ABSTRACT
Background
American Indians and Alaska Natives experience diet-related health disparities compared with non-Hispanic whites. Navajo Nation's colonial history and remote setting present unique challenges for healthy food access.
Objective
This study aims to understand the impact of the Healthy Navajo Stores Initiative (HNSI) on fruit and vegetable purchasing on Navajo Nation.
Methods
We conducted a cross-sectional survey of 692 customers shopping at 28 convenience stores, trading posts, and grocery stores on Navajo Nation. Individual- and household-level sociodemographic data and food purchasing behaviors were collected. Descriptive and bivariate analyses for customers’ individual- and household-level characteristics were conducted using chi-squared tests. The impact of individual-, household-, and store-level factors on fruit and vegetable purchasing was assessed using multiple logistic regression modeling.
Results
Store participation in the HNSI was significantly associated with customers’ purchase of produce. Customers experienced 150% higher odds of purchasing produce if they shopped in participating stores, compared with nonparticipating stores (P < 0.001). Store type was strongly associated with customers’ purchase of fruits or vegetables. Customers shopping at a grocery store had 520% higher odds of purchasing produce than did customers shopping at convenience stores (P < 0.001). Customers shopping at trading posts had 120% higher odds of purchasing fruits or vegetables than did customers shopping at convenience stores (P = 0.001).
Conclusions
Our findings reveal increased produce purchasing at stores participating in the HNSI. Customers were significantly more likely to purchase fruits or vegetables in stores enrolled in a healthy store intervention than in nonenrolled stores, after controlling for quantity of produce stocked and store type. Customers shopping in grocery stores and trading posts were significantly more likely to purchase produce than customers shopping in convenience stores. These findings have implications for food access in rural tribal communities.
Keywords: health promotion/methods, fruits, vegetables, American Indians, Alaska Natives, adult, health behavior, health disparity
Introduction
American Indians and Alaska Natives (AIs/ANs) experience health disparities compared with the general US population (1). AI/AN individuals are more than twice as likely to have diabetes and obesity as are non-Hispanic whites (2–4). These health disparities are likely in part due to high poverty levels, access barriers and discrimination in health care delivery, and a long history of racist laws and policies that have systematically disrupted indigenous food systems (5–9).
These structural factors contribute to limited healthy, affordable food access in AI/AN communities, particularly on rural reservations. A recent USDA study found that only 25.6% of all tribal communities lived within 1 mile of a supermarket, compared with 58.8% of the general US population (10). Grocery store inaccessibility has been shown to be associated with decreased shopping frequency and increased obesity prevalence (11). In contrast, local affordability and variety of produce are associated with increased purchasing and consumption (12, 13). In addition to geographic barriers, food access is also limited by disproportionately high poverty rates experienced by AI/AN individuals and communities. One-half of all AI/AN individuals have incomes ≤200% of the Federal Poverty Level (10).
Navajo Nation provides an exemplar of these structural challenges and their resulting impact on health outcomes. Almost the entire Navajo Nation is classified as a food desert by the USDA (14). Only 13 grocery stores operate within the reservation, an area the size of West Virginia (15). Grocery stores and small retailers on Navajo Nation predominately offer highly processed foods with low nutritional value, and at higher prices than off-reservation stores (6, 15, 16). Stores on Navajo Nation stock limited varieties and quantities of fruits and vegetables [(6); unpublished Navajo Nutrition Environment Measurement Survey in Stores (NEMS-S) assessment conducted by the authors]. This combination of limited accessibility to grocery stores and high prices has tangible impacts on food security and health. Navajo Nation's food insecurity rates are among the highest reported in the United States, at 76.7% (17, 18). Household food insecurity is associated with increased risks of overweight, obesity, hypertension, and type 2 diabetes (19–22).
Responding to this challenge, our organization launched the Healthy Navajo Stores Initiative (HNSI) in 2014. This was a multifaceted intervention, drawing from national “Healthy Corner Store” best practices. Store owners across Navajo Nation were invited to participate in the HNSI; if they accepted, our team helped owners identify and implement changes in 4 areas: store environment, promotion, staff training, and participation in a local food voucher program. Environmental changes included produce placement in the front of the store or at the points of sale, as well as acquisition of produce shelves and coolers. Stores were offered free, culturally adapted promotional materials including shelf talkers, labels, and recipe cards to promote produce. We offered staff training on produce handling to maintain freshness and promote longevity. Stores that met predefined produce stocking requirements were also invited to participate in a local voucher program, the Navajo Fruit and Vegetable Prescription Program (FVRx), in which local health care teams prescribed vouchers to families with children or mothers at risk of obesity, diabetes, or food insecurity. “FVRx stores” were qualified to accept vouchers from families in turn, receiving reimbursement for the vouchers via our organization.
The objective of this study was to investigate if the HNSI was associated with increased produce purchasing on Navajo Nation. We hypothesized that store participation in the intervention was associated with customer produce purchasing, compared with nonparticipating stores. A secondary aim of the study was to identify other individual and store characteristics associated with healthier purchasing behavior.
Methods
Study setting
The Navajo Nation is located in the Four Corners region of the Southwest United States, spanning 27,000 square miles in New Mexico, Arizona, and Utah. In 2013, we collected data on stores from a 2011 national proprietary data set of businesses from InfoUSA, supplemented with information from the Yellow Pages and calls to all local communities (Chapters). InfoUSA uses standardized criteria verified by businesses to assign Standard Industrial Classification to define the store type. A total of 13 grocery stores and 99 small stores were identified on Navajo Nation.
We also categorized stores into 3 groups. Convenience stores are small stores that are corporately owned, attached to a gas station, and often stock snack foods and limited amounts of grocery items. By contrast, trading posts are independently owned stores that often stock groceries, many of which are dried or canned goods; traditional food items (e.g., blue corn meal, juniper berries); and Navajo-made pottery, rugs, and jewelry. Finally, grocery stores are larger stores that stock a wide variety of food items.
Sampling approach
From June to December 2016, we conducted a cross-sectional survey of customers at 28 stores (5 grocery, 16 convenience, and 7 trading posts) on Navajo Nation. Stores participating in the HNSI were matched with nonparticipating stores, based on the baseline (2013) Fruit and Vegetable Index (FVI), a measure of the quantity of fruits and vegetables stocked in a store. At the time of the survey period, stores had participated in the HNSI for ≥1 y.
The day and time of each customer intercept survey were randomized using computer-generated assignment based on 3 variables: weekday/weekend, beginning/end of month, and AM/PM. Surveys were conducted within the randomly assigned time and day constraints at each store. A minimum of 2 different store visits to intercept customers were made at each store to provide a broader sample of shopping behavior. Each of the 2 visits per store was randomized separately. The study team aimed to intercept 12–15 customers at each store visit, for a total goal of 30 customers per store. In 5 stores, low numbers of shoppers necessitated >2 visits to conduct surveys.
Customers exiting the store were consecutively approached during each store visit. Customer eligibility criteria included 1) 18 y of age or older; 2) not currently pregnant or breastfeeding; 3) a primary food shopper in their household; and 4) living on Navajo Nation. Willing customers were interviewed by trained research assistants outside of stores. Among 739 customers approached, 692 customers met the eligibility criteria and were surveyed. Information on customers who refused to participate was not collected, but the main reason for refusal was lack of time.
Data collection
Tablet-based surveys were conducted by 7 trained Navajo research assistants and the study supervisor. Participants were given a reusable grocery bag and water bottle upon completion of the survey. On average, the survey took 7 min to complete.
All project evaluation was approved by the Navajo Nation Human Research Review Board and deemed exempt by Partners Healthcare Institutional Review Board.
Measurements
The consumer intercept survey used in this study was adapted from previous studies (13, 23) for use in a multiphase longitudinal study to evaluate the HNSI. The survey instrument (Supplement 1) was pilot tested at 3 distinct store locations. Feedback from Navajo staff and community members regarding word choice, reading level, and cultural competency was incorporated. Although the final survey was deemed comprehensible and culturally appropriate by Navajo stakeholders, formal validation of the survey instrument was not conducted.
Food shopping behavior questions included where customers did the majority of their food shopping, shopping frequency at the current store, and knowledge of whether the current store sold fresh fruits and vegetables. Customers were first asked if they had bought any fresh or frozen fruits or vegetables that day at the store. Customers were presented with a list of fresh and frozen produce items, including photos, from which to choose. The food items included 1) fresh fruits (12 types and an “other” category); 2) frozen fruits (8 types and an “other” category); 3) fresh vegetables (16 types and an “other” category); and 4) frozen vegetables (14 types and an “other” category). Customers were then asked if they had bought any fresh or frozen fruits or vegetables within the past week at the store.
Sociodemographic information collected included age, sex, education, and employment. Household demographic information included size of household, household food security, participation in assistance programs including the Supplemental Nutrition Assistance Program (SNAP) and Food Distribution Program on Indian Reservations (FDPIR), electricity in the home, presence of a reliable refrigerator, presence of a sink with running water, food production, usual mode of transport to the store at which the interview occurred, and travel time from home to the current store. Although household food security was not formally measured, we explored food security with the following question: “In the past month, were you worried (at any time) that you wouldn't have enough food to feed your family?”
Data on the store environment were collected using the NEMS-S (15, 22), which was modified for use in the Navajo Nation by the authors. Store information included type of store (convenience compared with trading post compared with grocery), FVI score, and participation in the HNSI. The FVI score was derived from adapted recommendations by the Robert Wood Johnson Foundation (RWJF) on healthful produce stocking levels for small retail food stores (Figure 1) (24). The RWJF recommendations define 2 categories of stores—“Basic” and “Preferred”—based on the quantity of fruits and vegetables available. With these criteria as a foundation, we used data collected from the Navajo NEMS-S survey and thresholds that were felt to be locally achievable and meaningful to community members to derive the FVI: an “excellent” store must have ≥6 different types of fruit, ≥3 of which must be fresh, and ≥8 types of vegetables, ≥4 of which must be fresh. A “good” store must have ≥4 types of fruit, ≥2 of which must be fresh, and 6 types of vegetables, ≥4 of which must be fresh. Only fresh and frozen fruits and vegetables were considered qualifying items, and to qualify, frozen vegetables must have low or no sodium content, and frozen fruit must have no added sugar. HNSI participation by stores was determined based on the list of stores actively participating in the HNSI program via the implementing team. Of note, all HNSI stores were redeeming FVRx vouchers at the time of the survey or had been a redemption site within the past year.
FIGURE 1.
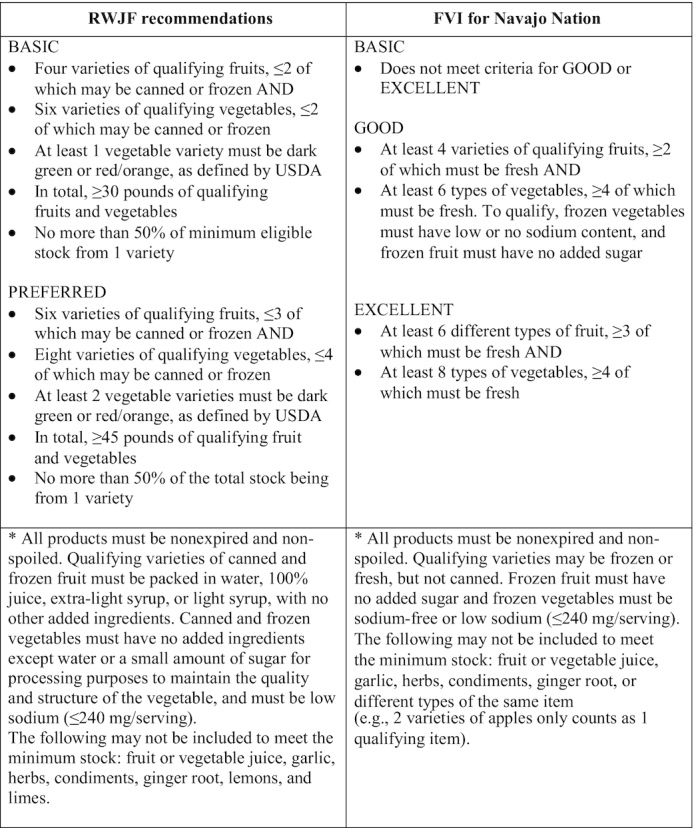
Small store produce stocking levels—RWJF recommendations and the FVI. FVI, Fruit and Vegetable Index; RWJF, Robert Wood Johnson Foundation.
Data analysis
The key outcome variable was fruit or vegetable purchasing, defined as purchase of ≥1 type of fruit or vegetables (fresh or frozen) within the last week, at the store of survey completion. The outcome variable of fruit or vegetable purchasing is also referred to as fruits or vegetables purchasing or produce purchasing throughout the article. The independent variables examined were age, sex, employment, education, household size, household food security, receipt of food assistance, family food production, household electricity, household refrigeration, household running water, shopping frequency, transportation to store, travel time to store, type of store, FVI, and HNSI participation.
Data were analyzed using Stata 14 software (StataCorp LP) (25). Descriptive and bivariate analyses for customers’ individual- and household-level characteristics (Table 1) and for store-level characteristics (Table 2) were conducted using chi-squared tests for categorical data. Descriptive statistics for surveyed stores were calculated using data from the Navajo NEMS-S assessment. Spearman's rank correlation coefficients were used to assess potential collinearity among independent variables. Multiple logistic regression modeling was used to assess the impact of individual-, household-, and store-level factors on fruit and vegetable purchasing, controlling for potential covariates. The final logistic regression model assesses the impact of factors on fruit and vegetable purchasing, adjusting for age, sex, education, shopping frequency, travel time to store, type of store, FVI, HNSI participation, household size, receipt of food assistance, household refrigeration, and household running water. Variables were included in the model if their unadjusted association with fruit and vegetable purchasing was statistically significant at a level of P < 0.2 (Table 3). Logistic regression significance was established at the P < 0.05 level.
TABLE 1.
Individual and household characteristics, by purchase of ≥1 fruit or vegetable within the last week1
| Characteristic | n (%) (n = 692) | Did not buy fruits or vegetables (n = 408) | Bought fruits or vegetables (n = 284) | χ2P value |
|---|---|---|---|---|
| Age, y | <0.001 | |||
| 18–29 | 61 (8.8) | 30 (7.4) | 31 (11.0) | |
| 30–44 | 151 (21.9) | 70 (17.2) | 81 (28.6) | |
| 45–59 | 255 (36.9) | 146 (35.8) | 109 (38.5) | |
| ≥60 | 224 (32.4) | 162 (39.7) | 62 (21.9) | |
| Sex | 0.042 | |||
| Male | 158 (22.9) | 104 (25.6) | 54 (19.0) | |
| Female | 532 (77.1) | 302 (74.4) | 230 (81.0) | |
| Employment | 0.44 | |||
| Employed full time | 223 (32.5) | 127 (31.4) | 96 (34.2) | |
| Education | 0.024 | |||
| <High school | 175 (25.6) | 90 (22.4) | 85 (30.3) | |
| High school | 365 (53.4) | 217 (54.0) | 148 (52.7) | |
| ≥College degree | 143 (20.9) | 95 (23.6) | 48 (17.1) | |
| Shopping frequency at store | <0.001 | |||
| Weekly or more | 497 (72.2) | 257 (63.5) | 240 (84.8) | |
| Biweekly to monthly | 138 (20.1) | 101 (24.9) | 37 (13.1) | |
| Few times per year | 53 (7.7) | 47 (11.6) | 6 (2.1) | |
| Transportation to store | 0.36 | |||
| Get a ride or walk | 90 (13.1) | 57 (14.0) | 33 (11.7) | |
| Drive oneself | 599 (86.9) | 349 (86.0) | 250 (88.3) | |
| Travel time to store, min | <0.001 | |||
| ≤5 | 163 (23.6) | 96 (23.5) | 67 (23.6) | |
| 6–30 | 363 (52.5) | 187 (45.8) | 176 (62.0) | |
| 31–60 | 117 (16.9) | 84 (20.6) | 33 (11.6) | |
| >60 | 49 (7.1) | 41 (10.1) | 8 (2.8) | |
| Household size, persons | <0.001 | |||
| 1–2 | 242 (35.0) | 168 (41.2) | 74 (26.1) | |
| 3–5 | 323 (46.7) | 175 (42.9) | 148 (52.1) | |
| ≥6 | 127 (18.4) | 65 (15.9) | 62 (21.8) | |
| Worried about having enough food2 | 386 (56.2) | 235 (58.0) | 151 (53.6) | 0.24 |
| Receiving food assistance2,3 | 286 (41.3) | 142 (34.8) | 144 (50.7) | <0.001 |
| Family food production2 | 425 (61.4) | 246 (60.3) | 179 (63.0) | 0.47 |
| Household electricity2 | 613 (89.2) | 366 (90.4) | 247 (87.6) | 0.25 |
| Household refrigeration2 | 621 (90.4) | 373 (92.1) | 248 (87.9) | 0.07 |
| Household running water2 | 590 (85.8) | 354 (87.4) | 236 (83.4) | 0.14 |
n = 692. n may not sum to 692 owing to missing data and percentages may not sum to 100% because of rounding.
Binary variable with only 1 outcome reported.
Receiving food assistance defined for this study as participation in the Supplemental Nutrition Assistance Program or the Food Distribution Program on Indian Reservations.
TABLE 2.
Store-level characteristics, by purchase of ≥1 fruit or vegetable within the last week1
| Characteristic | n (%) (n = 692) | Did not buy fruits or vegetables (n = 408) | Bought fruits or vegetables (n = 284) | χ2P value |
|---|---|---|---|---|
| Type of store | <0.001 | |||
| Convenience | 381 (55.1) | 260 (63.7) | 121 (42.6) | |
| Trading post | 177 (25.6) | 109 (26.7) | 68 (23.9) | |
| Grocery | 134 (19.4) | 39 (9.6) | 95 (33.5) | |
| Fruit and Vegetable Index | <0.001 | |||
| <Good/excellent | 277 (40.0) | 186 (45.6) | 91 (32.0) | |
| Good/excellent | 415 (60.0) | 222 (54.4) | 193 (68.0) | |
| HNSI status | <0.001 | |||
| Non-HNSI store | 429 (62.0) | 288 (70.6) | 141 (49.7) | |
| HNSI store | 263 (38.0) | 120 (29.4) | 143 (50.4) |
n = 692. n may not sum to 692 owing to missing data and percentages may not sum to 100% because of rounding. HNSI, Healthy Navajo Stores Initiative.
TABLE 3.
Logistic regression model of factors associated with purchase of ≥1 fruit or vegetable within the last week1
| Characteristic | Unadjusted OR (95% CI) | χ2P value | Adjusted OR (95% CI) | χ2P value |
|---|---|---|---|---|
| Age, y (ref: 18–29) | ||||
| 30–44 | 1.1 (0.6, 2.0) | 0.709 | 1.6 (0.8, 3.1) | 0.20 |
| 45–59 | 0.7 (0.4, 1.3) | 0.255 | 1.1 (0.6, 2.1) | 0.81 |
| ≥60 | 0.4 (0.2, 0.7) | 0.001 | 0.5 (0.2, 0.9) | 0.034 |
| Sex (ref: male) | ||||
| Female | 1.5 (1.0, 2.1) | 0.043 | 1.7 (1.1, 2.6) | 0.026 |
| Education (ref: <high school) | ||||
| High school | 0.7 (0.5, 1.0) | 0.079 | 0.6 (0.4, 0.9) | 0.019 |
| ≥College degree | 0.5 (0.3, 0.8) | 0.007 | 0.4 (0.2, 0.8) | 0.006 |
| Shopping frequency at store (ref: weekly or more) | ||||
| Biweekly to monthly | 0.4 (0.3, 0.6) | <0.001 | 0.3 (0.2, 0.6) | <0.001 |
| Few times per year | 0.1 (0.1, 0.3) | <0.001 | 0.1 (0.1, 0.4) | <0.001 |
| Travel time to store, min (ref: ≤5) | ||||
| 6–30 | 1.3 (0.9, 2.0) | 0.117 | 1.4 (0.9, 2.1) | 0.18 |
| 31–60 | 0.6 (0.3, 0.9) | 0.027 | 0.6 (0.3, 1.1) | 0.12 |
| >60 | 0.3 (0.1, 0.6) | 0.002 | 0.5 (0.2, 1.3) | 0.16 |
| Store type (ref: convenience store) | ||||
| Trading post | 1.3 (0.9, 1.9) | 0.122 | 2.2 (1.4, 3.4) | 0.001 |
| Grocery store | 5.2 (3.4, 8.1) | <0.001 | 6.2 (3.4, 11.1) | <0.001 |
| Fruit and Vegetable Index (ref: <good/excellent) | ||||
| Good/excellent | 1.8 (1.3, 2.4) | <0.001 | 1.5 (1.0, 2.3) | 0.07 |
| HNSI store (ref: non-HNSI store) | 2.4 (1.8, 3.3) | <0.001 | 2.5 (1.6, 3.7) | <0.001 |
| Household size, persons (ref: 1–2) | ||||
| 3–5 | 1.9 (1.4, 2.7) | <0.001 | 1.6 (1.0, 2.5) | 0.041 |
| ≥6 | 2.2 (1.4, 3.4) | <0.001 | 1.4 (0.8, 2.4) | 0.23 |
| Receiving food assistance2 (ref: not receiving assistance) | 1.9 (1.4, 2.6) | <0.001 | 1.2 (0.8, 1.9) | 0.28 |
| Household refrigeration (ref: no refrigeration) | 0.6 (0.4, 1.0) | 0.071 | 1.0 (0.5, 2.1) | 0.98 |
| Household running water (ref: no running water) | 0.7 (0.5, 1.1) | 0.139 | 1.2 (0.6, 2.3) | 0.57 |
n = 692. n may not sum to 692 owing to missing data and percentages may not sum to 100% because of rounding. HNSI, Healthy Navajo Stores Initiative.
Receiving food assistance defined for this study as participation in the Supplemental Nutrition Assistance Program or the Food Distribution Program on Indian Reservations.
Results
Individual- and household-level customer characteristics
A total of 692 customers were eligible and consented to be surveyed, providing a participation rate of 93.6% (Table 1). The sample was predominately female (77.1%). The average age of customers was 51.1 y, with 32.4% of respondents being 60 y old or older and only 8.8% of respondents being 18–29 y old. The majority of respondents were employed less than full time (67.5%) and had achieved a high school degree as their highest level of formal education (53.4%). Shopping frequency was relatively high, with 72.2% of customers shopping at the surveyed store at least once per week. A majority of customers drove themselves to the store where they were surveyed (86.9%). Customers’ average travel time to the store was 33 min (range: 0–900 min), with 24.0% of respondents traveling >30 min. The majority of customers were surveyed at a convenience store (55.1%) and at a store with a “Good/Excellent” FVI score (60.0%). The average household size was 3.7 people, with 18.4% of customers living in households with >5 people (Table 1). A large proportion of customers reported they were worried about having enough food to feed their family (43.8%) and a similarly large proportion received food assistance through SNAP or FDPIR (41.3%). A majority of customers (61.4%) grew food for consumption, through either personal or family engagement in farming, gardening, or ranching. A relatively large proportion of households did not have electricity (10.8%), reliable refrigeration (9.6%), or running water (14.2%).
Survey store characteristics
The majority of surveyed stores were convenience stores (57.1%), followed by trading posts (25.9%) and grocery stores (18.5%). The majority of surveyed stores (60.7%) met the “Good/Excellent” FVI threshold, with 39.3% falling below this threshold. At the time of the survey, 35.7% of stores either were current HNSI stores or had been participating sites within the past year.
Bivariate analysis of customer shopping behavior
Customers who purchased any fruits or vegetables tended to be younger than nonproduce purchasers (P < 0.001) (Table 1). Among those who purchased produce, a greater proportion were female than among those who did not purchase produce (P = 0.04). A greater proportion of customers who purchased fruits or vegetables had completed less than a high school degree, than of customers who did not purchase fruits or vegetables (P = 0.02). A greater proportion of produce purchasers shopped at least once per week than of nonproduce purchasers (P < 0.001). Decreased travel time was also significantly associated with fruits or vegetables purchase (P < 0.001); a greater proportion of customers buying fruits or vegetables traveled ≤30 min to the store, than of customers who did not purchase fruits or vegetables. Customers’ method of transportation to the store was not significantly associated with purchasing of fruits or vegetables (P = 0.36). Full-time employment was also not significantly associated with purchasing of fruits or vegetables (P = 0.44).
A greater proportion of customers buying fruits or vegetables lived in larger households, than of those not purchasing produce (P < 0.001) (Table 1). Produce purchasing was also significantly associated with participation in food assistance programs; SNAP or FDPIR participants made up a larger proportion of individuals purchasing produce than of those who did not purchase produce (P < 0.001). Household food security (P = 0.24) and food production (P = 0.47) did not significantly vary by purchase of fruits or vegetables. Household electricity (P = 0.25), running water (P = 0.14), and refrigeration (P = 0.07) also did not significantly vary by fruits or vegetables purchase.
Produce purchasing was significantly associated with several store-level factors, including type of store (P < 0.001), FVI score (P < 0.001), and FVRx participation (P < 0.001) (Table 2). A greater proportion of customers purchasing produce shopped at grocery stores, stores with FVI ratings of “Good/Excellent,” and stores that redeemed FVRx prescriptions, than of customers who did not purchase produce.
Multivariable logistic regression analysis of shopping behaviors
Multivariable analysis showed that store participation in the HNSI program was strongly associated with customers’ purchase of fruits or vegetables. Customers experienced 150% higher odds of purchasing produce if they shopped in HNSI stores, compared with non-HNSI stores (P < 0.001) (Table 3), controlling for FVI score, type of store, and other potential covariates. Store type was also significantly associated with customers’ purchase of fruits or vegetables. Customers shopping at a grocery store had 520% higher odds of purchasing produce than customers shopping at convenience stores (P < 0.001). Customers shopping at trading posts had 120% higher odds of purchasing fruits or vegetables than customers shopping at convenience stores (P = 0.001).
Discussion
Our study findings reveal increased healthy purchasing at stores participating in a multifaceted healthy store intervention implemented on a tribal nation. This finding is particularly relevant because it suggests that a multilevel store intervention—offering a suite of strategies to partnering stores including participation in a fruit and vegetable prescription program—may be associated with increased fruit and vegetable purchasing across a variety of store types. The combination of produce prescriptions along with environmental and promotional strategies may be particularly effective for stores in rural settings, because vouchers may provide monetary incentive and mitigate the risk of stocking increased fresh produce.
Our findings also highlight the importance of food environments for customers’ purchasing behaviors in an American Indian reservation. To our knowledge, this is the first study to demonstrate the relation between type of store and the likelihood of produce purchasing in an AI/AN population or a rural setting. This finding is supported by previous research demonstrating that customers shopping in large grocery stores purchase more fruits and vegetables than those shopping in small grocery, specialty, or convenience stores, in an off-reservation urban setting (26). It is possible that trading posts being independently owned allowed them to more easily adopt healthy store interventions (i.e., moving the produce cooler to the front of the store) and respond to customer requests for produce. In addition, trading posts have had long-standing presences in many Navajo communities as sources of dry goods and other traditional food items; customers may be more likely to purchase fruits and vegetables in a store that they already associate with food purchasing than in convenience stores. Although our findings should not exclude convenience stores from participation in future food environment interventions, the importance of store type for customers’ healthy purchasing behavior should be considered when designing intervention dosage and delivery.
Associations between individual-level factors, including age, sex, employment, household size, and food assistance, and fruit and vegetable purchasing were in line with expectations. After multivariable analysis, increased shopping frequency was found to be significantly associated with increased fruits or vegetables purchasing, but travel time to the store was not. Our findings are supported by previous research demonstrating that fruit and vegetable consumption is more closely associated with grocery store choice and frequency of shopping trips than with physical distance to a grocery store (27, 28).
More research is needed to fully understand the factors associated with shopping frequency on Navajo Nation so that food access programming can effectively intervene on the most relevant barriers.
Limitations
Our research has several limitations. The study's design resulted in a convenience sampling of customers exiting stores. It is possible that customers who declined to participate had purchasing habits distinct from those of participating customers, introducing a potential for response bias. However, given that only 6.4% of approached customers refused to participate, we feel confident in the validity of our findings. In addition, the survey instrument did not include measures of fruit or vegetable consumption and shopping behavior was based on self-reported purchasing of fruits or vegetables, rather than direct observations or sales data. Although this approach introduces the possibility of participant bias, our methodology is less intrusive and comparable with recent evaluations of other food environment interventions (29–31). We did not formally assess food insecurity, and incorporating a validated instrument in the future would strengthen our understanding of food insecurity among participants. Although these factors limit the scope of our research conclusions, they did contribute to the brevity of the survey, a feature that allowed our study to achieve high participation rates and a large sample size. Lastly, store inventory data were collected at a different time than customer intercept surveys, limiting the conclusions that can be made regarding produce availability and purchasing behaviors.
Conclusions
Our study findings suggest that healthy store interventions in rural Native communities may be associated with increased fruit and vegetable purchasing among local shoppers. However, further evaluation is needed to better understand which HNSI components were more widely adopted and whether certain components had greater or lesser impact on sales and purchasing of healthy foods. In addition, we recognize that healthy store initiatives are just 1 component of what is needed to meaningfully improve food access in tribal communities. Future food environment initiatives in indigenous communities should prioritize strong partnerships with stakeholders across the entire food system, including health policy, environmental justice, and food sovereignty groups working in their respective communities.
Supplementary Material
ACKNOWLEDGEMENTS
The authors’ responsibilities were as follows—CVG, SSS, OWM, DSC, and TMW: designed and implemented the HNSI; CVG, SSS, EMP, and JL-F: designed the research; CVG, SMS, CC, and QJA: conducted the research; OWM, RP-E, and JL-F: analyzed the data; OWM, CVG, RP-E, and SSS: wrote the paper; OWM and SSS: had primary responsibility for the final content; and all authors: read and approved the final manuscript.
Notes
Supported in part by CDC grant 6 NU58DP005874-03 (to SSS).
Author disclosures: SSS serves as the Executive Director for Community Outreach and Patient Empowerment, which supports the activities described in this manuscript. All other authors report no conflicts of interest.
The views expressed in this manuscript do not necessarily reflect the official policies of the Department of Health and Human Services, nor does the mention of trade names, commercial practices, or organizations imply endorsement by the US Government.
Supplement 1 is available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/cdn/.
The publication of this paper was supported by the Shakopee Mdewakanton Sioux Community, through a gift to the University of Minnesota from its Seeds of Native Health campaign.
Abbreviations used: AI/AN, American Indian/Alaska Native; FDPIR, Food Distribution Program on Indian Reservations; FVI, Fruit and Vegetable Index; FVRx, Fruit and Vegetable Prescription Program; HNSI, Healthy Navajo Stores Initiative; NEMS-S, Nutrition Environment Measurement Survey in Stores; RWJF, Robert Wood Johnson Foundation; SNAP, Supplemental Nutrition Assistance Program.
References
- 1. Hutchinson RN, Shin S. Systematic review of health disparities for cardiovascular diseases and associated factors among American Indian and Alaska Native populations. PLoS One. 2014;9(1):e80973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. US Department of Health and Human Services Office of Minority Health. Obesity and American Indians/Alaska Natives. [Internet] Rockville (MD): Office of Minority Health; 2017. [Last accessed 2019 Jun 11]. Available from: https://minorityhealth.hhs.gov/omh/content.aspx?lvl=3&lvlID=62&ID=6457. [Google Scholar]
- 3. US Department of Health and Human Services Office of Minority Health. Diabetes and American Indians/Alaska Natives. [Internet]. Rockville (MD): Office of Minority Health; 2014. [Last accessed 2019 Jun 11]. Available from: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=33. [Google Scholar]
- 4. O'Connell J, Yi R, Wilson C, Manson SM, Acton KJ. Racial disparities in health status: a comparison of the morbidity among American Indian and U.S. adults with diabetes. Diabetes Care. 2010;33(7):1463–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ballew C, White LL, Strauss KF, Benson LJ, Mendlein JM, Mokdad AH. Intake of nutrients and food sources of nutrients among the Navajo: findings from the Navajo Health and Nutrition Survey. J Nutr. 1997;127(10 Suppl):2085S–93S. [DOI] [PubMed] [Google Scholar]
- 6. Pareo-Tubbeh S, Shorty M, Bauer M, Agbolosoo E. The variety, affordability, and availability of healthful foods at convenience stores and trading posts on the Navajo Reservation [dissertation]. [Internet] Tsaile (AZ): Diné College; 2000. [Last accessed 2019 Jun 11]. Available from: http://nptao.arizona.edu/sites/nptao/files/thevarietyaffordabilityandavailabilityofhealthfulfoods.pdf. [Google Scholar]
- 7. Indian Health Service. Disparities fact sheet. [Internet] Rockville (MD): Indian Health Service; 2018. [Last accessed 2019 Jun 11]. Available from: https://www.ihs.gov/newsroom/factsheets/disparities/. [Google Scholar]
- 8. Tribal Public and Environmental Health Think Tank. Priorities in tribal public health. [Internet] Washington (DC): American Public Health Association, CDC's Office for State, Tribal, Local and Territorial Support; 2018. [Last accessed 2019 Feb 10]. Available from: https://www.apha.org/-/media/files/pdf/topics/environment/partners/tpeh/priorities_tribal_health_2018.ashx?la = en&ash = C06951A62A5E215BE6C99442A9E1E9DDD060B7C6. [Google Scholar]
- 9. Isaac G, Finn S, Joe JR, Hoover E, Gone JP, Lefthand-Begay C, Hill S. Native American perspectives on health and traditional ecological knowledge. Environ Health Perspect. 2018;126(12):125002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kaufman P, Dicken C, Williams R. Measuring access to healthful, affordable food in American Indian and Alaska Native tribal areas. [Internet] Report no. EIB-131 Washington (DC): USDA, Economic Research Service; 2014. [Last accessed 2019 Jul 10]. Available from: https://www.ers.usda.gov/webdocs/publications/43905/49690_eib131_errata.pdf?v = 42103. [Google Scholar]
- 11. Morland KB, Evenson KR. Obesity prevalence and the local food environment. Health Place. 2009;15(2):491–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dong D, Biing-Hwan L. Fruit and vegetable consumption by low-income Americans: would a price reduction make a difference?. [Internet] Report No. 70 Washington (DC): USDA, Economic Research Service; 2009. [Last accessed 2019 Jun 11]. Available from: https://naldc.nal.usda.gov/download/28882/PDF. [Google Scholar]
- 13. Martin KS, Havens E, Boyle KE, Matthews G, Schilling EA, Harel O, Ferris AM. If you stock it, will they buy it? Healthy food availability and customer purchasing behaviour within corner stores in Hartford, CT, USA. Public Health Nutr. 2012;15(10):1973–8. [DOI] [PubMed] [Google Scholar]
- 14. USDA. Food access research atlas. [Internet] Washington (DC): USDA, Economic Research Service; 2015; [cited 2019 Jun 11]. Available from: https://www.ers.usda.gov/data-products/food-access-research-atlas/go-to-the-atlas.aspx. [Google Scholar]
- 15. Eldridge D, McKenzie J, Jackson R, Denny A, Yazzie R, Crotty AK, Curley C. Diné food sovereignty report. Tsaile (AZ): Diné Policy Institute; 2014. [Google Scholar]
- 16. Kumar G, Jim-Martin S, Piltch E, Onufrak S, McNeil C, Adams L, Williams N, Blanck HM, Curley L. Healthful nutrition of foods in Navajo Nation stores: availability and pricing. Am J Health Promot. 2016;30(7):501–10. [DOI] [PubMed] [Google Scholar]
- 17. Pardilla M, Prasad D, Suratkar S, Gittelsohn J. High levels of household food insecurity on the Navajo Nation. Public Health Nutr. 2014;17(1):58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household food security in the United States in 2017. Report No. 256 Washington (DC): USDA, Economic Research Service; 2018. [Last accessed 2019 Jun 23]. Available from: https://www.ers.usda.gov/webdocs/publications/90023/err-256.pdf?v=0. [Google Scholar]
- 19. Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. J Gen Intern Med. 2007;22(7):1018–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Townsend MS, Peerson J, Love B, Achterberg C, Murphy SP. Food insecurity is positively related to overweight in women. J Nutr. 2001;131(6):1738–45. [DOI] [PubMed] [Google Scholar]
- 21. Wilde PE, Peterman JN. Individual weight change is associated with household food security status. J Nutr. 2006;136(5):1395–400. [DOI] [PubMed] [Google Scholar]
- 22. Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140(2):304–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Glanz K, Sallis JF, Saelens BE, Frank LD. Nutrition Environment Measures Survey in Stores (NEMS-S): development and evaluation. Am J Prev Med. 2007;32(4):282–9. [DOI] [PubMed] [Google Scholar]
- 24. Laska M, Pelletier J. Minimum stocking levels and marketing strategies of healthful foods for small retail food stores. Report No. 1088 Minneapolis (MN): Healthy Eating Research, Robert Wood Johnson Foundation; 2016. [Google Scholar]
- 25. StataCorp. Stata. [software]. College Station (TX): StataCorp LP; 2015. [Google Scholar]
- 26. Zenk SN, Lachance LL, Schulz AJ, Mentz G, Kannan S, Ridella W. Neighborhood retail food environment and fruit and vegetable intake in a multiethnic urban population. Am J Health Promot. 2009;23(4):255–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Aggarwal A, Cook AJ, Jiao J, Seguin RA, Vernez Moudon A, Hurvitz PM, Drewnowski A. Access to supermarkets and fruit and vegetable consumption. Am J Public Health. 2014;104(5):917–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gustat J, O'Malley K, Luckett BG, Johnson CC. Fresh produce consumption and the association between frequency of food shopping, car access, and distance to supermarkets. Prev Med Rep. 2015;2:47–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lawman HG, Vander Veur S, Mallya G, McCoy TA, Wojtanowski A, Colby L, Sanders TA, Lent MR, Sandoval BA, Sherman S et al.. Changes in quantity, spending, and nutritional characteristics of adult, adolescent and child urban corner store purchases after an environmental intervention. Prev Med. 2015;74:81–5. [DOI] [PubMed] [Google Scholar]
- 30. Dannefer R, Williams DA, Baronberg S, Silver L. Healthy bodegas: increasing and promoting healthy foods at corner stores in New York City. Am J Public Health. 2012;102(10):e27–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lent MR, Vander Veur S, Mallya G, McCoy TA, Sanders TA, Lawman HG, Wylie-Rosett J, Foster GD. Purchasing patterns of adults, adolescents and children in urban corner stores: quantity, spending and nutritional characteristics. Public Health Nutr. 2015;18(9):1706–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


