Abstract
Purpose
In ophthalmology, injuries due to lightning strikes have been documented as various entities ranging from keratitis, cataracts, uveitis in the anterior segments to retinal detachments, papillitis, and macular hole formation in the posterior segment. We report the largest case series so far with a total of seven cases of lightning injuries with ocular involvement and its management and a brief review of the literature on this topic.
Patients and Methods
All of the patients were evaluated for ocular injuries due to a lightning strike and each of the cases has been individually described as case series with their findings and management in this report.
Results
Ocular injuries caused by lightning are very rare, but when they occur, they can present with various ocular tissue pathology-ranging from anterior to the posterior segment structures. Most of the cases presented with maculopathy and foveschitic lesions, which resolved over time with the use of steroids.
Conclusion
Lightning injuries to the eyes, if detected early and managed appropriately, have a very good prognosis. The recovery is usually good with minimal functional loss if there is a quick referral. The macular region seems to be particularly involved in most cases and OCT can be a valuable diagnostic tool to detect and monitor the pathology.
Keywords: lightning injuries, ophthalmology, lightning, eye, cataract, uveitis, keratitis
Introduction
The odds of being struck by lightning in a year are approximately 1 in 960,000. Surprisingly the odds of surviving one of these major bolts are very good, with nearly 9 in 10 people escaping death.1 The human body is a good conductor of electricity and most of the time the electrical energy just passes from one contact point with very little damage. However, this is not true in all cases. Collateral damage depends upon the type of strike/contact.2
In ophthalmology, injuries due to lightning strikes have been documented as various entities – ranging from keratitis, cataracts, uveitis in the anterior segments to retinal detachments, papillitis, and macular hole formation in the posterior segment.3,4 A few works of literature can also be found on the formation of macular cysts and how investigative tools such as optical coherence tomography (OCT) can help in diagnosis and determining the response to treatment.5,6
It has been hypothesized that the melanin the melanocytes provide the main resistance to the current and hence injuries occur more in the tissue with melanocytes. The resultant injury can occur in the form of mechanical disruption or local inflammation secondary to the high energy transfer in the form of electricity or heat.2,3
We report the largest case series so far with a total of seven cases of lightning injuries with ocular involvement, and its management and a brief review of the literature on this topic (Table 1).
Table 1.
Table Depicting the Mode of Lightning Injury, Clinical Findings, Treatment, and Outcome of the Patients
| Case | Mode of Lightning Injury | Clinical Finding | OCT Findings | Treatment | Outcome |
|---|---|---|---|---|---|
| 1 | Side splash | Flash burn to the face, bilateral cataract | Not available | Lens aspiration with intraocular lens implantation. Topical antibiotics (tobramycin) Steroids (prednisolone acetate 1%) Cycloplegics (cyclopentolate 1%) |
Uneventful |
| 2 | Ground current | Dull fovolar reflex | Bilateral parafoveolar cyst | Topical steroids (prednisolone acetate 1%) |
Uneventful |
| 3 | Direct | Dull foveolar reflex | Bilateral parafoveolar cyst | Topical steroids (prednisolone acetate 1%) |
Persistent parafoveolar cyst in the right eye up to 6 weeks. Lost to follow-up. |
| 4 | Direct | Conjunctivitis with orbital swelling | Unilateral parafoveolar cyst in the left eye. | Systemic steroids (prednisolone 1 mg/kg tapering weekly over 4 weeks) |
Uneventful |
| 5 | Direct | Uveitis | Bilateral parafoveolar cyst with foveoschisis like lesion | Topical steroids (prednisolone acetate 1%) Cycloplegic homatropine (2%) Systemic steroids (prednisolone 1 mg/kg) |
Persistent parafoveolar cyst in the right eye up to 4 weeks. Lost to follow-up. |
| 6 | Direct | Dull foveolar reflex | Unilateral foveal cyst in the right eye. | Topical steroids (prednisolone acetate 1%) Cycloplegic homatropine (2%) |
Decreased level of the parafoveolar cyst but still persistent at 3 weeks after which the patient was lost to follow-up. |
| 7 | Contact/direct | Uveitis, cataract, exudative retinal detachment | Unilateral foveal cyst in the right eye. | Topical steroids (prednisolone acetate 1%) Cycloplegic homatropine (2%) |
No improvement. Lost to follow-up at 4 months. |
Case 1
A 26-month-old female child was referred to our emergency department with swelling of eyelids and face with a history of a lightning strike 3 days previously. Her elder brother died at the site of incidence. The patient's vitals were stable. On ocular examination, there was evidence of 1st-degree flash burn over the facial region, involving the eyebrows, lashes, and the eyelid. On retraction of the lid, the cornea was hazy and the conjunctiva was chemosed bilaterally (Figure 1A–C). The patient followed the light projected from a torchlight but further evaluation of inner ocular structures was not possible. Ultrasonography (USG) of the eyes was done and they were found to be normal (Figure 1D and E).
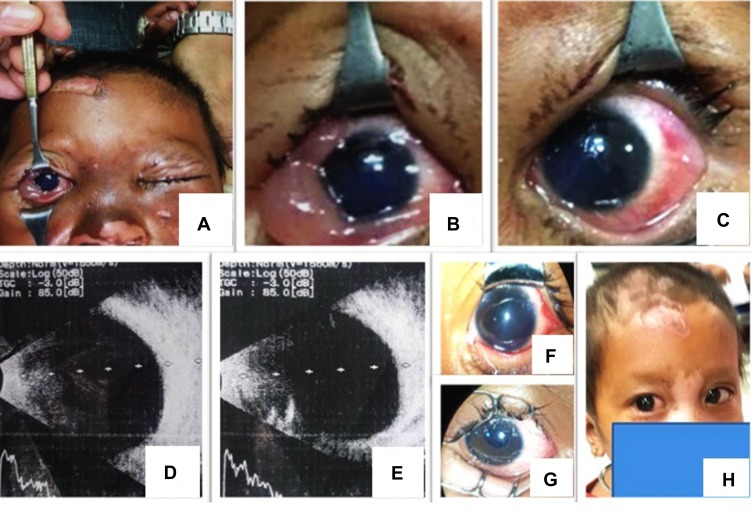
Figure 1.
(A) A child patient with resultant burn secondary to lightning strike. (B, C) Conjunctival congestion and chemosis with corneal edema. Lens was cataractous. (D, E) Normal posterior segment findings in B-scan. (F, G) Post-operative findings in both eye after lens aspiration and posterior chamber intraocular lens implantation. (H) Healing of the burn scars after 3 weeks.
The patient was admitted and treated with topical antibiotics, cycloplegics, and steroids. After a week’s treatment, the child was re-evaluated. The corneal haze and conjunctival chemosis had receded (Figure 1F and G). The anterior chamber findings were normal but the patient was found to be cataractous lens bilaterally. The patient's party was advised that lens aspiration with anterior vitrectomy with intraocular lens implant was recommended. The patient underwent surgery in the right eye (OD), followed by the left eye (OS) a week apart (Figure 1F and G). Fundus evaluation was done intraoperatively using indirect ophthalmoscopy and was found to be normal. The patient recovered uneventfully.
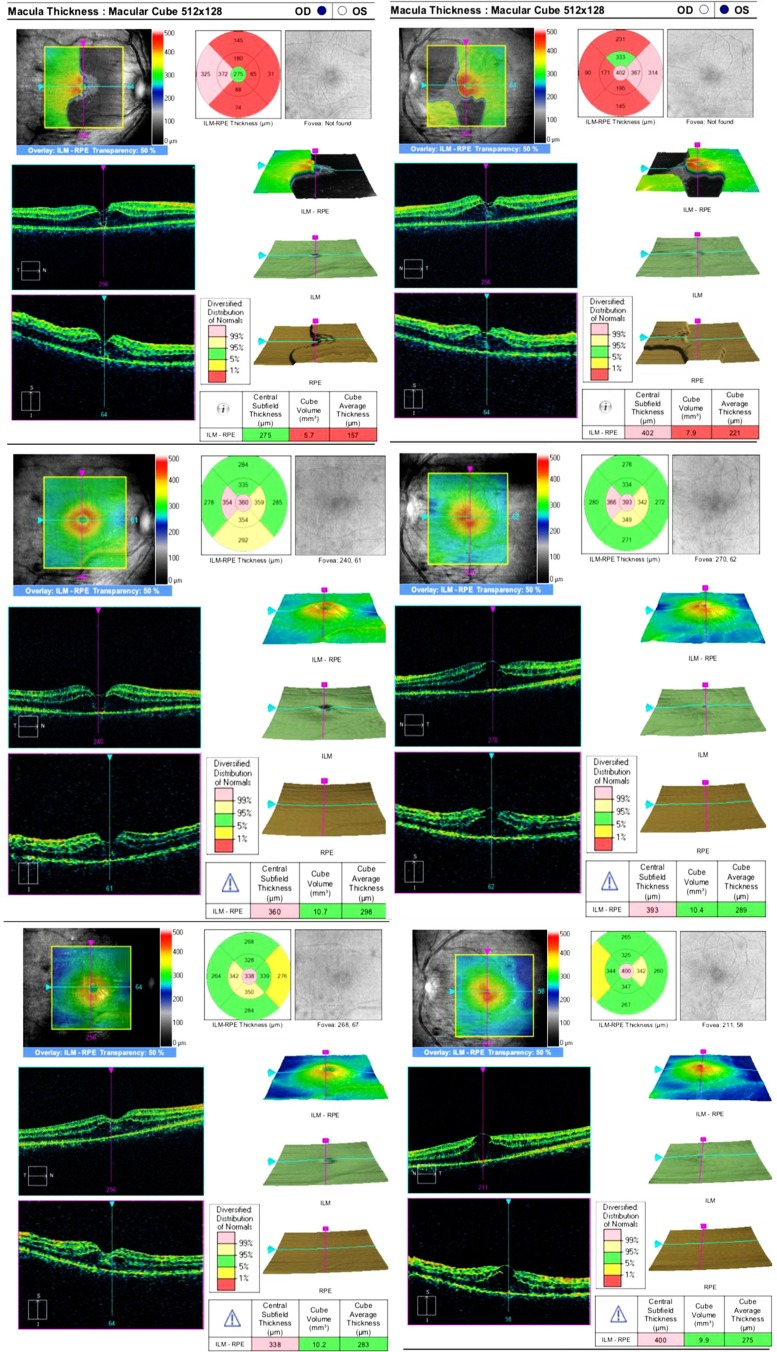
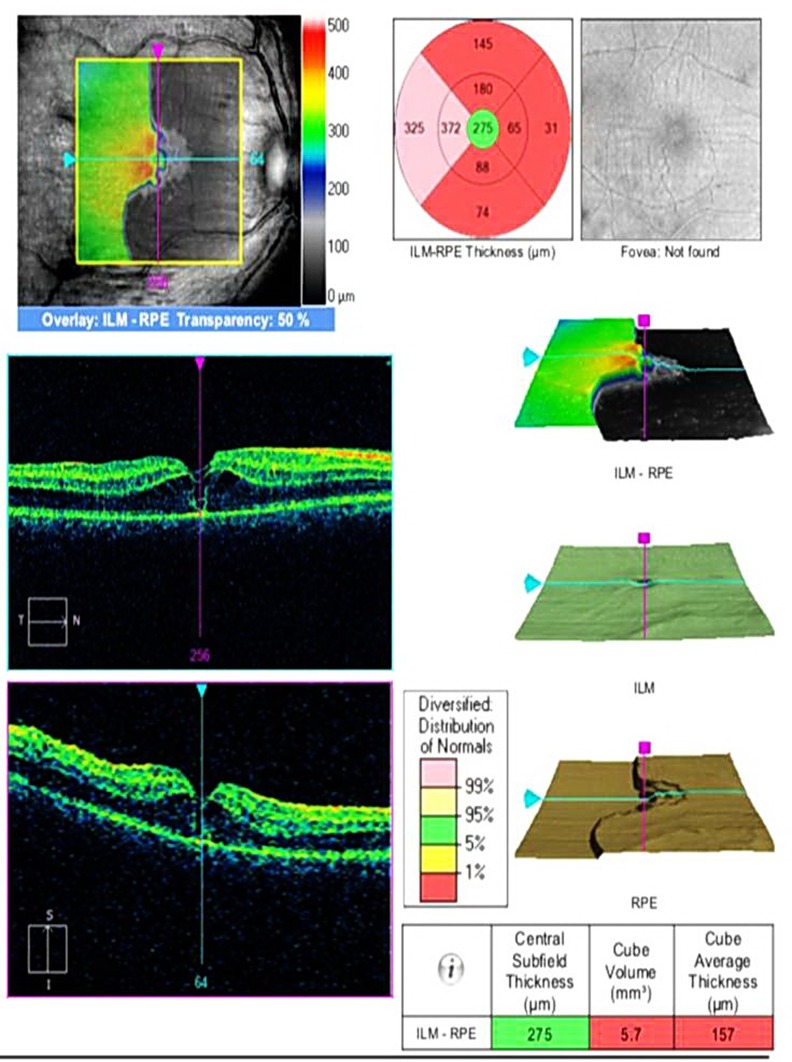
Case 2
A 25-year-old male presented with diminution of vision after recovering from unconsciousness which was preceded by a bright flash-like event nearby on a rainy day. He stated that initially after recovering he had loss of vision for 4–5 hours, which gradually improved but never fully recovered. On ocular examination, his best corrected visual acuity (BCVA) was 6/18 bilaterally (OU). The anterior segment findings were normal. Foveal reflex was found to be dull OU (Figure 2). OCT revealed OU parafoveolar cysts (PFC). The patient was treated with topical steroids and asked to follow up weekly. The PFC decreased over time and eventually resolved by the end of 3 months, with BCVA of 6/12 OD and 6/9 OS.
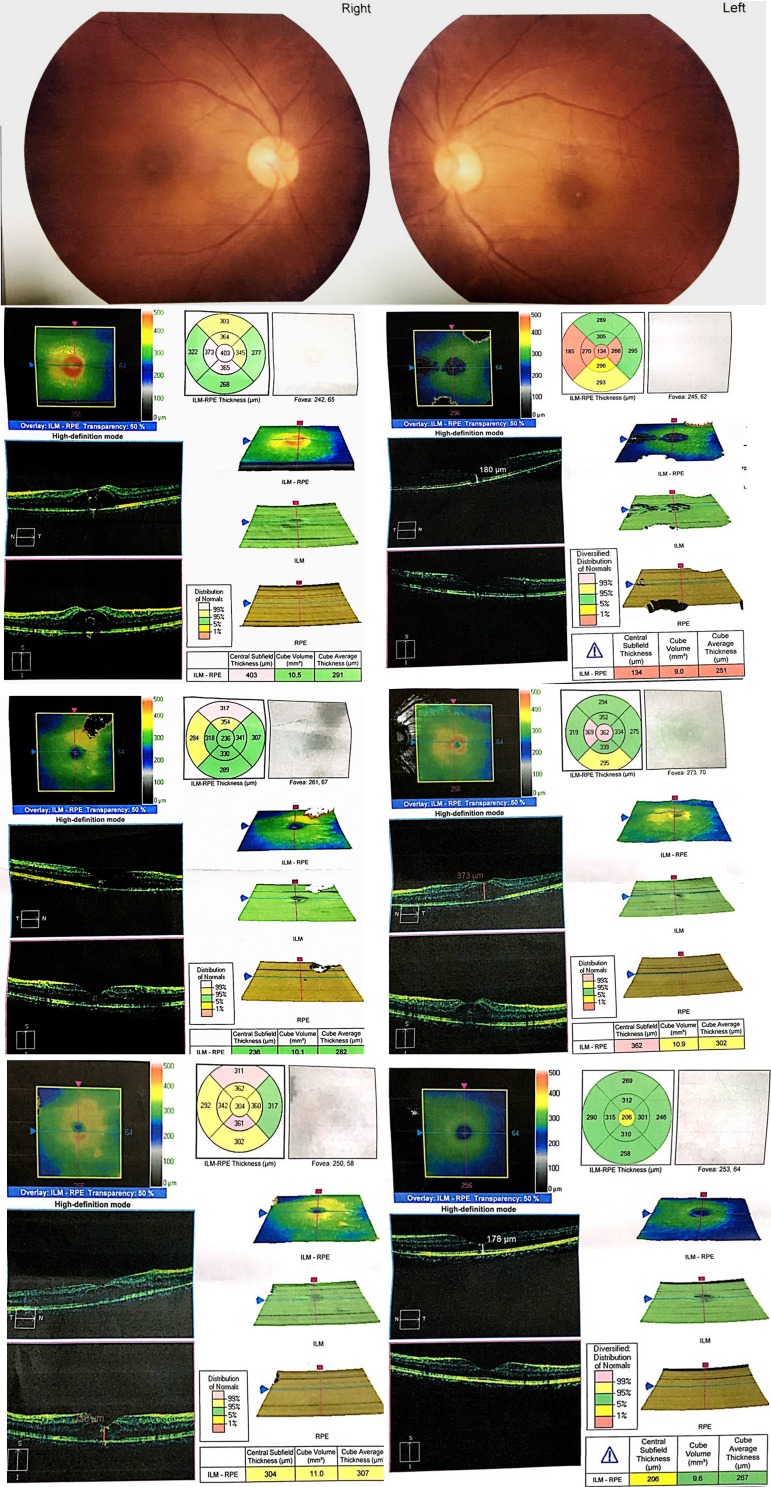
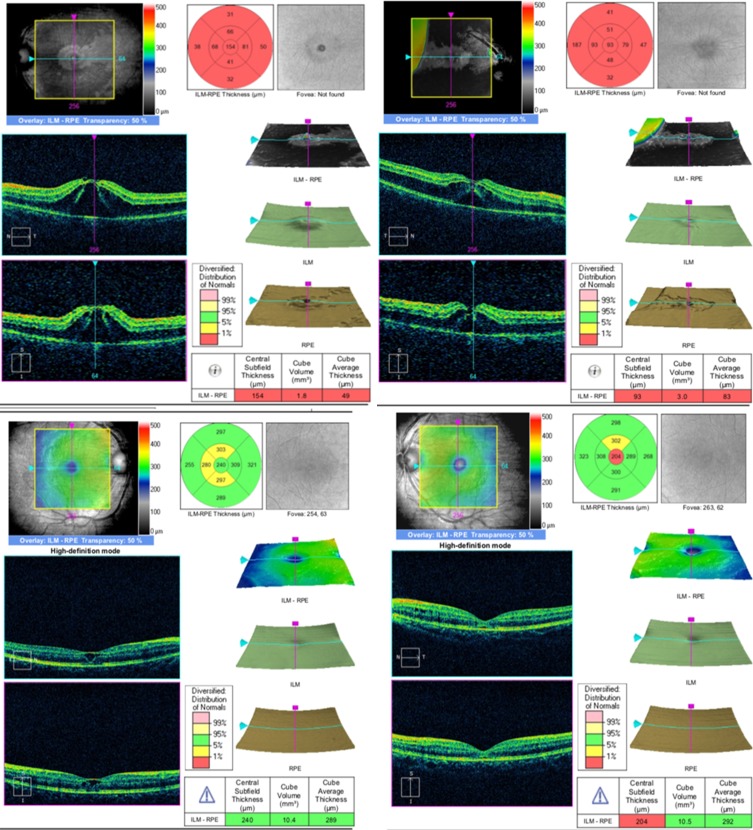
Figure 2.
OCT findings in a young male patient suggesting bilateral foveolar cysts. Both cysts disappeared with improvement of vision by 3 months following treatment with topical steroids.
Case 3
A 21-year-old female presented with redness and blurring of vision after a lightning strike while working in the field 12 days previously. The patient's party gave a history of the patient being unconscious for 7 h after being found in the field. Her BCVA was 6/36 OU. The anterior segment findings were normal, and again, the foveal reflex was found to be dull OU. OCT revealed OU PFC (Figure 3). The patient was treated with topical steroids and cycloplegics and asked to follow up weekly. The PFC of the OS resolved. In OD, the FC decreased over time but did not resolve until the last follow-up, after which the patient was lost to follow-up. BCVA was 6/24 OD and 6/12 OS.
Figure 3.
A young female patient stuck by lightning in an open area. She presented with diminution of vision and on OCT examination presented with bilateral foveolar cysts.
Case 4
A 16-year-old male presented with swelling of the left eye, redness, discharge, and blurring of vision after a lightning strike a month previously. The patient's party gave a history of the patient being unconscious for 2 h. His BCVA was 6/9 OD and 6/60 OS. The patient had a clinical presentation as a case of conjunctivitis and was prescribed topical antibiotics and anti–inflammatory agents. At follow-up of 10 days t,he patient was symptomatically better but the BCVA remained 6/60 in OS. OCT was done which revealed the presence of unilateral PFC in OS (Figure 4). In this case, the patient was prescribed a topical and systemic steroid (prednisolone 1 mg/kg) along with proton pump inhibitors in a tapering fashion over a period of 4 weeks. The patient had a complete resolution of the PFC with BCVA in OS of 6/12 at the 6th week.
Figure 4.
A young male patient with foveal cysts following a lightning strike.
Case 5
A 26-year-old male presented with photophobia. The patient gave a history of being struck by lightning followed by blackout for approximately 20 minutes, 6 days previously. His BCVA was 6/18 OD and 6/18 OS. The patient had conjunctival and circumciliary congestion with cells of 3+ in the anterior chamber of OU (Figure 5). OCT was done which revealed the presence of OU PFC, with foveoschisis-like lesions. This patient was already treated with a topical and systemic steroid (oral prednisolone 1 mg/kg) along with PPI and cycloplegics. The patient had persistent PFC at 1 month with similar BCVA as of baseline and was lost to follow-up.
Figure 5.
OCT of a young male patient who presented with uveitis and macular edema following a lightning strike.
Case 6
A 20-year-old female presented with diminution of vision in OD for 13 days following a lightning strike. Her BCVA was 6/36 in OD (Figure 6) and 6/6 OS. The rest of the ocular findings were normal. The patient was advised for OCT with revealed a PFC in the OD. This patient was treated with topical steroid cycloplegics. The patient had decreased PFC at 3 weeks with BCVA of 6/18 in OD but was lost to follow-up.
Figure 6.
OCT of a young female patient with macular edema and “foveoscitic” lesion following lightning strike who presented nearly at 2 weeks following trauma.
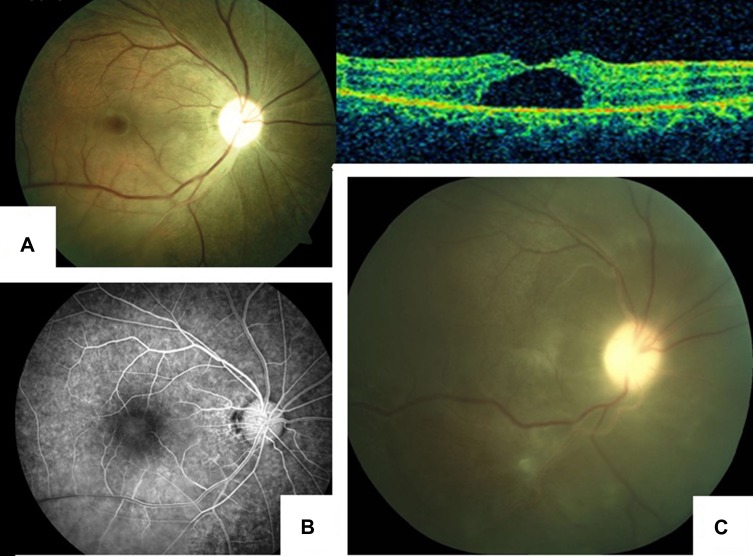
Case 7
A 25-year-old female came in with the chief complaint of a sudden loss of vision in OD following exposure to a lightning strike. She was standing near a window on a rainy day when lightning struck the ground about 5 m away from her.
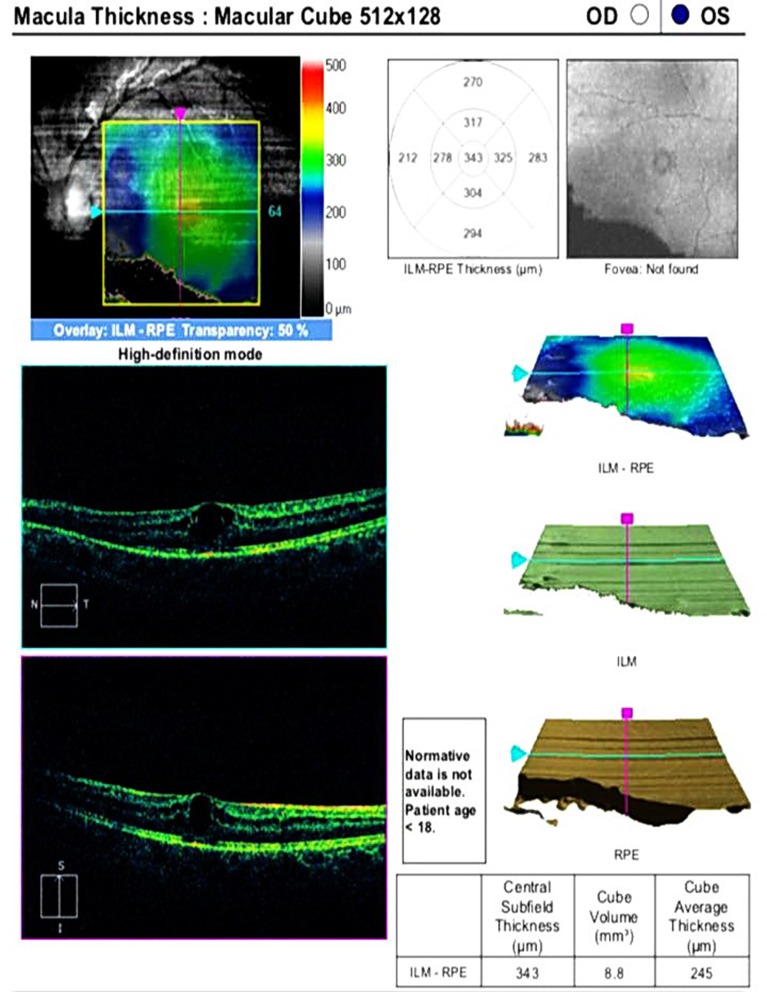
Following the incident, she was unconscious for about 30 minutes. On examination, her best corrected vision was hand movement in OD and 6/9 in OS. IOP was 13 and 12 mmHg g, respectively. OD had lid edema, mild conjunctival congestion, corneal edema with descemet’s membrane folds, 2 + cells, and flare in anterior chamber (AC); relative afferent pupillary defect (RAPD) was present, the lens was clear and posterior segment details were not visible. OS was normal. The patient was treated with topical steroids and cycloplegic. After 5 days BCVA was HM, the cornea was clear, AC was quiet, RAPD was still present, vitreous was clear, disc and retinal vessels were normal but a foveal cyst was present in RE. OCT showed a large intraretinal cyst at the fovea with a thin overlying tissue suggestive of an impending macular hole (Figure 7A). Fundus fluorescein angiography (FFA) showed mild diffuse hyper fluorescence in the foveal area with no leakage (Figure 7B). The probable cause of poor vision in RE was a foveal cyst and optic neuropathy. On follow-up after four months, posterior subcapsular cataract was present, the disc was pale, there was no change in the size of the foveal cyst and inferior RD was noted. No retinal breaks were seen, posterior hyaloid was intact, and shifting fluid was present with retinal pigment epithelium (RPE) mottling, suggestive of exudative RD (Figure 7C). The vision was still HM. The patient deferred any further treatment in view of poor visual prognosis.
Figure 7.
Fundus images of a young woman who presented with exudative retinal detachment following a lightning strike. (A) Fundus photo and OCT image, 5 days following treatment. (B) Fundus fluorescein angiography (FFA) showed mild diffuse hyper fluorescence in the foveal area with no leakage. (C) Shifting fluid with retinal pigment epithelium (RPE) mottling suggestive of exudative RD.
Discussion
It has been suggested that there are three main mechanisms by which lightning can strike: (a) direct, where the person is part of the flash due to direct contact and may also be affected by the resulting sonic blast; (b) indirect, due to a side flash, where the lightning strikes a nearby object but takes the route of least resistance and as result, the human body is involved, or due to the aftereffect of the electromagnetic pulse; and (c) resultant injuries secondary to the strike, eg, fire, blast, and accidents.7–9
In Nepal, lightning has emerged as one of the deadliest natural disasters, and causes the second highest number of casualties due to a natural disaster.10 In 2012–2018, 9 lightning detection centers were installed across the country. Statistics show that 773 people were killed and 1695 were injured during this period.11
Lightning injuries can present with an ocular injury that may involve the anterior or the posterior segment of the eye and, in some instances, both7,8,12,13 The heat energy produced can also cause burns as it did in our case 1. The child presented with facial burns with bilateral corneal edema and cataractous lens. Corneal edema and cataract formation are well-known lightning injuries and have been documented in the literature.13 Definite treatment is cataract surgery and, in our case, we performed this earlier due to the case being a child and there was a risk of development of amblyopia. The patient recovered well with resolution of the corneal edema with the treatment of topical steroids and antibiotics after the surgery.
It has been advised that OCT should be performed in all cases of lightning injuries to rule out macular involvement.5,6,14,15 We were unable to perform OCT in case 1 due to the patient being a child. However, OCT was performed in all other cases. All the other 5 cases were found to have parafoveal cysts. This phenomenon has been well documented in the literature. Rivas-Aguiño et al6 reported a similar finding in a 14-year-old female bilaterally, which was initially confused as a macular hole at fundus examination. Cases 2 and 3 presented with similar findings and had complete resolution of the parafoveal cysts following treatment with topical steroids by the third month. Liu et al5 have also described a similar finding in a young female who was struck by lightning. They termed the condition “delayed-onset cystoid macular abnormalities” which was caught by OCT. It was also only unilateral. They proposed it could be a result of thermal injury of the outer retina, causing proteins to denature and cellular dysfunction. Three of our cases, cases 4, 6, and case 7, also presented with unilateral involvement of the macula with similar lesions. Case 6 was treated with topical steroids and showed significant improvement in visual acuity. The case was however lost at a month’s follow-up. Case 4 had initially presented with conjunctivitis of the left eye. The patient was recommended for OCT as he complained of persistent diminution of vision. OCT revealed a parafoveal cyst with a “foveoschisis” like lesion and was treated with both topical and systemic steroids. At the 6-week follow-up, the lesions had disappeared, and visual acuity improved to 6/12. Case 7, which earlier presented with a foveolar cyst, presented with inferior exudative retinal detachment with optic atrophy at a follow-up of 4 months. The patient was planned for a systemic steroid trial but denied treatment. Optic neuropathy and rhegmatogenous retinal detachments have been described as a complication of lightening injury to an eye13 but we were not able to find any literature on exudative retinal detachment.
Parafoveal cyst with “foveoschisis”-like lesion was also found bilaterally in case 5 who had initially presented with anterior uveitis. However, the patient did not respond to the treatment of topical and systemic steroids. The lesions persisted until 4 weeks with no improvement in visual acuity. The patient was lost to follow-up.
Conclusion
Our case series highlights how lightning strike injury can present with various ocular manifestations. It also highlights that parafoveolar cysts are almost a common finding and hence OCT examination is mandatory. The presentation of such pathology can also be unilateral and can masquerade as conjunctivitis, corneal edema, uveitis initially, and even as exudative retinal detachment in later stages. Topical (1% prednisolone acetate) and oral steroids (prednisolone 1 mg/kg) for 10–14 days remain the mainstay of treatment but may not respond in a similar manner and have different final outcomes. Parafoveolar cysts in adjunct to “foveoschisis-like lesions” in particular may respond poorly. Even if resolutions of such lesions do occur, visual acuity may not improve.
Ethics Statement
We confirm that written informed consent was obtained from the patients and this consent included the permission to publish the case details.
For patients who were younger than 18 years, informed and written consent was obtained from parents/liable guardians. The research has been approved by the ethics committee and the institutional review board of Tilganga Institute of Ophthalmology, Kathmandu, Nepal and has adhered to the tenets of the declaration of Helsinki.
Disclosure
The authors report no competing interests.
References
- 1.Vavrek JR, Kithil R, Holle RL, Allsopp J, Cooper MA. The Science of Thunder. Earth Sci 2006;22(3):5–9. [Google Scholar]
- 2.Lagrèze WD, Bömer TG, Aiello LP. Lightning-induced ocular injury. Arch Ophthalmol. 1995;113:1076–1077. doi: 10.1001/archopht.1995.01100080128041 [DOI] [PubMed] [Google Scholar]
- 3.Handa JT, Jaffe GJ. Lightning maculopathy. A case report. Retina. 1994;14:169–172. doi: 10.1097/00006982-199414020-00011 [DOI] [PubMed] [Google Scholar]
- 4.Espaillat A, Janigian R Jr, To K. Cataracts, bilateral macular holes, and rhegmatogenous retinal detachment induced by lightning. Am J Ophthalmol. 1999;127:216–217. doi: 10.1016/S0002-9394(98)00294-3 [DOI] [PubMed] [Google Scholar]
- 5.Liu TYA, See C, Singman E, Han IC. Delayed onset of intraretinal cystoid abnormalities in lightning retinopathydelayed onset of intraretinal cystoid abnormalities letters. JAMA Ophthalmol. 2016;134(7):840–842. doi: 10.1001/jamaophthalmol.2016.1018 [DOI] [PubMed] [Google Scholar]
- 6.Rivas-Aguiño PJ, Garcia RA, Arevalo JF. Bilateral macular cyst after lightning visualized with optical coherence tomography. Clin Exp Ophthalmol. 2006;34:893–894. doi: 10.1111/j.1442-9071.2006.01377.x [DOI] [PubMed] [Google Scholar]
- 7.Lee MS, Gunton KB, Fischer DH, Brucker AJ. Ocular manifestations of remote lightning strike. Retina. 2002;22:808–810. doi: 10.1097/00006982-200212000-00023 [DOI] [PubMed] [Google Scholar]
- 8.Ritenour AE, Morton MJ, McManus JG, Barillo DJ, Cancio LC. Lightning injury: a review. Burns. 2008;34(5):585–594. doi: 10.1016/j.burns.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 9.Grover S, Goodwin J. Lightning and electrical injuries: neuro-ophthalmologic aspects. Semin Neurol. 1995;15:335–341. doi: 10.1055/s-2008-1041041 [DOI] [PubMed] [Google Scholar]
- 10.Lightning emerges as second deadliest natural calamity. The Himalayan Times; April28, 2018 Available from: https://thehimalayantimes.com/kathmandu/lightning-emerges-as-second-deadliest-natural-calamity/. Accessed January28,2019.
- 11.National Emergency Operation Centre, Ministry of Home Affairs, Nepal. Avaliable from: http://neoc.gov.np/en/. Accessed January21, 2019.
- 12.Rishi E, Indu VP, Rishi P. Lightning injury of posterior segment of the eye. Indian J Ophthalmol. 2016;64(2):151–152. doi: 10.4103/0301-4738.179724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Norman ME, Albertson D, Younge BR. Ophthalmic manifestations of lightning strike. Surv Ophthalmol. 2001;46(1):19–24. doi: 10.1016/S0039-6257(01)00232-6 [DOI] [PubMed] [Google Scholar]
- 14.Dhillon PS, Gupta M. Ophthalmic manifestations postlightning strike case reports. Case Rep. 2015;2015:bcr2014207594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Armstrong B, Fecarotta C, Ho AC, Baskin DE. Evolution of severe lightning maculopathy visualized with spectral domain optical coherence tomography. Ophthalmic Surg Lasers Imaging. 2010;41(Suppl):S70–3. doi: 10.3928/15428877-20101031-02 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Lightning emerges as second deadliest natural calamity. The Himalayan Times; April28, 2018 Available from: https://thehimalayantimes.com/kathmandu/lightning-emerges-as-second-deadliest-natural-calamity/. Accessed January28,2019.