Through a national sample of adolescents and young adults, we investigated the incidence of persistent opioid use after common pediatric surgeries.
Abstract
BACKGROUND:
Despite efforts to reduce nonmedical opioid misuse, little is known about the development of persistent opioid use after surgery among adolescents and young adults. We hypothesized that there is an increased incidence of prolonged opioid refills among adolescents and young adults who received prescription opioids after surgery compared with nonsurgical patients.
METHODS:
We performed a retrospective cohort study by using commercial claims from the Truven Health Marketscan research databases from January 1, 2010, to December 31, 2014. We included opioid-naïve patients ages 13 to 21 years who underwent 1 of 13 operations. A random sample of 3% of nonsurgical patients who matched eligibility criteria was included as a comparison. Our primary outcome was persistent opioid use, which was defined as ≥1 opioid prescription refill between 90 and 180 days after the surgical procedure.
RESULTS:
Among eligible patients, 60.5% filled a postoperative opioid prescription (88 637 patients). Persistent opioid use was found in 4.8% of patients (2.7%–15.2% across procedures) compared with 0.1% of those in the nonsurgical group. Cholecystectomy (adjusted odds ratio 1.13; 95% confidence interval, 1.00–1.26) and colectomy (adjusted odds ratio 2.33; 95% confidence interval, 1.01–5.34) were associated with the highest risk of persistent opioid use. Independent risk factors included older age, female sex, previous substance use disorder, chronic pain, and preoperative opioid fill.
CONCLUSIONS:
Persistent opioid use after surgery is a concern among adolescents and young adults and may represent an important pathway to prescription opioid misuse. Identifying safe, evidence-based practices for pain management is a top priority, particularly among at-risk patients.
What’s Known on This Subject:
Opioid-related morbidity and mortality among US adolescents and young adults continues to rise. Postoperative opioid prescriptions vary widely and are often in excess among children and adults. Postoperative care is an important risk factor for prolonged opioid use among adults.
What This Study Adds:
This study is the first to investigate persistent opioid use among adolescents and young adults after surgery. This study highlights the need for safe prescribing and monitoring habits in the postoperative setting to prevent long-term addiction, misuse, and adverse effects.
Since the 1990s, opioid prescribing and use have increased dramatically across all age groups in the United States, resulting in a major, national public health problem.1–3 Among adolescents, self-reported rates of medical and nonmedical opioid use have only recently begun to decline, which is likely a result of increased awareness4; yet, rates of serious adverse events secondary to prescription opioid misuse continue to rise.5,6 Hospitalizations from prescription opioid use and heroin use from 1997 to 2012 within this age group have risen by 175% and 161%, respectively.5 Adolescents have a 3- to 5-times greater risk for serious medical outcomes when presenting for care with opioid exposure, such as life-threatening symptoms or death, than children in any other age group.6
Prescription opioids remain an important analgesic for treating postoperative acute pain, and surgical care is 1 of the most common medical encounters associated with opioid prescription.7 Yet, postoperative opioid prescribing often varies widely and results in excess among both children and adults, even after minor procedures.8–11 Recent studies have demonstrated that postoperative care is an important risk factor for prolonged opioid use among adults.7,12–14 For example, among opioid-naïve adults undergoing major and minor elective surgical procedures, rates of prolonged opioid use are estimated to range from 3% to 10% and are more pronounced among adults with coexisting medical and mental health conditions.7,13,15 Prescription opioids have a high potential for misuse and adverse effects, particularly among adolescents and young adults, who may be more vulnerable than adults because of changes in the reward and habit formation centers of the brain15–17; however, little is known about prescription opioid misuse after acute exposure in the surgical setting in this age group.
In this retrospective study, we examined the incidence of prolonged opioid refills as a surrogate for persistent opioid use after surgery among 88 637 patients ages 13 to 21 years in the United States. We further examined the contribution of demographic, comorbid, and mental health conditions to the risk of persistent opioid use among adolescents and young adults. We hypothesized that persistent opioid use among adolescent and young adult patients would be similar to previously described rates among adult patients after common surgical procedures.
Methods
This study was approved by the Institutional Review Board at the University of Michigan. We examined insurance claims from all patients ages 13 to 21 years who underwent 1 of 13 inpatient or outpatient surgical procedures identified by Current Procedural Terminology (CPT) codes from January 1, 2010, to December 31, 2014, by using Truven Health Marketscan, a national data set of employer-based insurance claims. The procedures from across pediatric surgical specialties included tonsillectomy and/or adenoidectomy, inguinal hernia (open or laparoscopic), umbilical or epigastric hernia, appendectomy, cholecystectomy, pectus repair (open or minimally invasive), colectomy (open or laparoscopic), open supracondylar fracture fixation, open epicondylar fracture fixation, posterior arthrodesis, arthroscopic knee repair (anterior cruciate ligament [ACL] and/or meniscus), orchiopexy (open or laparoscopic), and hypospadias repair (Supplemental Table 1). Patients undergoing selected surgical procedures were included if they met the following criteria: (1) had continuous insurance coverage during the 12 months before the procedure through the 6 months after, (2) did not undergo an additional surgical procedure or anesthesia during the 6 months after the procedure, and (3) were opioid naïve without any previous opioid prescription fills during the 11 months before the 30-day period before the procedure.13 For all further analyses, we included patients with at least 1 opioid prescription fill during the perioperative period, which was defined as 30 days before to 2 weeks after the procedure.13
For a comparison cohort of patients who did not undergo surgery, we identified a random sample of 3% of the 2 968 832 nonsurgical patients ages 13 to 21 years in the Truven Health Marketscan during the study period (n = 110 432). Patients in the control group were assigned a random, fictitious surgery date, and the 3 inclusion criteria, including continuous insurance coverage, no additional procedures, and opioid-naïve status, were applied.13,14 We examined patient-level covariates, including age, sex, and comorbidities (as defined by Feudtner’s complex chronic condition codes [CCCCs]),18 mental health diagnoses (depression, anxiety, and substance use disorder [SUD]),13 and chronic pain diagnoses identified with International Classification of Diseases, Ninth Revision (ICD-9) codes in the 12 months preceding the surgery date among surgical and nonsurgical patients. Pediatric pain diagnoses were verified as chronic according to the Agency for Healthcare Research, the quality Chronic Condition Indicator, and by the ICD-9. Any chronic pain diagnoses that were secondary to chronic medical conditions captured in the CCCC were excluded (Supplemental Table 4).18,19 For colectomy, we also examined surgical indication as the primary diagnosis for hospitalization.
Opioid prescriptions from pharmacy claims were identified by matching generic drug names with National Drug Codes, which detail specific drug doses and types. For each prescription, we converted the unit of the opioid component to milligrams and calculated oral morphine equivalents (OMEs) for each unit by using standard published conversions for the morphine equivalent conversion factor per milligram.20 The OME dosage for each individual opioid prescription that was filled was calculated as the unit OME exposure multiplied by the total quantity filled in this prescription and was reported as total OME per initial prescription. A dose of >100 OMEs per day has previously been defined as a possible marker of potential misuse or inappropriate prescribing patterns21; thus, the proportion of the cohort with initial high daily dosage was also calculated.
Our primary outcome, persistent opioid use after surgery, was defined as 1 or more additional opioid prescription(s) filled between 90 and 180 days after the procedure and was defined a priori before data extraction.7,13 The time frame was based on the definition from the International Association for the Study of Pain,22 which defines long-term postsurgical pain as pain that is persistent beyond 3 months after surgical intervention. Univariate descriptive statistics were used to characterize the common attributes of postoperative prescriptions among adolescents and young adults undergoing surgery, including daily and total OMEs for each postoperative month and patient characteristics. A multivariate logistic regression model was estimated to examine differences in persistent opioid use between surgical types and controlled for patient age, sex, CCCCs, mental health diagnoses, and chronic pain diagnoses. To obtain a parsimonious model, a stepwise logistic regression (P < .3 for inclusion) was used to identify relevant patient characteristics as control variables in the final model. All analyses were conducted by using SAS version 9.4 (SAS Institute, Inc, Cary, NC).
Results
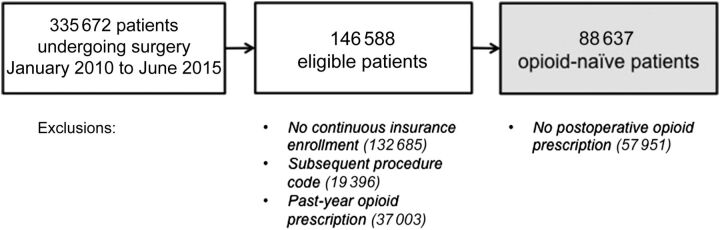
We identified 146 588 opioid-naïve patients during the study period who underwent surgery between 2010 and 2014. Among these patients, 60.5% (88 637) filled a prescription from 30 days before to 2 weeks after the operation (Fig 1), and 29.3% (25 951) filled multiple prescriptions during this period. Prescriptions were filled in the postoperative period only by 80.7% (71 511) of surgical patients, in the preoperative period only by 9.0% (7953), and in both the pre- and postoperative periods by 10.4% (9173) of patients. The control cohort included 110 432 opioid-naïve comparison patients, and the demographics of the 2 cohorts are shown in Table 1. Opioid-naïve surgical patients who filled perioperative prescriptions were 54.4% women with an average age of 17 ± 2.4 years. The most common procedures among the surgical cohort were tonsillectomy and/or adenoidectomy (35.9%), arthroscopic knee repair (25.3%), and appendectomy (18.6%). Among 46 patients undergoing colectomy, the indications for surgery included inflammatory bowel disease (22 patients), benign neoplasm (11 patients), constipation (6 patients), ischemia (3 patients), malignancy of the cecum (1 patient), and unspecified (3 patients).
FIGURE 1.
Data set construction. The final data set was constructed after excluding patients without continuous insurance enrollment surrounding surgery, with subsequent procedure or anesthesia codes, or opioid prescriptions in the year before surgery. Patients were also excluded if they did not receive a perioperative opioid prescription.
TABLE 1.
Characteristics of the Study Population
| Characteristic | Surgical, n (%) | Control, n (%) |
|---|---|---|
| Total | 88 637 | 110 432 |
| Female sex | 48 200 (54.4) | 54 583 (49.4) |
| Age, y | ||
| 13 | 7050 (8) | 13 376 (12.1) |
| 14 | 8434 (9.5) | 13 969 (12.6) |
| 15 | 10 367 (11.7) | 13 694 (12.4) |
| 16 | 11 507 (13) | 13 516 (12.2) |
| 17 | 12 448 (14) | 12 903 (11.7) |
| 18 | 11 156 (12.6) | 12 012 (10.9) |
| 19 | 10 147 (11.4) | 11 137 (10.1) |
| 20 | 9234 (10.4) | 10 613 (9.6) |
| 21 | 8294 (9.4) | 9212 (8.3) |
| Procedure | ||
| Tonsillectomy and/or adenoidectomy | 31 847 (35.9) | — |
| Inguinal hernia (open or laparoscopic) | 4335 (4.9) | — |
| Umbilical or epigastric hernia | 941 (1.1) | — |
| Pectus repair (open or minimally invasive) | 739 (0.8) | — |
| Appendectomy | 16 512 (18.6) | — |
| Cholecystectomy | 7993 (9.0) | — |
| Colectomy (open or laparoscopic) | 46 (0.1) | — |
| Supracondylar fracture fixation | 162 (0.2) | — |
| Epicondylar fracture fixation | 620 (0.7) | — |
| Posterior arthrodesis | 2018 (2.3) | — |
| Arthroscopic knee repair (ACL and/or meniscus) | 22 434 (25.3) | — |
| Orchiopexy (open or laparoscopic) | 955 (1.1) | — |
| Hypospadias repair | 35 (0.0) | — |
| Complex chronic conditions | ||
| Neurologic and neuromuscular | 686 (0.8) | 244 (0.2) |
| Cardiovascular | 1865 (2.1) | 659 (0.6) |
| Respiratory | 83 (0.1) | 25 (0.0) |
| Renal and urologic | 209 (0.2) | 75 (0.1) |
| Gastrointestinal | 741 (0.8) | 140 (0.1) |
| Hematologic or immunologic | 471 (0.5) | 137 (0.1) |
| Metabolic | 1604 (1.8) | 794 (0.7) |
| Other congenital or genetic defect | 3707 (4.2) | 862 (0.8) |
| Malignancy | 2018 (2.3) | 888 (0.8) |
| Past-year mental health disorders | ||
| Depression | 1911 (2.2) | 1717 (1.6) |
| Anxiety | 2758 (3.1) | 2638 (2.4) |
| SUD | 1075 (1.2) | 827 (0.7) |
| Chronic pain diagnoses | 7230 (8.2) | 1982 (1.8) |
| Opioid prescription in 30 d before procedure | 17 126 (19.3) | — |
—, not applicable.
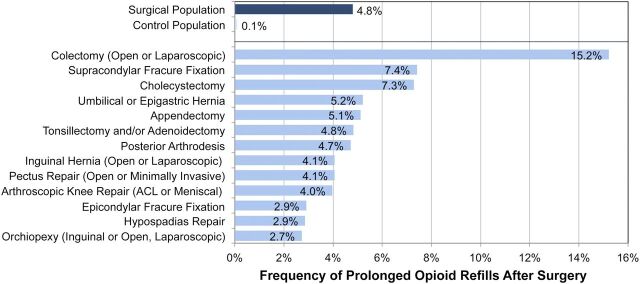
Among these patients, persistent opioid use was found in 4.8% (4267 patients), ranging from 2.7% to 15.2% across surgical procedures (Fig 2). By comparison, 53 patients (0.1%) in the nonsurgical comparison group filled an opioid prescription during the analogous time period. Among the 57 951 patients who did not fill a perioperative opioid prescription, 1.1% (616 patients) filled an opioid prescription between 3 and 6 months after surgery.
FIGURE 2.
Prolonged opioid refills by cohort and surgical procedure. The incidences of prolonged opioid refills (y-axis) among past-year opioid-naïve pediatric patients undergoing surgery, among a control cohort, and individually by procedure (x-axis) are shown.
Table 2 presents the patient and procedural factors associated with persistent opioid use. Prolonged opioid refill was most often associated with cholecystectomy (adjusted odds ratio [aOR], 1.13; 95% confidence interval [CI], 1.00–1.26) and colectomy (aOR, 2.33; 95% CI, 1.01–5.34). Risk factors that were independently associated with new persistent opioid use included older age (aOR, 1.07; 95% CI, 1.05–1.08), female sex (aOR, 1.22; 95% CI, 1.14–1.31), past-year SUD (aOR, 1.41; 95% CI, 1.12–1.77), chronic pain diagnosis (aOR, 1.48; 95% CI, 1.33–1.66), and opioid prescription filled within 30 days before surgery (aOR, 1.26; 95% CI, 1.17–1.36).
TABLE 2.
Multivariable Logistic Regression for Prolonged Opioid Refills
| aOR | 95% CI | |
|---|---|---|
| Intercept | ||
| Age | 1.07 | 1.05–1.08 |
| Female sex | 1.22 | 1.14–1.31 |
| Procedure | ||
| Appendectomy | — | — |
| Tonsillectomy and/or adenoidectomy | 0.85 | 0.77–0.92 |
| Inguinal hernia (open or laparoscopic) | 0.81 | 0.69–0.96 |
| Umbilical or epigastric hernia | 0.98 | 0.73–1.31 |
| Pectus repair (open or minimally invasive) | 0.86 | 0.59–1.26 |
| Cholecystectomy | 1.13 | 1.00–1.26 |
| Colectomy (open or laparoscopic) | 2.33 | 1.01–5.34 |
| Supracondylar fracture fixation | 1.46 | 0.81–2.65 |
| Epicondylar fracture fixation | 0.63 | 0.39–1.01 |
| Posterior arthrodesis | 0.68 | 0.54–0.87 |
| Arthroscopic knee repair (ACL and/or meniscus) | 0.74 | 0.67–0.81 |
| Orchiopexy (open or laparoscopic) | 0.62 | 0.42–0.92 |
| Hypospadias repair | 0.69 | 0.09–5.05 |
| Complex chronic conditions | ||
| Cardiovascular | 1.17 | 0.96–1.42 |
| Renal and urologic | 1.55 | 0.93–2.59 |
| Gastrointestinal | 1.29 | 0.98–1.70 |
| Malignancy | 1.16 | 0.96–1.40 |
| Past-year mental health diagnoses | ||
| Depression | 1.15 | 0.95–1.39 |
| Anxiety | 1.16 | 0.98–1.36 |
| SUD | 1.41 | 1.12–1.77 |
| Chronic pain diagnoses | 1.48 | 1.33–1.66 |
| Opioid prescription in 30 d before procedure | 1.26 | 1.17–1.36 |
—, not applicable.
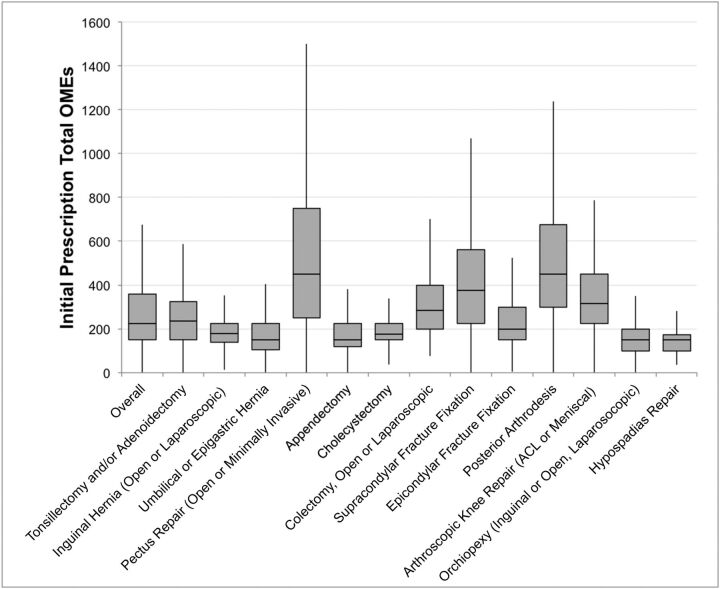
To investigate the common attributes of postoperative prescriptions among adolescents and young adults undergoing surgery, we next examined variation in the total OMEs of the initial postoperative opioid prescription by box-and-whisker plot and excluding outliers (Fig 3). The procedures with the 3 highest initial median total OMEs were posterior arthrodesis (median, 450 OMEs; mean, 695.7 OMEs; 95% CI, 0.20–1500 OMEs), pectus repair (median, 450 OMEs; mean, 776.1 OMEs; 95% CI, 0.20–2100 OMEs), and supracondylar fracture fixation (median, 375 OMEs; mean, 7400.3 OMEs; 95% CI 0.22–1000 OMEs). Evaluating for high daily dosage, there were 6317 patients (7.1%) with >100 OMEs daily on the initial postoperative prescription.
FIGURE 3.
Box-and-whisker plot of the initial prescription total OMEs. Each box represents the 25th to 75th percentiles, with the line representing the median. Outliers were excluded.
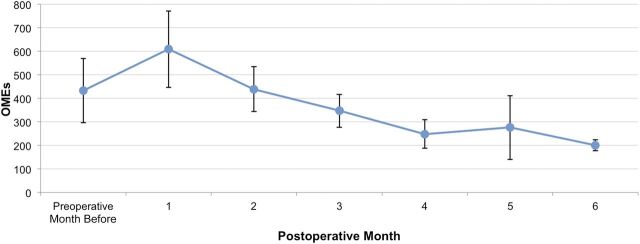
To look at dose trends over time, we calculated the average total OMEs per refill and SD among persistent opioid users as a function of postoperative month. As shown in Fig 4, there was an initial peak with the first postoperative opioid prescription (mean, 609.0 OMEs; 95% CI, 446.7–771.4 OMEs). Total OMEs per refill decreased to 347.0 OMEs (95% CI, 277.1–416.9 OMEs) by postoperative month 3 and further decreased to 248.6 OMEs (95% CI, 188.3–308.9 OMEs) at postoperative month 4, 276.2 OMEs (95% CI, 140.4–412.1 OMEs) at postoperative month 5, and 200.9 OMEs (95% CI 177.7–224.1 OMEs) at postoperative month 6.
FIGURE 4.
Average total OMEs prescribed per new prolonged user by postoperative month. The error bar represents 95% of the population.
Discussion
In this national cohort of 88 637 patients ages 13 to 21 years, we observed that ∼5% of the past-year opioid-naïve patients filled opioid prescriptions >90 days after surgery. The incidence of persistent opioid use during this time period ranged from 2.7% to 15.2% across procedures but was not entirely related to the magnitude or type of surgical procedure alone. Furthermore, patients with persistent opioid use filled additional opioid prescriptions of substantial quantity, with an average prescription of 200 to 300 OMEs up to 6 months after surgery. To place this in the context of the most commonly prescribed opioid analgesics in the United States, this is equivalent to refills of 40 tablets of hydrocodone (5 mg tablets) or 26 tablets of oxycodone (5 mg tablets) at 6 months after surgery. These findings raise concern that acute exposure to opioids for postoperative pain management may be associated with a risk of long-term use for a significant number of adolescents and young adults.
Certain procedures, such as cholecystectomy and colectomy, were associated with persistent opioid use; in contrast, other procedures that commonly result in high levels of postoperative pain, such as spinal fusion and pectus repair, showed no higher risk of persistent opioid use than the reference group (appendectomy). Because cholecystectomy and colectomy may be related to high levels of preoperative pain and inflammation with potential for visceral and central sensitization, it is possible that this finding is related to pain that failed to resolve despite surgery or that these factors may predispose the patient to long-term pain. Patient-level factors, such as past-year SUD, chronic pain diagnoses, and preoperative opioid fill, had a highly significant association with persistent opioid use at 3 to 6 months after surgery. This points toward the multifactorial etiology of postoperative pain and its complex nature in both the short- and long-term. Future work is needed to elucidate the mechanism that underlies new persistent opioid use after certain procedures and better understand the efficacy of multimodal pharmacologic and nonpharmacologic pain management approaches to ameliorate patient- and procedure-specific risk factors.
To date, the extent to which prolonged postoperative opioid use confers increased risk of subsequent opioid misuse and dependence is debated, although previous work has demonstrated that early onset of nonmedical use of prescription opioids is associated with increased risk of developing subsequent opioid abuse and other SUD later in life.23,24 Although the medical use of prescription opioids alone in adolescence has not been associated with an increased risk of SUD later in life, a significant association between medical use of prescription opioids alone in adolescence and subsequent nonmedical use of prescription opioids was observed at age 35 years (aOR, 1.74; 95% CI, 1.10–2.76).25 In addition, any nonmedical use (with or without concomitant medical use) in adolescence increased the odds of nonmedical use (aOR, 2.1–3.2) and SUD symptoms (aOR, 1.5–2.6) at age 35 years.25 The majority of US high school seniors with both medical use and nonmedical use of prescription opioids reported medical use before initiating nonmedical use of prescription opioids, suggesting a role of leftover prescriptions in the transition to a nonmedical use of prescription opioids.4 This may be due, in part, to the perception that prescription opioids are safe if they are prescribed by physicians despite the fact that the addiction potential is similar to heroin. In the Monitoring the Future study, 73% of eighth-graders among a nationally representative sample perceived an occasional use of heroin as high risk compared with 26% who perceived an occasional use of Vicodin and 33% who perceived an occasional use of OxyContin as high risk.26 They may be more to prone to use these medications, which are perceived as a pain medication, for themselves or share with others for pain purposes aside from those for which they were prescribed.
Our study is the first in which researchers evaluated persistent opioid use after surgical care in the adolescent and young adult age group, although our study has several notable limitations. First, although our findings do not reflect actual opioid consumption after pediatric surgical procedures, we captured opioid dispensing by pharmacy fills. It is likely that if refills are provided, the medication has been consumed, stored for later use, or diverted to an unintended user. Furthermore, it represents 1 of the first objective reports of opioid exposure among adolescents and young adults. The majority of existing data are drawn from self-reporting, which may be discordant to actual use.27,28 For example, 37% of high school seniors who reported past-year nonmedical use of Vicodin did not report past-year nonmedical use of prescription opioids on the same survey.28 Second, because of the administrative nature of the database, we were unable to identify the indications for prescription refills or link refills to chronic postsurgical pain or opioid use disorder. However, the higher incidence of new persistent use among postsurgical patients with opioid exposure compared with controls and those without opioid exposure raises concern that perioperative opioid prescribing may prime the patients for future opioid use for any cause and increase the quantity of prescription opioids that are accessible to the patient and community. Finally, our study is limited to a population of dependents of individuals with employer-based insurance and may not be generalizable to patients without insurance or those with exclusively state or federal health care coverage, such as Medicare or Medicaid programs. Of children, ∼37% are insured by the Children’s Health Insurance Program or Medicaid programs29 and will be an important population cohort to evaluate in the future.
Despite these limitations, our findings have important implications for future efforts with regard to perioperative prescribing for the adolescent and young adult age group. Our findings echo those of recent studies of adult populations7,12–14,30–32 in observing an increase in long-term opioid use after new opioid prescriptions in both the general population and postoperative settings. Yet, these results must be taken with specific regard to the age of this young cohort, contributing to an even greater overall, lifetime risk for chronic opioid use and its downstream effects. It is concerning not only that patients may be requesting prescription opioids for prolonged periods after surgery but also that providers are continuing to prescribe opioids. Recent guidelines suggest limiting the reliance on opioids for treating chronic noncancer pain; however, evidence-based guidelines for postoperative opioid prescribing and monitoring in children and self-administering adolescents and young adults are limited or primarily adapted from adult dosing despite recent studies suggesting overprescribing after surgery.8,33–35 Future work must be aimed at identifying in what settings (surgery clinic, emergency department, primary care clinic, etc) these prescriptions are being obtained. This will allow guidelines to be effectively targeted at the highest-yield audience to optimize acute and chronic postoperative pain management.
Opioids are highly effective for acute postoperative pain relief; however, our findings offer new evidence that prolonged perioperative opioid refills may be placing vulnerable adolescent and young adult patients and their local communities at a higher risk than previously appreciated. Prescription drug use in an unmonitored setting by a patient who is not familiar with dosing and side effect profiles may place the user at undue risk even if the drug is used without recreational intent. This has been highlighted by rises in the most serious prescription opioid–related adverse outcomes among adolescents despite declining overall use over the last 5 years.4–6 As a result of this work, we may better identify those patients who are at the highest risk for new persistent opioid use, such as adolescents and young adults with past-year SUD and chronic pain conditions. Importantly, we are not suggesting that patients should be prescribed fewer opioid pain medications on the basis of preexisting diagnoses nor that pain should be underappreciated and undertreated. Instead, we recommend that all providers should screen for preexisting risk factors to identify those who may require increased monitoring and intervention for the patient’s safety. Furthermore, this emphasizes the need for multimodal analgesic techniques to control pain and avoid unnecessary opioid exposure when feasible. It is our responsibility as providers to identify evidence-based strategies for safe postoperative prescribing, appropriate patient and parent education, and proper disposal avenues for unused medications with the intent to improve surgical quality and prevent opioid-associated morbidity and mortality.
Conclusions
Among a cohort of past-year opioid-naïve adolescents and young adults, ∼5% filled opioid prescriptions >3 months after surgery. Certain procedural and patient risk factors are associated with persistent postoperative opioid use among adolescents and young adults. Understanding these risks may help clinicians to strategize methods to minimize opioid exposure for those at the highest risk for later misuse.
Supplementary Material
Glossary
- ACL
anterior cruciate ligament
- aOR
adjusted odds ratio
- CCCC
complex chronic condition code
- CI
confidence interval
- CPT
Current Procedural Terminology
- ICD-9
International Classification of Diseases, Ninth Revision
- OME
oral morphine equivalent
- SUD
substance use disorder
Footnotes
Dr Harbaugh conceptualized and designed the study, interpreted the data, drafted the initial manuscript, and reviewed and revised the manuscript; Drs Lee and Englesbe conceptualized and designed the study and reviewed the manuscript; Dr Hu acquired, analyzed, and interpreted the data, and reviewed and revised the manuscript; Drs McCabe and Voepel-Lewis critically reviewed and revised the manuscript for important intellectual content; Drs Waljee and Brummett conceptualized and designed the study, interpreted the data, and critically reviewed and revised the manuscript for important intellectual content; and all authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
FUNDING: Funded by the Michigan Department of Health and Human Services.
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2017-3054.
References
- 1.Kolodny A, Courtwright DT, Hwang CS, et al. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health. 2015;36:559–574 [DOI] [PubMed] [Google Scholar]
- 2.Bohnert AS, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315–1321 [DOI] [PubMed] [Google Scholar]
- 3.Bohnert AS, Ilgen MA, Trafton JA, et al. Trends and regional variation in opioid overdose mortality among Veterans Health Administration patients, fiscal year 2001 to 2009. Clin J Pain. 2014;30(7):605–612 [DOI] [PubMed] [Google Scholar]
- 4.McCabe SE, West BT, Veliz P, McCabe VV, Stoddard SA, Boyd CJ. Trends in medical and nonmedical use of prescription opioids among US adolescents: 1976-2015. Pediatrics. 2017;139(4):e20162387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gaither JR, Leventhal JM, Ryan SA, Camenga DR. National trends in hospitalizations for opioid poisonings among children and adolescents, 1997 to 2012. JAMA Pediatr. 2016;170(12):1195–1201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Allen JD, Casavant MJ, Spiller HA, Chounthirath T, Hodges NL, Smith GA. Prescription opioid exposures among children and adolescents in the United States: 2000-2015. Pediatrics. 2017;139(4):e20163382. [DOI] [PubMed] [Google Scholar]
- 7.Clarke H, Soneji N, Ko DT, Yun L, Wijeysundera DN. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ. 2014;348:g1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hill MV, McMahon ML, Stucke RS, Barth RJ Jr. Wide variation and excessive dosage of opioid prescriptions for common general surgical procedures. Ann Surg. 2017;265(4):709–714 [DOI] [PubMed] [Google Scholar]
- 9.Waljee JF, Zhong L, Hou H, Sears E, Brummett C, Chung KC. The use of opioid analgesics following common upper extremity surgical procedures: a national, population-based study. Plast Reconstr Surg. 2016;137(2):355e–364e [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wunsch H, Wijeysundera DN, Passarella MA, Neuman MD. Opioids prescribed after low-risk surgical procedures in the United States, 2004-2012. JAMA. 2016;315(15):1654–1657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Voepel-Lewis T, Wagner D, Tait AR. Leftover prescription opioids after minor procedures: an unwitting source for accidental overdose in children. JAMA Pediatr. 2015;169(5):497–498 [DOI] [PubMed] [Google Scholar]
- 12.Alam A, Gomes T, Zheng H, Mamdani MM, Juurlink DN, Bell CM. Long-term analgesic use after low-risk surgery: a retrospective cohort study. Arch Intern Med. 2012;172(5):425–430 [DOI] [PubMed] [Google Scholar]
- 13.Brummett CM, Waljee JF, Goesling J, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017;152(6):e170504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sun EC, Darnall BD, Baker LC, Mackey S. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016;176(9):1286–1293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schramm-Sapyta NL, Walker QD, Caster JM, Levin ED, Kuhn CM. Are adolescents more vulnerable to drug addiction than adults? Evidence from animal models. Psychopharmacology (Berl). 2009;206(1):1–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCabe SE, West BT, Boyd CJ. Leftover prescription opioids and nonmedical use among high school seniors: a multi-cohort national study. J Adolesc Health. 2013;52(4):480–485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vaughn MG, Nelson EJ, Salas-Wright CP, Qian Z, Schootman M. Racial and ethnic trends and correlates of non-medical use of prescription opioids among adolescents in the United States 2004-2013. J Psychiatr Res. 2016;73:17–24 [DOI] [PubMed] [Google Scholar]
- 18.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014;14:199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Friedrichsdorf SJ, Giordano J, Desai Dakoji K, Warmuth A, Daughtry C, Schulz CA. Chronic pain in children and adolescents: diagnosis and treatment of primary pain disorders in head, abdomen, muscles and joints. Children (Basel). 2016;3(4):e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention . Calculating total daily dose of opioids for safer dosage. Available at: https://www.cdc.gov/drugoverdose/pdf/calculating_total_daily_dose-a.pdf. Accessed July 7, 2017
- 21.Liu Y, Logan JE, Paulozzi LJ, Zhang K, Jones CM. Potential misuse and inappropriate prescription practices involving opioid analgesics. Am J Manag Care. 2013;19(8):648–665 [PubMed] [Google Scholar]
- 22.International Association for the Study of Pain . IASP task force for the classification of chronic pain in ICD-11 prepares new criteria on postsurgical and posttraumatic pain. 2016. Available at: https://www.iasp-pain.org/PublicationsNews/NewsDetail.aspx?ItemNumber=5134&navItemNumber=643. Accessed March 17, 2017
- 23.McCabe SE, West BT, Morales M, Cranford JA, Boyd CJ. Does early onset of non-medical use of prescription drugs predict subsequent prescription drug abuse and dependence? Results from a national study. Addiction. 2007;102(12):1920–1930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miech R, Johnston L, O’Malley PM, Keyes KM, Heard K. Prescription opioids in adolescence and future opioid misuse. Pediatrics. 2015;136(5). Available at: www.pediatrics.org/cgi/content/full/136/5/e1169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McCabe SE, Veliz P, Schulenberg JE. Adolescent context of exposure to prescription opioids and substance use disorder symptoms at age 35: a national longitudinal study. Pain. 2016;157(10):2173–2178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future National Survey Results on Drug Use, 1975–2015. Ann Arbor, MI: The University of Michigan; 2016 [Google Scholar]
- 27.Johnson TP. Sources of error in substance use prevalence surveys. Int Sch Res Notices. 2014;2014:923290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Palamar JJ, Shearston JA, Cleland CM. Discordant reporting of nonmedical opioid use in a nationally representative sample of US high school seniors. Am J Drug Alcohol Abuse. 2016;42(5):530–538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Medicaid and Children’s Health Insurance Program Payment and Access Commission . Section 1: overview—key statistics. MACStats: Medicaid and CHIP Data Book. Washington, DC: Medicaid and CHIP Payment and Access Commission; 2016 [Google Scholar]
- 30.Bateman BT, Franklin JM, Bykov K, et al. Persistent opioid use following cesarean delivery: patterns and predictors among opioid-naïve women. Am J Obstet Gynecol. 2016;215(3):353.e1–353.e18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Deyo RA, Hallvik SE, Hildebran C, et al. Association between initial opioid prescribing patterns and subsequent long-term use among opioid-naïve patients: a statewide retrospective cohort study. J Gen Intern Med. 2017;32(1):21–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shah A, Hayes CJ, Martin BC. Characteristics of initial prescription episodes and likelihood of long-term opioid use—United States, 2006-2015. MMWR Morb Mortal Wkly Rep. 2017;66(10):265–269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schechter NL, Walco GA. The potential impact on children of the CDC guideline for prescribing opioids for chronic pain: above all, do no harm. JAMA Pediatr. 2016;170(5):425–426 [DOI] [PubMed] [Google Scholar]
- 34.Dautremont EA, Ebramzadeh E, Beck JJ, Bowen RE, Sangiorgio SN. Opioid prescription and usage in adolescents undergoing orthopaedic surgery in the United States: a systematic review. JBJS Rev. 2017;5(8):e5. [DOI] [PubMed] [Google Scholar]
- 35.Bicket MC, Long JJ, Pronovost PJ, Alexander GC, Wu CL. Prescription opioid analgesics commonly unused after surgery: a systematic review [published online ahead of print August 2, 2017]. JAMA Surg. doi: 10.1001/jamasurg.2017.0831 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.