ABSTRACT
International sporting competitions, including the Paralympic Games, are increasingly being held in hot and/or humid environmental conditions. Thus, a greater emphasis is being placed on preparing athletes for the potentially challenging environmental conditions of the host cities, such as the upcoming Games in Tokyo in 2020. However, evidence-based practices are limited for the impairment groups that are eligible to compete in Paralympic sport. This review aims to provide an overview of heat-related issues for Paralympic athletes alongside current recommendations to reduce thermal strain and technological advancements in the lead up to the Tokyo 2020 Paralympic Games. When competing in challenging environmental conditions, a number of factors may contribute to an athlete’s predisposition to heightened thermal strain. These include the characteristics of the sport itself (type, intensity, duration, modality, and environmental conditions), the complexity and severity of the impairment and classification of the athlete. For heat vulnerable Paralympic athletes, strategies such as the implementation of cooling methods and heat acclimation can be used to combat the increase in heat strain. At an organizational level, regulations and specific heat policies should be considered for several Paralympic sports. Both the utilization of individual strategies and specific heat health policies should be employed to ensure that Paralympics athletes’ health and sporting performance are not negatively affected during the competition in the heat at the Tokyo 2020 Paralympic Games.
KEYWORDS: Paralympic, heat, Tokyo 2020, performance, sport
Introduction
Since the beginning of the Paralympic movement in 1948, the Paralympic Games has experienced rapid growth and is now considered one of the largest multi-sport events in the world. From humble beginnings in 1948 to 4,328 athletes from 159 nations competing at the Games in Rio De Janeiro in 2016 [1], Paralympic athletes have a prominent worldwide stage to display their sporting prowess. Such growth can be partly explained by the evolution of both bespoke equipment [2] and evidence-based sport science and medicine support [3], enabling advancements in elite competitive performance of Paralympic sports.
In recent years a greater emphasis has been placed on preparing athletes, both Olympic and Paralympic, for the potential challenging environmental conditions of the host cities, such as Rio de Janeiro in 2016 and the upcoming Games in Tokyo in 2020. Despite previous Games being held in Athens, Beijing, and Rio, the impending Games in Tokyo could be one of the most thermally demanding for both athletes and spectators alike [4,5]. Competing nations are dedicating time and resources to employ techniques which either adapt training to cope with the conditions and/or develop strategies that can be utilized during the competition to reduce the risk of heat-related illnesses and a decrement in sporting performance. To highlight the expected environmental conditions for Tokyo 2020, Figure 1 shows hourly temperature and relative humidity for Tokyo during the dates corresponding to the Paralympic Games period in 2020, based on meteorological data collected from 1990 to 2018 from the Japan Meteorological Agency [5]. The figure clearly shows the potential environmental challenge athletes may face. Of note, the ambient temperature peaks at 13:00 h at 29.7 ± 3.4°C, while the relative humidity peaks at 05:00 at 78 ± 9%, decreasing to 59 ± 13% at the hottest part of the day before rising again [5].
Figure 1.
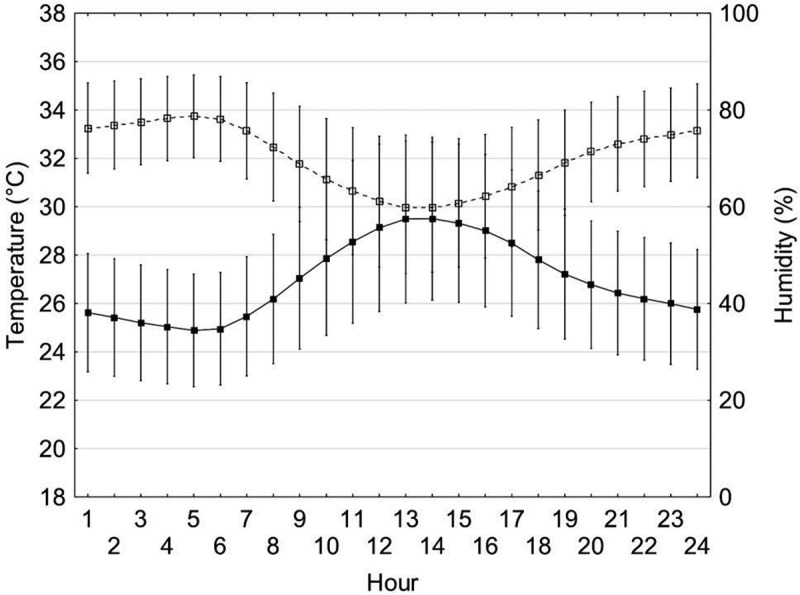
Hourly temperature and relative humidity for Tokyo during the dates corresponding to the Paralympic Games period in 2020, based on meteorological data collected from 1990 to 2018 [5]. Copyright permission has been granted from the authors of [5]
For many Paralympic athletes, their impairment affects both training and performance capabilities. The burden of thermally stressful environmental conditions will likely only exacerbate any decrement in training and competition capability and functionality. This review aims to encompass a number of topic areas within the broader scope of heat-related issues for Paralympic athletes, in order to provide an overview of heat-related issues for Paralympic athletes, alongside current recommendations in the lead up to the Tokyo 2020 Paralympic Games.
Heat-related issues for Olympic athletes
It is well recognized that exercising in hot and or/humid ambient conditions increases physiological and psychological strain causing a decrement in sporting performance compared to performing exercise in cooler conditions [6–8]. The diminished performance is associated with cardiovascular, neuromuscular, perceptual and metabolic alterations [9] resulting in an increase in core temperature, premature fatigue and the potential for heat-related illnesses. In hot and humid environments, heat gain will be increased due to the environmental heat load, while heat loss will be impaired as a result of a reduced temperature and vapor pressure gradient between the skin and environment. Thus, the need for strategies that prevent excessive heat storage is paramount from both a health and performance perspective.
Paralympic games
The Tokyo Paralympic Games will be held from 25 August to 6 September 2020 with an expected 4,400 athletes competing across 22 sports [10]. Paralympic sports either develop as an adaptation to an able-bodied (AB) equivalent sport (i.e. wheelchair basketball) or are designed to accommodate a particular impairment type (i.e. goalball for athletes with a visual impairment). Athletes with a range of physical and intellectual impairments are eligible to compete at the Paralympic Games categorized into 10 impairment types according to the International Paralympic Committee (IPC): impaired muscle power, impaired passive range of movement, limb deficiency, leg length difference, short stature, hypertonia, ataxia, athetosis, vision impairment and intellectual impairment [11]. For the purposes of this review and to align with the terms used by research conducted in this area, athletes will be grouped according to the following six disability groups, which encompass all 10 of the impairment types listed above; spinal cord-related disability, cerebral palsy, amputee, visual impairment, les autres (others) and intellectual impairment.
To obtain fair competition between athletes with varying levels of impairment, Paralympic sports utilize classification systems [11]. The premise of these systems is that classification should only cover the effect of the impairment on the individual’s sporting performance. In team sports, an athlete’s classification can play an important role in determining the individual’s role within the team [12]. However, athletes are classified according to their functional ability obtained from a range of functional tests and observational assessment during the sporting performance, rather than their physiology. Hence, athletes within the same class may be similar in relation to their functionally, yet as a result of their impairment, their physiological responses while competing in their sport, such as temperature regulation, may greatly differ [13].
Paralympic athletes at greatest thermoregulatory risk
Paralympic sport is growing rapidly, creating new challenges for athletes, coaches, governing bodies, practitioners, and researchers. One of these challenges is how to best prepare athletes for international competitions with limited evidence-based practices available for the different impairment groups. Restrictions within national high-performance systems to share training practice data and the small heterogeneous group of elite Paralympic athletes inhibit the distribution of scientific evidence and practice [14]. As a consequence, anecdotal evidence and case study work are heavily relied upon in addition to the application of AB guidance. For some instances, AB guidance may be sufficient, yet considerations regarding the athlete’s impairment and the athlete–equipment interface (where applicable) are vital.
In Paralympic sports, a number of factors may contribute to an athlete’s predisposition to heightened thermal strain when competing in challenging environmental conditions. These include not only the characteristics of the sport itself (type, intensity, duration, modality, and environmental conditions), fitness, and physical attributes of the athlete (e.g. body composition) but also the complexity of the impairment and classification of the athlete. Figure 2 depicts the interaction of these factors to illustrate the most at risk Paralympic athletes when competing in the heat, categorized by sport. The following sections provide detail on each of the impairment groups (spinal cord injury, cerebral palsy, amputation, visual impairment, and multiple sclerosis (within les autres category) that are eligible to compete in the most at-risk sports to heat stress or illness. For clarification, Table 1 depicts the sports that each of these impairment groups is eligible to compete in.
Figure 2.

Graphical representation of Paralympic athletes’ risk of thermal strain stratified by sport. The grey shaded dots represent indoor sports, while the white dots represent outdoor sports. The figure is subjectively determined through the combination of the demands of the environment and/or the sport (type, intensity, duration, modality) and the commonality of athletes within the sport that have impairments that affect their ability to thermoregulate effectively, e.g. athletes with a spinal cord injury.
Table 1.
Summary of the 22 Paralympic summer sports, the at-risk impairment groups are eligible to compete in. Note: Multiple sclerosis has not been listed as an impairment group as the health condition is only a small proportion of the les autres impairment group.
| Impairment type |
|||||
|---|---|---|---|---|---|
| Sport | Tetraplegic | Paraplegic | Cerebral palsy | Amputee | Visual Impairment |
| Archery | * | * | * | * | |
| Athletics | * | * | * | * | * |
| Badminton | * | * | * | * | |
| Boccia | * | * | * | * | |
| Canoe | * | * | * | ||
| Cycling | * | * | * | * | * |
| Equestrian | * | * | * | * | * |
| Football | * | ||||
| Goalball | * | ||||
| Judo | * | ||||
| Powerlifting | * | * | * | ||
| Rowing | * | * | * | * | * |
| Shooting | * | * | * | * | |
| Sitting volleyball | * | * | * | ||
| Swimming | * | * | * | * | * |
| Table tennis | * | * | * | * | |
| Taekwondo | * | * | |||
| Triathlon | * | * | * | * | * |
| Wheelchair basketball | * | * | * | ||
| Wheelchair fencing | * | * | * | * | |
| Wheelchair rugby | * | * | * | * | |
| Wheelchair tennis | * | * | * | * | |
Protective clothing may also increase thermal strain, especially for athletes competing in sports such as equestrian, wheelchair fencing, and shooting. The additional weight of the clothing increases metabolic heat production, and the additional clothing layer increases insulation, impairing heat loss from the skin surface to the environment. The resulting reduction in convective and evaporative heat loss for athletes wearing protective clothing while competing has implications for both sports of a moderate intensity and relatively static sports but of a longer duration. Hence, in addition to the potential difficulties faced by the different impairment groups mentioned below, Paralympic athletes competing in these sports with the additional burden of protective clothing should ensure appropriate strategies (see section current recommendations) are in place to avoid any heat-related issues.
Spinal cord injury
Out of the six impairment groups, spinal cord injury (SCI) is the most comprehensively researched in relation to athletic performance [14]. Athletes with an SCI are eligible to compete in a number of sports including wheelchair rugby, archery, triathlon, wheelchair tennis and athletics (See Table 1). An SCI may occur through either application of extreme traumatic forces or via degenerative and congenital disorders. Individuals with an SCI experience varying degrees of sensory, motor and functional loss depending on the level of their injury. Injury to the cervical region of the spinal cord is referred to as tetraplegia leading to impaired function of the arms, trunk, legs and pelvic organs. Injury to the thoracic, lumbar and sacral segments of the spinal cord, referred to as paraplegia affects the function of the trunk and pelvic organs below the lesion level and the legs. Spinal cord injuries are further classified as being neurologically complete or incomplete in relation to the motor or sensory function [15,16].
Individuals with an SCI have a reduced afferent input to the thermoregulatory center [17–19] and a loss of both sweating capacity and vasomotor control (efferent response) below the lesion level [17,20,21]. The magnitude of the thermoregulatory impairment is proportional to the level and completeness of the lesion. Due to the higher lesion level, individuals with tetraplegia possess a smaller area of sensate skin, a lesser amount of afferent input regarding their thermal state, and a reduced efferent response compared to individuals with paraplegia [21,22]. Depending on the level of the SCI, varying degrees of disruption to the sympathetic and parasympathetic nervous system are apparent. Below the level of the lesion, the lack of sympathetic vasoconstriction and muscle pump inactivity results in a limited ability to redistribute blood [23] with apparent consequences for convective heat loss. In a sporting context, as a result of muscular paralysis below the lesion level and the use of upper body exercise, the amount of heat produced by athletes with an SCI is likely determined by the amount of remaining active musculature.
Previous literature has consistently shown that athletes with an SCI demonstrate greater thermal strain compared to the AB during both rest [22,24] and exercise [25,26] in hot ambient conditions. In these conditions, athletes with tetraplegia experience a greater thermal strain compared to athletes with paraplegia during exercise [26]. Therefore, it may be surprising that out of all the sports that athletes with an SCI are eligible to compete in, only wheelchair tennis has a heat health policy specifically for wheelchair-bound athletes [27,28]. Despite the growing research in this population group, little has been translated into policy and practice. Thus, the current review sows the seeds for further discussion and research that may challenge or help guide practical and competitive scheduling recommendations.
Unlike the other impairment groups, wheelchair rugby players with tetraplegia demonstrate heightened thermal strain even when competing indoors (19–21°C), despite a lack of external heat load [29]. These players with tetraplegia tend to occupy defensive roles on the court due to their classification as low point players, hence cover less distance and achieve lower mean speeds than high point players [12,29]. However, as a consequence of a loss of vasomotor control and the lack of any sweating response [17,20–22], owing to the fact that the sympathetic innervation to eccrine sweat glands exits the spinal cord at T1-L2, these players can often reach high core temperatures (>39.5°C) during a match [29]. Additionally, the continual increase in core temperature post exercise [30] for a prolonged duration compared to the AB and the common occurrence of multiple matches in one day is likely to exacerbate the situation. It is clear that the heightened thermal strain for these athletes has implications for not only performance and decision-making abilities but also an increased risk of heat-related illnesses for both athletes competing in indoor and outdoor sports.
Unlike AB athletes when exercising in the heat, an increase in fluid intake is not physiologically required due to the limited sweating response of athletes with an SCI. Instead, the advice is to consume fluid little and often to not only ensure hydration, avoid excessive weight gain and gastrointestinal discomfort, but also to reduce the risk of urinary tract infections [31]. Athletes with an SCI must also be aware of triggering autonomic dysreflexia as a result of bladder distension through excessive over drinking, though this condition can be caused by a number of other stimuli. Autonomic dysreflexia is an acute condition of excessive, uncontrolled sympathetic output resulting in extreme hypertension with potential fatal consequences [32]. Prompt action must be undertaken to remove the cause and emptying of catheters is encouraged prior to exercise to prevent the occurrence. While the condition is reported to be fairly common, prevalence is highest in athletes with lesions above T6 [32]. It is also relatively common for athletes to purposefully dehydrate during long haul travel to avoid the inconvenience of visiting the toilet without assistance [31]. Therefore, an appropriate fluid strategy while traveling requires some planning and educational advice to prevent athletes from arriving at competitions in a dehydrated state.
Cerebral palsy
Cerebral palsy (CP) is a postural and movement disorder caused by central brain injury which results in altered neuromuscular physiology and diminished exercise capacity [33]. Cerebral palsy presents three main impairment profiles: hemiplegia where one side of the body is affected; diplegia where two limbs are affected (typically the lower limbs) and quadriplegia where all four limbs are affected [34]. Based on their functional capabilities assessed during the respective classification processes, athletes with CP may compete in wheelchair or ambulant sport classes, such as triathlon, road cycling, athletics, archery, and equestrian (Table 1).
Due to the presence of athetosis, hypertonia or ataxia, athletes with CP typically display an impairment in muscular coordination and thus movement efficiency. This impairment results in a greater metabolic cost of movement for a set intensity, relative to AB individuals [35]. Consequently, it has been shown that metabolic heat production for a given external workload is significantly greater in those with CP [36]. Maltais et al. [36] proposed that the etiology of this greater thermal strain relates to the elevated metabolic cost of absolute workloads. The lower efficiency of movement and higher energy cost is likely to result in an earlier onset of fatigue, exacerbated by an additional environmental heat load.
Another potential consequence of athletes’ high muscular tone is an impairment in venous return. Due to a diminished efficiency of muscle pumps, redistribution of venous blood from the periphery to the central circulation can be negatively impacted. This increases the relative intensity of exercise as heart rate increases to compensate for a lower stroke volume [37]. Moreover, there is potential that athletes with CP may employ medical techniques to ameliorate their muscle spasticity and limited range of motion. Specifically, it is common for children with CP to be treated with botulinum toxin A (Botox®) injections in the lower limbs to manage spasticity and improve range of motion [38]. Botulinum toxin A is also used to treat hyperhidrosis as it blocks the release of acetylcholine reducing sweat production at the site [39]. Although the prevalence of botulinum toxin A use in athletic populations to manage spasticity is currently unknown, the potential effect on local sweat production may result in a lower evaporative heat loss capacity and a diminished local adaptive potential during heat acclimation.
Athletes with CP not only display physiological differences to AB athletes that may increase their thermal strain but also cognitive differences. Although research is lacking, Runciman et al. [33] and Maltais et al. [36] demonstrated that there may be potential differences in pace awareness and/or perception of effort in athletes with CP. When competing in the heat, AB athletes typically progressively down-regulate their intensity of effort to redistribute work in a manner that allows them to complete the required task in the context of the accumulating heat strain [40]. This not only relates to physiological adjustments but also behavioral alterations to account for the cognitive interpretation of the environment, thermal state, and/or perceived effort [41,42]. If athletes with CP are unable to effectively process the aforementioned factors, they may increase the risk of heat-related illnesses and/or performance impairment as a consequence of maintaining an inappropriate workload for the environmental context. In support of this, anecdotal observations have shown elite CP athletes falling over in the closing stages of 100–400 m running races.
Amputation
Athletes with an amputation, especially of a lower limb, are of a particular concern when competing in sports in the heat, such as triathlon and cycling (road race), due to the intensity of these sports and the duration of exposure to the ambient environment. The potential for heightened heat strain in these athletes is mainly due to a combination of reduced surface area for convective and evaporative heat loss [43], particularly in athletes with a bilateral amputation, gait asymmetries elevating heat production and the disturbance of all thermal transfer mechanisms due to the prosthetic socket barrier [44].
Athletes with an amputation have a reduction in heat dissipation, as a result of a loss of limb and the covering of the residual limb with a prosthetic. Thus, a smaller body surface area is available for heat loss leading to a potential increase in heat storage during exercise. Skin grafts on the amputated limb could also further impair heat dissipation due to the absence of sweat gland responsiveness and a potential permanent impairment of cutaneous vasodilator capacity on grafted skin [43]. The magnitude of the effect on heat dissipation will likely depend on the amount of body surface area covered by the grafted skin.
Previous research has demonstrated that when walking at similar speeds, individuals with an amputation expend more energy than an individual with no amputation [45], and the more proximal the amputation, the larger the effort needed to walk [46]. For instance, transtibial amputees have been shown to expend between 9% and 33% more energy [47,48] and transfemoral amputees between 37% and 100% more energy compared to non-amputee individuals [49]. The mass of the prosthesis does not appear to significantly increase energy expended [50], yet metabolic cost can be reduced by improvements in both gait and physical fitness [45]. These findings suggest that during walking metabolic heat production may be greater in these individuals compared to the AB, coupled with a reduction in heat loss, these athletes may be at a greater risk of heat-related illnesses. However, due to the lack of thermoregulation research for this population group this speculation cannot currently be confirmed or extended to other modalities.
Although prosthetic technological development, in particular sport-specific prosthetics, has grown rapidly with the rise of Paralympic sport, issues with sweat accumulation, comfort, and skin breakdowns are still commonplace. To ensure a good prosthetic fit, close-fitting is required, consequently limiting ventilation at the socket–limb interface. Without adequate ventilation and low moisture permeability of the socket, a build-up of sweat and high residual limb skin temperature will occur. These effects have severe consequences, such as skin irritation, bacterial infection and a reduction in prosthetic use and activity. An increase in skin temperature of the amputated limb at rest is a clear sign of tissue stress and with the presence of slight moisture is likely to cause friction blisters [51]. In addition to these health-related concerns, individuals frequently report feelings of thermal discomfort inside the prosthesis regardless of the level of amputation or type of prosthesis [44]. The localized thermal discomfort could potentially affect their overall feelings of thermal comfort. For athletes, this could result in a decreased use of the prosthetic that will negatively impact on the quality of their training. It is also important to note that to accommodate both daily and sporting activities, athletes will have access to multiple prosthetics; therefore, the issues mentioned above would need to be addressed in all the prosthetics used by the athlete, i.e. both daily and sporting use.
Development of the material properties used in the prosthetic liner has been well studied, but less so for in vivo studies [52]. Despite the technological advancements in liner materials and the suggestion that increasing the thermal conductivity of interface components could improve heat transfer as well as integrated cooling systems [53], there does not seem to be a current solution to the problem [54]. A better understanding of the microclimate of the prosthetic-limb interface, although difficult to measure, is greatly warranted during exercise to help solve the problem of sweat accumulation within the prosthetic socket and liner.
Visual impairment
Visually impaired athletes eligible to compete in Paralympic sports have damage to either one or more components of the visual system, resulting in an impairment in the interaction of the individual with the surrounding environment. Similar to athletes with an amputation, visually impaired athletes are eligible to compete in a number of endurance sports, which also expose athletes to the challenging environmental conditions for a prolonged period. These athletes may be physiologically similar to AB athletes, but as a consequence of their impairment, additional considerations are needed when training for and competing in the heat.
Adopting an appropriate pacing strategy when competing in the heat is essential in the sports of triathlon, road race cycling and the marathon, all sports for which visually impaired athletes are eligible (Table 1). Athletes with a visual impairment are unable to rely on visual feedback and cues to adapt their pacing. Therefore, if an adjusted pacing strategy has not been set in accordance with the ambient conditions and the athlete is not using visual cues to potentially downregulate their effort, these athletes could face heightened thermal strain as a result of inappropriate pacing for the conditions. For visually impaired athletes that compete with a guide (depending on their classification and sport), this may be less of an issue, as the guide’s role is to read the environment and provide verbal and tactile cues to the athlete.
Ensuring sufficient hydration to replace sweat and respiratory water losses is key for athletes, especially when training for competition in the heat. Self-monitoring hydration is commonly conducted through checking urine color and volume, to prevent dehydration and hence reduce the amount of thermoregulatory strain. However, for athletes with a visual impairment, this is extremely difficult. Thus, these athletes are likely to require assistance or another method for assessing hydration status. A number of visually impaired athletes also suffer from albinism and are therefore prone to sunburn when exposed to ambient conditions of high radiant load, due to the lack of skin pigmentation [55]. Sunburn has a direct local effect on sweat gland responsiveness and capacity limiting the thermoregulatory effector response, but also heightening thermal sensation [56]. Hence, reducing time in the sun and ensuring sun cream is applied frequently is crucial for these athletes. Current research is however inconclusive regarding the effect of sun cream on sweat production and evaporation [57–59].
Les autres – multiple sclerosis
Athletes with multiple sclerosis (MS) form a small proportion of the les autres impairment group. Multiple sclerosis (MS) is a degenerative neurological disorder that disrupts axonal myelin in the central nervous system mostly affecting young individuals from 20 to 40 years old. In general, alterations in saltatory conduction, slowed conduction velocity, and a tendency to conduction block are as a result of the demyelination. Multiple sclerosis may also cause an impaired neural control of autonomic functions involving impaired sensory and effector responses, altered neural integration within the central nervous system or a combination of all these factors [60]. Symptoms vary between individuals but often include deficits related to coordinated movement, such as muscle weakness, spasms, and fatigue. MS lesions within thermoregulatory centers of the central nervous system, particularly the hypothalamus, likely result in impaired thermoregulatory function due to the alteration in neural conduction [61].
During exercise and/or during exposure to hot environments individuals with MS can experience heat intolerance, resulting in a rapid onset of fatigue and slowed or blocked conduction of demyelinated nerves [62,63]. The degree to which heat sensitivity limits physical function in these individuals is likely to be related to the severity of the condition. For example, the greater the degree of demyelination the less heat exposure is needed to cause blocked conduction [60]. A core temperature increase as little as 0.5°C can exacerbate MS symptoms transiently in 60–80% of MS patients (heat sensitivity), highlighting the need for this population group to reduce exercise-induced hyperthermia [64–66]. However, the effects of their heat sensitivity are temporary, transient and reversible by either providing cooling or removing the environmental stressor. For a thorough review of the impact of temperature sensitivity on sensory and cognitive function in individuals with MS, readers are directed to [67].
The ability of individuals with MS to dissipate heat is also likely impaired with significantly reduced sweat rates, as a function of core temperature, observed during whole body passive heating [68]. Allen et al. [68] suggested that this reduction in sweat rate may be due to either neural-induced changes in eccrine sweat glands or impairments in neural control of sudomotor pathways. Nonetheless, changes in skin blood flow appear to be similar to AB individuals suggesting reflex control of the cutaneous vasculature is preserved in individuals with MS [68]. However, it is unclear if a similar finding would be observed during greater heat stress.
Nevertheless, there are a lack of studies involving athletes with MS and exercise representative of high-performance Paralympic sport. A greater understanding of athletes with MS during exercise in the heat is needed to determine appropriate strategies to prevent the worsening of their symptoms. Similar to the other impairment groups, athletes with MS have varying degrees of functionality and mobility, thus for appropriate and individualized strategies case study work may be more appropriate.
Summary of paralympic athletes at greatest thermoregulatory risk
The aforementioned sections have demonstrated how thermoregulation and sporting performance of Paralympic athletes with various impairments may be compromised when competing in the heat. In summary, in relation to heat exchange, both convective and evaporative heat loss and metabolic heat production will be affected as a result of the Paralympic athlete’s disability, highlighted in Figure 3. The metabolic heat production of Paralympic athletes is likely to be altered because of their impairment, for instance being lower in athletes with an SCI, while greater in athletes with CP and athletes with an amputation, compared to the AB. In relation to heat loss, convective and evaporative heat loss are likely to be impaired due to a smaller body surface area of active muscle mass, reductions in vasomotor and sweating control and alterations in pacing strategy. Thus, the disability groups mentioned in the sections above are likely to store a greater amount of heat leading to an increase in thermal strain, as a result of a reduction in convective and evaporative heat loss and, for some groups, also an increase in metabolic heat production (Figure 3).
Figure 3.
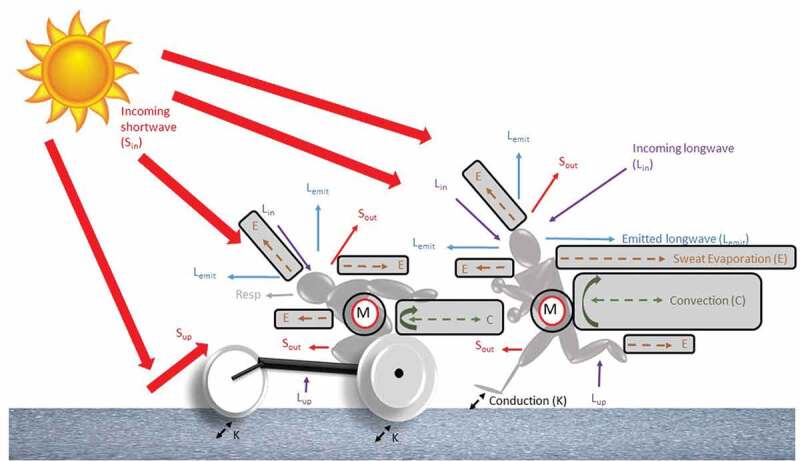
Heat exchange between the environment and the human body in an outdoor environment. In normal conditions, heat balance will increase due to an increase in metabolic heat production (M) and radiation in both shortwave (Sin and Sup) and longwave (Lin and Lup) radiation. A human usually loses heat through convection (C), evaporation (E), respiration (resp) and emitted longwave radiation (Lemit). The grey boxes highlight the heat exchange pathways (convective and evaporative heat loss and metabolic heat production) affected as a result of the Paralympic athlete’s disability, discussed in the review.
Current recommendations
Sporting performance can be broken down into four key components: athlete, physical capacity, equipment, and the competition environment (Figure 4). In Paralympic sports, although an athlete’s physical capacity, body composition, and overall health can be improved through training, the athlete’s impairment is likely to play a major role in the extent of this improvement. Hence, specific guidance for impairment groups, where appropriate, needs to be considered when utilizing strategies to aid performance in the heat. Another area of focus to improve performance outcomes is the interaction between the athlete and their equipment with the need to optimize configuration and maintenance of the equipment. Figure 4 depicts the key components that result in a performance outcome and strategies that could be utilized and implemented by Paralympic athletes to improve sporting performance at the Tokyo 2020 Paralympic Games. In addition to the strategies highlighted in Figure 4, at an organizational level specific heat policies should be introduced to ensure athlete safety enforced by sports governing bodies. With the growing number of competitions, including Paralympic Games, being hosted by countries that experience hot and humid conditions, regulations and a change in heat-health policy need to be considered for a number of Paralympic sports.
Figure 4.
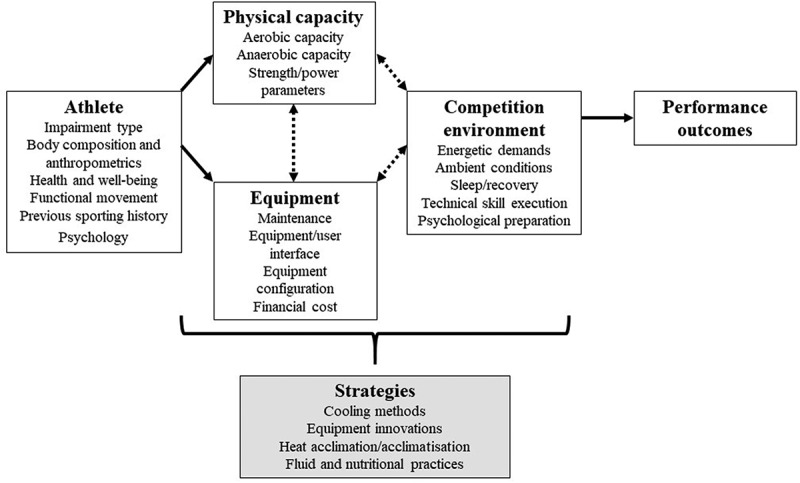
Four key components of sporting performance in Paralympic sport; athlete, physical capacity, equipment, and the competition environment. To implement strategies that improve in-competition performance one must consider the physiological consequences of an athlete’s impairment on their physical capacity and the interface between the athlete and equipment. Strategies/interventions that could be utilized and implemented by Paralympic athletes to improve sporting performance at the Tokyo 2020 Paralympic Games are highlighted in the grey-shaded box. This figure is adapted from [14].
To combat the increase in heat strain for heat-vulnerable Paralympic athletes strategies such as the implementation of cooling methods and heat acclimation can be utilized. There is presently no record of the number of Paralympic athletes, or athletes with a disability competing at international competitions, utilizing specific interventions to prepare themselves for the heat, while some insight of these numbers are available for the AB population. For example, at the International Association of Athletics Federations (IAAF) World Championships held in 2015 in Beijing despite the expected hot/humid conditions, out of the 307 athletes surveyed only 15% heat acclimatized prior to the Championships, 52% had a pre-cooling strategy and 96% had a fluid consumption strategy [69]. These values are perhaps even more surprising given that 48% of the athletes had previously experienced exertional heat illness symptoms. Despite less than 2% of the athletes experiencing exertional heat illness symptoms during the Championships, the authors did suggest that a greater awareness of adequate preparation for competing in the heat should be disseminated to optimize athlete health and sporting performance. A greater understanding of whether a similar situation is present in Paralympic and IPC competitions is clearly warranted, especially when some athletes are potentially likely to experience a greater amount of thermal strain than AB athletes.
Cooling strategies and fluid practices
Despite the considerable interest in the application of cooling strategies for the AB athlete, comparatively little is known concerning the Paralympic athlete. The majority of cooling methods used in the AB athletic population are either applied to the skin (i.e. ice vest [70,71], water immersion [72,73], iced towels/packs [74,75], via an ingested cooling medium (i.e. ice slurry [76–78], cold water ingestion [79,80]) or a combination of methods [81–84]. Cooling is applied either before, during (including rest periods),and/or post exercise and is largely determined by sporting demands, sporting regulations, logistics, environmental conditions, temperature of the coolant, anatomical location, and surface area of cooling. Pre-cooling aims to reduce core temperature and improve heat storage capacity, cooling provided during exercise intends to attenuate the rise in core temperature, while cooling provided post exercise aims to accelerate recovery. Previous research in the AB literature has shown cooling provided both before and during exercise is effective at improving sporting performance in both moderate and hot ambient conditions [85], while meta-analysis data shows the use of mixed method pre-cooling to have a substantial positive influence on performance [86]. Additionally, reducing an individual’s thermal sensation by utilizing specific cooling strategies (i.e. menthol), without a decrease in core temperature, has also been shown to improve sporting performance [87,88].
In Paralympic sport, although small in number, the majority of studies on cooling strategies has been for athletes with an SCI using water sprays [89,90], cooling garments [90–97], extremity cooling [98,99], cold water immersion [100], ice slurries [100] and mixed method cooling [100]. A previous review of the literature [101] stated that wearing an ice vest during intermittent exercise reduced thermal strain and enhanced performance for athletes with an SCI, while a combination of pre-cooling and cooling during exercise is likely to increase the effectiveness of the strategy. However, due to the paucity of research, it is difficult to determine the optimal cooling strategy for this population group, and future studies should ensure strategies are studied under constraints of the actual competition and that outcomes can be transformed into meaningful practice. The fit of future cooling garments is also important, especially for wheelchair athletes. Commercially available garments are made for AB individuals and not for seated use or with abdominal binding both of which affect the contact with the skin. Wheelchair athletes, in particular wheelchair rugby players with tetraplegia, commonly use water sprays to cool themselves during breaks in play. To investigate the effectiveness of this strategy Griggs et al. [90] examined elite wheelchair rugby players with tetraplegia undertaking a simulated wheelchair rugby match with either no cooling, cooling using water sprays during rest periods or a combination of pre-cooling using an ice vest and water sprays during rest periods. Both cooling trials attenuated the increase in core temperature during the simulated match, with the effect greatest in the combined cooling trial, while the combination trial also lowered mean skin temperature. Hence, the combined cooling trial lowered thermal strain to a greater degree, though there was no improvement in performance. In the ambient conditions expected in Tokyo 2020, the addition of a fan directed onto the athlete is likely to lower thermal strain further by increasing both convective and evaporative heat loss. It should also be noted that due to the reduction in afferent sensation, athletes with an SCI are unable to perceive their thermal state, therefore relying on thermal perceptions to determine thermal strain is not appropriate.
Where possible, similar to AB athletes, Paralympic athletes should determine their sweat rate when competing in the heat to enable an individualized fluid strategy to be put in place to replace fluid losses. Fluid practices must be practiced prior to competition, in particular when combined with external cooling strategies, as athletes may reduce ab libitum fluid intake [95] if they perceive themselves to be cooler. The ingestion of fluid can also act as a cooling strategy with the ingestion of cold water or ice slurries becoming popular in recent years in the athletic AB population. However, a recent study has shown that the use of ice slurries during exercise may actually hinder net heat loss via a larger reduction in the whole body sweating compared to the amount of internal heat lost to the ingested ice slurry [102].
Yet in athletes with an SCI, evaporative heat loss is already reduced because of their impairment; thus, the effect of ice slurries as a pre-cooling or during exercise tool requires more investigation. The volume of ice ingested would need to be carefully considered for this population group as large volumes of fluid ingestion, leading to frequent voiding, can cause gastrointestinal discomfort, be logistically difficult for athletes using catheters and could increase the risk of autonomic dysreflexia [31]. Therefore, further investigation into whether this internal method would be beneficial and practical for athletes with an SCI is greatly needed.
Cooling studies have also been undertaken in individuals with heat sensitive MS, albeit not in athletes. Studies have typically provided cooling through the use of cooling garments [103–105], lower limb water immersion [106], extremity cooling [107] and cold water ingestion [108]. Regardless of the cooling strategy chosen, cooling typically reduced core temperature and improved functional capacity and physical performance. Nevertheless, Chaseling et al. [108] observed no differences in core or skin temperature when patients with MS cycled until volitional exhaustion in 30°C and 30% RH while ingesting cold water (1.5°C) or neutral temperature water (37°C). Despite this, time to exhaustion was increased when ingesting cold water, suggesting that this simple cooling strategy could enhance exercise tolerance for this population group, yet the effect this cooling method has on MS symptoms is not known. It is also important to note that during heat stress, individuals with MS have reported a reduced skin thermosensitivity to cold [109]. Thus, similar to individuals with an SCI, the perceptual benefit of a cooling aid could be hindered, i.e. individuals may be unable to perceive the “true coldness” of the aid, and this must be accounted for when developing cooling strategies for athletes with MS and an SCI [109].
Choosing the correct cooling strategy for an individual or team of athletes will largely depend on the needs and impairment of the athlete and the sport itself, such as environmental conditions, access to freezers or baths, logistics, cost and unclothed body surface area to cool for external cooling. Cooling provided before competition should be provided as close to the start as possible and avoid cooling active body parts. For example, cooling the hands before competition for wheelchair athletes or cooling the lower limbs of a runner would be inappropriate. Thus, fully understanding the sporting demands, the competition environment, the athlete and their equipment (see Figure 4) will enable coaches and practitioners to target appropriate cooling strategies.
Heat acclimation
Heat acclimation (HA) has been extensively researched in the AB population due to its application in military, occupational and athletic settings and has been described as the most important intervention one can adopt to reduce physiological strain, optimize performance in the heat and improve heat tolerance [110]. Commonly reported adaptations include: lower core and skin temperature; submaximal heart rate; carbohydrate metabolism; sweat electrolyte content; perceived exertion and thermal strain; and increased sweat rate and plasma volume expansion with a resultant improved performance in the heat [8,111–113].
To induce the aforementioned adaptations, HA typically consists of 5–16 days of daily or alternate days heat exposure, with individual exposures of 1–2 h in temperatures equal to or greater than 35.0°C [114]. A significant proportion of HA adaptations occurs within the first week of chronic heat exposure [115] though longer durations enable full adaptation of several parameters such as sweat rate and sudomotor threshold [116]. These parameters are particularly meaningful for the preparation of athletes competing in endurance events [114,116,117]. Regardless of long or short duration HA, heat exposures must be of sufficient thermal strain to increase core temperature, skin temperature and sweat rate above a set threshold, which appear to be the main drivers for adaptation in AB athletes [116,118,119].
Commonly, HA protocols have consisted of exercise at a fixed external workload over the acclimation period [111,120–124]. However, it has been speculated that this approach results in diminishing adaptations during the intervention as the relative thermal strain imposed gradually lessens [116,125]. Consequently, isothermic approaches have been employed, which maintain a set thermal strain, commonly a core temperature of ~38.5°C over the acclimation period, while the external workload gradually increases concurrently to thermoregulatory adaptation to invoke continued adaptations.
However, the application of isothermic HA for athletes, especially pre-competition, has been questioned [126–128], due to the impact excessive exercising heat stress may have on athletes’ fatigue and hence the “quality” of training [118]. Therefore, the efficacy of passive HA has been studied, such as the use of hot water immersion [126–128] and sauna exposure [129,130]. These methods have been employed immediately after exercise in temperate environments, thus invoking HA while allowing athletes the opportunity to train without impacting planned exercise intensity. Furthermore, exercise prior to passive heat exposure results in elevated core temperature, skin temperature and sweat rate before the commencement of passive HA, thus reducing the required heat exposure duration. Passive HA has been shown to induce positive physiological adaptations [127–130] with some evidence of improved endurance performance [128,129]. Nonetheless, it is unclear whether the adaptations from the sole use of passive HA are similar to that of active HA.
The effectiveness of HA has been comprehensively studied in AB athletes [111,113,121,123,125,126,128,130]; however, to date, only the study of Castle et al. [131] has investigated its use for Paralympic athletes. A small group of target shooters with tetraplegia (n = 2) or paraplegia (n = 3) undertook a 7-day consecutive HA intervention consisting of 20-min moderate intensity, isothermic arm crank ergometry, and 40-min rest in 33.4°C and 64.8% RH. HA resulted in a decrease in resting and exercising aural temperature, a decrease in the rating of perceived effort (RPE) and thermal sensation and a small increase in plasma volume. This was the first evidence of beneficial adaptations in Paralympic athletes [131]. Nonetheless, due to the lack of change in exercising heart rate or whole body sweat rate, as a consequence of athletes’ impairments, the responses were deemed only partial acclimation. More recently, Trbovich et al. [132] found no beneficial adaptations in a larger group of individuals with an SCI (tetraplegia and paraplegia) undergoing the same protocol of Castle et al. [131], albeit in recreationally active individuals. Similarly, Gass and Gass [133] utilized a 5-day passive HA protocol and demonstrated no change in thermoregulatory parameters in individuals with paraplegia, yet improvements were evident in an AB group. Thus, the study of Castle et al. [131] provides the only evidence that Paralympic athletes are capable of displaying partial HA, although this is the only work to date in highly trained athletes with a physical impairment.
Heat regulations and policy
The most commonly used index of environmental heat stress in sports settings is the wet bulb globe temperature (WBGT). This empirical index is largely recommended by international sport organizations and federations, such as the International Olympic Committee and International Tennis Federation [134,135], and general guidance has been stipulated by the American College of Sports Medicine (ACSM) regarding safe exercising WBGT ranges [136]. Recent evidence has shown that based on historical geographical data, the ambient conditions of the Tokyo 2020 Olympic Games will be held amid extremely high WBGT levels [4], initiating considerations to be made regarding venues and scheduling of events.
Various sporting governing bodies use WBGT ranges and limits to implement additional breaks and suspension of play. While WBGT has undoubtedly greatly mitigated the risk of hyperthermia in numerous environments, similar to all direct indices, WBGT has its limitations and has faced some criticism for its use in sport due to its frequent underestimation of heat stress [137]. Despite the index not taking into account metabolic heat production and variability in clothing, and thus cannot predict heat dissipation, the index can be used as a rough screening index [138,139], especially with the addition of correction factors to account for specific clothing garments.
Regardless of any criticism of WBGT, having a form of heat stress index is better than having none at all. To the authors’ knowledge, wheelchair tennis is the only Paralympic sport to have its own heat health policy, which is based on WBGT [27,28]. Even though many impairment groups are at a potential-heightened risk of heat-related issues compared to AB athletes, specific policies have not been implemented to reflect this. Such safeguarding of Paralympic athletes at an increased risk of thermal strain during competition requires urgent attention.
Of note, a recent retrospective audit of illness surveillance reports [140] from the 2015 Para athletic World Championships observed that there was, in fact, a low rate of heat-related illnesses despite WBGT levels regularly exceeding the ACSM and IAAF guidelines for cancelation of events. The authors of the audit suggested that the countermeasures put in place by the IAAF andthe preparation of the athletes for this particular event were sufficient to prevent a high incidence of heat-related illnesses. Countermeasures included scheduling of events to be held at night, increased shade covering, increased provision of ice and cold fluids, increased additional schedule breaks and increased surveillance and education by team medical staff. However, it should be noted that athletes who reported to their own team physicians were not included in the survey and whether a similar outcome would be apparent across Paralympic sports with various countermeasures in place remains to be seen.
Future technological advancements
Technology plays an important role in improving sport performance in Paralympic sport, for instance, the development of sport-specific and individualized wheelchairs [141] and prosthetics [142]. An understanding of the requirements of the athlete to effectively match the technology of the equipment, plus the interface of the athlete and equipment (Figure 4), is key for advancements in sporting performance in Paralympic sport [2]. An ongoing challenge is to decide whether the improvements in equipment signify “performance enhancement” or are “essential for performance.”
An increasing number of portable and non-invasive wearable technology (devices and clothing) have been developed predominately to monitor and predict real-time work-related heat strain [143]. A number of these wearables could be implemented within sport settings to help prepare athletes, enabling a greater understanding of how the athlete will cope when competing in the heat. However, it must be noted that the majority of the devices do still require validation in sport-specific environments. Examples of wearables currently available are the Astroskin vest (Carre Technologies Inc., Montreal, Quebec., Canada), the Questemp II ear sensor (3M, St. Paul, Minnesota., USA) and the BioNomadix hip worn logger (BIOPAC Systems Inc., Goleta, California., USA). For a review of wearable technologies for monitoring heat strain, the reader is directed to [143]. The use of wearable technology could increase the understanding of how a Paralympic athlete with a particular impairment responds to training and simulated races/match play in various environmental conditions. This greater understanding of the physiological responses of the athlete would enable coaches and support staff to individualize strategies to combat an increase in heat strain.
Of utmost importance when using a wearable physiological monitor worn as a clothing garment is whether the benefit of wearing the monitor is offset by any potential increase in heat strain and hence decrease in evaporative heat loss by wearing an additional clothing layer [144]. While these devices could be used during training, due to regulations of individual sports and difficulty incorporating such garments into athletic clothing they are unlikely to be used in the imminent future in actual competition. Practically, intra-individual factors (i.e. hydration status) need to be considered for any user, but additionally for Paralympic athletes, further personalization and adaptation of algorithms used by the wearable may be required to account for physiological, biomechanical, and anatomical differences to AB individuals. For example, to ensure validity, an algorithm used in a wearable may need to take into account a lack of sympathetic innervation to the heart for athletes with tetraplegia or the change in gait for athletes with a leg amputation. While consideration must also be given to the financial cost of such garments and whether monitoring various physiological markers during training is of greater benefit to the athlete than readily available traditional methods.
Practical recommendations
This review has presented an overview of heat-related issues for Paralympic athletes, plus current recommendations and future technological advancements to reduce thermal strain. To aid support staff and practitioners working with Paralympic athletes competing in Tokyo 2020, Table 2 provides a list of practical recommendations to ensure that athletes’ health and sporting performance are not negatively affected by the potential environmental challenges.
Table 2.
Practical recommendations for Paralympic athletes competing at Tokyo 2020 to reduce thermal strain.
| Type of recommendation | Advice |
|---|---|
| Education |
|
| Health and fitness |
|
| Environment |
|
| Cooling strategies/fluid and nutritional practices/acclimation |
|
| Technology |
|
| Policy |
|
Conclusions
The Tokyo 2020 Paralympic Games may present an environmental challenge for many Paralympic athletes due to the expected high heat and humidity. The combination of the complexity of an athlete’s impairment and the make-up of the sport in which they compete will largely contribute to an athlete’s predisposition to heightened thermal strain during the competition in the heat. Despite the paucity of thermoregulatory research in Paralympic athletes and limited sharing of knowledge, to combat the increase in heat strain, the implementation of cooling methods and heat acclimation should be recommended alongside the introduction of specific heat policies for sports. Finally, practical recommendations should be employed to ensure that Paralympic athletes’ health and sporting performance are not negatively affected during the competition in the heat at the Tokyo 2020 Paralympics.
Biographies
Katy Griggs is a Lecturer in Sport Engineering at Nottingham Trent University. She previously worked as a researcher and undertook her PhD at the Peter Harrison Centre for Disability Sport (School of Sport and Exercise and Health Sciences, Loughborough University) and the Environmental Ergonomics Research Centre (Design School, Loughborough University). Her research focuses on exercise and environmental physiology, Paralympic sport and human performance.

Ben Stephenson is a physiologist at the English Institute of Sport and postdoctoral research assistant at School of Sport, Exercise and Health Sciences (Peter Harrison Centre for Disability Sport), Loughborough University. His research has focussed on thermoregulation and heat adaptation in Paralympic athletes.

Dr Mike Price is a Reader in Exercise Physiology at Coventry University. He has published over 80 peer reviewed journal articles and book chapters across a number of sport and exercise science subject areas including thermoregulation in upper body exercise in both able-bodied and individuals with a spinal cord injury. He has also published in the applied physiology of fencing, equestrian athletes and wheelchair athletes, being involved in specific Paralympic projects prior to the Atlanta (1996), Athens (2004) and Rio (2016) Games.

Professor Vicky Tolfrey is the Director of the Peter Harrison Centre for Disability Sport which is based within the School of Sport and Exercise and Health Sciences at Loughborough University. Vicky is an accredited British Association of Sport and Exercise Sciences (BASES) physiologist and has provided applied sport science support to Paralympic athletes since 1994, she has attended numerous Paralympic Games as a sports science practitioner.

Acknowledgments
The authors would like to thank Dr Steve Faulkner for proofreading the manuscript.
Disclosure statement
No potential conflict of interest was reported by the authors.
Abbreviations
- AB
able-bodied
- ACSM
American College of Sports Medicine
- CP
cerebral palsy
- IAAF
International Association of Athletics Federations
- IPC
International Paralympic Committee
- HA
heat acclimation
- MS
multiple sclerosis
- RH
relative humidity
- SCI
spinal cord injury
- WBGT
wet bulb globe temperature
References
- [1].International Paralympic Committee . Rio 2016 [Online]. [cited 2019 Jan 7]. Available from: https://www.paralympic.org/rio-2016
- [2].Burkett B. Technology in Paralympic sport: performance enhancement or essential for performance? Br J Sports Med. 2010;44(3):215–220. [DOI] [PubMed] [Google Scholar]
- [3].Webborn N, Van de Vliet P. Paralympic medicine. Lancet. 2012. 7;380(9836):65–71. [DOI] [PubMed] [Google Scholar]
- [4].Kakamu T, Wada K, Smith DR, et al. Preventing heat illness in the anticipated hot climate of the Tokyo 2020 summer olympic games. Environ Health Prev Med. 2017;22(1):68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Gerrett N, Kingma BRM, Sluijter R, et al. Ambient conditions prior to Tokyo 2020 olympic and paralympic games: considerations for acclimation or acclimatization strategies. Front Physiol. 2019;10:414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Ely BR, Ely MR, Cheuvront SN, et al. Evidence against a 40 degrees C core temperature threshold for fatigue in humans. J Appl Physiol. 2009;107(5):1519–1525. [DOI] [PubMed] [Google Scholar]
- [7].Galloway SD, Maughan RJ. Effects of ambient temperature on the capacity to perform prolonged cycle exercise in man. Med Sci Sports Exerc. 1997;29(9):1240–1249. [DOI] [PubMed] [Google Scholar]
- [8].Périard JD, Racinais S, Sawka MN. Adaptations and mechanisms of human heat acclimation: applications for competitive athletes and sports. Scand J Med Sci Sports. 2015;25:20–38. [DOI] [PubMed] [Google Scholar]
- [9].Cheung SS, Sleivert GG. Multiple triggers for hyperthermic fatigue and exhaustion. Exerc Sport Sci Rev. 2004;32(3):100–106. [DOI] [PubMed] [Google Scholar]
- [10].International Paralympic Committee . Tokyo 2020 [Online]. [cited 2018 Dec 6]. Available from: https://www.paralympic.org/tokyo-2020
- [11].International Paralympic Committee . International paralympic committee athlete classification code. Bonn (Germany): International Paralympic Committee; 2015. [Google Scholar]
- [12].Rhodes JM, Mason BS, Perrat B, et al. Activity profiles of elite wheelchair rugby players during competition. Int J Sports Physiol Perform. 2015;10(3):318–324. [DOI] [PubMed] [Google Scholar]
- [13].West CR, Gee CM, Voss C, et al. Cardiovascular control, autonomic function, and elite endurance performance in spinal cord injury. Scand J Med Sci Sports. 2015;25(4):476–485. [DOI] [PubMed] [Google Scholar]
- [14].Paulson T, Goosey-Tolfrey V. Current perspectives on profiling and enhancing wheelchair court sport performance. Int J Sports Physiol Perform. 2017;12(3):275–286. [DOI] [PubMed] [Google Scholar]
- [15].Kirshblum SC, Burns SP, Biering-Sorensen F, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34(6):535–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].American Spinal Injury Association . International standards for neurological classification of spinal cord injury, revised 2002. Chicago: American Spinal Injury Association; 2002. [Google Scholar]
- [17].Freund PR, Brengelmann GL, Rowell LB, et al. Attenuated skin blood flow response to hyperthermia in paraplegic men. J Appl Physiol. 1984;56(4):1104–1109. [DOI] [PubMed] [Google Scholar]
- [18].Rawson RO, Hardy JD. Sweat inhibition by cutaneous cooling in normal sympathectomized and paraplegic man. J Appl Physiol. 1967;22(2):287–291. [DOI] [PubMed] [Google Scholar]
- [19].Tam HS, Darling RC, Cheh HY, Downey JA . Sweating response: a means of evaluating the set-point theory during exercise. J Appl Physiol. 1978;45(3):451–458. [DOI] [PubMed] [Google Scholar]
- [20].Hopman MT. Circulatory responses during arm exercise in individuals with paraplegia. Int J Sports Med. 1994;15(3):126–131. [DOI] [PubMed] [Google Scholar]
- [21].Normell LA. Distribution of impaired cutaneous vasomotor and sudomotor function in paraplegic man. Scand J Clin Lab Invest. 1974;138:25–41. [PubMed] [Google Scholar]
- [22].Guttmann L, Silver J, Wyndham CH. Thermoregulation in spinal man. J Physiol. 1958;142(3):406–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Hopman MT, Oeseburg B, Binkhorst RA. Cardiovascular responses in paraplegic subjects during arm exercise. Eur J Appl Physiol Occup Physiol. 1992;65(1):73–78. [DOI] [PubMed] [Google Scholar]
- [24].Attia M, Engel P. Thermoregulatory set point in patients with spinal cord injuries (spinal man). Paraplegia. 1983;21(4):233–248. [DOI] [PubMed] [Google Scholar]
- [25].Hopman MT, Oeseburg B, Binkhorst RA. Cardiovascular responses in persons with paraplegia to prolonged arm exercise and thermal stress. Med Sci Sports Exerc. 1993;25(5):577–583. [PubMed] [Google Scholar]
- [26].Price MJ, Campbell IG. Effects of spinal cord lesion level upon thermoregulation during exercise in the heat. Med Sci Sports Exerc. 2003;35(7):1100–1107. [DOI] [PubMed] [Google Scholar]
- [27].Federation IT . International tennis federation, regulations for wheelchair tennis 2013. Bank Lane, Roehampton, London: ITF Ltd; 2013. [Google Scholar]
- [28].Girard O. Thermoregulation in wheelchair tennis-How to manage heat stress? Front Physiol. 2015;2(6):175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Griggs KE, Havenith G, Price MJ, et al. Thermoregulatory responses during competitive wheelchair rugby match play. Int J Sports Med. 2017;38(3):177–183. [DOI] [PubMed] [Google Scholar]
- [30].Griggs KE, Leicht CA, Price MJ, et al. Thermoregulation during intermittent exercise in athletes with a spinal-cord injury. Int J Sports Physiol Perform. 2015;10(4):469–475. [DOI] [PubMed] [Google Scholar]
- [31].Goosey-Tolfrey VL, Paulson T, Graham-Paulson T. Practical considerations for fluid replacement for athletes with a spinal cord injury. In: Meyer F, Szygula Z, Boca Raton WB, editors. Fluid balance, hydration, and athletic performance. FL: CRC Press; 2015. p. 331–355. [Google Scholar]
- [32].Blackmer J. Rehabilitation medicine: 1. Autonomic dysreflexia. Cmaj. 2003;69(9):931–935. [PMC free article] [PubMed] [Google Scholar]
- [33].Runciman P, Tucker R, Ferreira S, et al. Paralympic athletes with cerebral palsy display altered pacing strategies in distance-deceived shuttle running trials. Scand J Med Sci Sports. 2016;26(10):1239–1248. [DOI] [PubMed] [Google Scholar]
- [34].Bax MC. Terminology and classification of cerebral palsy. Dev Med Child Neurol. 1964;6:295–297. [DOI] [PubMed] [Google Scholar]
- [35].Blauwet CA, Brook EM, Tenforde AS, et al. Low energy availability, menstrual dysfunction, and low bone mineral density in individuals with a disability: implications for the para athlete population. Sport Med. 2017;47(9):1697–1708. [DOI] [PubMed] [Google Scholar]
- [36].Maltais D, Wilk B, Unnithan V, et al. Responses of children with cerebral palsy to treadmill walking exercise in the heat. Med Sci Sports Exerc. 2004;36(10):1674–1681. [DOI] [PubMed] [Google Scholar]
- [37].Kloyiam S, Breen S, Jakeman P, et al. Soccer-specific endurance and running economy in soccer players with cerebral palsy. Adapt Phys Act Q. 2011;28(4):354–367. [DOI] [PubMed] [Google Scholar]
- [38].Elkamil AI, Andersen GL, Skranes J, et al. Botulinum neurotoxin treatment in children with cerebral palsy: a population-based study in Norway. Eur J Paediatr Neurol. 2012;16(5):522–527. [DOI] [PubMed] [Google Scholar]
- [39].Heckmann M, Ceballos-Baumann AO, Plewig G. Botulinum toxin a for axillary hyperhidrosis (excessive sweating). N Engl J Med. 2001;344:488–493. [DOI] [PubMed] [Google Scholar]
- [40].Tucker R, Marle T, Lambert EV, et al. The rate of heat storage mediates an anticipatory reduction in exercise intensity during cycling at a fixed rating of perceived exertion. J Physiol. 2006;574(3):905–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Flouris AD, Schlader ZJ. Human behavioral thermoregulation during exercise in the heat. Scand J Med Sci Sports. 2015;25(Suppl 1):52–64. [DOI] [PubMed] [Google Scholar]
- [42].Schmit C, Duffield R, Hausswirth C, et al. Pacing adjustments associated with familiarization: heat versus temperate environments. Int J Sports Physiol Perform. 2016;11(7):855–860. [DOI] [PubMed] [Google Scholar]
- [43].Crandall CG, Davis SL. Cutaneous vascular and sudomotor responses in human skin grafts. J Appl Physiol. 2010;109(5):1524–1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Ghoseiri K, Safari MR. Prevalence of heat and perspiration discomfort inside prostheses: literature review. J Rehabil Res Dev. 2014;51(6):855–868. [DOI] [PubMed] [Google Scholar]
- [45].Schmalz T, Blumentritt S, Jarasch R. Energy expenditure and biomechanical characteristics of lower limb amputee gait: the influence of prosthetic alignment and different prosthetic components. Gait Posture. 2002;34(1):31–36. [DOI] [PubMed] [Google Scholar]
- [46].Waters RL, Mulroy S. The energy expenditure of normal and pathologic gait. Gait Posture. 1999;9(3):207–231. [DOI] [PubMed] [Google Scholar]
- [47].Huang CT, Jackson JR, Moore NR, et al. Amputuation: energy cost of ambulation. Arch Phys Med Rehabil. 1979;60:18–24. [PubMed] [Google Scholar]
- [48].Ganguli S, Datta SR, Chatterjee B, et al. Performance evaluation of an amputee prosthesis system in below knee amputees. Ergonomics. 1973;16(6):797–810. [DOI] [PubMed] [Google Scholar]
- [49].Ganguli S, Bose KS, Datta SR, et al. Ergonomics evaluation of above-knee amputee-prosthesis combinations. Ergonomics. 1974;17(2):199–210. [DOI] [PubMed] [Google Scholar]
- [50].Gailey RS, Nash MS, Atchley TA, et al. The effects of prosthesis mass on metabolic cost of ambulation in non-vascular trans-tibia1 amputees. Prosthet Orthot Int. 1997;21:9–16. [DOI] [PubMed] [Google Scholar]
- [51].Pye G, Bowker P. Skin temperature as an indicator of stress in soft tissue. Eng Med. 1976;5:58–60. [DOI] [PubMed] [Google Scholar]
- [52].Klute GK, Glaister BC, Berge JS. Prosthetic liners for lower limb amputees: a review of the literature. Prosthet Orthot Int. 2010;34(2):146–153. [DOI] [PubMed] [Google Scholar]
- [53].Klute GK, Kantor C, Darrouzet C, et al. Lower-limb amputee needs assessment using multistakeholder focus-group approach. J Rehabil Res Dev. 2009;46(3):293–304. [PubMed] [Google Scholar]
- [54].Williams RJ, Washington ED, Miodownik M, et al. The effect of liner design and materials selection on prosthesis interface heat dissipation. Prosthet Orthot Int. 2018;42(3):275–279. [DOI] [PubMed] [Google Scholar]
- [55].Bothwell JE. Pigmented skin lesions in tyrosinase-positive oculocutaneous albinos: a study in black South Africans. Int J Dermatol. 1997;36(11):831–836. [DOI] [PubMed] [Google Scholar]
- [56].Pandolf KB, Gange RW, Latzka WA, et al. Human thermoregulatory responses during cold water immersion after artificially induced sunburn. Am J Physiol Integr Comp Physiol. 1992;262:R617–R623. [DOI] [PubMed] [Google Scholar]
- [57].Aburto-Corona J, Aragón-Vargas L. Sunscreen use and sweat production in men and women. J Athl Train. 2016;51:696–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Ou-Yang H, Meyer K, Houser T, et al. Sunscreen formulations do not interfere with sweat cooling during exercise. Int J Cosmet Sci. 2018;40(1):87–92. [DOI] [PubMed] [Google Scholar]
- [59].House JR, Breed M. Sunscreen use reduces sweat evaporation but not production. In: 15th International Conference on Environmental Ergonomics. Queenstown (New Zealand); 2013. p. 117. [Google Scholar]
- [60].Huang M, Jay O, Davis SL. Autonomic dysfunction in multiple sclerosis: implications for exercise. Auton Neurosci Basic Clin. 2015;188:82–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Davis SL, Jay O, Wilson TE. Chapter 42 - Thermoregulatory dysfunction in multiple sclerosis. In: Romanovsky AA, editor. Thermoregulation: from basic neuroscience to clinical neurology, part II. Elsevier; 2018. p. 701–714. [DOI] [PubMed] [Google Scholar]
- [62].Rasminsky M. The effects of temperature on conduction in demyelinated single nerve fibers. Arch Neurol. 1973;28(5):287–292. [DOI] [PubMed] [Google Scholar]
- [63].Schauf CL, Davis FA. Impulse conduction in multiple sclerosis: a theoretical basis for modification by temperature and pharmacological agents. J Neurol Neurosurg Psychiatry. 1974;37(2):152–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Nelson DA, McDowell F. The effects of induced hyperthermia on patients with multiple sclerosis. J Neurol Neurosurg Psychiatry. 1959;22:113–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Nelson D, Jeffreys W, McDowell F. Effects of induced hyperthermia on some neurological diseases. AMA Arch Neurol Psychiatry. 1958;79:31–39. [DOI] [PubMed] [Google Scholar]
- [66].Duckworth WC, Solomon SS, Jallepalli P, et al. Glucose intolerance due to insulin resistance in patients with spinal cord injuries. Diabetes. 1980;29:906–910. [DOI] [PubMed] [Google Scholar]
- [67].Christogianni A, Bibb R, Davis SL, et al. Temperature sensitivity in multiple sclerosis: an overview of its impact on sensory and cognitive symptoms. Temperature. 2018;5(3):208–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Allen DR, Huang M, Parupia IM, et al. Impaired sweating responses to a passive whole body heat stress in individuals with multiple sclerosis. J Neurophysiol. 2017;118:7–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Périard JD, Racinais S, Timpka T, et al. Strategies and factors associated with preparing for competing in the heat: A cohort study at the 2015 IAAF world athletics championships. Br J Sports Med. 2017;51(4):264–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Faulkner SH, Hupperets M, Hodder SG, et al. Conductive and evaporative precooling lowers mean skin temperature and improves time trial performance in the heat. Scand J Med Sci Sports. 2015;25:183–189. [DOI] [PubMed] [Google Scholar]
- [71].Arngrimsson SA, Petitt DS, Stueck MG, et al. Cooling vest worn during active warm-up improves 5-km run performance in the heat. J Appl Physiol. 2004;96(5):1867–1874. [DOI] [PubMed] [Google Scholar]
- [72].Skein M, Duffield R, Cannon J, et al. Self-paced intermittent-sprint performance and pacing strategies following respective pre-cooling and heating. Eur J Appl Physiol. 2012;112(1):253–266. [DOI] [PubMed] [Google Scholar]
- [73].Duffield R, Green R, Castle P, et al. Precooling can prevent the reduction of self-paced exercise intensity in the heat. Med Sci Sports Exerc. 2010;42(3):577–584. [DOI] [PubMed] [Google Scholar]
- [74].Castle PC, Macdonald AL, Philp A, et al. Precooling leg muscle improves intermittent sprint exercise performance in hot, humid conditions. J Appl Physiol. 2006;100(4):1377–1384. [DOI] [PubMed] [Google Scholar]
- [75].Minett GM, Duffield R, Marino FE, et al. Volume-dependent response of precooling for intermittent-sprint exercise in the heat. Med Sci Sports Exerc. 2011;43(9):1760–1769. [DOI] [PubMed] [Google Scholar]
- [76].Ross ML, Garvican LA, Jeacocke NA, et al. Novel precooling strategy enhances time trial cycling in the heat. Med Sci Sports Exerc. 2011;43(1):123–133. [DOI] [PubMed] [Google Scholar]
- [77].Siegel R, Mate J, Brearley MB, et al. Ice slurry ingestion increases core temperature capacity and running time in the heat. Med Sci Sports Exerc. 2010;42(4):717–725. [DOI] [PubMed] [Google Scholar]
- [78].Siegel R, Mate J, Watson G, et al. Pre-cooling with ice slurry ingestion leads to similar run times to exhaustion in the heat as cold water immersion. J Sports Sci. 2012;30(2):155–165. [DOI] [PubMed] [Google Scholar]
- [79].Mündel T, King J, Collacott E, Jones DA . Drink temperature influences fluid intake and endurance capacity in men during exercise in a hot, dry environment. Exp Physiol. 2006;91(5):925–933. [DOI] [PubMed] [Google Scholar]
- [80].Riera F, Trong TT, Sinnapah S, et al. Physical and perceptual cooling with beverages to increase cycle performance in a tropical climate. PLoS One. 2014;9(8):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Quod MJ, Martin DT, Laursen PB, et al. Practical precooling: effect on cycling time trial performance in warm conditions. J Sports Sci. 2008;26(14):1477–1487. [DOI] [PubMed] [Google Scholar]
- [82].Minett GM, Duffield R, Kellett A, et al. Effects of mixed-method cooling on recovery of medium-fast bowling performance in hot conditions on consecutive days. J Sports Sci. 2012;30(13):1387–1396. [DOI] [PubMed] [Google Scholar]
- [83].Duffield R, Steinbacher G, Fairchild TJ. The use of mixed-method, part-body pre-cooling procedures for team-sport athletes training in the heat. J Strength Cond Res. 2009;23(9):2524–2532. [DOI] [PubMed] [Google Scholar]
- [84].Duffield R, Coutts A, McCall A, et al. Pre-cooling for football training and competition in hot and humid conditions. Eur J Sport Sci. 2013;13(1):58–67. [Google Scholar]
- [85].Bongers CC, Thijssen DH, Veltmeijer MT, et al. Precooling and percooling (cooling during exercise) both improve performance in the heat: a meta-analytical review. Br J Sports Med. 2015;49:377–384. [DOI] [PubMed] [Google Scholar]
- [86].Bongers CCWG, Hopman MTE, Eijsvogels TMH. Cooling interventions for athletes: an overview of effectiveness, physiological mechanisms, and practical considerations. Temperature. 2017;4(1):60–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [87].Stevens CJ, Kittel A, Sculley DV, et al. Running performance in the heat is improved by similar magnitude with pre-exercise cold-water immersion and mid-exercise facial water spray. J Sports Sci. 2016;8:1–8. [DOI] [PubMed] [Google Scholar]
- [88].Stevens CJ, Thoseby B, Sculley DV, et al. Running performance and thermal sensation in the heat are improved with menthol mouth rinse but not ice slurry ingestion. Scand J Med Sci Sports. 2016;26:1209–1216. [DOI] [PubMed] [Google Scholar]
- [89].Pritchett RC, Bishop PA, Yang Z, et al. Evaluation of artificial sweat in athletes with spinal cord injuries. Eur J Appl Physiol. 2010;109(1):125–131. [DOI] [PubMed] [Google Scholar]
- [90].Griggs KE, Havenith G, Paulson TAW, et al. Effects of cooling before and during simulated match play on thermoregulatory responses of athletes with tetraplegia. J Sci Med Sport. 2016;20(9):819–824. [DOI] [PubMed] [Google Scholar]
- [91].Armstrong LE, Maresh CM, Riebe D, et al. Local cooling in wheelchair athletes during exercise-heat stress. Med Sci Sports Exerc. 1995;27(2):211–216. [PubMed] [Google Scholar]
- [92].Webborn N, Price MJ, Castle PC, et al. Effects of two cooling strategies on thermoregulatory responses of tetraplegic athletes during repeated intermittent exercise in the heat. J Appl Physiol. 2005;98(6):2101–2107. [DOI] [PubMed] [Google Scholar]
- [93].Webborn N, Price MJ, Castle P, et al. Cooling strategies improve intermittent sprint performance in the heat of athletes with tetraplegia. Br J Sports Med. 2010;44(6):455–460. [DOI] [PubMed] [Google Scholar]
- [94].Trbovich M, Ortega C, Schroeder J, et al. Effect of a cooling vest on core temperature in athletes with and without spinal cord injury. Top Spinal Cord Inj Rehabil. 2014;20:70–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [95].Goosey-Tolfrey VL, Diaper NJ, Crosland J, et al. Fluid intake during wheelchair exercise in the heat: effects of localized cooling garments. Int J Sports Physiol Perform. 2008;3(2):145–156. [DOI] [PubMed] [Google Scholar]
- [96].Bongers CC, Eijsvogels TM, van Nes IJ, et al. Effects of cooling during exercise on thermoregulatory responses of men with paraplegia. Phys Ther. 2016;96(5):650–658. [DOI] [PubMed] [Google Scholar]
- [97].Diaper NJ, Goosey-Tolfrey V. A physiological case study of a paralympic wheelchair tennis player: reflective practise. J Sports Sci Med. 2009;8(2):300–307. [PMC free article] [PubMed] [Google Scholar]
- [98].Hagobian TA, Jacobs KA, Kiratli BJ, et al. Foot cooling reduces exercise-induced hyperthermia in men with spinal cord injury. Med Sci Sports Exerc. 2004;36(3):411–417. [DOI] [PubMed] [Google Scholar]
- [99].Goosey-Tolfrey V, Swainson M, Boyd C, et al. The effectiveness of hand cooling at reducing exercise-induced hyperthermia and improving distance-race performance in wheelchair and able-bodied athletes. J Appl Physiol. 2008;105(1):37–43. [DOI] [PubMed] [Google Scholar]
- [100].Forsyth P, Pumpa K, Knight E, et al. Physiological and perceptual effects of precooling in wheelchair basketball athletes. J Spinal Cord Med. 2016;39(6):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [101].Griggs KE, Price MJ, Goosey-Tolfrey VL. Cooling athletes with a spinal cord injury. Sports Med. 2015;45(1):9–21. [DOI] [PubMed] [Google Scholar]
- [102].Morris NB, Coombs G, Jay O. Ice slurry ingestion leads to a lower net heat loss during exercise in the heat. Med Sci Sports Exerc. 2016;48(1):114–122. [DOI] [PubMed] [Google Scholar]
- [103].Nilsagård Y, Denison E, Gunnarsson LG. Evaluation of a single session with cooling garment for persons with multiple sclerosis-a randomized trial. Disabil Rehabil Assist Technol. 2006;1(4):225–233. [DOI] [PubMed] [Google Scholar]
- [104].Meyer-Heim A, Rothmaier M, Weder M, et al. Advanced lightweight cooling-garment technology: functional improvements in thermosensitive patients with multiple sclerosis. Mult Scler J. 2007;13(2):232–237. [DOI] [PubMed] [Google Scholar]
- [105].Reynolds LF, Short CA, Westwood DA, et al. Head pre-cooling improves symptoms of heat-sensitive multiple sclerosis patients. Can J Neurol Sci. 2011;38(1):106–111. [DOI] [PubMed] [Google Scholar]
- [106].White AT, Wilson TE, Davis SL, et al. Effect of precooling on physical performance in multiple sclerosis. Mult Scler. 2000;6(3):176–180. [DOI] [PubMed] [Google Scholar]
- [107].Grahn DA, Murray J, Craig HC. Cooling via one hand improves physical performance in heat-sensitive individuals with multiple sclerosis: A preliminary study. BMC Neurol. 2008;8:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [108].Chaseling GK, Filingeri D, Barnett M, et al. Cold water ingestion improves exercise tolerance of heat-sensitive people with MS. Med Sci Sports Exerc. 2018;50(4):643–648. [DOI] [PubMed] [Google Scholar]
- [109].Filingeri D, Chaseling G, Hoang P, et al. Afferent thermosensory function in relapsing–remitting multiple sclerosis following exercise-induced increases in body temperature. Exp Physiol. 2017;02:887–893. [DOI] [PubMed] [Google Scholar]
- [110].Racinais S, Alonso JM, Coutts AJ, et al. Consensus recommendations on training and competing in the heat. Scand J Med Sci Sports. 2015;25:6–19. [DOI] [PubMed] [Google Scholar]
- [111].Lorenzo S, Halliwill JR, Sawka MN, et al. Heat acclimation improves exercise performance. J Appl Physiol. 2010;109(4):1140–1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [112].Sawka MN, Wenger CB, Pandolf KB. Thermoregulatory responses to acute exercise‐heat stress and heat acclimation. Compr Physiol Suppl. 2011;14:57–185. [Google Scholar]
- [113].Racinais S, Périard JD, Karlsen A, et al. Effect of heat and heat acclimatization on cycling time trial performance and pacing. Med Sci Sports Exerc. 2014;47(3):601–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [114].Daanen HAM, Racinais S, Périard JD. Heat acclimation decay and re-induction: a systematic review and meta-analysis. Sport Med. 2018;48(2):409–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [115].Garrett AT, Rehrer NJ, Patterson MJ. Induction and decay of short-term heat acclimation in moderately and highly trained athletes. Sport Med. 2011;41(9):757–771. [DOI] [PubMed] [Google Scholar]
- [116].Tyler CJ, Reeve T, Hodges GJ, et al. The effects of heat adaptation on physiology, perception and exercise performance in the heat: a meta-analysis. Sport Med. 2016;46(11):1699–1724. [DOI] [PubMed] [Google Scholar]
- [117].Guy JH, Deakin GB, Edwards AM, et al. Adaptation to hot environmental conditions: an exploration of the performance basis, procedures and future directions to optimise opportunities for elite athletes. Sport Med. 2015;45(3):303–311. [DOI] [PubMed] [Google Scholar]
- [118].Casadio JR, Kilding AE, Siegel R, et al. Periodizing heat acclimation in elite Laser sailors preparing for a world championship event in hot conditions. Temperature. 2016;3(3):437–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [119].Taylor NAS, Tipton MJ, Kenny GP. Considerations for the measurement of core, skin and mean body temperatures. J Therm Biol. 2014;46:72–101. [DOI] [PubMed] [Google Scholar]
- [120].Febbraio MA, Snow RJ, Hargreaves M, et al. Muscle metabolism during exercise and heat stress in trained men: effect of acclimation. J Appl Physiol. 1994;7(7):1804–1806. [DOI] [PubMed] [Google Scholar]
- [121].Houmard JA, Costill DL, Davis JA, et al. The influence of exercise intensity on heat acclimation in trained subjects. Med Sci Sports Exerc. 1990;22(5):615–620. [DOI] [PubMed] [Google Scholar]
- [122].Nielsen B, Strange S, Christensen NJ, et al. Acute and adaptive responses in humans to exercise in a warm, humid environment. Pflugers Arch Eur J Physiol. 1997;434(1):49–56. [DOI] [PubMed] [Google Scholar]
- [123].Schmit C, Duffield R, Hausswirth C, et al. Optimizing heat acclimation for endurance athletes: high- versus low-intensity training. Int J Sports Physiol Perform. 2018;13(6):816–823. [DOI] [PubMed] [Google Scholar]
- [124].Wingfield GL, Gale R, Minett GM, et al. The effect of high versus low intensity heat acclimation on performance and neuromuscular responses. J Therm Biol. 2016;58:50–59. [DOI] [PubMed] [Google Scholar]
- [125].Garrett AT, Creasy R, Rehrer NJ, et al. Effectiveness of short-term heat acclimation for highly trained athletes. Eur J Appl Physiol. 2012;112(5):1827–1837. [DOI] [PubMed] [Google Scholar]
- [126].Ruddock AD, Thompson SW, Hudson SA, et al. Combined active and passive heat exposure induced heat acclimation in a soccer referee before 2014 FIFA World Cup. Springerplus. 2016;5(617):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [127].Zurawlew MJ, Mee JA, Walsh NP. Heat acclimation by post-exercise hot water immersion in the morning reduces thermal strain during morning and afternoon exercise-heat-stress. Int J Sports Physiol Perform. 2018;13(10):1281–1286. [DOI] [PubMed] [Google Scholar]
- [128].Zurawlew MJ, Walsh NP, Fortes MB, et al. Post-exercise hot water immersion induces heat acclimation and improves endurance exercise performance in the heat. Scand J Med Sci Sports. 2016;26(7):745–754. [DOI] [PubMed] [Google Scholar]
- [129].Scoon GSM, Hopkins WG, Mayhew S, et al. Effect of post-exercise sauna bathing on the endurance performance of competitive male runners. J Sci Med Sport. 2007;10(4):259–262. [DOI] [PubMed] [Google Scholar]
- [130].Stanley J, Halliday A, D’Auria S, et al. Effect of sauna-based heat acclimation on plasma volume and heart rate variability. Eur J Appl Physiol. 2015;115(4):785–794. [DOI] [PubMed] [Google Scholar]
- [131].Castle PC, Kularatne BP, Brewer J, et al. Partial heat acclimation of athletes with spinal cord lesion. Eur J Appl Physiol. 2013;113(1):109–115. [DOI] [PubMed] [Google Scholar]
- [132].Trbovich MB, Kiratli JB, Price MJ. The effects of a heat acclimation protocol in persons with spinal cord injury. J Therm Biol. 2016;62:56–62. [DOI] [PubMed] [Google Scholar]
- [133].Gass EM, Gass GC. Thermoregulatory responses to repeated warm water immersion in subjects who are paraplegic. Spinal Cord. 2001;39(3):149–155. [DOI] [PubMed] [Google Scholar]
- [134].Bergeron MF, Bahr R, Bärtsch P, et al. International olympic committee consensus statement on thermoregulatory and altitude challenges for high-level athletes. Br J Sports Med. 2012;46(11):770–779. [DOI] [PubMed] [Google Scholar]
- [135].Mountjoy M, Alonso JM, Bergeron MF, et al. Hyperthermic-related challenges in aquatics, athletics, football, tennis and triathlon. Br J Sports Med. 2012;46(11):800–804. [DOI] [PubMed] [Google Scholar]
- [136].Medicine AC of S, Armstrong LE, Casa DJ, Millard-Stafford M, et al. American college of sports medicine position stand. Exertional heat illness during training and competition. Med Sci Sports Exerc 2007;39(3):556–572. [DOI] [PubMed] [Google Scholar]
- [137].Brocherie F, Millet GP. Is the wet-bulb globe temperature (WBGT) Index relevant for exercise in the heat? Sport Med. 2015;45(11):1619–1621. [DOI] [PubMed] [Google Scholar]
- [138].Budd GM. Wet-bulb globe temperature (WBGT)-its history and its limitations. J Sci Med Sport. 2008;11:20–32. [DOI] [PubMed] [Google Scholar]
- [139].Havenith G, Thermal Indices FD. Thermophysiological modeling for heat stress. Compr Physiol. 2015;6(1):1–48. [DOI] [PubMed] [Google Scholar]
- [140].Grobler L, Derman W, Racinais S, et al. Illness at a para athletics track and field world championships under hot and humid ambient conditions. J Inj Funct Rehabil. 2019. [DOI] [PubMed] [Google Scholar]
- [141].Mason BS, van der Woude LH, Goosey-Tolfrey VL. The ergonomics of wheelchair configuration for optimal performance in the wheelchair court sports. Sports Med. 2013. January;43(1):23–38. [DOI] [PubMed] [Google Scholar]
- [142].De Luigi AJ, Cooper RA. Adaptive sports technology and biomechanics: prosthetics. Pm&R. 2014;6:S40–S57. [DOI] [PubMed] [Google Scholar]
- [143].Notley SR, Flouris AD, Kenny GP. On the use of wearable physiological monitors to assess heat strain during occupational heat stress. Appl Physiol Nutr Metab. 2018;43(9):869–881. [DOI] [PubMed] [Google Scholar]
- [144].D’Souza AW, Notley SR, Brown EK, et al. The Hexoskin® physiological monitoring shirt does not impair whole-body heat loss during exercise in hot-dry conditions. Appl Physiol Nutr Metab. 2019;44(3):332–335. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- International Paralympic Committee . Rio 2016 [Online]. [cited 2019 Jan 7]. Available from: https://www.paralympic.org/rio-2016


