Abstract
Background.
Evidence from high-income countries suggests that childhood trauma is associated with schizophrenia. Studies of childhood trauma and schizophrenia in low and middle income (LMIC) countries are limited. This study examined the prevalence of childhood traumatic experiences among cases and controls and the relationship between specific and cumulative childhood traumatic experiences and schizophrenia in a sample in South Africa.
Methods.
Data were from the Genomics of Schizophrenia in the South African Xhosa people study. Cases with schizophrenia and matched controls were recruited from provincial hospitals and clinics in the Western and Eastern Cape regions in South Africa. Childhood traumatic experiences were measured using the Childhood Trauma Questionnaire (CTQ). Adjusted logistic regression models estimated associations between individual and cumulative childhood traumatic experiences and schizophrenia.
Results.
Traumatic experiences were more prevalent among cases than controls. The odds of schizophrenia were 2.44 times higher among those who experienced any trauma than those who reported no traumatic experiences (95% CI 1.77–3.37). The odds of schizophrenia were elevated among those who experienced physical/emotional abuse (OR 1.59, CI 1.28–1.97), neglect (OR 1.39, CI 1.16–1.68), and sexual abuse (OR 1.22, CI 1.03–1.45) compared to those who did not. Cumulative physical/emotional abuse and neglect experiences increased the odds of schizophrenia as a dose–response relationship.
Conclusion.
Childhood trauma is common in this population. Among many other benefits, interventions to prevent childhood trauma may contribute to a decreasing occurrence of schizophrenia.
Keywords: Case–control, childhood trauma, psychosis, South Africa
Introduction
Childhood trauma refers to adverse experiences and conditions during childhood and includes emotional, physical and sexual abuse as well as emotional and physical neglect (Morgan and Fisher, 2007). Research suggests that childhood trauma has enduring neurobiological effects (Gunnar and Quevedo, 2007; McCrory et al., 2011) and is associated with a range of physical and mental illnesses in adolescence and adulthood (Kraan et al., 2015; Mandelli et al., 2015; Baumeister et al., 2016). These include both clinical and subclinical levels of schizophrenia (Matheson et al., 2012). Further, childhood trauma may impact the course of schizophrenia and affect symptom severity and prognosis (Matheson et al., 2012; van Dam et al., 2012; Trotta et al., 2015).
Two recent meta-analyses of observational studies found that experiences of childhood adversity were significantly higher among schizophrenia cases compared with controls (Matheson et al., 2012) (Varese et al., 2012). These analyses found an increased risk of psychosis or schizophrenia due to childhood trauma, irrespective of study designs or trauma measure.
Nearly all studies to date have examined these relationships using samples from high-income countries (Trotta et al., 2013; Fisher et al., 2014; Dantchev et al., 2018; Sideli et al., 2018). Among the few studies conducted in low- and middle-income countries, South African studies found that childhood trauma was associated with premorbid adjustment and schizophrenia outcomes (Kilian et al., 2017a, 2017b; Asmal et al., 2018). Further, studies in LMICs have rarely considered the type of event or the number of cumulative traumas. It is important to study these relationships in LMICs in order to understand the context-specific schizophrenia risk and morbidity associated with childhood trauma, and to potentially inform appropriate interventions and policies to improve social and mental health outcomes for children. South Africa has a high prevalence of childhood trauma in the general population and more evidence is needed to understand the experience of trauma among people with severe mental illness (Jewkes et al., 2010; Denckla et al., 2017).
The current paper seeks to contribute to the literature on childhood trauma and schizophrenia in LMICs through the following aims: (1) to describe the prevalence of an array of childhood traumas in cases and controls; (2) to examine how types of childhood trauma are associated with schizophrenia; and (3) to examine the associations between the cumulative number of traumas and schizophrenia.
Methods
Sample
This study utilized data from the Genomics of Schizophrenia in the South African Xhosa people (SAX) project. SAX is a case–control study designed to identify genetic variations and social exposures related to schizophrenia risk in a sample of the Xhosa population. Xhosa speaking people are one of the largest indigenous groups in South Africa and live mainly in the Eastern and Western Cape regions of South Africa (Koen et al., 2012; Campbell et al., 2017a).
The recruitment strategies of the study have been described in previous publications (Campbell et al., 2017a, 2017b). Initiated in January 2013, participants were Xhosa speaking people recruited from provincial hospitals and clinics in the Western and Eastern Cape regions of South Africa over a 5-year period. Xhosa language and ethnicity were self-reported.
Cases were defined using the following criteria: respondents who received a clinical diagnosis of schizophrenia or schizoaffective disorder for at least 2 years duration, and could give informed consent. Controls were defined as respondents who presented for treatment of non-psychiatric medical conditions at university-affiliated general medical hospitals and community health centers (CHC) that draw from similar catchment areas to the psychiatric hospitals and clinics where cases were recruited, matched by age group (e.g. 21–25) and gender.
The complete sample consists of 1420 cases (50.77%) and 1377 controls (49.23%) (n = 2797). Within the study sample, exposure data were completely missing for 326 respondents (11.6% of the total sample), and partially missing for 374 respondents (13.3% of the full sample). We attribute this to the inconsistent administering of the CTQ when the study began in 2013. To maximize the sample size, the main analysis imputed missing items for respondents with partial exposure data, using multiple imputations with 15 combined datasets, with corrected standard errors (Rubin, 1987). Imputation models included schizophrenia status, age, education, and all traumatic experience items. Those with missing responses for all traumatic experiences were excluded. Imputed model estimates were compared to unimputed estimates to examine the robustness of the analytic models to the degree of missing data. The final analytic sample comprised 2471 individuals (49.5% cases). Compared with the analytic sample, respondents with completely missing data were younger (age 34.9 v. 36.2, p = 0.0195) and more likely to be cases (60.7% v. 49.5%, p = 0.0002). There were no differences in education and gender between included and excluded samples.
Measures
The Structured Clinical Interview for Diagnosis for axis I disorders (DSM IV-TR version) (SCID-I), a widely used semi-structured interview tool (Spitzer et al., 1992; First et al., 1997) was administered to participants in Xhosa by one of the trained psychiatric nurses. The SCID-I has been found to have acceptable internal consistency, test–retest reliability as well as concurrent and predictive reliability (Spitzer et al., 1992). The SCID-I collects data on psychopathology and physical illnesses including cardiovascular disease, diabetes, Tuberculosis and HIV/AIDS. For this study, interrater reliability for the translated Xhosa version of the SCID-I was obtained on a smaller sample of participants (N = 22). Reliability was good for the principle psychotic disorder diagnosis (κ = 0.74, p < 0.001). In addition to the patient interview, information was considered in the diagnostic process from referral notes, past and current clinical records, interviews with other members of the multidisciplinary teams and information from family members or other acquaintances of the patients. SCID-I interviews typically lasted 1.5–4.5 h.
The Childhood Trauma Questionnaire (CTQ) was administered to measure participants’ childhood trauma experiences. The CTQ has been employed in several contexts, including in South Africa (Martin et al., 2014; Kilian et al., 2017b). The CTQ consists of 25 items designed for retrospective self-report of childhood trauma (Fink et al., 1995), and was originally designed to capture five broad trauma domains: emotional abuse, sexual abuse, physical abuse, emotional and physical neglect. In order to consider the cumulative effects of experiencing multiple traumas, each item was dichotomized as ever versus never experienced, consistent in several previous studies employing the CTQ to examine the onset of various psychopathologies (Gil et al., 2009; Tucci et al., 2010; Powers et al., 2016). A full list of CTQ items can be found in online Supplementary Appendix 1. Respondents were asked to self-report how often a traumatic event occurred, from 1 (never) to 5 (often). Six items that refer to positive childhood experiences were reversecoded so that a higher total score reflected a greater level of childhood trauma.
In addition, the CTQ includes a three-item minimization or denial scale used to assess respondents’ potential for extreme reporting bias (Fink et al., 1995; Bernstein et al., 2003; McGrath et al., 2010). However, there is disagreement regarding the validity of the scale as a measure of response bias (MacDonald et al., 2014), and it has been inconsistently used, including in several previous studies of South African samples (Kenny et al., 2007; Gerdner and Allgulander, 2009; Lochner et al., 2010; Spies and Seedat, 2014; Spies et al., 2016). Therefore we did not remove respondents who met minimization/denial criteria.
Several covariates were considered to control for unmeasured confounding, based on previous studies of childhood trauma and schizophrenia (Powers et al., 2016) as well as to remove the bias introduced by our matching strategy (Pearce, 2016). These included sex, continuous age (range: 21–54), education level (0–8th grade versus more than 8th grade), urbanicity (rural, urban, township), and region (Western Cape, Eastern Cape). A second set of models were run adjusting for additional covariates that represent potential comorbidities with schizophrenia, including lifetime depression (any v. none); lifetime alcohol use disorder (none v. abuse or dependence), and lifetime cannabis disorder (none v. abuse or dependence).
Those who were visually impaired or unable to read were assisted in completing the questionnaire by a nurse. All survey items were translated and back-translated into Xhosa in line with World Health Organization translation procedures (Menon et al., 2012).
CTQ validation
There has been limited use of the CTQ in Xhosa-speaking samples and previous studies have not translated the instrument (Spies et al., 2016). Therefore, in a preliminary analysis, we examined validity and internal consistency of the translated instrument in our sample using factor analysis and ω coefficients (Dunn et al., 2014). In the validation, an initial confirmatory factor analysis (CFA) was run to attempt to replicate the factor structure as originally designed. In the event of a poor CFA fit, we allowed for a newly derived factor structure, using exploratory factor analysis (EFA) in order to identify the best-fitting factor model of latent trauma domains. This exploratory approach was chosen over the use of CFA modification indices, to derive the most interpretable factor solution from the instrument. Factor loadings were estimated using weighted least squares means and variances, in order to handle categorical variables with non-normally distributed errors (Costello and Osborne, 2005). Goodness-of-fit was evaluated using the Root Mean Square Error of Approximation (RMSEA) and its 95% confidence interval (CI), and the Comparative Fit Index (CFI). Based on previous recommendations, we set cutoffs for acceptable fit at RMSEA < 0.10 and CFI > 0.90, and good fit at RMSEA < 0.05 and CFI > 0.95 (Hu and Bentler, 1999; Wall and Amemiya, 2000). Additionally, in order to obtain an interpretable factor solution, we excluded items with low (<0.3) loadings on all factors, as well as statistically significant cross-loadings on multiple factors. Factor correlation was estimated using Pearson’s r coefficient. Using the best-fitting factor solution, we then examined the internal consistency of each factor and the total CTQ scale with ω coefficients. Subsequent analyses were based on the best-fitting interpretable factor solution.
Data analysis
First, to better understand the degree of co-occurring traumatic events, we estimated the correlations between individual childhood trauma experiences. Second, we estimated the prevalence of individual traumas in the total sample, and compared the prevalence of each item among cases and controls using χ2 tests. Third, we estimated the prevalence of each trauma domain, dichotomized as ever versus never experienced, in the total sample and among cases and controls. Fourth, we estimated the odds ratios (ORs) of schizophrenia among those who experienced each trauma domain, compared with those who did not, in adjusted logistic regression models. Fifth, to examine the total burden of childhood traumatic experiences, we calculated the prevalence of experiencing cumulative individual traumas and estimated the odds of schizophrenia among those who experienced 1, 2, or 3 or more cumulative trauma domains compared with no trauma. Data were analyzed using SAS version 9.4 and Mplus version 7.
Ethical considerations
Ethical approval was granted by the Human Ethics Committee of the Faculty of Health Sciences, University of Cape Town, South Africa (HREC number: 049/2013) to conduct the study. Prior to data collection, our fieldworkers carefully explained in Xhosa the purpose and procedures of the study emphasizing that participation is entirely voluntary. He or she also explained that withdrawing from the study at any time is the participant’s right and that data will be kept confidential by the study team. Individuals with schizophrenia may experience cognitive decline (Keefe and Harvey, 2012; Bora, 2015) so to ensure that informed consent was fully understood, all participants were screened for decisional capacity using the University of California, San Diego Brief Assessment of Capacity to Consent (UBACC) questionnaire (Seaman et al., 2015; Campbell et al., 2017b). This is a well validated tool for screening for decisional capacity in participants with cognitive impairment.
Results
The initial EFA included the entire 25-item instrument. The model fit of a five-factor solution was good, however, there were several items with significant cross-loadings onto multiple factors. After removing four items, we identified a three-factor model with 21 items that evidenced good fit (CFI = 0.98; TLI = 0.97; RMSEA = 0.054), was interpretable, and was consistent with the original CTQ design. The ω coefficients for each factor domain indicated acceptable to excellent internal consistency. The three-factors included: (1) physical/emotional abuse (12 items; ω = 0.94); (2) neglect which comprises the lack of protective factors during childhood (4 items; ω = 0.85); and (3) sexual abuse (5 items; ω = 0.93). The total scale ω coefficient was 0.96 and the factor correlation coefficients ranged from 0.45 to 0.71. The final factor model is presented in online Supplementary Table S1. Together these findings suggest that the 21-item modified version of the CTQ has acceptable reliability and validity in this population.
The analytic sample comprised 88.1% men. The mean age of the sample was 36.1 years (S.D. = 9.13, range 21–54 years) and 71.9% had a minimum of primary school education. Overall, correlations between CTQ items were greater than 0.05 ranging from 0.16 to 0.70. The factor correlations were moderate, ranging from 0.21 to 0.42. All correlations are presented in online Supplementary Table S2.
The prevalence of individual childhood traumatic experiences overall and among cases and controls is presented in Table 1. Notably, the prevalence of experiencing any trauma was very high among cases (94.4%) as well as among controls (87.1%). All individual traumatic events were more prevalent among cases than controls. The prevalence of experiencing each trauma domain is presented in Table 2. Cases were significantly more likely to have experienced all trauma domains compared with controls. In the fully adjusted logistic regression models, the odds of schizophrenia was higher among those who experienced physical/emotional abuse (OR 1.63, 95% CI 1.28–2.1), neglect (OR 1.23, 95% CI 1.0–1.52) and sexual abuse (OR 1.22, 95% CI 1.0–1.48), compared with those who did not have these experiences. The odds of schizophrenia were 2.05 times higher among those who experienced any trauma than those who did not (95% CI 1.45–2.91). All model estimates are presented in Table 3.
Table 1.
Prevalence of childhood traumatic events among those with and without schizophrenia
| Total | Controls | Cases | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p value | |
| Physical/emotional abuse | |||||||
| I didn’t have enough to eat | 885 | 42.2 | 440 | 40.4 | 445 | 48.1 | 0.0829 |
| People in my family called me things like ‘stupid’, ‘lazy’, or ‘ugly’ | 934 | 44.5 | 425 | 39.0 | 509 | 50.5 | <0.0001 |
| My parents were too drunk or high to take care of me | 723 | 34.5 | 351 | 32.2 | 372 | 36.9 | 0.025 |
| I had to wear dirty clothes | 702 | 33.5 | 326 | 29.9 | 376 | 37.3 | 0.0004 |
| I thought that my parents wished I had never been born | 784 | 37.4 | 379 | 34.8 | 405 | 40.2 | 0.011 |
| I got hit so hard by someone in my family that I had to see a doctor | 642 | 30.6 | 312 | 28.7 | 330 | 32.7 | 0.042 |
| People in my family hit me so hard that it left bruises or marks | 730 | 34.8 | 353 | 32.4 | 377 | 37.4 | 0.017 |
| I was punished with a belt, a board, a cord, or some hard object | 982 | 46.8 | 470 | 43.2 | 512 | 50.8 | 0.001 |
| People in my family said hurtful or insulting things to me | 847 | 40.4 | 398 | 36.6 | 449 | 44.5 | 0.0002 |
| I believe that I was physically abused | 825 | 39.3 | 409 | 37.6 | 416 | 41.3 | 0.082 |
| I got hit or beaten so badly that it was noticed by someone like a teacher | 618 | 29.5 | 300 | 27.6 | 318 | 31.6 | 0.045 |
| I felt that someone in my family hated me | 876 | 41.8 | 417 | 38.3 | 459 | 45.5 | 0.001 |
| Neglect | |||||||
| I knew there was someone to take care of me and protect me | 871 | 41.5 | 427 | 39.2 | 444 | 44.1 | 0.025 |
| There was someone in my family who helped me feel important or special | 1055 | 50.3 | 519 | 47.7 | 536 | 53.2 | 0.012 |
| I felt loved | 1077 | 51.4 | 531 | 48.8 | 546 | 54.2 | 0.013 |
| There was someone to take me to the doctor if I needed it | 1099 | 52.4 | 539 | 49.5 | 560 | 55.6 | 0.006 |
| Sexual abuse | |||||||
| Someone tried to touch me in a sexual way, or tried to make me touch them | 632 | 30.1 | 307 | 28.2 | 325 | 32.2 | 0.043 |
| Someone threatened to hurt me or tell lies about me unless I did something | 624 | 29.8 | 315 | 28.9 | 309 | 30.7 | 0.387 |
| Someone tried to make me do sexual things or make me watch sexual things | 629 | 30.0 | 306 | 28.1 | 323 | 32.0 | 0.049 |
| Someone molested me | 730 | 34.8 | 370 | 34.0 | 360 | 35.2 | 0.404 |
| I believe that I was sexually abused | 768 | 36.6 | 381 | 35.0 | 387 | 38.4 | 0.106 |
Table 2.
Prevalence of childhood traumatic experiences by domain, among those with and without schizophrenia
| Controls | Cases | |||||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | p value | ||||
| Total | 2097 | 1089 | 51.9 | 1008 | 48.1 | |||
| Physical/emotional abuse | 1671 | 79.7 | 829 | 76.1 | 842 | 83.5 | <0.0001 | |
| Neglect | 1447 | 69.0 | 714 | 65.6 | 733 | 72.7 | 0.0004 | |
| Sexual abuse | 1126 | 53.7 | 558 | 51.2 | 568 | 56.4 | 0.0191 | |
| Any trauma | 1900 | 90.6 | 949 | 87.1 | 951 | 94.4 | <0.0001 | |
| Cumulative trauma domains | 0 | 197 | 9.4 | 140 | 12.9 | 57 | 5.7 | <0.0001 |
| 1 | 493 | 23.5 | 255 | 23.4 | 238 | 23.6 | ||
| 2 | 470 | 22.4 | 236 | 21.7 | 234 | 23.2 | ||
| 3 | 937 | 44.7 | 458 | 42.1 | 479 | 47.5 | ||
Table 3.
Unadjusted and adjusted ORs of schizophrenia, among those who ever experienced each traumatic event domain, compared with those who never experienced each domain
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Trauma domain | OR | 95% CI | OR | 95% CI | OR | 95% CI | |||
| Physical/emotional abuse | 1.37 | 1.13 | 1.67 | 1.34 | 1.10 | 1.65 | 1.63 | 1.28 | 2.09 |
| Neglect | 1.37 | 1.15 | 1.64 | 1.35 | 1.13 | 1.61 | 1.23 | 1.00 | 1.52 |
| Sexual abuse | 1.16 | 0.99 | 1.36 | 1.15 | 0.97 | 1.35 | 1.22 | 1.00 | 1.48 |
| Any trauma | 2.25 | 1.66 | 3.06 | 2.21 | 1.63 | 2.99 | 2.05 | 1.45 | 2.91 |
CI, confidence interval.
Note: Model 2 adjusted for sex, education, age, urbanicity, locality; Model 3 adjusted for model 2 covariates + lifetime depression, lifetime alcohol use disorder, and lifetime cannabis use disorder.
Figure 1 and online Supplementary Table S1 present the prevalence of cumulative traumas within each latent domain. A substantial proportion of the sample reported experiencing the maximum number of traumas within the domains of physical/emotional abuse (15.6%), neglect (26.7%), and sexual abuse (18.2%). In the fully adjusted logistic regression models, there was evidence of a dose–response relationship in the number of physical/emotional abuse experiences, increasing from 1.23 (95% CI 0.86–1.76) to 2.44 (95% CI 1.61–3.71). Those with two and three neglect-type traumas had 1.63 (95% CI 1.17–2.28) and 1.32 (95% CI 0.96–1.81) times the odds of schizophrenia, compared with those who experienced no neglect. There was no clear dose response for sexual abuse events. The odds of schizophrenia increased with increases in cumulative trauma experiences (range: 1.85–2.14). Compared with unimputed models, estimates were slightly attenuated after imputation, though were not substantively different. All model estimates are presented fully in Table 4.
Fig. 1.
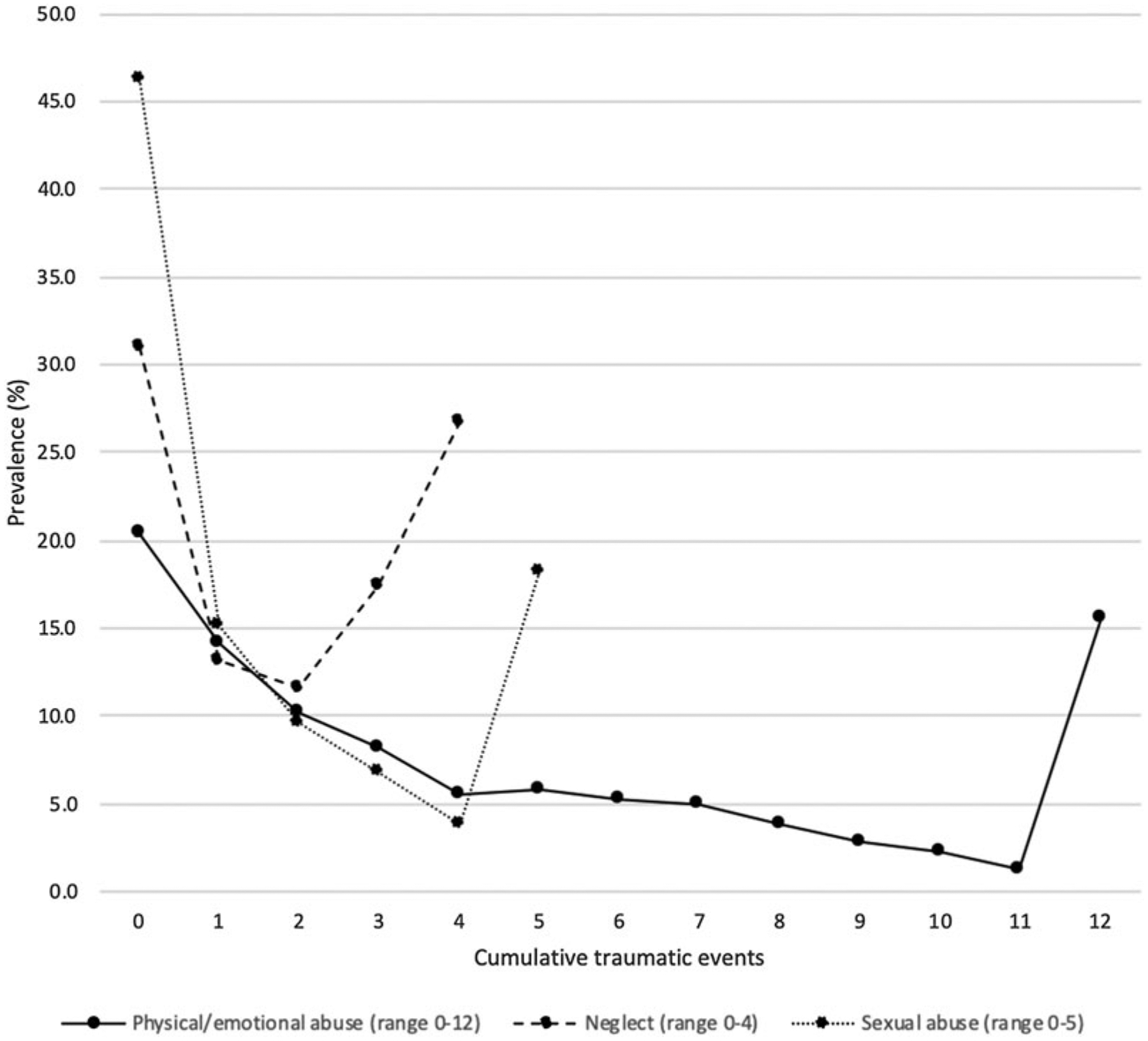
Cumulative proportion of traumatic events experienced for each domain.
Table 4.
Adjusted ORs of schizophrenia, by a number of cumulative traumatic events experienced in each domain, compared with no traumatic experiences
| Model 1 | Model 2 | Model 3 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number of traumatic events by domain (0 = ref) | OR | 95% CI | OR | 95% CI | OR | 95% CI | ||||
| Physical/emotional abuse | 1 | 1.07 | 0.79 | 1.43 | 1.06 | 0.79 | 1.43 | 1.23 | 0.86 | 1.76 |
| 2 | 1.40 | 1.02 | 1.94 | 1.41 | 1.02 | 1.95 | 1.78 | 1.21 | 2.62 | |
| 3+ | 1.88 | 1.33 | 2.65 | 1.87 | 1.32 | 2.65 | 2.44 | 1.61 | 3.71 | |
| Neglect | 1 | 1.22 | 0.93 | 1.59 | 1.22 | 0.93 | 1.59 | 1.26 | 0.92 | 1.72 |
| 2 | 1.60 | 1.21 | 2.11 | 1.58 | 1.20 | 2.08 | 1.63 | 1.17 | 2.28 | |
| 3+ | 1.52 | 1.19 | 1.94 | 1.51 | 1.18 | 1.92 | 1.32 | 0.96 | 1.81 | |
| Sexual abuse | 1 | 1.29 | 1.01 | 1.63 | 1.28 | 1.01 | 1.63 | 1.46 | 1.11 | 1.93 |
| 2 | 1.00 | 0.75 | 1.33 | 1.00 | 0.75 | 1.32 | 1.25 | 0.89 | 1.75 | |
| 3+ | 1.33 | 0.95 | 1.84 | 1.30 | 0.94 | 1.81 | 1.44 | 0.94 | 2.20 | |
| Any trauma domains | 1 | 2.11 | 1.50 | 2.97 | 2.09 | 1.49 | 2.93 | 1.85 | 1.25 | 2.74 |
| 2 | 2.34 | 1.67 | 3.28 | 2.31 | 1.65 | 3.25 | 2.11 | 1.43 | 3.12 | |
| 3+ | 2.28 | 1.66 | 3.13 | 2.21 | 1.61 | 3.03 | 2.14 | 1.49 | 3.08 | |
CI, confidence interval.
Note: Model 2 adjusted for sex, education, age, urbanicity, locality; Model 3 adjusted for model 2 covariates + lifetime depression, lifetime alcohol use disorder, and lifetime cannabis use disorder.
Discussion
This study sought to examine the prevalence of childhood traumas, whether exposure to childhood trauma is associated with increased risk of schizophrenia, and whether that risk increased with cumulative trauma exposure in a South African, Xhosa-speaking population. First, our findings suggest that childhood traumatic events are very common among controls as well as cases. Second, all three latent domains of physical/emotional abuse, neglect, and sexual abuse are nonetheless associated with an increased risk of schizophrenia, most evident for those who had more than one traumatic event within a domain. Third, there is some evidence of a dose–response relationship between the number of physical/emotional abuse experiences and schizophrenia. There are several strengths to the methodology of the study, including the care taken to translate instruments into Xhosa.
Our findings that childhood traumatic events are high among cases and controls are consistent with several previous studies examining trauma and related conditions in South Africa (Jewkes et al., 2016; Gibbs et al., 2018). Our results of the increased risk of schizophrenia among those who have experienced cumulative traumas are generally consistent with previous studies (Anda et al., 2006; van Os et al., 2008) including three systematic reviews of the relationship between childhood trauma and schizophrenia (Read et al., 2005; Matheson et al., 2012; Varese et al., 2012). We note that several studies of trauma in schizophrenia suggest that specific experiences of childhood trauma, e.g. physical or emotional neglect may have differential patterns of impact on various outcomes (i.e. premorbid adjustment, cognition and white matter abnormalities) (Kilian et al., 2017a, 2017b; Asmal et al., 2018). To our knowledge where previous studies have examined the relationship between childhood trauma and cognition in schizophrenia Kilian et al. (2017a), pre morbid adjustment (Kilian et al., 2017b) and white matter abnormalities (Asmal et al., 2018), no previous study has compared the relationship between childhood trauma and schizophrenia as outcome.
In modeling the exposure as cumulative traumatic events, we found evidence of potential threshold and dose–response effects. Experiencing a single physical/emotional abuse- and neglect-type event was not significantly associated with schizophrenia, and odds increased to significance among those who experienced 2 and 3+ events, in a dose–response manner for physical/emotional abuse. This may suggest that when experienced infrequently, children can overcome these forms of adversity without an increased risk of schizophrenia. In contrast, a single experience of sexual abuse was associated with elevated odds of disorder, emphasizing the severity of these particular experiences. Future research should further interrogate individual and accumulated traumas and the specific mechanisms underlying their potential differential effects.
These findings should be interpreted in light of several limitations. First, the case–control study design could be subject to recall bias where cases and controls could over or under report traumatic experiences. Also, the design limited our ability to determine the temporal ordering between each trauma and the onset of schizophrenia. It is plausible that traumatic experiences may have been a consequence of victimization after sub-clinical symptoms of schizophrenia (Beards et al., 2013; Tsigebrhan et al., 2014; Kraan et al., 2015), which might introduce bias due to reverse causation. Third, the psychological burden or social desirability of disclosing childhood trauma may have led to under-reporting of exposures (Susser and Widom, 2012). This type of misclassification may be non-differential, or under-reporting may have been greater among the cases, though both types of misclassification would have biased the study estimates toward a null association, as found by Widom and colleagues in their 2015 study of intergenerational childhood trauma (Widom et al., 2015). Fourth, the SAX survey recorded a limited set of covariates (sex, education, and age) which could be considered confounders in this study. As such, we consider the impact of unmeasured confounding as a source of bias. Fifth, we did not collect physician verified data of physical health conditions. Finally, the CTQ does not ask explicitly about the severity or duration of individual traumatic events. These characteristics should be considered in future research. We also suggest that future studies consider comorbid psychiatric conditions in schizophrenia, e.g. depression (Rössler et al., 2005; Peralta and Cuesta, 2009; Herniman et al., 2017) or substance use as potential interaction variables of the relationship between childhood trauma and schizophrenia (Sideli et al., 2018). Several studies suggest that childhood trauma is associated with mental disorders other than schizophrenia and further work is needed to determine whether there is specificity to these associations.
Conclusion
This study is a meaningful contribution to the literature examining childhood trauma in schizophrenia in low- and middle-income countries. The results strengthen the claim that childhood trauma is an important determinant for psychosis and schizophrenia and may be useful to consider when designing interventions to reduce psychosis incidence.
Supplementary Material
Acknowledgements.
We wish to acknowledge the support of Dr Adele Pretorius, project manager of the SAX study and the data team for their assistance with data management, quality control and access.
Financial support. The SAX study receives funding from the National Institute of Mental Health (NIMH: Grant number 5UO1MH096754) and is a member of the Human Heredity and Health in Africa Consortium (H3 Africa) (http:h3africa.org/). SM has received support from the Harry Crossley and National Research Foundation of South Africa’s post-doctoral research fellowships, a Claude Leon Foundation early career research award and a seed award from the School of Public Health, University of the Witwatersrand, Johannesburg, South Africa. SM has received funding from the Columbia University Southern African AIDS International Training/Research Program. JP has received support from National Institute of Mental Health (grant T32-MH1304346). DJS has received research grants and/or consultancy honoraria from Biocodex, Lundbeck, Servier, and Sun.
Footnotes
Supplementary material. The supplementary material for this article can be found at https://doi.org/10.1017/S0033291719001703.
References
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, Dube SR and Giles WH (2006) The enduring effects of abuse and related adverse experiences in childhood: a convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience 256, 174–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asmal L, Kilian S, du Plessis S, Scheffler F, Chiliza B, Fouche J-P, Seedat S, Dazzan P and Emsley R (2018) Childhood trauma associated white matter abnormalities in first-episode schizophrenia. Schizophrenia Bulletin 45(2), 369–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumeister D, Akhtar R, Ciufolini S, Pariante CM and Mondelli V (2016) Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-α. Molecular Psychiatry 21, 642–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beards S, Gayer-Anderson C, Borges S, Dewey ME, Fisher HL and Morgan C (2013) Life events and psychosis: a review and meta-analysis. Schizophrenia Bulletin 39(4), 740–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T,Stokes J, Handelsman L, Medrano M, Desmond D and Zule W (2003) Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse and Neglect 27, 169–190. [DOI] [PubMed] [Google Scholar]
- Bora E (2015) Neurodevelopmental origin of cognitive impairment in schizophrenia. Psychological Medicine 45, 1–9. [DOI] [PubMed] [Google Scholar]
- Campbell M, Susser E, Mall S, Mqulwana SG, Mndini MM, Ntola OA, Nagdee M, Zingela Z, Van Wyk S and Stein DJ (2017a) Using iterative learning to improve understanding during the informed consent process in a South African psychiatric genomics study. PLoS ONE 12(11), e0188466 10.1371/journal.pone.0188466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell MM, Sibeko G, Mall S, Baldinger A, Nagdee M, Susser E and Stein DJ (2017b) The content of delusions in a sample of South African Xhosa people with schizophrenia. BMC Psychiatry 17, 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello A and Osborne J (2005) Best practices in exploratory factor analysis : four recommendations for getting the most from your analysis. Practical Assessment, Research & Evaluation 10, 1–9. [Google Scholar]
- Dantchev S, Zammit S and Wolke D (2018) Sibling bullying in middle childhood and psychotic disorder at 18 years: a prospective cohort study. Psychological Medicine 48, 2321–2328. [DOI] [PubMed] [Google Scholar]
- Denckla CA, Consedine NS, Spies G, Cherner M, Henderson DC, Koenen KC and Seedat S (2017) Associations between neurocognitive functioning and social and occupational resilience among South African women exposed to childhood trauma. European Journal of Psychotraumatology 8, 1394146 10.1080/20008198.2017.1394146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn TJ, Baguley T and Brunsden V (2014) From alpha to omega: a practical solution to the pervasive problem of internal consistency estimation. British Journal of Psychology 105, 399–412. [DOI] [PubMed] [Google Scholar]
- Fink LA, Bernstein D, Handelsman L, Foote J and Lovejoy M (1995) Initial reliability and validity of the childhood trauma interview: a new multidimensional measure of childhood interpersonal trauma. American Journal of Psychiatry 152, 1329–1335. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M and Williams JBW (1997). Structured Clinical Interview for DSM-IVAxis I Disorders, Clinician Version (SCID-CV) for DSMIV.
- Fisher HL, McGuffin P, Boydell J, Fearon P, Craig TK, Dazzan P, Morgan K, Doody GA, Jones PB, Leff J, Murray RM and Morgan C (2014) Interplay between childhood physical abuse and familial risk in the onset of psychotic disorders. Schizophrenia Bulletin 40, 1443–1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerdner A and Allgulander C (2009) Psychometric properties of the Swedish version of the Childhood Trauma Questionnaire-Short Form (CTQ-SF). Nordic Journal of Psychiatry 63, 160–170. [DOI] [PubMed] [Google Scholar]
- Gibbs A, Dunkle K, Washington L, Willan S, Shai N and Jewkes R (2018) Childhood traumas as a risk factor for HIV-risk behaviours amongst young women and men living in urban informal settlements in South Africa: a cross-sectional study. PLoS ONE 13(4), e0195369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gil A, Gama CS, de Jesus DR, Lobato MI, Zimmer M and Belmonte-de-Abreu P (2009) The association of child abuse and neglect with adult disability in schizophrenia and the prominent role of physical neglect. Child Abuse and Neglect 33(9), 618–624. [DOI] [PubMed] [Google Scholar]
- Gunnar M and Quevedo K (2007) The neurobiology of stress and development. Annual Review of Psychology 58, 145–173. [DOI] [PubMed] [Google Scholar]
- Herniman SE, Allott KA, Killackey E, Hester R and Cotton SM (2017) The psychometric validity of the Center for Epidemiological Studies-Depression Scale (CES-D) in first episode schizophrenia spectrum. Psychiatry Research 252, 16–22. [DOI] [PubMed] [Google Scholar]
- Hu L and Bentler PM (1999) Structural equation modeling : a multidisciplinary journal cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling 6, 37–41. [Google Scholar]
- Jewkes RK, Dunkle K, Nduna M, Jama PN and Puren A (2010) Associations between childhood adversity and depression, substance abuse and HIV and HSV2 incident infections in rural South African youth. Child Abuse & Neglect 34(11), 833–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewkes R, Nduna M, Jama-Shai N, Chirwa E and Dunkle K (2016) Understanding the relationships between gender inequitable behaviours, childhood trauma and socio-economic status in single and multiple perpetrator rape in rural South Africa: structural equation modelling. PLoS ONE 11(5), e0154903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keefe RSE and Harvey PD (2012) Cognitive impairment in schizophrenia. Handbook of Experimental Pharmacology 213, 11–37. [DOI] [PubMed] [Google Scholar]
- Kenny DT, Lennings CJ and Nelson PK (2007) The mental health of young offenders serving orders in the community: implications for rehabilitation. Journal of Offender Rehabilitation 45, 123–148. [Google Scholar]
- Kilian S, Asmal L, Chiliza B, Olivier M, Phahladira L, Scheffler F, Seedat S, Marder S, Green M and Emsley R (2017a) Childhood adversity and cognitive function in schizophrenia spectrum disorders and healthy controls: evidence for an association between neglect and social cognition. Psychological Medicine 48(13), 2186–2193. [DOI] [PubMed] [Google Scholar]
- Kilian S, Burns JK, Seedat S, Asmal L, Chiliza B, du Plessis M, Olivier R, Kidd M and Emsley R. (2017b) Factors moderating the relationship between childhood trauma and premorbid adjustment in first-episode schizophrenia. PLoS ONE 12(1), e0170178 10.1371/journal.pone.0170178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koen L, Niehaus DJH, Wright G, Warnich L, de Jong G, Emsley RA and Mall S (2012) Chromosome 22q11 in a Xhosa schizophrenia population. South African Medical Journal 102, 165–166. [DOI] [PubMed] [Google Scholar]
- Kraan T, Velthorst E, Smit F, de Haan L and van der Gaag M (2015) Trauma and recent life events in individuals at ultra high risk for psychosis: review and meta-analysis. Schizophrenia Research 161, 143–149. [DOI] [PubMed] [Google Scholar]
- Lochner C, Seedat S, Allgulander C, Kidd M, Stein D and Gerdner A (2010) Childhood trauma in adults with social anxiety disorder and panic disorder: a cross-national study. African Journal of Psychiatry 13, 376–381. [DOI] [PubMed] [Google Scholar]
- MacDonald K, Thomas ML, MacDonald TM and Sciolla AF (2014) A perfect childhood? Clinical correlates of minimization and denial on the childhood trauma questionnaire. Journal of Interpersonal Violence 30, 988–1009. [DOI] [PubMed] [Google Scholar]
- Mandelli L, Petrelli C and Serretti A (2015) The role of specific early trauma in adult depression: a meta-analysis of published literature. Childhood trauma and adult depression. European Psychiatry 30, 665–680. [DOI] [PubMed] [Google Scholar]
- Martin L, Viljoen M, Kidd M and Seedat S (2014) Are childhood trauma exposures predictive of anxiety sensitivity in school attending youth? Journal of Affective Disorders 168, 5–12. [DOI] [PubMed] [Google Scholar]
- Matheson SL, Shepherd AM, Pinchbeck RM, Laurens KR and Carr VJ (2012) Childhood adversity in schizophrenia: a systematic meta-analysis. Psychological Medicine, 1–13. [DOI] [PubMed] [Google Scholar]
- McCrory E, De Brito SA and Viding E (2011) The impact of childhood maltreatment: a review of neurobiological and genetic factors. Frontiers in Psychiatry 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrath RE, Mitchell M, Kim BH and Hough L (2010) Evidence for response bias as a source of error variance in applied assessment. Psychological Bulletin 136, 450–470. [DOI] [PubMed] [Google Scholar]
- Menon B, Cherkil S, Aswathy S, Unnikrishnan A and Rajani G (2012) The process and challenges in the translation of World health organization quality of Life (WHOQOL-BREF) to a regional language; Malayalam. Indian Journal of Psychological Medicine 34, 149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan C and Fisher H (2007) Environmental factors in schizophrenia: childhood trauma – a critical review. Schizophrenia Bulletin 33, 3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce N (2016) Analysis of matched case-control studies. BMJ (Clinical Research Ed.) 10.1136/bmj.i969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peralta V and Cuesta MJ (2009) Characterization of affective domains within the nonaffective psychotic disorders. Schizophrenia Research 111(1–3), 61–69. [DOI] [PubMed] [Google Scholar]
- Powers A, Fani N, Cross D, Ressler KJ and Bradley B (2016) Childhood trauma, PTSD, and psychosis: findings from a highly traumatized, minority sample. Child Abuse and Neglect 58, 111–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read J, Van Os J, Morrison AP and Ross CA (2005) Childhood trauma, psychosis and schizophrenia: a literature review with theoretical and clinical implications. Acta Psychiatrica Scandinavica 112, 330–350. [DOI] [PubMed] [Google Scholar]
- Rössler W, Joachim Salize H, Van Os J and Riecher-Rössler A (2005) Size of burden of schizophrenia and psychotic disorders. European Neuropsychopharmacology 15, 399–409. [DOI] [PubMed] [Google Scholar]
- Rubin DB (1987) Multiple Imputation for Nonresponse in Surveys Donald B. Rubin. Wiley Series in Probability and Statistics. [Google Scholar]
- Seaman JB, Terhorst L, Gentry A, Hunsaker A, Parker LS and Lingler JH (2015) Psychometric properties of a decisional capacity screening tool for individuals contemplating participation in Alzheimer’s disease research. Journal of Alzheimer’s Disease 46, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sideli L, Fisher HL, Murray RM, Sallis H, Russo M, Stilo SA, Paparelli A, Wiffen BDR, O’Connor JA, Pintore S, Ferraro L, La Cascia C, LaBarbera D, Morgan C and Di Forti M (2018) Interaction between cannabis consumption and childhood abuse in psychotic disorders: preliminary findings on the role of different patterns of cannabis use. Early Intervention in Psychiatry 12, 135–142. [DOI] [PubMed] [Google Scholar]
- Spies G and Seedat S (2014) Depression and resilience in women with HIV and early life stress: does trauma play a mediating role? A cross-sectional study. BMJ Open 4, e004200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spies G, Ahmed-Leitao F, Fennema-Notestine C, Cherner M and Seedat S (2016) Effects of HIV and childhood trauma on brain morphometry and neurocognitive function. Journal of NeuroVirology 22, 149–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M and First MB (1992) The Structured Clinical Interview for DSM-III-R (SCID): I: history, rationale, and description. Archives of General Psychiatry 49, 624–629. [DOI] [PubMed] [Google Scholar]
- Susser E and Widom CS (2012) Still searching for lost truths about the bitter sorrows of childhood. Schizophrenia Bulletin 38, 672–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trotta A, Di Forti M, Mondelli V, Dazzan P, Pariante C, David A, Mulè A, Ferraro L, Formica I, Murray RM and Fisher HL (2013) Prevalence of bullying victimisation amongst first-episode psychosis patients and unaffected controls. Schizophrenia Research 150, 169–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trotta A, Murray RM and Fisher HL (2015) The impact of childhood adversity on the persistence of psychotic symptoms: a systematic review and meta-analysis. Psychological Medicine 150, 1–18. [DOI] [PubMed] [Google Scholar]
- Tsigebrhan R, Shibre T, Medhin G, Fekadu A and Hanlon C (2014) Violence and violent victimization in people with severe mental illness in a rural low-income country setting: a comparative cross-sectional community study. Schizophrenia Research 152, 275–282. [DOI] [PubMed] [Google Scholar]
- Tucci AM, Kerr-Corrêa F and Souza-Formigoni MLO (2010) Childhood trauma in substance use disorder and depression: an analysis by gender among a Brazilian clinical sample. Child Abuse & Neglect 34, 95–104. [DOI] [PubMed] [Google Scholar]
- van Dam DS, van der Ven E, Velthorst E, Selten JP, Morgan C and de Haan L (2012) Childhood bullying and the association with psychosis in non-clinical and clinical samples: a review and meta-analysis. Psychological Medicine 42, 2463–2474. [DOI] [PubMed] [Google Scholar]
- van Os J, Rutten BP and Poulton R (2008) Gene-environment interactions in schizophrenia: review of epidemiological findings and future directions. Schizophrenia Bulletin 34, 1066–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, Read J, Van Os J and Bentall RP (2012) Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophrenia Bulletin 38, 661–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wall MM and Amemiya Y (2000) Estimation for polynomial structural equation models. Journal of the American Statistical Association 95, 929–940. [Google Scholar]
- Widom CS, Czaja SJ and DuMont KA (2015) Intergenerational transmission of child abuse and neglect: real or detection bias? Science 347, 1480–1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


