajectories for Mother-Child Relationship Quality
Maternal mental health: depression.
Visual inspection of maternal depression suggested high levels of between-person variation and marked within-person variation, see Figure 3. A regression predicting maternal depression from child age in months revealed no significant effect of time (t = −1.58, p = 0.12). The repeated-measured ANOVA also revealed no significant effect of time, F(2,42) = 1.08, p = 0.35. Post-hoc tests indicated no significant mean differences between Time 1 and 2 (t = 0.44, p = 0.66), Time 2 and 3 (t = 1.47, p = 0.15), nor between Time 1 and 3 (t = 0.96, p = 0.34). Maternal depression remained stable over time.
Fig. 3:
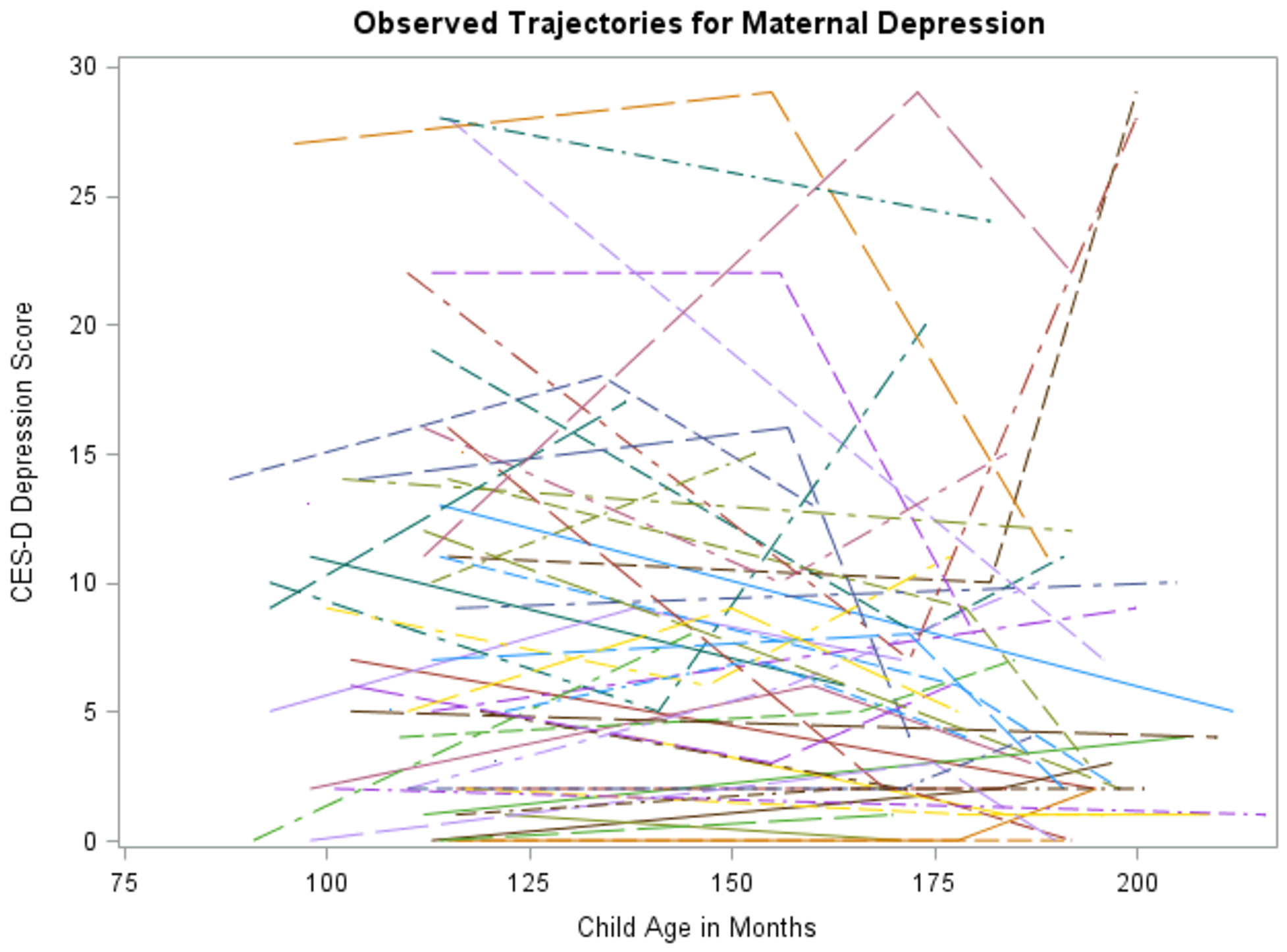
Observed Growth Trajectories for Maternal Depression
Maternal mental health: tension/anxiety.
Visual inspection of maternal tension/anxiety suggested high levels of between-person variation with some within-person variation, see Figure 4. A regression predicting maternal tension/anxiety from child age in months revealed no significant effect of time (t = −0.01, p = 0.38). The repeated-measured ANOVA also revealed no significant effect of time, F(2,42) = 0.15, p = 0.86. Post-hoc tests revealed no significant mean differences between Time 1 and 2 (t = 0.40, p = 0.69), Time 2 and 3 (t = 0.09, p = 0.93), nor between Time 1 and 3 (t = 0.50, p = 0.62). Maternal tension/anxiety remained stable over time.
Fig. 4:
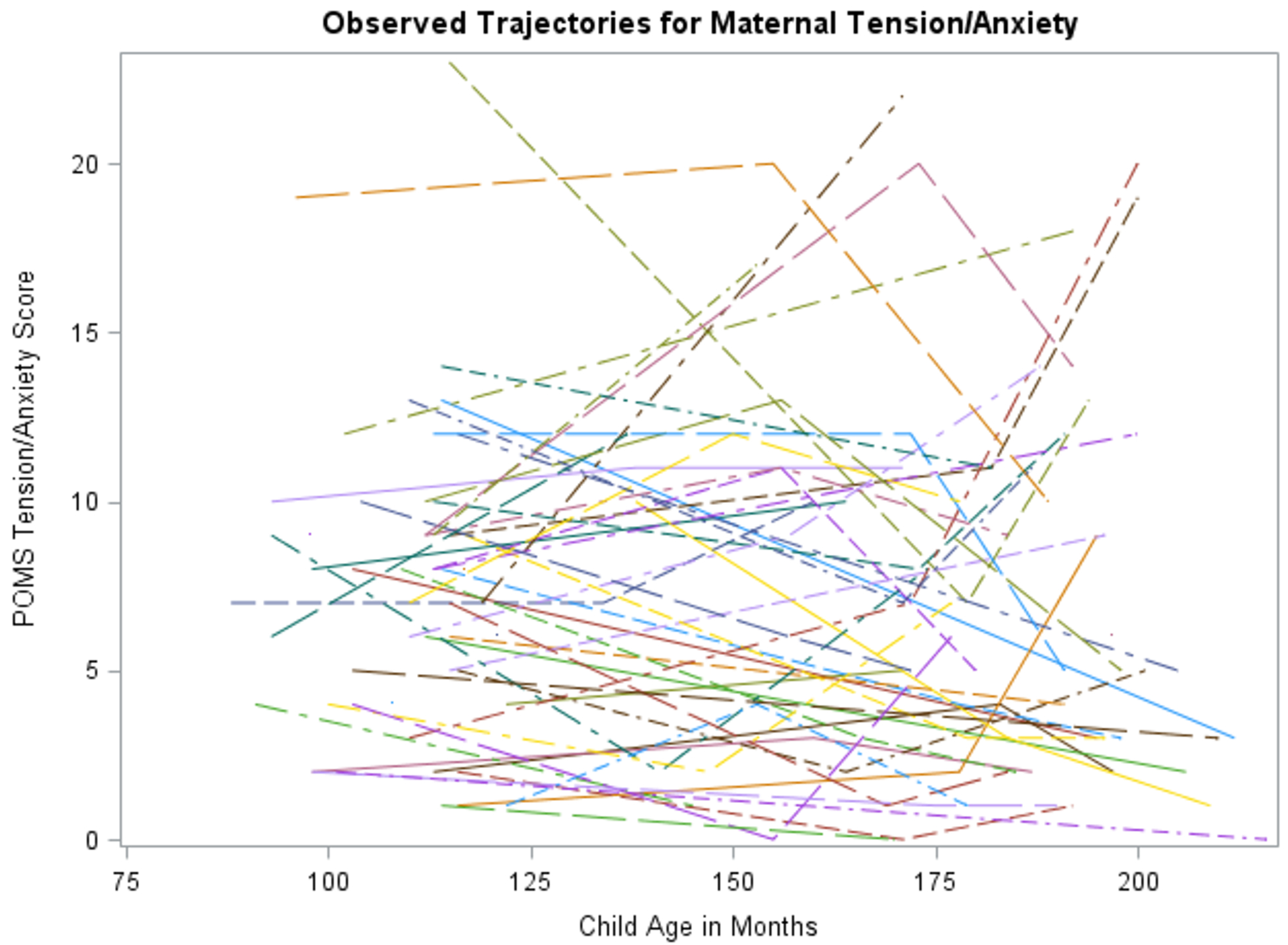
Observed Growth Trajectories for Maternal Tension/Anxiety
Maternal mental health: anger/hostility.
Visual inspection of maternal anger/hostility suggested high levels of between-person variation and marked within-person variation, see Figure 5. A regression predicting maternal anger/hostility from child age in months revealed no significant effect of time (t = −1.57, p = 0.12). The repeated-measured ANOVA also revealed no significant effect of time, F(2,42) = 1.09, p = 0.35. Post-hoc tests indicated no significant mean differences between Time 1 and 2 (t = 0.70, p = 0.49), Time 2 and 3 (t = 1.46, p = 0.15), nor between Time 1 and 3 (t = 0.68, p = 0.50). Maternal anger/hostility remained stable over time.
Child Challenging Behaviors Predicting Maternal Mental Health
To determine if child challenging behaviors predicted maternal mental health, we conducted a multilevel linear model for each mental health outcome: depression, tension/anxiety, and anger/hostility. Because women with pmFXS and FXS may have a genetic predisposition toward mental health concerns, we controlled for maternal CGG repeat length. We also controlled for maternal IQ (from the first visit in the larger ongoing study) and maternal anti-depressant and anti-anxiety medication use (from Time 3, or the most recent visit in the larger study) by including these as time-invariant predictors. To ensure that we accounted for variance at the between- and within-person levels, we created level-1 and level-2 predictors from single variables using person mean centering (Hoffman, 2015). In person mean centering, the level-2 variable is created by averaging the person’s score across the occasions. The level-1 variable comes from the difference between the person’s average and their score at each occasion. Using this method, the level-2 predictor represents how the person is characterized on average and the level-1 predictor represents how far that person deviates from their mean at each occasion. Contextual effects were examined to determine the difference between level-1 and level-2 effects.
Maternal depression.
An empty means, random intercept model was estimated to partition sources of variation in maternal depression. The resulting intraclass correlation (ICC; Hoffman, 2015) of 0.54 was significantly greater than 0, −2ΔLL(df=1) = 31.93. This was indicative of similar levels of variation due to between- and within-person sources. Next, we added level-1 and level-2 child challenging behaviors into the model, controlling for maternal psychiatric medication use. We found that level-1 and level-2 child challenging behaviors were significant predictors of maternal depression, see Table 4. The main effect for level-2 child challenging behaviors suggested that for every point higher the child scored relative to the sample’s average level of behavior problems, the mother’s depression symptoms increased by 0.13 (p = 0.003). The main effect for level-1 child challenging behaviors suggested that for every point higher the child scored relative to their own average, the mother’s depression symptoms increased by 0.13 (p = 0.016). The contextual effect was 0.006 (p = .93) and suggested that the effects of level-1 and level-2 child challenging behaviors were not significantly different. Maternal CGG repeat length, IQ, and medication were not significant predictors of maternal depressive symptoms. This model accounted for 23% of the variance in maternal depressive symptoms.
Table 4:
Multilevel Models Predicting Maternal Mental Health from Child Challenging Behaviors
| Maternal Depression | Maternal Tension/Anxiety | Maternal Anger/Hostility | |||||
|---|---|---|---|---|---|---|---|
| Model for the Means | Est. | SE | Est. | SE | Est. | SE | |
| Intercept | 11.55 | 7.11 | 10.29** | 4.40 | 3.45 | 4.52 | |
| Maternal CGG Repeat Length | −0.04 | 0.03 | −0.03^ | 0.02 | −0.01 | 0.02 | |
| Maternal IQ | .0002 | .05 | 0.001 | 0.03 | 0.03 | 0.03 | |
| Maternal Medication | 2.23 | 1.91 | 1.04 | 1.17 | −1.21 | 1.21 | |
| Child Challenging Behavior Effects | |||||||
| Level-2 Between-Dyad | 0.13** | 0.04 | 0.11** | 0.03 | 0.12* | 0.03 | |
| Level-1 Within-Dyad | 0.13* | 0.05 | 0.04 | 0.04 | 0.03 | 0.03 | |
| Contextual Effect | 0.01 | 0.07 | 0.07 | 0.05 | 0.08^ | 0.04 | |
| Model for the Variance | |||||||
| Random Intercept Variance | 19.72* | 6.28 | 5.22** | 2.43 | 7.67* | 2.61 | |
| Residual Variance | 23.66* | 3.84 | 14.67* | 2.35 | 10.30* | 1.69 | |
| Total R2 | 0.23 | 0.30 | 0.24 | ||||
Note.
p < 0.01,
p ≤ 0.05,
p < 0.10.
Maternal tension/anxiety.
As before, we conducted an empty means, random intercept model for maternal tension/anxiety. The ICC was 0.43 and was significantly greater than 0, −2ΔLL(df=1) = 20.31, indicating that 43% of the variation in maternal tension/anxiety was due to between-person sources. After adding child challenging behavior effects and controlling for maternal IQ, medication, and CGG repeats, we found that level-2 child challenging behaviors but not level-1 challenging behaviors were predictive of maternal tension/anxiety, see Table 4. The level-2 main effect of challenging behaviors suggested that for every point higher the child scored relative to the sample’s average, the mother’s tension/anxiety increased by 0.11 (p = 0.000). There was no significant effect of level-1 child challenging behavior nor of maternal IQ or medication. Mother’s CGG repeat length was marginally significant (p = 0.05), potentially implicating a role of genetic predisposition towards tension/anxiety. The significant random intercept suggested individual differences in mother’s average tension and anxiety symptoms. This model accounted for 30% of the variance in maternal tension/anxiety.
Maternal anger/hostility.
Finally, we conducted an empty means, random intercept model for maternal anger/hostility. The ICC was 0.54 and was significantly greater than 0, −2ΔLL(df=1) = 28.43, again indicating similar levels of between- and within-person sources of variation. We found that level-2 child challenging behaviors were predictive of maternal anger/hostility but that level-1 child challenging behaviors were not. The level-2 main effect of challenging behaviors suggested that for every point higher the child scored relative to the sample’s average, the mother’s anger/hostility increased by 0.12 (p = 0.000). No other predictors were significant. The random intercept was not significant. This model accounted for 24% of the variance in maternal anger and hostility symptoms.
Maternal Mental Health and Child Challenging Behaviors Predicting Relationship Quality
To determine the effects of child challenging behaviors and maternal mental health on mother-child relationship quality we conducted a series of multilevel linear models. First, we conducted an empty means, random intercept model to partition the variation in relationship quality. The empty model confirmed there were sources of both between- and within-person variance in mother-child relationship quality, ICCrelationship quality = 0.69 such that 69% of the variance in relationship quality was due to between-person factors, and the remaining variance due to within-person factors. Next, we added the level-1 and level-2 child challenging behaviors and controlled for maternal medication, which remained non-significant. We found that level-1 and level-2 child challenging behaviors were both significantly predictive of mother-child relationship quality over time, see Table 5. The main effect of level-1 (or within-person) challenging behaviors demonstrated that for every additional behavior the child exhibited at an occasion relative to their usual number of challenging behaviors, the predicted level of mother-child relationship quality decreased by 0.11 (p = 0.001) relative to the dyad’s usual relationship quality. This suggests that mothers may rate their relationship quality lower when their children are demonstrating higher levels of challenging behaviors than usual. The main effect of level-2 (or between-person) child challenging behaviors suggested that for every additional behavior endorsed relative to the sample’s mean, or relative to their peers, the predicted level of relationship quality decreased by 0.14 (p = 0.000) relative to the sample’s mean level of relationship quality. This indicates that mothers whose children have higher levels of challenging behaviors on average report having significantly lower levels of relationship quality or reciprocated closeness. At this step during the modeling, 25% of the variance in relationship quality was accounted for.
Table 5:
Multilevel Models Predicting Mother-Child Relationship Quality from Child Challenging Behaviors and Maternal Depression
| Model Effects | Step 1: Empty Model | Step 2: Add Challenging Behaviors | Step 3: Add Depression | Step 4: Interactions | ||||
|---|---|---|---|---|---|---|---|---|
| Est. | SE | Est. | SE | Est. | SE | Est. | SE | |
| Model for the Means | ||||||||
| Intercept | 51.61* | 0.71 | 51.00* | 0.72 | 53.72* | 1.08 | 53.57* | 1.10 |
| Maternal Medication | 1.74 | 1.55 | 2.18 | 1.43 | 2.30 | 1.46 | ||
| Child Challenging Behavior Effects | ||||||||
| Level-2 Between-Dyad | −0.14* | 0.03 | −0.09** | 0.04 | −0.12** | 0.05 | ||
| Level-1 Within-Dyad | −0.11* | 0.03 | −0.12* | 0.03 | −0.11* | 0.03 | ||
| Maternal Depression Effects | ||||||||
| Level-2 Between-Dyad | −0.33* | 0.11 | −0.34* | 0.11 | ||||
| Level-1 Within-Dyad | 0.01 | 0.07 | 0.07 | 0.07 | ||||
| Moderation Effects | ||||||||
| Level-2 by Level-2 | 0.004 | 0.005 | ||||||
| Level-1 by Level-1 | −0.01 | 0.01 | ||||||
| Model for the Variance | ||||||||
| Random Intercept Variance | 22.46* | 5.43 | 16.73* | 4.34 | 13.89* | 3.79 | 14.09* | 3.95 |
| Residual Variance | 10.13* | 1.67 | 8.98* | 1.52 | 9.12* | 1.55 | 8.91* | 1.54 |
| Total R2 | 0.25 | 0.34 | 0.35 | |||||
| -2 Log Likelihood | 753.6 | 724.2 | 721.0 | 735.1 | ||||
| AIC | 757.6 | 728.2 | 725.0 | 739.1 | ||||
| BIC | 761.6 | 732.2 | 729.0 | 743.0 | ||||
Note.
p < 0.01,
p ≤ 0.05,
p < 0.10.
The next steps involved adding maternal mental health measures. Because we were limited by sample size, we conducted separate analyses for depression, tension/anxiety and anger/hostility. We chose not to combine or conflate these three measures into an aggregate measure of mental health because there is evidence to suggest that mothers with pmFXS may be susceptible to anxious and depressive symptoms (Wheeler et al., 2014), but little is known about angry or hostile symptoms in women with pmFXS. In Step 3 we added level-1 and level-2 depression symptoms. Maternal depression at level-2 was a significant predictor of relationship quality, see Table 5. The main effect of level-2 depression suggested that for every point higher the mother scored on the CES-D relative to her peers over time, the relationship quality between her and her child decreased by 0.33 (p = 0.005) relative to her peers’ average over time. The level-1 effect of maternal depression was not significant. This step of the model accounted for 34% of the variance in mother-child relationship quality. Finally, we added same-level interaction effects to determine whether maternal depression acts as a moderator of the effect of child challenging behaviors on mother-child closeness. Neither the level-2 interaction nor the level-1 interaction between maternal depression and child challenging behaviors was significant. The change in explained variance was unremarkable, as it only increased by 1%. Furthermore, at this step the Akaike and Bayesian Information Criteria (AIC and BIC, respectively) and the −2 log likelihood increased, suggesting that the moderation model was worse fitting than the challenging behavior plus depression model.
Next, we conducted the same steps for maternal tension/anxiety and anger/hostility. The same patterns emerged for these mental health variables as for maternal depression. Level-2 tension/anxiety and anger/hostility were significantly predictive of mother-child closeness. This suggests that mothers who report higher levels of tension/anxiety or anger/hostility than their peers on average over time report lower levels of mother-child relationship quality than their peers on average over time. The effects of level-1 tension/anxiety and anger/hostility did not reach significance, see Tables 6 and 7, respectively. This suggests that within a dyad, higher-than-average levels of tension/anxiety and anger/hostility were not associated with lower-than-average mother-child relationship quality. The moderation effects were not significant for either tension/anxiety or anger/hostility. Finally, the model fit information again suggested that the models that included child challenging behaviors and maternal mental health variables at two levels were the best-fitting models.
Table 6:
Multilevel Models Predicting Mother-Child Relationship Quality from Child Challenging Behaviors and Maternal Tension/Anxiety
| Model Effects | Step 1: Empty Model | Step 2: Add Challenging Behaviors | Step 3: Add Tension/Anxiety | Step 4: Interactions | ||||
|---|---|---|---|---|---|---|---|---|
| Est. | SE | Est. | SE | Est. | SE | Est. | SE | |
| Model for the Means | ||||||||
| Intercept | 51.61* | 0.71 | 51.00* | 0.72 | 54.49* | 1.49 | 53.61* | 1.70 |
| Maternal Medication | 1.74 | 1.55 | 2.09 | 1.47 | 1.62 | 1.52 | ||
| Child Challenging Behavior Effects | ||||||||
| Level-2 Between-Dyad | −0.14* | 0.03 | −0.08* | 0.04 | −0.19** | 0.09 | ||
| Level-1 Within-Dyad | −0.11* | 0.03 | −0.12* | 0.03 | −0.12* | 0.03 | ||
| Maternal Tension/Anxiety Effects | ||||||||
| Level-2 Between-Dyad | −0.48** | 0.18 | −0.42** | 0.19 | ||||
| Level-1 Within-Dyad | 0.12 | 0.09 | 0.15^ | 0.09 | ||||
| Moderation Effects | ||||||||
| Level-2 by Level-2 | 0.01 | 0.01 | ||||||
| Level-1 by Level-1 | −0.03 | 0.02 | ||||||
| Model for the Variance | ||||||||
| Random Intercept Variance | 22.46* | 5.43 | 16.73* | 4.35 | 14.39* | 3.95 | 15.43* | 4.22 |
| Residual Variance | 10.13* | 1.67 | 8.98* | 1.52 | 8.92 | 1.53 | 8.39 | 1.46 |
| Total R2 | 0.25 | 0.34 | 0.34 | |||||
| -2 Log Likelihood | 753.6 | 724.2 | 720.3 | 729.9 | ||||
| AIC | 757.6 | 728.2 | 724.3 | 733.9 | ||||
| BIC | 761.6 | 732.2 | 728.3 | 737.8 | ||||
Note.
p < 0.01,
p ≤ 0.05,
p < 0.10.
Table 7:
Multilevel Models Predicting Mother-Child Relationship Quality from Child Challenging Behaviors and Maternal Anger/Hostility
| Model Effects | Step 1: Empty Model | Step 2: Add Challenging Behaviors | Step 3: Add Anger/Hostility | Step 4: Interactions | ||||
|---|---|---|---|---|---|---|---|---|
| Est. | SE | Est. | SE | Est. | SE | Est. | SE | |
| Model for the Means | ||||||||
| Intercept | 51.61* | 0.71 | 51.00* | 0.72 | 53.431* | 1.02 | 53.73* | 1.23 |
| Maternal Medication | 1.74 | 1.55 | 1.18 | 1.50 | 1.08 | 1.50 | ||
| Child Challenging Behavior Effects | ||||||||
| Level-2 Between-Dyad | −0.14* | 0.03 | −0.08** | 0.04 | −0.12** | 0.05 | ||
| Level-1 Within-Dyad | −0.11* | 0.03 | −0.11* | 0.03 | −0.11* | 0.03 | ||
| Maternal Anger/Hostility Effects | ||||||||
| Level-2 Between-Dyad | −0.44** | 0.18 | −0.56* | 0.20 | ||||
| Level-1 Within-Dyad | −0.13 | 0.11 | −0.11 | 0.11 | ||||
| Moderation Effects | ||||||||
| Level-2 by Level-2 | 0.01 | 0.01 | ||||||
| Level-1 by Level-1 | −0.03 | 0.02 | ||||||
| Model for the Variance | ||||||||
| Random Intercept Variance | 22.46* | 5.43 | 16.73* | 4.35 | 14.88* | 4.00 | 14.69* | 4 |
| Residual Variance | 10.13* | 1.67 | 8.98* | 1.52 | 8.94* | 1.52 | 8.65* | 1.49 |
| Total R2 | 0.25 | 0.31 | 0.34 | |||||
| -2 Log Likelihood | 753.6 | 724.2 | 721.4 | 731.3 | ||||
| AIC | 757.6 | 728.2 | 725.4 | 735.3 | ||||
| BIC | 761.6 | 732.2 | 729.4 | 739.2 | ||||
Note.
p < 0.01,
p ≤ 0.05,
p < 0.10.
Discussion
In this study we demonstrated that child challenging behaviors decreased from childhood and early adolescence to adolescence in individuals with FXS. Mother-child relationship quality on average remained stable from childhood into adolescence, as did measures of maternal depression, anxiety, and anger. We also examined the relationship between maternal mental health and child challenging behaviors controlling for maternal IQ, medication use, and CGG repeat length. Challenging behaviors accounted for between-person differences in maternal depression, anxiety, and anger. They also accounted for within-person fluctuation in maternal depression. Finally, we found that child challenging behaviors accounted for between- and within-dyad variation in mother-child relationship quality, with maternal mental health measures additionally accounting for between-dyad variation in relationship quality. Maternal mental health did not moderate the relationship between child challenging behaviors and mother-child relationship quality.
The stability of maternal mental health is important to note for several reasons. First, mothers in our study demonstrated low levels of mental health disorders, with very few falling into the clinical range for depression. Only 12 mothers in our sample (23%) were prescribed medication for depression or anxiety. Stable maternal mental health may foster a supportive and engaging relationship between the mother and child, which could have important ramifications as the child progresses into adolescence and then into the transition into adulthood. Additionally, stable mental health symptoms confound our understanding of the association between genetics and mental health disorders in pmFXS. Our models did not implicate genetics in mental health symptoms unlike some previous findings (Franke et al., 1996). Although maternal mental health was significantly correlated with CGG repeat length, these correlations were negative. This suggests that higher repeat length is not associated with higher symptoms of mental illness. However, we did not have a control group which limits our interpretation of this finding.
Similar to studies of adolescents and adults with autism, our findings suggest that mother-child closeness may be a stable trait from childhood into adolescence in families with FXS (Hartley, Barker, Baker, Seltzer, & Greenberg, 2012; Smith et al., 2008; Taylor & Seltzer, 2011). While no pattern of change in relationship quality was detected, there was significant variability both between dyads and within dyads. Dyads differed on their initial level of relationship quality and in how their relationship quality fluctuated with time. Within-person fluctuations and average levels of child challenging behavior were strongly associated with mother-child relationship quality. When children were displaying more severe behavior problems than usual, mothers rated the reciprocated closeness in their relationship lower. Similarly, mothers whose children demonstrated higher average levels of challenging behaviors reported lower relationship quality overall. Although this contrasts with previous findings (Hauser et al., 2014), we believe that increased levels of child challenging behaviors may impact the mother’s trust, understanding, affection, fairness, and respect towards her child and her perception of these traits as they are directed by the child towards the mother. These dimensions of relationship quality, particularly child-directed trust and perceived fairness, respect, and affection, may limit the closeness of the relationship. Additionally, mothers whose children demonstrate more severe problem behaviors may feel more burdened by their child and rate relationship quality lower. In the context of mixed findings, it seems that while mother-child relationship quality may be sensitive to child challenging behaviors, the direction of this relationship remains unclear.
Again, similar to reports on autism symptomology in children and adolescents with FXS (Abbeduto, McDuffie, & Thurman, 2014), our data suggested that child challenging behaviors decreased on average once participants entered adolescence. Specifically, there was a significant decrease in challenging behaviors between 9 and 15.9 years of age. Although we did not include a measure of autism symptomology in this study, our findings support the notion that challenging behaviors, whether associated with autism symptomology or not, may decrease as children with FXS move into adolescence. Further research is needed to determine whether reduced challenging behaviors remain stable into adulthood.
Average levels of child challenging behaviors were significantly predictive of maternal depression, such that higher levels of challenging behaviors were associated with increased symptoms of depression. This is inconsistent with previous findings suggesting that higher levels of challenging behaviors related to decreased maternal depression over time (Hauser et al., 2014). We propose two reasons why our results differed. First, our sample may be a more accurate representation of the FXS family population than previous studies. All of the mothers in the Hauser et al. (2014) sample were part of two-parent households, suggesting a certain level of paternal assistance in child-rearing. At Time 3, 29% of mothers in our sample were single, divorced, or separated and did not have paternal support in the home. This is comparable to the 2016 United States Consensus which indicated that roughly 23% of children live in mother-only households (U.S. Census Bureau, 2016). Two-parent households, particularly ones that are highly educated and earning salaries well above the poverty-line, may experience maternal stress, maternal mental health, and child challenging behaviors differently than single-mother households. Single mothers are disproportionately more likely to live in poverty, have lower educational attainment, and identify as minorities than mothers who co-reside with their spouses (U.S. Census Bureau, 2018). They are also more likely to experience psychological distress dues to financial hardship and subsequently limited access to childcare, quality housing, and health care (Broussard, 2010; Stack & Meredith, 2018). Secondly, our measures of child challenging behaviors were completed by the mother, rather than by the father (Hauser et al., 2014). When fathers are the informants, this suggests that fathers are involved in parenting to such an extent that they are perceived as reliable reporters. Although this may reduce mother-reporting bias, it can introduce a sample bias wherein the mothers may have had access to higher levels of emotional support than is typical of this population. Therefore, given the proportion of single mothers in our sample, and our reliance on mother-reported measures, it is not surprising that our results differ from previous work (Hauser et al., 2014).
Although child challenging behaviors accounted for between- and within-person variation in maternal depression, it did not account for maternal anxiety and anger. This is surprising, given that depression and anxiety are highly comorbid and tend to trend together. Our longitudinal findings are inconsistent with cross-sectional findings indicating increased risk of anxiety disorders for pmFXS mothers of children with elevated problem behaviors (Roberts et al., 2008). Perhaps mothers in our sample did not experience higher anxiety when their children were misbehaving because they are accustomed to their child’s challenging behaviors. Or, perhaps they were reliant on medication to alleviate symptoms of anxiety, as one quarter of mothers in our sample were taking prescription anti-anxiety and/or anti-depressant medication. Finally, there may have been an effect of the data-collection setting, such that mothers felt more relaxed providing data in their own home despite their children’s challenging behaviors.
We initially hypothesized that decreased maternal mental health would interact with child challenging behaviors to influence how the mother rated the quality of her relationship with her child with FXS. However, we found no significant interactions between child challenging behaviors and our three measures of maternal mental health. This suggests that mother-child relationship quality may be a measure of the mother’s feelings about her child independent of her depressive, anxious, or hostile symptoms. Poor maternal mental health could influence maternal perceptions of positive constructs, but relationship quality may be a robust construct that remains immune to negative perceptions. Although not a variable in our study, maternal optimism has been associated with better maternal mental health, reduced feelings of stress, and less severe child problem behaviors in families of children with intellectual disability (Jess, Hastings, & Totsika, 2017). Higher levels of maternal optimism are associated with higher relationship quality in adults and adolescents with ASD (Orsmond et al., 2006). Therefore, there may be a moderating effect of maternal optimism on how child challenging behaviors impact relationship quality. Additionally, social support, child characteristics, concerns over the child’s future, and other external factors may interact with child challenging behaviors to impact relationship quality, rather than an interaction between maternal mental health and challenging behaviors. Taken together, these factors may represent maternal resilience, which could protect against negative effects of mental health disorders, parenting stress, genetic liability, or child challenging behaviors.
Our study only considered a small number of possible variables that could account for variation in mother-child relationship quality. Future studies might investigate the relationships between additional aspects of maternal disposition including positivity, warmth, and predisposition towards poor mental health in combination with environmental factors such as social support, marital satisfaction, and child characteristics. It would also be useful to investigate these variables through direct observation rather than parental self-report. A study examining the strength of the association between observed child challenging behaviors and maternal warmth and demonstrated relationship quality could further validate this relationship.
Clinical Implications
Together, the between-dyad and within-dyad findings may have important clinical implications. Specifically, our models suggest that for each additional point scored on the CBCL (which can indicate either higher total number of challenging behaviors or higher severity of those behaviors), mothers may report roughly 0.12 points higher on measures of depression, anxiety, and anger. Although this may seem like a small point estimate, when we consider an example wherein a child demonstrates eight additional challenging behaviors relative to his peers, his mother might report one point higher on the CES-D or POMS. Considering the clinical cut off on the CES-D is 16, this may quickly push the mother into a concerning or even clinically significant range for depression. Additionally, mothers who experience high levels of mental health symptoms may need additional support because poor mental health is associated with worse child behavior and compromised mother-child closeness. Reduced mother-child reciprocated closeness could impact maternal responsivity, which has been linked to positive child outcomes (Brady, Warren, Fleming, Keller, & Sterling, 2014; Warren et al., 2010). Thus, it is important to monitor maternal well-being along with child challenging behaviors as these could have lasting effects on the relationship between the mother and child.
Strengths and Limitations
Strengths.
Our sample shows some diversity in socioeconomic status, maternal education, marital status, and race despite being a sample of convenience. The size of our sample was sufficient to perform sophisticated multilevel analyses to determine the relationship between maternal mental health, child challenging behaviors, and mother-child relationship quality. Additionally, a strength of this study lies in the time span that it covers. We examined variables of interest from when the children were on average 9 years old until they were near 16. This time span is longer than many previous studies, and begins at a younger age than previous studies (Hauser et al., 2014). Accordingly, our longitudinal study provides insight into the nature of maternal mental health, child challenging behaviors, and mother-child relationship quality as children with FXS transition from childhood into adolescence in a relatively representative sample. Finally, a significant strength of our study lies in our high subject retention across a large time span. More than eighty percent of our sample was retained from early childhood into adolescence, enabling us to observe change and fluctuation over time in children with FXS and their mothers.
Limitations.
Our sample does not accurately represent a population mode, as there is skew towards higher SES. This sample of convenience may include a disproportionately high level of mothers and children with strong relationship quality. An additional possible limitation lies in the fact that all the measures in this study were completed by the mother, and we did not include observational data on maternal mental health, child challenging behaviors, or mother-child relationship quality. Mothers reported their child’s level of challenging behaviors, their own mental health symptoms, and their impressions of the relationship quality between herself and her child. This could lead to maternal-reporting bias. Independent ratings of child challenging behaviors and maternal mental health symptoms would disentangle how maternal mood may affect ratings. A second limitation in this study is the likelihood of a ceiling effect for the PAI. At Time 1, 29% of mothers endorsed greater than 54 out of 60 on the PAI, suggesting very high relationship quality. At Time 2, 37% endorsed this high level, and at Time 3 41% endorsed it. A sizeable proportion of mothers at each time endorsed extremely high mother-child relationship quality, and 12 mothers endorsed consistently high relationship quality across time. This is suggestive of a bias towards high ratings, which may not be the case. The PAI asks mothers to rate their feelings of closeness and their perceptions of reciprocated closeness with their child. Some mothers may be uncomfortable with this measure and report elevated relationship quality if they believe that reporting lower relationship quality would reflect poorly on them in the eyes of our research team. Although these limitations are important to note, similar measurement methods are widely used in this field. As such, our results should be interpreted relative to these previous findings (Greenberg et al., 2004; Hartley et al., 2012; Smith et al., 2008; Taylor & Seltzer, 2011).
Conclusion
The relationship between maternal mental health, child challenging behaviors and mother-child relationship quality is complex in families with FXS. Child challenging behaviors can negatively affect both maternal mental health and mother-child relationship quality (Bailey et al., 2008; Hauser et al., 2014; Zeedyk & Blacher, 2017). In our sample of families with FXS, we found evidence that child challenging behaviors and maternal mental health affect mother-child relationship quality over time. If child challenging behaviors are left untreated, this could have detrimental downstream effects. Mothers may experience compromised mental health and mother-child relationship quality. Over time, this could lead to impaired family functioning which may interfere with positive outcomes in children and adolescents with FXS. This is particularly important in families with FXS where both mother and child may experience symptoms of the disorder. Therefore, clinical interventions might focus in part on ensuring that child challenging behaviors, maternal mental health, and mother-child relationship quality remain positive and stable in families with FXS.
Acknowledgements:
The authors would like to thank Shelley Bredin-Oja from the Fragile X Lab at the University of Kansas for her wonderful data management, Katie Schneider for assistance with an earlier version of this study, and Lesa Hoffman for her invaluable knowledge of statistical analyses. Finally, we thank the families for their continued participation and support in our ongoing study.
Funding: This study is supported by the following NICHD grants: P30 HD00310, P30 HD02538, and R01 HD084563 (PIs Steve Warren and Nancy Brady). The first author is supported by NICDC T32 DC000052 (PI: Mabel Rice).
Footnotes
Conflicts of Interest: The authors declare that they have no conflicts of interest.
Ethical approval: All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional review board (University of Kansas IRB, study reference number 17261) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed consent was obtained from all individual participants included in the study. Mothers gave informed consent for themselves and their children.
References
- Abbeduto L, Brady N, & Kover ST (2007). Language Development and Fragile X Syndrome: Profiles, Syndrome-Specificity, and Within-Syndrome Differences. Mental Retardation and Developmental Disabilities Research Reviews, 13, 36–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abbeduto L, McDuffie A, & Thurman AJ (2014). The fragile X syndrome-autism comorbidity: What do we really know? Frontiers in Genetics, 5, 3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abbeduto L, Seltzer MM, Shattuck P, Krauss MW, Orsmond GI, & Murphy MM (2004). Psychological Well-Being and Coping in Mothers of Youths With Autism, Down Syndrome, or Fragile X Syndrome. American Journal on Mental Retardation, 109(3), 237–254. doi: [DOI] [PubMed] [Google Scholar]
- Achenbach TM, & Rescorla LA (2001). Manial for the ASEBA School-Age Forms and Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families. [Google Scholar]
- Bailey DB, Sideris J, Roberts JE, & Hatton DD (2008). Child and Genetic Variables Associated with Maternal Adaptation to Fragile X Syndrome: A Multidimensional Analysis. American Journal of Medical Genetics Part A, 146A, 720–729. [DOI] [PubMed] [Google Scholar]
- Bengtson VL, & Schrader S (1982). Parent-Child Relations In Mangen D & Peterson W (Eds), Research Instruments in Social Gerontology (Vol. 2, pp. 115–186). Minneapolis, MN: University of Minnesota Press. [Google Scholar]
- Brady N, Warren SF, Fleming K, Keller J, & Sterling A (2014). Effect of Sustained Maternal Responsivity on Later Vocabulary Development in Children with Fragile X Syndrome. Journal of Speech, Language, and Hearing Research, 2014(57). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broussard CA (2010). Research regarding low-income single mothers’ mental and physical health: A decade in review. Journal of Poverty, 14, 433–451. [Google Scholar]
- Bureau UC (2016). 2016 Current Population Survey Annual Social and Economic Supplement. Retrieved from www.census.gov/hhes/families
- Bureau USC (2018). Decennial Census 1960 and Current Population Survey, Annual Social and Economic Supplements 1968 to 2018. [Google Scholar]
- Cohen D, Pichard N, Tordjman S, Baumann C, Burglen L, Excoffier E, … Heron D (2005). Specific genetic disorders and autism: clinical contribution towards their identification. J Autism Dev Disord, 35(1), 103–116. [DOI] [PubMed] [Google Scholar]
- Curran SL, Andrykowski MA, & Studts JL (1995). Short Form of the Profile of Mood States (POMS-SF): Psychometric Information. Psychological Assessment, 7(1), 80–83. [Google Scholar]
- Darnell JC, Warren ST, & Darnell RB (2004). The fragile X mental retardation protein, FMRP, recognizes G-quartets. Ment Retard Dev Disabil Res Rev, 10(1), 49–52. doi: 10.1002/mrdd.20008 [DOI] [PubMed] [Google Scholar]
- Debrey SM, Leehey MA, Klepitskaya O, Filley CM, Shah RC, Kluger B, … Hall DA (2016). Clinical Phenotype of Adult Fragile X Gray Zone Allele Carriers: a Case Series. The Cerebellum, 15(5), 623–631. doi: 10.1007/s12311-016-0809-6 [DOI] [PubMed] [Google Scholar]
- Franke P, Maier W, Hautzinger M, Weiffenbach O, Gansicke M, Iwers B, … Froster U (1996). Fragile-X Carrier Females: Evidence for a Distinct Psychopathological Phenotype? American Journal of Medical Genetics, 64, 334–339. [DOI] [PubMed] [Google Scholar]
- Greenberg JS, Seltzer MM, Krauss MW, Chou RJ-A, & Hong J (2004). The Effect of Quality of Relationship Between Mothers and Adult Children with Schizophrenia, Autism, or Down Syndrome on Maternal Well-Being: The Mediating Role of Optimism. American Journal of Orthopsychiatry, 74(1), 14–25. doi: 10.1037/0002-9432.74.1.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagerman PJ, & Hagerman RJ (2004). The Fragile-X Premutation: A Maturing Perspective. American Journal of Human Genetics, 74, 805–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagerman RJ, & Hagerman PJ (2013). Advances in clinical and molecular understanding of theFMR1premutation and fragile X-associated tremor/ataxia syndrome. Lancet Neurology, 12(8), 786–798. doi: 10.1016/S1474-4422(13)70125-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardiman RL, & McGill P (2018). How common are challenging behaviors amongst individuals with Fragile X Syndrome? A systematic review. Research in Developmental Disabilities, 76, 99–109. [DOI] [PubMed] [Google Scholar]
- Hartley SL, Barker ET, Baker JK, Seltzer MM, & Greenberg JS (2012). Marital satisfaction and life circumstances of grown children with autism across 7 years. Journal of Family Psychology, 26(5), 688–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatton DD, Hooper SR, Bailey DB, Skinner ML, Sulliva KM, & Wheeler A (2002). Problem Behavior in Boys with Fragile X Syndrome. American Journal of Medical Genetics, 108, 105–116. doi: 10.1002/ajmg.10216 [DOI] [PubMed] [Google Scholar]
- Hauser CT, Kover ST, & Abbeduto L (2014). Maternal well-being and child behavior in families with fragile X syndrome. Research in Developmental Disabilities, 35, 2477–2486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman L (2015). Longitudinal analysis: Modeling within-person fluctuation and change. New York, NY: Routledge Academic. [Google Scholar]
- Hunter JE, Rohr JK, & Sherman SL (2010). Co-occuring diagnoses amoing FMR1 premutation allele carriers. Clinical Genetics, 77, 374–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inc SI(2013). SAS 9.4. Cary, NC: SAS Institute Inc. [Google Scholar]
- Jess M, Hastings RP, & Totsika V (2017). The construct of maternal positivity in mothers of children with intellectual disability. Journal of Intellectual Disability Research, 61(10), 928–938. [DOI] [PubMed] [Google Scholar]
- Johnston LC, Hessl LD, Blasey LC, Eliez LS, Erba LH, Dyer-Friedman LJ, … Reiss LA (2003). Factors Associated with Parenting Stress in Mothers of Children with Fragile X Syndrome. Journal of Developmental & Behavioral Pediatrics, 24(4), 267–275. doi: 10.1097/00004703-200308000-00008 [DOI] [PubMed] [Google Scholar]
- Klusek J, Martin GE, & Losh M (2014). Consistency Between Research and Clinical Diagnoses of Autism Among Boys and Girls with Fragile X Syndrome. Journal of Intellectual Disability Research, 58(10), 940–952. doi: 10.1111/jir.12121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Seeley JR, Roberts RE, & Allen NB (1997). Center for Edipemiologic Studies Depression Scale (CES-D) As a Screening Instrument for Depression Among Community-Residing Older Adults. Psychology and Aging, 12(2), 277–287. [DOI] [PubMed] [Google Scholar]
- Lewis P, Abbeduto L, Murphy MM, Richmond E, Giles N, Bruno L, & Schroeder S (2006). Cognitive, language and social-cognitive skills of individuals with fragile X syndrome with and without autism. Journal of Intellectual Disability Research, 50(7), 532–545. [DOI] [PubMed] [Google Scholar]
- Lewis P, Abbeduto L, Murphy MM, Richmond E, Giles N, Bruno L, … Orsmond GI (2006). Psychological well-being of mothers of youth with fragile X syndrome: syndrome specificity and within-syndrome variability. Journal of Intellectual Disability Research, 50(2), 894–904. [DOI] [PubMed] [Google Scholar]
- Mazzocco MMM, Kates WR, Baumgardner TL, Freund LS, & Reiss AL (1997). Autistic Behaviors Among Girls with Fragile X Syndrome. Journal of Autism and Developmental Disorders, 27(4), 415–435. [DOI] [PubMed] [Google Scholar]
- McNair DM, Lorr M, & Droppleman LF (1971). Manual for the Profile of Mood States. San Diego, CA: Educational and Industrial Testing Services. [Google Scholar]
- Orsmond GI, Seltzer MM, Greenberg JS, & Krauss MW (2006). Mother-Child Relationship Quality Among Adolescents and Adults with Autism. American Journal on Mental Retardation, 111(2), 121–137. [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D Scale: A self report depression scale for research in the general population. Applied Psychological Measurements, 1, 385–401. [Google Scholar]
- Rinehart NJ, Cornish KM, & Tonge BJ (2010). Gender Differences in Neurodevelopmental Disorders: Autism and Fragile X Syndrome. In Neill JC & Kulkarni J (Eds.), Biological Basis of Sex Differences in Psychopharmacology. [DOI] [PubMed] [Google Scholar]
- Roberts JE, Bailey DB, Mankowski J, Ford A, Sideris J, Weisenfeld LA, … Golden RN (2008). Mood and Anxiety Disorders in Females with the FMR1 Premutation. American Journal of Medical Genetics Part B, 150B, 130–139. [DOI] [PubMed] [Google Scholar]
- Seltzer MM, Greenberg JS, & Krauss MW (1995). A Comparison of Coping Strategies of Aging Mothers of Adults with Mental Illness or Mental Retardation. Psychology and Aging, 10(1), 64–75. doi: 10.1037/0882-7974.10.1.64 [DOI] [PubMed] [Google Scholar]
- Smith LE, Greenberg JS, Seltzer MM, & Hong J (2008). Symptoms and behavior problems of adolescents and adults with autism: Effects of mother-child relationship quality, warmth, and praise. American Journal on Mental Retardation, 113(5), 387–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stack RJ, & Meredith A (2018). The impact of financial hardship on single parents: An exploration of the journey from social distress to seeking help. Journal of Family and Economic Issues, 39(2), 233–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan AK, Marcus M, Epstein MP, Allen EG, Anido AE, Paquin JJ, … Sherman SL (2005). Association of FMR1 repeat size with ovarian dysfunction. Human Reproduction, 20(2), 402–412. doi: 10.1093/humrep/deh635 [DOI] [PubMed] [Google Scholar]
- Taylor JL, & Seltzer MM (2011). Changes in the mother-child relationship during the transition to adulthood for youth with autism spectrum disorders. Journal of Autism and Developmental Disorders, 41(10), 1397–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verkerk AJ, Pieretti M, Sutcliffe JS, Fu YH, Kuhl DP, Pizzuti A, … et al. (1991). Identification of a gene (FMR-1) containing a CGG repeat coincident with a breakpoint cluster region exhibiting length variation in fragile X syndrome. Cell, 65(5), 905–914. [DOI] [PubMed] [Google Scholar]
- Warren SF, Brady N, Sterling A, Fleming K, & Marquis J (2010). Maternal responsivity predicts language development in young children with fragile X syndrome. American Journal of Intellectual and Developmental Disabilities, 115(1), 54–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D (1997). Wechsler Adult Intelligence Scale-III (3rd ed). San Antonio, TX: Harcourt Assessment. [Google Scholar]
- Wheeler A, Bailey DB, Berry-Kravis E, Greenberg JS, Losh M, Mailick M, … Hagerman RJ (2014). Associated features in females with an FMR1 premutation. Journal of Neurodevelopmental Disorders, 6(30). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeedyk SM, & Blacher J (2017). Longitudinal Correlates of Maternal Depression Among Mothers of Children With or Without Intellectual Disability. American Journal of Intellectual and Developmental Disabilities, 122(5), 374–391. [DOI] [PubMed] [Google Scholar]


