ABSTRACT
International competition inevitably presents logistical challenges for athletes. Events such as the Tokyo 2020 Olympic Games require further consideration given historical climate data suggest athletes will experience significant heat stress. Given the expected climate, athletes face major challenges to health and performance. With this in mind, heat alleviation strategies should be a fundamental consideration. This review provides a focused perspective of the relevant literature describing how practitioners can structure male and female athlete preparations for performance in hot, humid conditions. Whilst scientific literature commonly describes experimental work, with a primary focus on maximizing magnitudes of adaptive responses, this may sacrifice ecological validity, particularly for athletes whom must balance logistical considerations aligned with integrating environmental preparation around training, tapering and travel plans. Additionally, opportunities for sophisticated interventions may not be possible in the constrained environment of the athlete village or event arenas. This review therefore takes knowledge gained from robust experimental work, interprets it and provides direction on how practitioners/coaches can optimize their athletes’ heat alleviation strategies. This review identifies two distinct heat alleviation themes that should be considered to form an individualized strategy for the athlete to enhance thermoregulatory/performance physiology. First, chronic heat alleviation techniques are outlined, these describe interventions such as heat acclimation, which are implemented pre, during and post-training to prepare for the increased heat stress. Second, acute heat alleviation techniques that are implemented immediately prior to, and sometimes during the event are discussed.
Abbreviations: CWI: Cold water immersion; HA: Heat acclimation; HR: Heart rate; HSP: Heat shock protein; HWI: Hot water immersion; LTHA: Long-term heat acclimation; MTHA: Medium-term heat acclimation; ODHA: Once-daily heat acclimation; RH: Relative humidity; RPE: Rating of perceived exertion; STHA: Short-term heat acclimation; TCORE: Core temperature; TDHA: Twice-daily heat acclimation; TS: Thermal sensation; TSKIN: Skin temperature; V̇O2max: Maximal oxygen uptake; WGBT: Wet bulb globe temperature
KEYWORDS: Heat acclimation, heat acclimatization, thermoregulation, cooling, adaptation, athlete
Introduction
Heat stress negatively impacts performance in middle- and long-distance events [1], intermittent sprint activity [2], and during skill-based competition [3]. Strategies to attenuate heat strain i.e. reducing physiological and perceptual disruption prior to and during events such as the Tokyo 2020 Olympic Games are essential and can be divided into two distinct techniques, chronic heat alleviation and acute heat alleviation. This review details the current state of knowledge in these areas and makes recommendations for practitioners implementing heat alleviation techniques. This review should direct practitioners preparing non-disabled individuals for competition in heat stress to the optimal methods to attenuate the heat-induced performance decrements and to protect athlete health. Whilst many thermophysiology principles are shared, we direct the reader to literature describing techniques to alleviate heat strain in para-athletes, given critical and pertinent nuances should be considered from health and performance perspectives in this cohort [4–7].
The need for this interpretive summary of the literature is borne from data identifying that only 15% of surveyed athletes competing at the 2015 IAAF World Athletics Championships (host city Beijing, China), where heat stress was highly probable (Mean daily temperature and WBGT during the championships were 27 ± 3°C and 24 ± 2°C at 8:00, 31 ± 3°C and 27 ± 2°C at 12:00, and 30 ± 4°C and 25 ± 2°C at 16:00), adopted a recognized chronic heat alleviation strategy. Such strategies include acclimation (physiological or behavioral changes occurring within an organism, which reduces the strain or enhances endurance of strain caused by experimentally induced stressful changes in particular climatic factors [8]) or acclimatization (physiological or behavioral changes occurring within the lifetime of an organism that reduce the strain caused by stressful changes in the natural climate [8]). It was also reported that 52% of the surveyed had an acute heat alleviation strategy e.g. pre-cooling [9]. This despite of 48% of competing athletes having previously suffered from symptoms of a heat-related illness/symptoms which may impact performance e.g. cramping, vomiting, nausea, headache, fainting or fatigue [9]. Further to this, unpublished data collated by the authors highlight that a barrier to the implementation of heat alleviation strategies arises from an array of logistical issues or being unable to interpret contradictions and ambiguities in the literature effectively. Moreover, an ill-considered notion that athletes are “protected” from heat stress by virtue of their training status or prior warm weather training reinforces the avoidance of heat alleviation strategies, despite a lack of empirical evidence to support this [10]. It should not be assumed that an athlete’s high aerobic fitness prevents issues related to the heat/heat-related illness risk, with performance data clearly highlighting that heat negatively impacts performance in elite endurance events [1]. Though highly trained endurance athletes are partially heat acclimated (e.g. typically with high sweat rates), they are not excluded from the detrimental effect of heat on performance in the same way that athletes are not protected from altitude-related illness or performance detriments because they have greater red cell mass than those who are untrained [11]. Indeed, greater absolute detriments in performance come with increasing altitude in trained vs. untrained individuals [12] and even small, relative detrimental effects of heat stress on sports performance will greatly impact individual success at major international tournaments [1,13].
This review will highlight how acute and chronic heat alleviation techniques can be integrated into a preparation strategy through pertinent, applied questions, to prepare for heat stress and enhance thermoregulatory and performance physiology. The aim of chronic heat alleviation strategy/strategies is the induction of heat adaptation, which for many athletes is achieved through the completion of a heat acclimatization or heat acclimation (HA) protocol. Heat acclimatization is typically implemented as a training mesocycle immediately prior to competition, with HA a potent intervention which can be implemented as a micro- or mesocycle to induce a myriad of physiological, cellular and perceptual adaptations, which enhances an individual’s ability to tolerate heat stress. Heat adaptations can be induced rapidly (e.g. <5 d [14]), and whilst decay occurs over time (e.g. ~1–3 wk), expedient reinduction is possible [15,16]. HA can be implemented in different ways i.e. passively via resting in heat stress, actively via exercise in hot or hot-humid conditions, or a combination thereof. Acute heat alleviation utilizes techniques which provide additional “protection” against heat stress for the athlete(s) in the immediate hours and minutes prior to competing or indeed during the competition. Acute heat alleviation is similarly centered around optimizing the thermoregulatory and performance physiology, with emerging research now realizing the importance of improving the perceptual status of the athlete immediately prior to, and if appropriate and regulations permit, during the event [17–19].
Whilst the efficacy of acute techniques is robust, the authors are of the opinion that adopting robust chronic techniques cannot be understated. Indeed, there is good evidence to suggest chronic heat alleviation will be more effective [20,21]. Well-rehearsed, acute techniques to optimize thermoregulatory and performance physiology in the heat and minimize risks to health should not be considered as a “quick fix” alternative, but complementary to pre-planned and well-considered chronic alleviation strategies. The timeline from publication of this review to Tokyo 2020 will allow for repeated rehearsal and practise of these chronic and acute techniques to maximize their benefit and minimize the disruption to ongoing training.
In keeping with previous work [15,22,23], this review is written with the practitioner in mind and with athlete-centric considerations at the forefront of the content. To that end, the experiences of practitioners working with elite athletes have informed the perspectives within this review. Greater emphasis has been put on content, that to the authors knowledge, has been considered to a lesser extent elsewhere e.g. the time of day of HA, environmental conditions for HA, male vs. female differences to HA and, structuring HA around training. The authors direct the research-orientated reader to a number of excellent review articles and meta-analyses that consider specific elements of heat adaptation and/or thermoregulatory function from a mechanistic viewpoint [14,16,24–31].
Chronic heat alleviation
What adjustments are made to the thermoregulatory and performance physiology of the athlete following heat acclimation?
The homoeothermic nature of humans is reflected by the integrated physiological response to maintain an acceptable magnitude of exercise-induced hyperthermia, even when training/competing at performance intensities. The defense of core (deep) body temperature (TCORE) whilst attempting to maintain performance is supported by the multi-systemic adaptations that occur following repeated disruption to an individual’s thermal equilibrium. Figure 1 depicts the empirically supported adaptations to thermoregulatory, perceptual and performance physiology which occur following repeated bouts of exercise-heat stress via HA.
Figure 1.
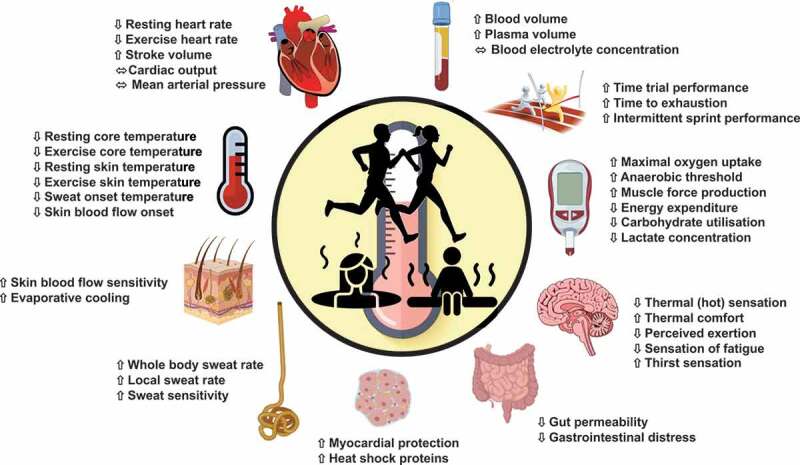
Summary of adaptations to thermoregulatory and performance physiology following exercise heat acclimation.
Chronic heat alleviation such as HA may induce; reductions in body temperature with lower TCORE and skin temperature (TSKIN) [32,33], sudomotor adaptations which initiate earlier sweat onset (i.e. greater sensitivity and lower temperature thresholds for sweating), greater sweat volume which can enhance heat dissipation via evaporation and more dilute sweat is secreted (i.e. conserved sweat mineral concentration) which preserves electrolyte balance [34–38]. Whilst large sweat volumes are generally a positive adaptation, athletes may already be capable of high sweat volumes such that, particularly in hot-humid environments where evaporation is limited, excess sweating beyond maximal skin wettedness is undesirable, leading to dehydration and/or increased feelings of discomfort. This may be particularly detrimental in prolonged events in heat stress where dehydration is likely to impact performance [39,40]. Strategies to optimize the magnitude of adaptation e.g. by varying the number of HA sessions are discussed later. Alterations in body water content with heat adaptation are mostly reflected by the hypervolemic response of the extracellular blood plasma over intracellular and interstitial fluid responses [41]. This hematological adaptation improves cardiovascular responses and reduces sensations of thirst sensitivity [42,43], that can combine with dehydration to impair performance [44,45]. Cardiovascular adaptations include reduced heart rate (HR) [46] and greater stroke volume [25,47], facilitating a more stable cardiac output and blood pressure response to the demands of exercise, despite the competing demands for blood between the skin and muscle as an athlete’s body temperature rises [48]. The myocardium itself may become more compliant and efficient in its contractions following HA [25,26]. Peripheral cardiovascular adaptations improve skin blood flow via earlier vasodilatory onset thresholds and greater rates of skin blood flow, that improve heat exchange between the skin and the environment [36]. Less well reported, but with important event/athlete-specific relevance, are improved thermal perception, in the form of reduced thermal sensation (TS) and improved thermal comfort [49,50], lowered ratings of perceived exertion (RPE) [51,52], and attenuated sensations of fatigue [53]. Metabolic adaptations (albeit reported in non-elite populations) include; lowered metabolic rates, reduced rates of glycolysis associated with a reduction in the relative intensity of exercise [54], and improved muscle contractility [55]. Heat adaptation is associated with elevated heat shock proteins (HSPs) with acute and chronic elevations in HSPs supporting/facilitating heat adaptation [56] and maintaining epithelial tight junctions in the gut, mitigating gastrointestinal distress when an athlete competes in the heat [57,58] and attenuating circulating precursors to heat illness [59]. With the athlete in mind, at a cellular level, the induction of heat adaptation via short- and medium-term HA does not appear to impact circulating markers of immune function negatively [60–63].
When considering the determinants of performance and the performance per se, HA has been demonstrated to improve maximal oxygen uptake [48,64–67], facilitate a rightward shift of the anaerobic threshold [48,60,64,68], and most relevantly, improve exercise capacity/tolerance in the heat [46,47,60,69–77], in some cases to levels comparable to temperate conditions [78]. In field-based team-sports, HA also improves intermittent exercise capacity and tolerance to the heat [79–85]. It is of course challenging to prove the erogenicity of HA in elite populations given it is near-impossible to assess this against an ecologically relevant control condition and thus, is something the practitioner should be mindful of when comparing responses in athletes to experimental data which is commonly collected on less well-trained individuals.
Should the athlete undertake acclimatization or acclimation?
Heat acclimatization typically occurs in a natural environment, in a location where training activities may combine with mean daytime temperatures to provide sufficient stimuli (elevated TCORE, TSKIN, and high sweat rates) for adaptation (e.g. >25°C) [26]. This allows athletes to live and most importantly, train in heat stress for extended periods (e.g. 1–4-wk mesocycle) prior to competition. In contrast, HA induces heat adaptations in an artificially created environment for shorter durations (e.g. a 4–14-d microcycle), whereby athletes repeatedly exercise in an environmental chamber as part of an active intervention or undertake a passive/resting intervention, typically involving post-training saunas or hot baths. To date, no published experimental work has effectively compared acclimatization with acclimation from an athlete perspective (i.e. using similar exercise intensities and protocol durations), though it has long been known the physiological basis of natural acclimatization is identical with that of HA [86]. In spite of the lack of specific comparative data in elite athletes, the timeline of performance adaptations is similar when examining endurance performance in individuals during acclimatization [78,84,87], HA [48,64,88–91], and when examining intermittent-sprint performance following acclimatization or HA [49,79,80,92–94]. Until experimental work demonstrates that one method is superior, the decision whether to acclimatize or acclimate athletes remains a consideration based upon individual circumstance (e.g. time, cost, logistical challenges, training disruption).
There are positive and negative aspects to both heat acclimatization and HA strategies with considerations to this effect outlined in Figure 2. HA proffers less disruption and expense, without diverse weather implications and likely travel fatigue associated with acclimatization [9]. That said, HA will require specialist facilities, with training often having to be completed on a stationary ergometer (i.e. running, cycling or rowing) [15], though “circuit/strength training” activity can be implemented [91]. The use of ergometry may be considered as a limitation, but this is arguably offset by the ability to individualize the protocol and regulate stimuli more precisely. Further to chamber-based HA protocols, alternate, cheaper and more accessible methods are now acknowledged as methods for passive (e.g. hot water bath) [95–98] and active HA strategies (e.g. overdressing and restricting heat loss during routine training) [99–101]. The authors acknowledge that different athletes will receive different levels of funding/support and this may influence their decision-making more greatly than the weight of empirical data, accordingly, discussions of the practicalities of implementing HA for the athlete follow. It is also acknowledged that access to specific facilities immediately prior to competition (e.g. athletics track or rowing lake) is necessary for specific training sessions to determine readiness for competition.
Figure 2.
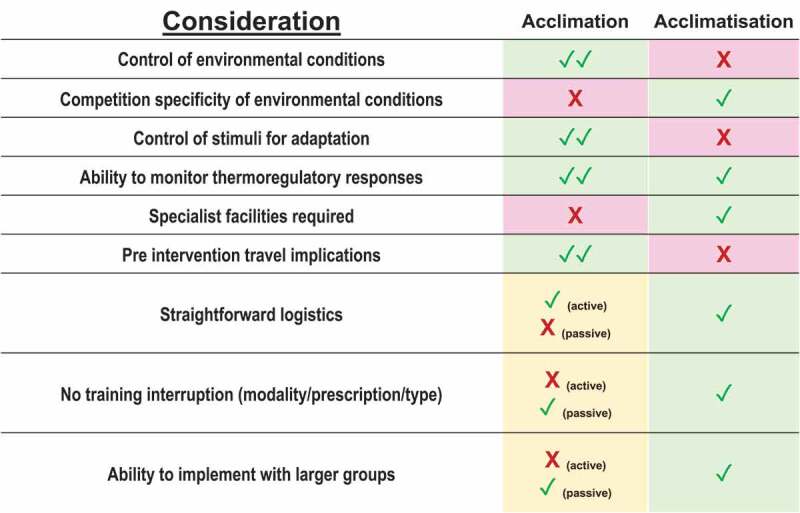
Advantages and disadvantages of using heat acclimatization or heat acclimation interventions with athletes. Note ✓ depicts positive, ✓✓ depicts very positive, X depicts negative, XX depicts very negative.
What are my options when implementing heat acclimatization/acclimation?
Exercise heat acclimation methods
Exercise HA to induce heat adaptation include exercising within naturally hot, hot-humid (e.g. acclimatization), simulated hot (e.g. acclimation) or temperate conditions with the use of additional clothing or restrictive heat loss attire (e.g. alternate acclimation) [16]. For inducing heat adaptations, the type of exercise does not appear to be a relevant consideration (aside from athlete preference) though most protocols utilize either cycling or running ergometry, unless a sport-specific ergometer is available (e.g. rowing), or a large indoor facility can be used to generate hot conditions for running/circuit training. Cycling may be more beneficial than running for athletes seeking general thermoregulatory and performance physiology adaptations, who must manage musculoskeletal load, given the non-weight bearing nature, lowering risk of injury/soreness. Similarly, from a practitioner perspective, cycling ergometry often allows larger groups of athletes to exercise. However, a limitation of ergometry is the inability to utilize sport-specific apparel (e.g. running spikes or protective attire). Typically, higher rates of heat production and storage, resulting from greater muscle mass recruitment and subsequently greater oxygen uptake, occur with running. This may be advantageous when utilizing isothermic techniques (outlined below), expediting the onset of heat strain during training. Nonetheless, practitioners, coaches, and athletes may choose their preferred modality (e.g. sport-specific) if available, to ensure maintenance of training and perceptual adaptation specificity, whilst ensuring the primary objective of adequate heat strain is achieved. Active HA strategies are categorized by their prescription method and typically fall into one of the following; self-regulated, fixed-intensity or isothermic [16,26].
Fixed-intensity HA
Fixed-intensity HA methods are the most commonly reported in experimental literature, particularly data collected >5 y ago, with this active method requiring athletes to exercise at a pre-selected intensity, which is fixed to elicit a certain cycling or rowing power output or running/walking speeds, relative to maximal aerobic capacity, or absolute/relative HR. The exercise intensity is typically set at ~50% maximal oxygen uptake (V̇O2max; i.e. in a moderate intensity domain) which may or may not be possible to prescribe accurately depending on how recently a maximal test has been conducted. Given the same fixed intensity is used for the entire session over the duration of the HA intervention, this method is simple to administer for individuals and groups of athletes alike. However, a critique of this method is that the stimulus for adaptation at the start of the intervention diminishes by the end of the intervention (especially over longer-term protocols), as the athlete enhances their ability to dissipate heat and aerobic capacity improvements are induced [26,102]. Recent data utilizing relative HR prescription [82] offer some progression in workload as cardiovascular adaptation occurs and therefore, this administration technique may offer some adaptation advantage despite reduced control over TCORE increase in comparison to other methods [103].
Suggestions have been made to optimize fixed-intensity HA and ensure complete heat adaptations are achieved. These may include progressive physiological strain by increasing the level of heat stress toward the latter stages of the HA intervention [104], increase exercise intensity (~5% V̇O2max per wk) [105], and/or prolong the duration of exercise (up to 2 min per HA session) [47,71,72,106]. This is required as athletes adapt to the intervention with day-to-day reductions in TCORE and exercising HR [104,107]. Progressively increasing these aforementioned metrics may not guarantee maintenance of the internal physiological stimuli for adaptation and thus, in spite of increased complexity of the intervention, increased adaptation may not always ensue. This has led to more recent support of independently controlling one of the primary drivers of human thermoregulation, TCORE, via isothermic HA.
Isothermic (controlled-hyperthermia) HA
Proposed as the current “optimal” method [108], isothermic HA (also referred to as controlled hyperthermia) involves an active heat stress phase (~30 min), where an elevated TCORE is achieved, followed by a maintenance phase, which is characterized by passive heat stress (e.g. resting in the hot environment) or low intensity exercise to elicit a prolonged period (~60 min) [103] at a targeted TCORE of ≥38.5°C [26,109]. The target TCORE (≥38.5°C) is a primary effector for heat adaptation with athletes maintaining sufficient, sizeable physiological strain for adaptation (e.g. continual elevations in TCORE and TSKIN with concurrent high sweat rates), even as they adapt during HA. It should be noted that experimental data highlights that there is no adaptive advantage to targeting an even higher TCORE (e.g. 39.0°C) [50,105], and therefore, more strain (in this context) is not necessarily more beneficial for the athlete. The primary benefit of the isothermic method is that athletes maintain the same absolute stimuli for adaptation within each session, rather than being exposed to a diminishing stimulus as adaptation occurs (as noted in fixed-intensity strategies).
The prescribed exercise intensity during the active phase of isothermic HA varies and can include; self-regulated intensity (e.g. a rating of perceived exertion [RPE] of 15 [106]), intensity relative to body mass (e.g. 2.0–2.7 W.kg−1 [64,103]), or as a percentage of HRmax, or V̇O2max (e.g. 50–65% V̇O2max [50,110]), to reach target temperatures within ~30 min. At the current time, recommendations are that relative power provides the best training prescription method given its closer relationship with increases in TCORE (and likely heat production) than perceptual responses or prescribing exercise based upon relative intensities aligned to physiological responses [103]. Moreover, this approach is simple to administer, negating additional interruption to training by removing the need for an a priori maximal exercise test to derive exercise intensities from. To implement isothermic protocols effectively and safely, TCORE must be continually monitored (e.g. every 5 min). The recommended method is rectal measurement or a gastrointestinal pill, although it is recognized alternative TCORE measurements (e.g. tympanic membrane) may be utilized by experienced practitioners who recognize the limitations of this method. Notably, the tympanic membrane may under-represent deep body temperature absolutely but should demonstrate similar change [111] and is an approach used safely and effectively [112].
Experimental comparisons have been made between fixed-intensity and isothermic HA protocols, with no difference in the magnitude of physiological adaptation occurring [50,105]. Figure 3 depicts exercise intensity and notional TCORE response to an isothermic HA protocol against a fixed-intensity HA protocol (~50% V̇O2max), commencing from a TCORE of 37.0°C. In this figure, the isothermic HA protocol commences with a higher exercise intensity (~70% V̇O2max), such that TCORE rises rapidly to the endogenous target of 38.5°C during the active phase (~30 min in duration [73,106,113,114]). Following the attainment of the target TCORE in 30 min, the 60 min maintenance phase follows, whereby, seated rest or low-intensity exercise effectively maintains the stimuli for adaptation throughout the session (total duration of 90 min). This biphasic method contrasts the fixed-intensity protocol, whereby, a lower exercise intensity elicits a slower increase in body temperature throughout the session. Isothermic protocols benefit from time-efficiency, involving a lower training volume [50], as exercise is closely matched to achieve a specific physiological target. However, the moderate intensity domain training may not be representative of a self-selected (performance) intensity, affecting the induction of perceptual adaptations. Higher intensity work in isothermic HA is not necessarily a negative, often it is favorable for an athlete to undertake higher intensity work (similar to regular training or competition intensity for a shorter duration, as opposed to exercising at lower intensities for long durations) [50].
Figure 3.
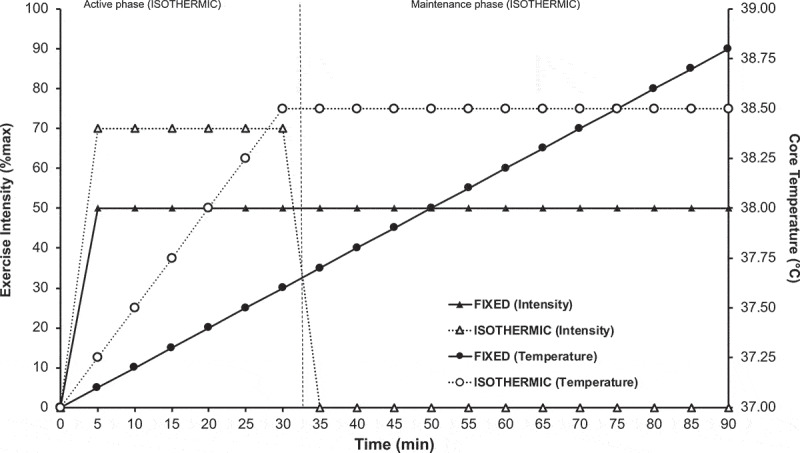
Notional core temperature responses to a fixed intensity protocol (filled circles [TCORE]/triangles [exercise intensity]) and isothermic HA protocol (open circles [TCORE]/triangles [exercise intensity]) performed on a cycle ergometer in 40°C and 40% RH. Change in temperature based upon an individual exercising at 1.3 W.kg−1 (fixed intensity) or 2.7 W.kg−1 (isothermic) [95].
Self-regulated HA
Self-regulated HA methods enable athletes to select their own exercise intensity based on their training status and perceived demand of the exercise and environmental conditions [115,116]. This can be achieved by clamping exercise in relation to their RPE, or another athlete-specific self-regulating variable, for all or part of the HA session [106]. Like relative intensity exercise prescription during isothermic HA [103], self-regulated methods may offer the greatest practical application for large groups of athletes training simultaneously, as minimal monitoring equipment is required and when time is restricted, the practitioner can forgo prior physiological assessments commonly required to prescribe relative intensities (e.g. V̇O2max testing). Whilst this method permits athletes to work at sport-specific/self-directed intensities, this method may sacrifice rigor and be subject to greater inter-session variability and therefore, compromise the attainment of precise stimuli for adaptation. This method may also be counterproductive if athletes push themselves too hard and compromise health in pursuit of adaptation.
Passive strategies
Passive strategies are a desirable intervention given the athlete experiences no additional external training load to accommodate HA, which may be especially important during a taper phase. This “live cool, train cool, acclimate hot” method, where HA occurs following training in temperate conditions to maintain training quality is akin to the “live high, train low” altitude paradigm. Passive strategies include; residing in simulated heat stress in environmental chambers [16,117–119], wearing restricted heat loss attire (e.g. over dressing in heat stress) [120], wearing water-perfused suits [109,121], sauna exposures [95,122] or hot water immersion (HWI) [96–98,112,123,124], all of which “raise and maintain” a moderately high TCORE (e.g. 38.0–38.5°C) alongside high TSKIN (>38.5°C). Passive sessions are typically completed as an individual strategy, independently of training commitments, prescribed prior to [120] or following routine training [98] in hot or temperate conditions. Access to sauna or HWI facilities should be as immediate as possible and practitioners should be mindful of this when planning passive strategies given debriefs, equipment storage and other practicalities are commonplace post-training. Evidence indicates that passive strategies, which provide higher TSKIN than active-only strategies, are effective when implemented in conjunction with active strategies, therefore athletes may choose to apply a combination of passive and active techniques, as successfully utilized prior to a major sporting competition in heat stress (e.g. World Cup 2014; Rio de Janeiro, Brazil) [112] providing flexibility to ensure that the primary objectives of the overarching physical training program are met.
A recent review of passive methods [125] concluded that these strategies can be used to induce heat adaptations, such as a reduced resting and/or exercising TCORE [96–98,119,121,124], TSKIN [96,98,121], and HR [96,98,118,126]. Passive methods for HA also improve sweat onset thresholds and enhance sweat capacity [98,127]. Expansion of plasma volume can occur depending on the protocol [95,98,121,122], and improved perceptual responses, such as RPE and TS have been reported [98]. These adaptations to thermoregulatory and performance physiology can also elicit improvements in endurance capacity (e.g. V̇O2max) and aerobic performance (e.g. 5 km time trial) [95,98]. Post-exercise HWI appears to be the most well-reported intervention to induce adaptations in thermoregulatory and performance physiology associated with HA, with the magnitude of adaptation similar irrespective of training status [97]. To implement this technique, athletes should undertake their normal training in routine environmental conditions, and then seek to immediately submerge themselves to shoulder height in ~40°C water, with immersion times ranging from 10 to 40 min. The HWI duration will depend on the athletes’ preference, tolerance, exposure number and stage of acclimation with an important acknowledgment being that the athlete should “feel hot” but cease the intervention if they feel “too hot, dizzy or lightheaded”. For the novice post-exercise HWI user, supervision and monitoring of TCORE may be desirable. Exposure time will likely increase as the athlete acclimates resulting from reduced TCORE, improved blood pressure regulation and enhanced thermal perception, providing an indication of adaptation in itself. This simple, effective protocol has improved running performance in untrained individuals [98], though performance adaptation has yet to be quantified in well-trained individuals. Whilst theoretically simple to implement, assuming access to hot water and a “bath” to reside in, if HWI is not feasible, sauna exposure is an alternative passive HA technique whereby, post-exercise implementation can lead to performance improvements [95]. The erogenicity of this technique apparently facilitated by hematological adaptation [95]. Observations of performance improvements following post-exercise sauna are not consistent, with others reporting that in spite of physiological adaptation, no performance adaptation occurred [122]. It may be that for athletes to improve exercise performance under heat stress, they potentially need to experience and exercise under heat stress (e.g. active HA), thus whilst physiological adaptation occurs, performance improvement may be contingent on enhanced pacing which would be observed with exercise-heat stress in accordance with familiarity to a representative sport-specific thermal discomfort.
Passive strategies are beneficial (e.g. inexpensive and limit training disruption), induce heat adaptations (e.g. reduced TCORE and HR), improve exercise performance [98] and therefore, address limitations associated with active strategies. For the practitioner, passive strategies still require considerable planning giving limited access to baths and hot water at training facilities at training camps/venues. At the current time, no data has compared passive and active HA. Cross-examination of studies investigating these methods independently identifies that the most measurable difference between passive and exercising adaptation appears to be plasma volume expansion [128] and enhanced sudomotor responses [129], that are common in active strategies, but not so clearly evidenced in passive strategies. As a direct comparison of active vs. passive HA interventions has yet to be conducted, it is not possible to identify whether one is preferential, thus both must be considered based upon their respective merits, or combined to suit the athlete(s) [112,130]. For athletes who struggle to train effectively in the heat, or those who do not wish for tactical or technical training to be impacted by exercise HA, passive HA could be implemented as a preliminary strategy to establish thermoregulatory adaptations prior to a commencing an active HA intervention. Similarly, for athletes who already sweat high volumes of unevaporated fluid, passive HA such as HWI, may effectively induce central adaptations e.g. reduced TCORE, without inducing excessive peripheral responses.
Can we utilize excess or specific clothing to restrict heat loss, and induce adaptation?
Another simple and inexpensive technique to inducing some elements of heat adaptation is to have athletes overdress (i.e. wear more clothing than typically required for the task) or wear a vinyl sauna/sweat suit (which restricts heat loss/evaporation, creating a hot-humid microclimate close to the skins’ surface) to increase TCORE and TSKIN above that of training in normal clothing in temperate conditions, and promote greater sweating. Whilst greater sweating occurs, from the outset the authors affirm sentiments from others that this should not be used as a tool to reduce body mass rapidly (e.g. prior to weight category competition) and well-considered plans to meet weight (mass) should be implemented [131–133]. In spite of many studies showing an acute session of “overdressing” provides some thermal strain for adaptation [100,101], experimental work conducted indoors in temperate conditions utilizing this method, suggests that this is unlikely to be as effective as a hot air/water HA interventions [134]. It may, however, prove partially effective for those who are unable to access genuine heat stress (simulated or natural), or be combined with established HA interventions to provide flexibility [112,120] and affordability. Overdressing during outdoor cycling exercise appears to be ineffective, reflecting the greater cooling air flow experienced when cycling outdoors (vs. stationary ergometry) and concurrent minimal changes in physiological/thermoregulatory strain, with no adaptations observed during an applied study [99].
At present, experimental data support the use of active isothermic HA or passive post-exercise heat exposures to induce adaptation and manage training disruption. A greater volume of data support improvements in exercise performance following active HA and accordingly, we encourage practitioners to consider this as the optimal technique to induce adaptation in athletes. Post-exercise passive heat exposures, e.g., HWI, may be considered a viable alternative when access to hot environmental facilities for active HA is not possible, for those who are intolerant of exercise in the heat, those wishing to make initial adaptations as a precursor to exercise training, and those who wish to combine chronic heat alleviation methods to fit an intervention around complex training and logistical plans.
How long does heat acclimation take to induce, and how long is a typical heat acclimation session?
In line with conventional training programs, HA must consider the overall timescale, session duration, session frequency and exercise prescription [26], but additionally, the heat stress mode and magnitude, as well as the option for passive heat exposures. The primary categorization is the intervention duration, with short-term ([STHA] ≤5 d), medium-term ([MTHA] 6–10 d) and long-term HA ([LTHA] >10 d) being common demarcations, though these are somewhat arbitrary. Within these timescales, individual sessions during HA vary in duration (from 30 to 120 min), reflecting the specific needs of the athlete and circumstances (e.g. aerobic fitness, time, training cycle, cost, facilities, and equipment). A concern when prescribing HA based upon the number of sessions alone is that this can lead to markedly different HA doses. STHA may require 2–10 h of athlete time, with MTHA ranging from 2.5 to 20 h and LTHA lasting 5–40 h, thus whilst two studies may report STHA, the training volume eliciting potentiating stimuli for adaptation may be vastly different (e.g. 5 × 30 min sessions vs. 5 × 120 min sessions). Experimental work has seldom considered the heat dose or volume, in this way (i.e. HA-minutes as proposed elsewhere for hypoxic exposures [135]), thus the minimum time required to induce adaptation is not well known and experimental work often cites mixed findings without effectively controlling this. Practitioners should be mindful of this when interpreting research findings as the variable HA dose may explain the wide range in magnitudes of adaptation, particularly following STHA [14]. In reality, the deciding factor when considering the duration of an acclimation intervention for athletes is likely to be their training schedule and whilst more exposures typically lead to a larger magnitude of adaptation, this may not be optimal given the diminishing returns in adaptation that occur at the latter stages of an HA intervention. The necessary training volume during MTHA/LTHA rationalizes the desire to minimize additional exercise training volume during HA and the greater interest in isothermic or post-exercise techniques that help to mitigate increases in external training load.
The adaptive effects of MTHA (>6–10 d) and LTHA (>10 d) have received much research attention, historically as a means for determining “maximal” adaptation [47,75,77,114,136]. Recent reviews have considered the application of STHA (≤5 d) [23,137] as a highly desirable intervention timescale for the athlete, particularly when training load is already high, or implementation of HA may require careful consideration prior to competition [138,139]. Central adaptations, such as reduced HR and TCORE, appear to be augmented during STHA timescales, with MTHA/LTHA maintaining or improving the HR and TCORE adaptation whilst eliciting greater sudomotor and hematological (e.g. increased plasma volume) responses [137,140–143]. The practitioner should consider the individual needs of the athlete when prescribing the number of HA sessions rather than pursue maximal adaptations. As stated earlier in this review, excessive sweating beyond the evaporative capacity of the environment may be more likely following MTHA/LTHA vs. STHA. This could be undesirable and lead to greater deficits of body water content which confound other HA adaptations.
Effective HA interventions have typically implemented minimum daily heat exposures which are combined with aerobic exercise of between 90–120 min in duration, irrespective of the precise method used [27]. However, considerable supportive evidence exists for shorter sessional protocols (e.g. 60 min), demonstrating effective heat adaptation [23,60,137]. Whilst HA sessions of 30 min continuous exercise have demonstrated adaptation [144], several studies have also demonstrated a minimal response for this duration (particularly over STHA) [52,145] and in this regard, even if exercise durations are minimized, the heat exposure duration should be prolonged, likely by implementing an extended maintenance phase post-exercise or combining exercise with a passive HA technique.
What are the optimal environmental conditions for HA?
Athletes will benefit from HA performed in the expected environmental conditions that the competition will occur within [108], with the reader directed to a recent review outlining anticipated heat stress, and indices to describe heat stress in Tokyo [146]. This strategy has been widely implemented and it is beneficial given athletes can specifically understand how they will respond to a representative environment to which they will compete in [147]. Whilst it might be logical for athletes to prepare in conditions which represent the mean environmental conditions in which they will be competing, for example, mean air conditions for Tokyo in August are 30–31°C, ~70% RH, the authors (and others) recommend that as a minimum, athletes train in the maximum/upper limit of environmental conditions which are forecast for the location at the time of year, for instance maximum air conditions for Tokyo in August are >34°C, >80% RH [146]. Indeed, it has been proposed that HA temperatures should be 5–10°C higher than the mean of the event location [148], in keeping with conventional training programs that mimic “worst-case scenario” game demands [149–151]. Athletes and practitioners should also be cautious of being reliant on mean temperatures, particularly given within day differences of ~5°C are likely and events/heats may be scheduled at different times of the day [146]. As part of a “prepare for the worst, hope for the best” mantra, this should evoke condition-specific adaptations, while optimizing HA toward the expected most oppressive conditions [143]. As such athletes and practitioners should also be cautious in relying on natural acclimatization upon arrival as the environmental conditions preceding the event may not reflect the conditions during the event.
As well as replicating event demands, athletes may also benefit from training in greater heat stress conditions than the expected environment [147]. The majority of experimental HA occurs in 40°C and 40% RH [14] to improve the efficiency of adaptation particularly when implementing isothermic HA, where external heat stress is a vehicle to achieve high internal heat strain (e.g. TCORE). A proposed modification to the aforementioned 40°C and 40% RH consensus would be to reduce the rate of evaporative heat dissipation, by increasing the relative humidity of the ambient conditions or prolonging the restriction of heat loss via other means (e.g. additional clothing or passive HA). It has been observed that under fixed workloads and absolute ambient temperature (~30°C), cycling time to achieve a fixed TCORE is reduced with increasing relative humidity, highlighting the effectiveness of elevated humidity in the earlier attainment of a target TCORE for isothermic HA due to impaired evaporative heat loss [152]. In simple terms, increasing humidity of the HA environment would inhibit heat loss via evaporation to a greater extent and reduce the time taken to achieve a targeted elevated body temperature e.g. target 70% RH, rather than 50% RH will expedite the attainment of a TCORE of 38.5°C. When matched for relative heat stress, no difference exists in performance, or acute physiological responses to exercise in hot-dry vs. hot-wet environments [153]. However, adaptation to HA between hot-dry and hot-wet environments may differ subtly [154,155]. To enhance adaptation, or at least improve the efficiency of the intervention by reducing the required training volume at the same absolute temperature, humidity could be increased, enhancing the relative heat stress. Given passive heat stress following exercise is a component of the maintenance phase of isothermic HA, a hotter/more humid environment would be more favorable for maintaining heat storage. Clearly, this flaws experimental comparisons between conditions due to differences in wet bulb globe temperature (WGBT) at an air temperature of 40°C, however, from an applied perspective for the athlete this is favorable. For athletes with a history of poor response to exercising under heat stress, dry heat stress may be preferable at the start of HA followed by progressive humid heat stress at the latter stages, to further stress cardiovascular and thermoregulatory function [108]. The initial dry heat stress being more tolerable and will allow heat adaptions to be made prior to the more stressful hot-humid section of the intervention to further refine adaptation later in the intervention. Similarly, progressive increases in simulated environmental conditions for HA are recommended for those who cannot maintain training quality or for individuals whose health may be compromised should unfamiliar heat strain be experienced.
A critique of much of the experimental work in HA is that it fails to account for radiative heat gain from the sun and competition surfaces [156], which athletes experience when exercising outdoors, and this may be an important consideration for pacing strategies and the performance intensity adopted [157]. The authors acknowledge this and recommend that athletes who undertake much of their chronic heat alleviation work indoors, should spend time exercising outdoors in hot environments with direct sun exposure to understand their physiological and perceptual responses, and better plan/practice their pacing/event strategy more comprehensively. Practitioners should be mindful that events may take place in the day and evening, and thus prepare athletes for both. Furthermore, appropriate protective clothing must be identified, in combination with appropriate sun-block [158]. Part of this planning should acknowledge HA can be implemented as a microcycle around training in the weeks and months leading up to competition. Whilst previously it has been recommended that HA should be performed immediately prior to competition, physiological adaptations to HA are induced potentially alongside a molecular memory, with researchers speculating that a more rapid re-induction occurs as a result of this [28,159,160], this concept has yet to be effectively examined mechanistically in humans/athletes. Based upon this understanding, we and others support the notion of undertaking dedicated HA microcyles periodically in the lead up to competition [16]. This means that prior to competition rapid re-induction/retention of HA can be obtained whilst experiencing actual competition conditions and may be appealing particularly for athletes/teams for whom extended periods at hot weather holding camps are not possible. Data supporting this concept are discussed in the section entitled “How long do the adaptations last and how can they be retained?”.
Do athletes need to train in the heat every day?
A long-standing consensus is that to optimize thermoregulatory adaptations, daily heat exposures are the priority HA technique, with minimal adaptation occurring when training includes regular “rest” days or without heat exposures (“intermittent” exposures). i.e. whilst end-exercise TCORE reduced during intermittent (every other day) HA, the reduction was lesser than a consecutive day method, this also being true of final exercise HR or TSKIN, suggesting inferiority. A theoretical model of the adaptation stimulus [161] proposes that intermittent exposures fail to stimulate adaptive pathways continually and potentially initiate a decay in adaptations, which is not observed with daily exposures. As eluded previously, a critique of this study is the use of 30 min HA sessions, with a longer session more likely to induce greater strain and thus greater adaptation. It is noteworthy that when team-sport athletes perform longer HA sessions (>40 min), it appears irrelevant whether eight HA sessions consisting of intermittent sprint activity are performed on consecutive or intermittent/alternate days as comparable adaptation occurs with either method [83]. More recently it has been shown that four 45 min HA sessions, administered over two consecutive days (i.e. twice-daily HA; TDHA), demonstrated similar adaptations to four consecutive once-daily HA sessions (ODHA), typical of an STHA intervention [89]. A follow-up study examined the magnitudes of adaptation within an MTHA intervention (10 x 60 min sessions) performed on alternative days but in a twice-daily technique. Equivalent heat adaptations and enhanced exercise performance (e.g. reduced TCORE HR, plasma volume expansion, perceptual responses, sweat setpoint and sweat gain, V̇O2max, and power at the lactate threshold) in the heat were induced by ODHA and TDHA, compared with equivalent temperate exercise [60]. Most importantly, no difference in the magnitude of adaptation and enhanced exercise performance were observed between either nonconsecutive twice-daily or consecutive once-daily HA when protocols were matched for volume and intensity. This highlights that nonconsecutive twice-daily HA provides an alternate method to consecutive once-daily HA to induce adaptation without requiring consecutive day training [60]. That said, it is essential that if athletes undergo two sessions of HA in 1 d (e.g. TDHA), emphasis toward recovery strategies (e.g. rehydration and nutrition) is imperative, with ~6 h spent in cool conditions recommended between successive bouts of exercise-heat stress (e.g. 08:00 and 16:00 h) to reduce any residual effects of the previous physiological strain [162]. The TDHA approach lends itself to the athlete who is familiar with training multiple times in the same day (e.g. endurance athletes), and practitioners should be carefully manage increases in training time/volume in individuals who are unfamiliar with this approach. Conceptually, these findings suggest the dose of HA (e.g. matched weekly exposure and intensity) is most important for the mechanisms which underpin adaptation, as opposed to the structure of HA (e.g. frequency [once- or twice-daily] and timing [morning or afternoon]) and therefore, athletes are able to adjust the integration of HA sessions around their training, travel and recovery commitments [60]. This has also been implemented well in an intermittent sprint application without compromising the taper or competition performance [112].
Is the time of day when HA is performed a relevant consideration?
Whilst the implementation of an HA intervention itself can be modified to suit individual circumstances, it has previously been proposed that HA adaptations are time-of-day/clock time specific, and in some instances, it has been explicitly recommended that HA be performed at the same clock time as the impending competition/event [137]. In reality, this would be hugely challenging for practitioners to achieve given variable event times during the day, as many athletes will travel across multiple time zones to compete. As discussed below, fortunately, it may not be as relevant consideration as initially perceived.
Recommendations for ensuring clock time for HA interventions and the subsequent task are equal, are predominantly attributable to data highlighting that prolonged passive HA (sitting in a hot room) reduced sweat latency and decreased the TCORE threshold for sweating [163]. These authors concluded the autonomic and behavioral thermoregulatory systems may be activated during or just before the specific clock time of HA, so that their heat tolerance ability is improved to prepare for a foreseen heat stress at a fixed time-of-day. More recent experimental data suggest clock time appears unlikely to have a strong influence on subsequent exercise heat stress as HA induces a myriad of multi-systemic adaptations [27,143], some of which are governed by autonomic control (which may be somewhat clock time specific) [25], yet others likely remain stable irrespective of clock time (e.g. plasma volume expansion) [114]. Contrary to the notion of a fixed clock time for adaptation, it has been reported that when implementing a post-exercise HWI model for inducing HA, morning HA induced adaptations at rest and during exercise-heat stress in both the morning and mid-afternoon [96]. It was noted that adaptation to the TCORE threshold for sweating onset was similar in the morning and afternoon, this was alongside reductions in resting and exercising TCORE, HR, RPE, and TS of a similar magnitude, irrespective of the time-of-day. In support of this lack of time-of-day-dependent adaptation, an isothermic exercise HA model with 40% of the HA taking place in the late afternoon (the remaining 60% taking place in the morning within a TDHA model) observed participants adapted to the intervention to the same extent as those undertaking ODHA (100% of sessions taking place in the morning) [60]. Collectively, these recent data suggest that HA is not as time-of-day dependent as previously thought and athletes should seek to implement HA in a manner which complements their existing training schedule, rather than make wholesale training adjustments to coincide with an event or avoid scheduling HA at all.
The time of day for HA may be of relevance depending on the type of intervention. Whilst fixed-intensity and isothermic HA interventions generally elicit similar magnitudes of adaptation when performed at the same time-of-day [50,105], isothermic HA has been proposed as superior/more efficient given they induce equal adaptations for a reduced workload [15]. It is in this regard that the time-of-day may greatly impact the exercise requirements to achieve the endogenous stimuli for adaptation (the change in TCORE) in an isothermic protocol, given typical fluctuations in circadian rhythm and thus, starting TCORE. To illustrate this, Figure 4 depicts isothermic and fixed-intensity protocols performed in the morning (starting TCORE of 36.5°C) vs. afternoon/evening (starting TCORE of 37.5°C [111]). In the fixed-intensity protocol, the increase in TCORE is equal (+1.8°C), but the mean/end TCORE is greater given the elevated starting temperature (AM = 38.3°C; PM = 39.0°C), suggesting the time-of-day is impacting upon the magnitude of endogenous stimuli experienced. The clock time for HA has a greater impact on the isothermic HA protocol. This is because the higher basal TCORE in the afternoon/evening requires a reduced volume of exercise to attain the isothermic TCORE target of 38.5°C (e.g. morning = +2°C, 40 min exercise duration; afternoon/evening = +1°C, 20 min exercise duration) further improving the “efficiency” of this type of intervention for those who wish to minimize training volume. The differences between morning and afternoon HA may be amplified toward the end of isothermic HA, given the lowering of TCORE is an expected adaptation. This has been demonstrated empirically with an increased exercise duration from 29 to 39 min in trained cyclists undertaking an 8-d isothermic protocol [106]. Accordingly, the notional TCORE responses (Figure 4) described as AM and PM could also be classified as post-acclimation and pre-acclimation, respectively, to illustrate the need to adjust workloads as adaptation ensues if matched exercise duration is required [111]. A caveat to both of these points is data indicating that the rate of TCORE increase may be slightly (but not significantly) greater in the AM vs. PM [164]. However, even accounting for the difference in the rate of change, the time to achieve a + 1.5°C increase in TCORE is <5 min slower, later in the day, which still supports the efficiency of adjusting the time of day for HA to suit the individual.
Figure 4.
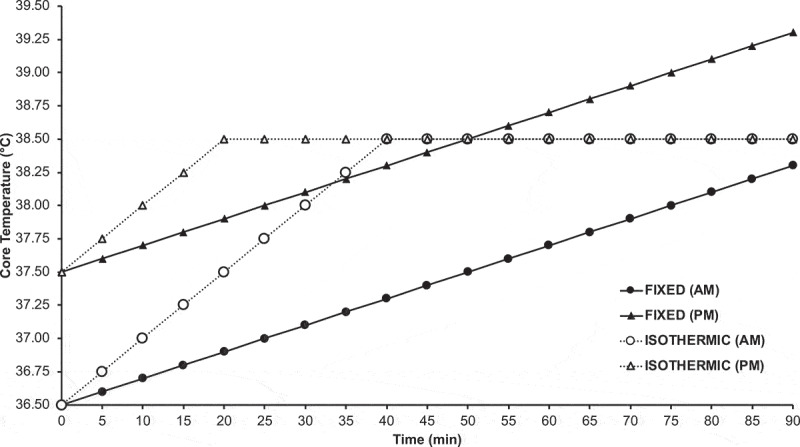
Notional core temperature responses to a fixed intensity protocol (filled circles/triangles) and isothermic HA protocol (open circles/triangles) performed during the morning (~08:00; circles) or evening (~18:00; triangles) on a cycle ergometer in 40°C and 40% RH. Change in temperature based upon an individual exercising at 1.3 W.kg−1 (fixed intensity) or 2.7 W.kg−1 (isothermic) from [95]. Resting morning and evening core temperature based upon data from [103].
To enhance experimental rigor, the time-of-day is an important consideration when examining the effects of HA on performance and physiological response pre-post intervention, largely due to the impact of circadian rhythm on TCORE and the concurrent changes in physiological responses/adaptations resulting from it. Researchers and practitioners should be mindful of the impact time-of-day may have on the implementation of HA interventions and the magnitude of adaptation attained. At the current time, it is not known with certainty whether time-of-day is a beneficial, negligible or inconsequential consideration in this regard. Importantly however, the need to be consistent in the time–of-day of an HA intervention for athletes appears debateable, therefore, difficulty in committing to a precise clock time for HA training should not preclude its use as a heat alleviation strategy altogether.
Do trained individuals adapt as much as untrained?
The effect of training status on the magnitude of adaptation has not been widely reported. It is commonly noted that individuals of a higher training status (i.e. higher aerobic capacity/power) demonstrate “partial HA” adaptations/characteristics from their habitual training (where they routinely experience elevated TCORE, TSKIN and sweat rates as a result of high absolute intensities). Recent work has suggested that improved aerobic fitness is a key predictor in mitigating against undesirable change in TCORE during exercise [165]. Seminal work (from an occupational rather than athletic setting) noted that higher aerobic fitness (V̇O2max ~60 mL.kg−1.min−1) from long-term training is of benefit during fixed-intensity exercise in the heat and that the magnitude of improvements in physiological strain with HA is greater in those with high aerobic fitness i.e. those who are more well trained adapt better [75]. This, however, should be taken in the context given these findings are drawn from a study where trained individuals demonstrate an improved thermoregulatory response to the same absolute intensity exercise task i.e. exercising at the same treadmill speed (but therefore different relative intensities), in comparison to those less well trained (V̇O2max ~46 mL.kg−1.min−1). When trained and untrained individuals exercise at the same absolute heat production, this effect is likely diminished [166,167]. An enhanced sudomotor response to equivalent tasks/heat production partially offsets the increase in temperature and cardiovascular strain more greatly in higher trained individuals for the same absolute speed/power/intensity. With regards to the magnitude of adaptation, more recently classical markers of HA, such as alterations in TCORE and HR, appear to respond equally to both isothermic exercise HA [168] and post-exercise HWI interventions [97] in recreationally active and endurance-trained individuals. Thus, the merits of the intervention are apparent for many individuals and the individual variability in the adaptation is likely of greater magnitude and unrelated to aerobic capacity [10].
Do females adapt at the same rate as males?
Given elevations in TCORE during the luteal phase of the menstrual cycle, and subsequent shifts in vascular and sudomotor heat loss pathways during this time [169,170], as already outlined by others [171], it has been proposed that in spite of similar absolute changes in TCORE when performing in the heat during the luteal phase, females face a greater performance detriment. This detriment resulting from a higher baseline at this stage of their menstrual cycle in comparison to the follicular phase. The concerns around performance in the heat during the luteal phase have recently been partially appeased, given that autonomic heat loss responses at rest and during fixed‐intensity exercise in well‐trained women, are not affected by menstrual cycle phase [172]. Similarly, though individuals report greater physiological/perceptual strain at different phases, exercise performance does not ubiquitously differ across the menstrual cycle [172], although a) manipulation of menstruation is common in athletes as a way of regulating performance [173], and b) for some individuals, menstruation is highly (negatively) impactful on training and performance. Together these points make it a necessity to tailor strategies to optimize thermoregulatory, physiological, and perceptual responses to training and performance in the heat at an individual athlete level. Data indicate that between 50% [173] and 80% [174] of female athletes take hormonal contraception, which is known to increase resting TCORE by ~0.3°C [175,176] and is likely to have other physiological consequences, although elucidation of this mechanism needs further investigation. Individual variability to athletic performance in the heat throughout the menstrual cycle should of course be at the forefront of the mind of the practitioner. All practitioners and female athletes should be mindful that hot-humid conditions will reduce evaporative cooling and therefore, present a greater performance detriment and risk of heat-related illness in comparison to hot-dry conditions [172]. This is particularly pertinent given thermoregulation is less effective in females vs. males at higher rates of heat production that are associated with performance intensities [177]. Specifically, females exhibit a reduced sudomotor response to exercise heat stress, that ultimately limits evaporative heat loss in comparison to males [177]. Challenges to thermoregulation and performance may be even more greatly compromised in amenorrheic athletes via direct and indirect means [178], with little currently known of the impact of amenorrhea on thermoregulation in athletes.
The majority of the literature describing chronic heat alleviation techniques is collected in male participants, and accordingly, this raises doubts as to the confidence with which these findings can be directly applied to females. Recent work has begun to address the disparity in data examining sex-specific responses to HA as it is known that oral contraceptive users likely have an altered sweat response [179] and there are notional effects of estrogen on the HSP response [180]; both hallmark adaptations of HA [27,143]. In a study examining the magnitude and temporal patterning of HA between males and females using an isothermic HA protocol [110], it was noted that while STHA may be effective in achieving partial adaptation in females, females require LTHA to establish reductions in cardiovascular and thermoregulatory strain that are comparable to males. This is despite similar within-session stimuli for adaptation (e.g. change in TCORE). It should be noted that this was observed in an experiment during which females exercised at lower absolute exercise intensities and therefore lower rates of absolute heat production which may account for differences [181]. More recent work is also supportive of the need for MTHA vs. STHA interventions in females, particularly those moderately trained (V̇O2max ~47 mL.kg−1.min−1) who are seeking performance adaptations [182], although due to the duration of the experimental design adopted in these HA studies [110,182], responses were invariably evaluated across different phases of the menstrual cycle in both eumenorrheic and oral contraceptive users, which in part explain their findings. HA protocols should therefore be tailored to target sex differences, as although STHA within one menstrual phase can effectively induce typical HA responses [80,120,183], sex determines the temporal patterning of HA [110]. Therefore, instead of additional HA training sessions or utilizing a more humid HA environment (e.g. mist sprays to achieve >60% RH), sudomotor priming can be used, to ensure earlier (and therefore greater total) sweating in females. This has been achieved through over-dressing in vinyl suits and passive heat exposure (50°C) prior to HA training, to improve the magnitude of adaptation in females [120]. Practitioners working with less aerobically trained individuals (e.g. some games players) may also consider this to induce adaptation prior to commencing more well-established HA protocols. When administered effectively, heat adaptation can be induced as effectively in females as males, with improvements in endurance [110,120,181] and intermittent sprint tasks [80] in both sexes, though data in elite female athletes remain scarce. The current literature suggests in order to ensure that appropriate magnitudes of adaptation take place, when working with female athletes, additional exposures should be considered to allow for any differences in temporal patterning be ameliorated in females. The use of additional thermal stress such as pre-HA warming or extended heat stress after or between HA as part of a multi-mixed/alternate model (e.g. sauna, hot water or prolonged maintenance phases of isothermic HA) may also be considered across the menstrual cycle/when amenorrhea is identified/around contraceptive use to improve the efficiency of HA.
How long do the adaptations last and how can they be retained?
An extensive overview of the retention, decay, and reinduction of heat adaptations has highlighted that in spite of a plethora of data describing the induction of thermoregulatory and performance physiology that follows HA, understanding of responses in the days and weeks following HA cessation is limited [16]. Indeed, data tracking the decay in athletic performance responses following HA are particularly limited. Consensus viewpoints highlight that once robust adaptations have been induced following MTHA/LTHA, that they are well retained, with similar physiological responses occurring 1 wk after the cessation of the HA training [108]. From this point onwards, heat adaptations reduce in magnitude unless an additional heat stimulus is an introduction. The typical rate of decay in adaptation has historically been described as “for every day of HA undertaken, the adaptation will be retained for two days” [184]. Accordingly, an athlete who undertakes 7 daily sessions of HA can expect to retain benefits for 14 d thereafter, though as with all physiological adaptations, a gradual decay rather than immediate withdrawal occurs. More recently, data examining fundamental HA adaptations, such as reduced TCORE and HR, alongside improved sweating capacity, have calculated that after STHA, a decay of 2.5% of adaptation made to TCORE and HR is lost daily thereafter [16]. This more recent analysis indicates that adaptations are retained effectively for some time after a dedicated HA intervention. Data examining the retention of passive HA decay is even more limited than that of exercise HA, however a recent study examining the retention of adaptations following post-exercise HWI suggests that the time course is similar to active HA and that reduced TCORE, HR and perceptual benefits are still present 2 wk following the final HA session [185]. With the team-sport athlete in mind, prolonged repeat-sprint exercise in the heat is improved after HA with performance well maintained over the subsequent 2 wk, despite removal of the heat stimulus [83]. One aspect of the research on decay of HA that complicates the issue is the training program following HA and how this influences the decay observed in key physiology. Essentially, research suggests low physical activity levels post-HA accelerate the loss of adaptation, but maintenance of high physical activity levels prolongs the adaptation; an artifact in the favor of the athlete [15] and a concept that could be further supported by having athletes overdress during training within a warm weather holding camp.
Given challenges of scheduling HA prior to competitions, we and others propose that individuals competing in the heat would benefit from undertaking a dedicated micro- or mesocycle of HA, well in advance of the competition, up to 4 wk prior. This could then be “topped up” with intermittent single or repeated HA sessions in the lead up to competition. Examples of this approach suggest it is possible to maintain thermoregulatory and performance physiology when individual heat exposures occur 5–7 d following an HA micro-cycle [186–188]. This concept mitigates the need to schedule prolonged HA immediately before competing i.e. within the taper [187]. It is also noteworthy that HA reinduction occurs at a faster rate following multiple cycles of HA [16,189,190]. This is advantageous to the athlete in two regards. First, an athlete may benefit from inducing the same magnitude of thermoregulatory and performance physiology adaption in a shorter duration (e.g. number of sessions) in subsequent cycles. Second, it could be decided that the athlete will undertake the same number of sessions in a subsequent cycle in order to elicit a greater adaptation. See Figure 5 for a suggested integration of HA into the final 16 wk of preparation prior to a major championship (e.g. Tokyo 2020 Olympic Games) with our proposed timeline avoiding the need to implement HA within the taper period.
Figure 5.
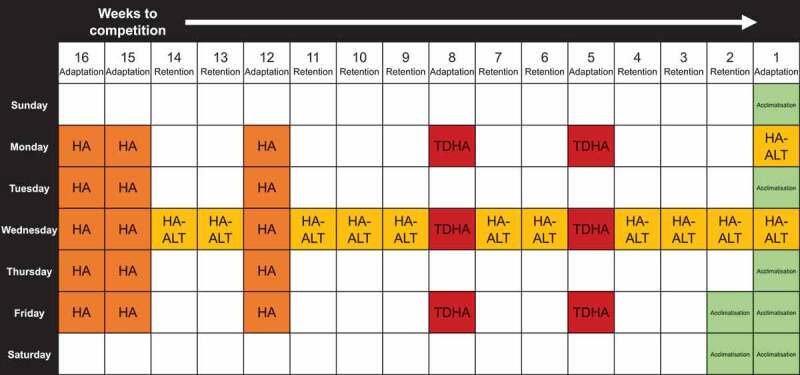
Proposed 16-wk chronic heat preparation approach which includes MTHA (ten 1-d HA sessions) commencing 16 wk prior to competition start, followed by STHA in the form of five 1-d HA (12 wk prior to competition start) and TDHA (8 and 5 wk prior to competition start). Weekly adaptation retention sessions using established exercise heat acclimation approaches e.g. isothermic method (HA) or alternative approaches (HA-ALT) e.g. over-dressing or post-exercise HWI/Sauna, punctuate these interventions. Days with no notation are regular training/recovery days. Athletes may consider implementing double sessions e.g. strength and conditioning or similar activity on acclimation days.
Are there hydration and nutritional considerations associated with HA?
The nutritional considerations for HA can be subdivided into fluid and macro/micronutrient considerations. From a fluid demand perspective, it has been proposed that permissively dehydrating (i.e. not drinking during HA sessions), may facilitate a greater magnitude of adaptation [191]. Despite data reporting that this may be evident during STHA [141], more recent data in both STHA/MTHA interventions highlight that irrespective of whether participants drink to retain body mass, or dehydrate intentionally during exercise-HA, the adaptive response is equivocal [106,113,192]. Rehydration following HA should include fluid and sodium given high sweat rates. It is recommended that isotonic beverages totalling 150% of the mass of fluid lost are consumed to replace the volume and composition of sweat lost more effectively [193].
Exercising in hot conditions has been reported to elevate substrate utilization in favor of glycolysis for a given activity [194], with HA subsequently reducing rates of glycolysis in favor of lipolysis at the same absolute intensity [195]. This is a result of the increased relative intensity of the task and is facilitated by elevated rates of glycolysis at submaximal intensities [196]. Accordingly, athletes, particularly those who are tightly regulating macronutrient intake, should seek to provide sufficient energy via this substrate during and after an HA session. Protein is also an important macronutrient to consider to aid adaptation, both given the established importance in supporting muscular recovery from exercise [197–199], but also given the mechanistic role of the plasma protein albumin in increasing plasma volume [114]. L-glutamine has also been implicated as an important amino acid in facilitating elevations in HSPs, and in maintaining gut function under heat stress [200–202]. These proteins have been evidenced as important in attenuating gastrointestinal (GI) permeability during heat stress which may improve symptoms of gastrointestinal distress [57,58], heat-related illness [59], and facilitating heat adaptation in general via HSPs [56]. Though proposed as beneficial, as yet, probiotic intake has not been evidenced as beneficial during repeated exercise in the heat [203]. The reader is directed to a recent comprehensive overview of the effects of nutrients on gastrointestinal distress in the heat for further information in this regard [204].
Considering the above, athletes may experience favorable adaptation and enhanced recovery from HA if they consume fluids containing both sodium and carbohydrate post-training [205], whilst also seeking to ingest L-glutamine rich protein following HA sessions [206]. Precise intakes for HA mediated benefits associated with protein/amino acid consumption are yet to be explored in a controlled research experiment, however the authors recommend adhering to guidelines allied to post-exercise recovery using nutritional protein [207].
Acute heat alleviation
The training volume associated with chronic heat training inevitably interferes with periodized training programs and has led to considerable research into heat-alleviating strategies that can be implemented on the day of performance. There are two predominant acute approaches to help combat this problem, pre-cooling, and per/mid-cooling. Pre-cooling targets the reduction of TSKIN and/or TCORE before the event begins, theoretically delaying the progressive, adverse effects of heat stress. Per/mid cooling may be used as a complementary, or independent strategy, which involves cooling during the event. In addition to a distinction for timing of cooling i.e. per/mid-cooling (referred to as mid-cooling hereafter), cooling studies are often further differentiated into internal or external cooling, depending upon where the cooling impulse is delivered. External cooling can be simplified as cooling the body from the “outside in”, predominantly through the lowering of TSKIN. Intuitively, internal cooling acts from the “inside out”, typically having been ingested prior too, or during competition.
The subsequent sections will discuss internal and external techniques in greater detail; however, some broad recommendations can be made irrespective of the strategy adopted. A number of reviews of cooling and athletic performance are now available [208–217], providing detailed discussions of mechanisms and likely performance benefits of different strategies. It is not within the scope of this review to examine each of these areas, therefore interested readers are directed to these significant citations. The focus of this section will be to summarize key findings and translate this information as key messages for practitioners who will support athletes competing in the heat.
Are there acute heat alleviation techniques that can be implemented on the day?
Despite the plethora of literature concerning pre/mid-cooling techniques, systematic interpretation is often hampered by divergence in experimental methodologies, notably concerning the timing that cooling occurs before the event, inclusion of representative warm-up, the type of exercise test implemented (i.e. open/closed loop, intensity, duration), heat strain experienced prior to cooling (both of which potentiate active and passive heat transfer), and a lack of true environmental simulation (e.g. representative air flow and solar/radiative heat exchange). Moreover, study findings may be impacted upon by the population used, with the participants’ biophysical and physiological profiles having direct influences on the magnitude of heat strain, for example, as a result of body size and/or mass [218], or fitness and therefore absolute energy expenditure [167,219]. Finally, whilst studies often report an absence of heat exposures preceding experimental trials, this does not ensure that these individuals are not partially heat acclimated, with fitter individuals often having a partial acclimation state, which may influence their response to acute interventions [165]. Thus, we recommend practitioners critically interpret study findings with regard to the potentially confounding variables highlighted above.
The mechanistic basis for elevated body temperature impairing sporting performance is multi-factorial [220], but the consequences may be crudely simplified to; reduced performance/thermoregulatory capacities, and feelings of extreme discomfort from the heat. Clearly such symptoms are interlinked, and it is intuitive therefore, that any acute heat alleviation intervention should consider addressing both of these elements, with two clear objectives, first, reduce body temperature or allow greater heat loss and second, ensure that the individual perceives themselves to be cooler/feel better immediately prior too, and during competition [208,221]. The effectiveness of pre-cooling is often a consequence of the degree of heat strain and magnitude of cooling. However, the importance of thermal comfort and sensation in determining athletic performance in the heat is now being realized [19,222,223], such that strategies which target only alleviated perceptual strain, for example menthol application or mouth rinsing, may elicit an ergogenic effect in some types of activity (e.g. during self-paced endurance exercise in untrained individuals [224]), but not other (e.g. intermittent sprint/team-sport activity [225]). It is pertinent however, to remind practitioners of the intuitive heat-related illness risk that may follow, from creating a dissociation between an individual’s TS and body temperature, and that excessive cooling may inhibit sweating and delay heat loss [226]. Together these comments reinforce our philosophy, that acute techniques should be well rehearsed and complementary to chronic heat alleviation, ideally in an event requiring utmost motivation to most closely reflect circumstances akin to the Tokyo 2020 Olympic Games. Given changes in perception of heat stress during competition [18], trialling thermoregulatory responses, with and without cooling during competitive preliminary events would be desirable.
What are external cooling techniques?
Principles of heat exchange determine that a greater amount of heat energy will be lost from the body when a large temperature gradient (i.e. difference) with an external material/environment exists and there is a large skin surface area (i.e. volume) for heat exchange to occur [227]. Thus, whole-body cold-water immersion (CWI) is considered the most effective external cooling method [228], reflecting the ability of cold water to contact with virtually all the skin, and water temperatures below 20°C providing a significant temperature gradient relative to typical TCORE (~36–40°C) and TSKIN (~28–37°C). CWI can be implemented either before an event or when an individual is already hot (i.e. between performance/exercise bouts). Typical protocols involve water of 15–25°C for a period of 10–20 min, with likely reductions in TSKIN in the region of 9°C, but may not elicit a visible reduction in TCORE within this duration [229,230]. A similar water temperature can be used for partial body water immersion, although a longer duration will be required to elicit the same magnitude of total body cooling.
Despite the proliferation of portable and inflatable ice-baths, water immersion still provides significant logistical challenges for implementation across many sporting environments. Water and ice supplies will be required to fill and maintain bath temperatures, whilst the athletes will be required to dry off, change, as well as warm-up prior to competing. Consequently, practical combinations of cold clothing and partial/localized body water immersion (e.g. just hands or feet) appear preferable for athletes [196,231–233]. When cold water is not available or feasible at events, other approaches such as cold, wet clothing/towels or ice packs can also lower body temperature, the effectiveness of which again will be determined by a combination of the temperature gradient, skin surface area coverage and cooling capacity [208]. Logically, research has identified both volume and duration-dependent relationships for pre-cooling strategies utilizing multiple garments [231,232], such that most research adopts “mixed-methods” cooling, targeting many body sites, with a cooling period of 20–30 min [208,210]. Cooling garments (e.g. ice-vest/cooling shorts) are typically applied frozen (0°C) and worn for over 20 min, similarly, cold/frozen/wet towels (0–20°C) which can be placed on the body (e.g. neck, back and torso [234–236]) until no longer cool. An applied cooling example, combining cooling techniques may include wet, iced towels (3°C) covering the head, neck and trapezius muscles, forearm and hand immersion in cold water (9°C), and an ice vest on the torso. On this point, the authors note that practitioners may wish to trial/avoid cooling-specific areas of the body in a sport-dependent manner, such as in sports requiring dexterity of hands (e.g. field hockey, rugby, sailing, rowing) and/or optimized lower limb major muscle group temperature (e.g. most team-sports) as cooling these regions may be counter-productive. Consideration may also be given to cooling areas that heavily influence TS and comfort, due to the distribution of localized thermoreceptor (e.g. found in the hands and face), which theoretically will help to attenuate or delay subsequent behavioral thermoregulation arising from perceived discomfort [223]. Purpose-made cooling garments, such as ice-vests or ice shorts are now available, though cooling shorts can also be improvised using ice packs or bags of ice and temporary bandages or cling film [237]. Indeed, loosely bagged ice is commonly seen attached to the limbs, neck, back, and torso or axilla in many sporting situations for recovery purposes, this same approach can be applied prior to competition.
Compared with internal cooling, external cooling will not always demonstrate a reduction in pre-exercise TCORE, especially when delivered to a static individual [196,231]. However, an “after-drop” may occur following external cooling, whereby TCORE falls following the onset of exercise as vasoconstriction reduces and warm blood is subsequently cooled in the periphery [238]. TSKIN may be lowered by 7°C when weighted averages from the chest, upper arm, quadriceps, and calf are used to estimate mean TSKIN [196,239]. It is this systematic reduction in peripheral TSKIN, thereby enhancing the TCORE:TSKIN gradient [240] and likely reducing the cutaneous blood flow demand [241], that in turn mediates cardiovascular strain [242] and underpins the physiological alleviation afforded by external cooling. Furthermore, there is evidence that external cooling maintains improved thermal sensation for longer, compared with internal cooling [196]. In summary, in addition to meaningful reductions in TSKIN, the benefits of external cooling are such that it can be easily adapted for different individuals or sports, requiring only cooling garments to be frozen at the team hotel or athletes’ village and then transported in ice boxes to the event; transit time is therefore a relevant consideration for the practitioner to ensure the efficacy of this technique.
Internal cooling
Principles of heat exchange determine that a larger transfer of heat energy is required to complete the phase change of ice into water, than to heat cold water. Thus, ingesting ice is preferable to ingesting liquids, because an equivalent cooling magnitude can be delivered from a smaller absolute dosage. Whilst colder drinks provide a greater temperature gradient and cooling effect, the optimal drink temperature may ultimately be determined by the individual. Athletes should seek to consume cold drinks (5–15°C) ad libitum, and if well tolerated, ice-slurry drinks (0°C). The benefits of cold water and ice-slurry ingestion can be summarized into directly cooling of core organs and circulating blood, enhanced thermal sensation through thermoreceptors in the mouth and gut, and can be complementary to existing pre-event hydration or nutrition supplementation strategies (e.g. combine with CHO and minerals) [196,208]. The use of internal cooling is not without risk and rehearsal of techniques should be trialled in event simulations to determine erogenicity at an individual level and understand whether gastrointestinal or elevated urination issues may occur. Mechanistically, the thermal stimulus to elicit a phase change from ice to water draws heat from internal tissue, reducing temperatures proximal to the gut directly and indirectly cools other regions, as blood of a lower temperature circulates the body. Therefore, unlike external cooling, internal cooling often displays minimal changes in TSKIN, but prompt changes in TCORE, reflecting the cooling site proximity to core organs and typical TCORE measurements in the gut (e.g. pill) or rectum (e.g. thermistor probe). Cooling via the mouth and gut may also positively influence indices of perceived thermal strain (i.e. thermal comfort and sensation), as a consequence of the relative prominence of thermoreceptors in these regions [243,244]. The systemic nature of cooling the periphery through the blood stream however does not lead to the same concerns around localized external cooling, with the maintenance of dexterity and muscle temperature.
Ice ingestion alone enhances the likelihood of sphenopalatine ganglioneuralgia (“brain freeze”) and carries a choking risk, therefore a mixture of liquid and crushed ice (i.e. slurry/slushy) is more suitable. A typical ice slurry drink may elicit a 0.2–0.6°C reduction in TCORE, when ingested over 20 min [196,230,245,246]. Despite the large reduction in TCORE, evidence exists that ice-slurry ingestion will likely inhibit with the sudomotor response, resulting in reduced evaporative heat loss [230,247,248]. This leads to increased heat storage during the initial phase of exercise, which may help explain the elevated finishing TCORE that has been observed following ice-slurry ingestion [230]. Despite this observation, ice-slurry ingestion is likely to benefit exercise performance in the heat particularly when environmental conditions or protective equipment (e.g. hockey goalkeeper) limit evaporative heat loss potential [249] and given reported reductions in brain temperature, cognition, and decision-making may also be improved [250].
Notwithstanding the benefits of internal cooling, questions remain concerning the optimal quantity and ingestion time before performance. A balance must be found between delivering a large cooling impulse (typically in the region of ~500–700 mL) and athlete comfort, ensuring feelings of being bloated and gastrointestinal complaints are avoided [246]. To this effect, it is recommended that smaller doses made relative to the athlete’s body mass (7.5 g.kg−1BM = e.g. 525 g (or 525 mL) for a 70 kg individual) are used. Spreading this out in small doses (1.25 g.kg−1BM per 5 min = e.g. 100 g (or 100 mL) for a 70 kg individual), rather than drinking a single bolus, appears to offer greater cooling and is likely to be better tolerated by athletes [251].
What practical cooling guidelines should I follow?
As with all competition day strategies, cooling must be meticulously planned and practiced from both athlete and practitioner perspectives. Anecdotally, athletes take time to identify a preferred pacing strategy within endurance events, not always utilizing the apparent alleviated physiological strain [20,21] and find the transition from cool to “very hot” is expedited when pre-cooled, challenging planned pacing strategies. Whilst “more is better” may be a pertinent cooling mantra, some are also better than none. Athletes and practitioners should therefore not discount apparently less effective cooling techniques, if these are easily integrated with other preparation priorities and are easy to use (e.g. ice-vests and/or electric fans).
Cooling strategies often require electrical power in the field, a local ice supply and/or effective storage of cooling devices, all of which should be discussed with event organizers prior to travel. It is also important for practitioners to note that 24 h supervision of ice slurry machines may be necessary to avoid contamination and robust hygiene protocols are required. We also emphasize that heat stress does not only affect the performance but also affects the rest of pre and post-competition routines. For example, increased sweat loss whilst traveling to the venue should be expected, as well as greater perceived exertion from activation and/or warm-up activities. Therefore, whilst this review focusses on competitive performance, athletes may also wish to utilize simple cooling methods, such as cold drinks, handheld electric fans and/or mist sprays throughout the day. Whilst such cooling practices may offer limited physiological impact during the performance, they are likely to maintain feelings of comfort and relaxation prior to the event, especially if the individual has to spend prolonged periods outside waiting where air conditioning is not available.
Guiding principles to be mindful of when implementing acute heat alleviation strategies include; 1) covering as much of the body (i.e. skin) surface area as possible and doing so as close to the performance as possible, and 2) practicing the routine in its entirety, including warm-up and event simulation from both athlete and practitioner perspectives. Pre-cooling is not going to remove thermal sensation as athletes will still feel hot after 10–15 min throughout most competitions, but these will likely be less than would otherwise have been the case. It is important to acknowledge that some individuals find the transition from feeling “cold” to “very hot” occurs quickly and they should familiarize to this. It is not advisable to neglect an effective technical, skill-based warm-up in lieu of staying cool, as there are a range of other beneficial consequences from a proper warm-up. Finally, 3) the athlete and practitioner should beware of “evaporative cooling” garments and not solely rely on these. Garments of this nature utilize moisture to enhance natural heat loss (via sweat evaporation), but do not deliver a cooling impulse as a phase-change/ice cooling product will, and the efficiency of these aids will be considerably reduced in humid climates that impair sweat evaporation.
Example pre-cooling approaches include implementing external cooling only, via 20 min of cold water immersion (10–20°C) in an inflatable pool, finishing just before the warm-up, or implementing internal cooling only via ice-slurry drinks (~500 mL) between arrival at venue and during warm-up (100 mL every 5 min). Superior to these approaches is the implementation of combined cooling approaches involving pre-travel CWI (20 min), upon arrival 20 min wearing ice-vest, cooling shorts, cold wet towels around head and neck, finishing just before warm-up. Many athletes, across multiple sports, can wear an ice-vest during warm-up and then use electric fans and drink an ice-slurry (containing CHO, electrolytes, and caffeine) post warm-up, until their event starts. The implementation of combined approaches is often dictated by the environment, as such a more pragmatic combined cooling would involve a ~500 mL ice-slurry drink prior to arrival at venue followed by a complete warm-up wearing ice-vest, neck cooling collar, cooling wrist wraps. Figure 6 provides a suggested pre- and mid-cooling schematic to be implemented in the buildup to and during a team-sport (field hockey) fixture.
Figure 6.
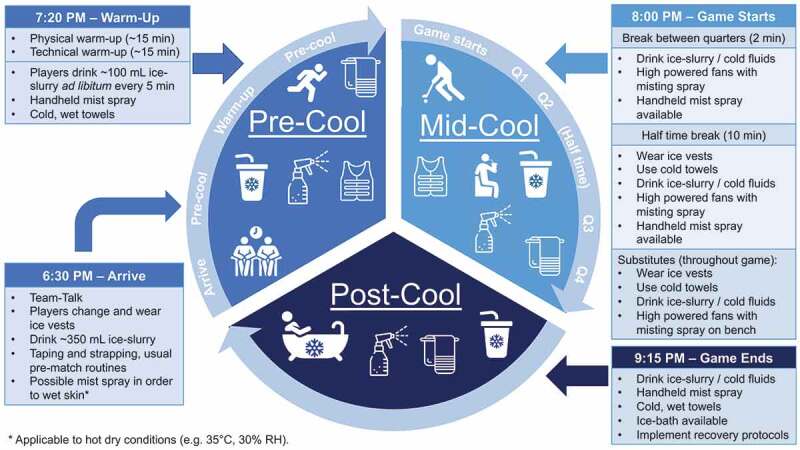
Practical cooling strategies for use before and during a field hockey game. Note. Field hockey permits unlimited substitutions, so cooling strategies can be implemented throughout the game.
Can cooling be used effectively mid-event?
There is strong evidence that cooling during exercise in the heat (mid-cooling or per-cooling) will elicit beneficial performance effects [211] and can be used additively with pre-cooling [214]. Mid-cooling techniques are directly informed by pre-cooling techniques and the similar importance of cooling magnitude (i.e. temperatures, duration and surface area), as well as alleviated perceptual strain should be noted, to benefit performance [210,211]. However, sporting regulations and/or practicalities associated with movement will ultimately determine how sport-specific strategies are implemented. In long-distance events, the most prevalent mid-cooling strategies are reliant upon the event organizer (e.g. feed stations/mist sprays) and/or team members (e.g. domestiques/staff members lining the route). Any benefits afforded by wearing additional cooling garments or carrying additional cold drinks may be offset by increased weight. Thus, simple recommendations include using cold water sprays, sipping, or pouring a cold drink [252], cold/wet/frozen towels or bags of ice. Whilst such techniques may be less effective for pre-cooling, during exercise the thermal strain is greater, with a likely greater perceived benefit from localized (otherwise underpowered) cooling, if they alleviate thermal discomfort [208,214]. For sports that have short breaks in play, such as team-sports (e.g. hockey), industrial fans with mist sprays are probably the simplest method of providing effective cooling to a large number of athletes in a short period of time. As with pre-cooling, the use of cooling vests [253] and vests/jackets with gloves [254], may also be considered during breaks in play (e.g. half time). To summarize, practitioners should consider a “toolbox”, containing ice-slurry/cool drinks in thermos flasks, ice packs, ice cubes (loose or wrapped in towels to form a cooling cylinder), with replacement clothing cooling inside the box to fit the individual needs of the athlete.
Combined chronic and acute heat alleviation strategies
Can we combine and conquer?
The benefit of combining chronic and acute heat alleviation interventions is yet to be convincingly demonstrated experimentally. In two studies utilizing intermittent sprint protocols, HA alone was sufficient to negate the effect of heat strain, leaving pre-cooling unnecessary [79,92]. Pre-cooling typically elicits larger effects on endurance performance, compared with intermittent sprinting [210]. The two studies to combine techniques in endurance performance revealed encouraging findings, although no performance advantage. Utilizing an ice-vest prior to a 20 km cycling time trial, following 10 d of acclimatization did not improve overall performance above acclimatization alone, although transient, beneficial pacing alterations were observed until the dissipation of pre-cooling effects indicating a more aggressive cooling approach may prolong this effect [20]. Implementing a 20 min mixed-method external pre-cooling following 5 d of STHA, afforded large differences in TCORE, TSKIN, TCORE:TSKIN gradient, TS and HR during the first half of a 5 km running trial, but without any change in initial self-selected running speed [21]. This alludes to a sub-optimal “flat” pacing strategy, which appears to prevail when individuals familiarize to exercising in the heat [242]. Thus, whilst an insensitivity or “ceiling effect” following HA has been proposed [79], when an aggressive pre-cooling technique is adopted and heat strain remains severe, these data indicate small, meaningful changes, notably in HR and TSKIN, that have the potential to benefit performance. Therefore, further familiarization to combined chronic and acute heat alleviation interventions appears necessary to ensure pacing and performance are optimized at an individual level.
Summary
To prepare for elite international competition, quality training, individualized nutrition, and appropriate recovery will always be fundamental. Events such as the Tokyo 2020 Olympics also require athletes to prepare for the demands of the climate in a manner that does not unduly impact or detract from these factors. Whilst it is optimistic, unrealistic even, to envisage all of the potential detriments associated with performing under heat stress can be ameliorated, well-structured, individualized heat alleviation strategies have the potential to moderate the thermal challenge. Key messages arising from this review include:
HA provides a robust opportunity to improve thermoregulatory and performance physiology, alongside thermal perception, for athletes who are likely to be impacted by the predicted climate.
Athletes may utilize a singular or combined method HA strategy that includes exercise-heat stress and/or post-exercise heat stress e.g. hot water/sauna, to fit individual needs and circumstances.
Once- or twice-daily HA sessions of 30–90 min may be used to optimize the magnitudes of adaptation in a manner that compliments training.
Athletes should “prepare for the worst” by preparing to perform in environments equal too or greater than maximum anticipated climatic conditions including radiative (solar) heat.
Female athletes, or those who are lesser trained (irrespective of sex), may require additional exposures than males, or those who are more aerobically trained to achieve optimal magnitudes of adaptation.
Female athletes should be familiarized to exercising at performance intensities under anticipated heat stress across the menstrual cycle.
Structured HA may be performed weeks prior to the competition, with subsequent “top-up” sessions implemented closer to individual events.
Athletes should rehydrate post HA and will benefit from carbohydrate and protein consumption to aid recovery and adaptation.
Acute heat alleviation such as pre- and mid-event cooling should compliment chronic HA strategies.
Acute strategies should be individualized, and well rehearsed prior to competition to optimize responses.
Biographies
Dr Oliver R. Gibson Oli is a researcher within the Centre for Human Performance, Exercise and Rehabilitation (CHPER) and a Lecturer in Exercise Physiology within the Division of Sport, Health and Exercise Sciences at Brunel University London. Oli’s research and consultancy falls predominantly in the field of Exercise and Environmental Physiology with a particular focus on acute and chronic responses to heat and/or hypoxic stress, and subsequent sporting or clinical/health applications. Oli’s research also examines cross adaptation between environmental stressors, and the role of heat shock proteins in thermal adaptation. Twitter - @iamolivergibson

Dr Carl A. James Carl is a Senior Physiologist at the National Sports Institute of Malaysia, working with the Malaysian national field hockey team. Carl received his PhD from the University of Brighton, where he investigated acute and chronic interventions to aid endurance performance in the hot andhumid conditions, including; precooling, ischemic preconditioning and heat acclimation. Dr James is also a BASES accredited physiologist and holds both a master’s degree (MSc) and bachelor’s degree (BSc Hons), from Sheffield Hallam University and Bangor University, respectively. Twitter @Tohelandback

Dr Jessica A. Mee Jessica is a Lecturer in Sport and Exercise Science at the University of Worcester. Before joining the University in 2019, she held a researcher and lecturer post at Bangor University following the completion of her PhD at the University of Brighton. Jessica is an Applied Sport Scientist who has research interests aligned to optimising athlete and occupational workers (including military personnel) for competing and working in hot climates using novel, accessible and effective strategies. She has a particular interest in understanding the additional challenges female endurance athletes may face associated with hormonal fluctuations during the menstrual cycle. Twitter - @JessicaAnneMee

Dr Ashley G.B. Willmott Ash joined the Cambridge Centre for Sport and Exercise Sciences at Anglia Ruskin University (ARU) as a lecturer in 2019. Ash specialises in the sensitivity and adaptation to extreme environmental conditions, specifically heat stress. He has undertaken many studies involving the acute and chronic heat alleviation strategies, which have translated into support for elite level endurance athletes. Alongside his research and consultancy, Ash is a BASES accredited physiologist, a trustee for an altitude awareness charity (Para-Monte), and also works alongside business partners to assess the efficacy of portable medical cooling products to prevent the severity of heat illness. Twitter - @AshWillmott

Dr Gareth Turner Gareth is a physiologist for the Great Britain Rowing Team having previously worked for British Athletics supporting endurance athletes. Gareth provides support to Team GB athletes in the UK and on training camps across the world where environmental conditions (altitude, heat) have been used as an additional stimulus for adaptation prior to international competition, particularly prior to travel to locations where the climate is a major challenge. Twitter - @1GTurner

Dr Mark Hayes Mark is a Senior Lecturer in Sport and Exercise Science at the University of Brighton working in the field of Exercise and Environmental Physiology within the Sport and Exercise Science and Sports Medicine Research and Enterprise Group. Mark’s research interests centre on understanding human tolerance to environmental extremes with a particular interest in the physiological responses to heat, cold and hypoxic stress from a performance, occupational and health perspective. Mark has consulted with a number of teams e.g. England Rugby and GB Hockey, prior to international competition.

Dr Neil S. Maxwell Dr Neil Maxwell is a Reader of Environmental Physiology within the School of Sport and Service Management at the University of Brighton. Through his research and innovation, Neil aims to inspire health, occupational and sporting communities to engage in safe and effective exercise in environmental extremes and reduce the incidence of illness. Neil leads the Environmental Extremes Laboratory, where his research focus is towards heat sensitivity during exercise and evaluating practical heat alleviation methods (e.g. heat acclimation, pre and per cooling and hydration manoeuvres) across sport, occupational, health and clinical populations. In the altitude domain, Neil researches susceptibility to altitude and effective screening measures while working with and a trustee for the charity, Para-Monte to raise awareness about altitude illnesses. Twitter - @UoB_EEL

Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Guy JH, Deakin GB, Edwards AM, et al. Adaptation to hot environmental conditions: an exploration of the performance basis, procedures and future directions to optimise opportunities for elite athletes. Sports Med. 2014;45:303–311. [DOI] [PubMed] [Google Scholar]
- [2].Nassis GP, Brito J, Dvorak J, et al. The association of environmental heat stress with performance: analysis of the 2014 FIFA world cup Brazil. Br J Sports Med. 2015;49:609–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Sunderland C, Nevill ME.. High-intensity intermittent running and field hockey skill performance in the heat. J Sports Sci. 2005;23:531–540. [DOI] [PubMed] [Google Scholar]
- [4].Griggs KE, Price MJ, Goosey-Tolfrey VL. Cooling athletes with a spinal cord injury. Sports Med. 2015;45:9–21. [DOI] [PubMed] [Google Scholar]
- [5].Price MJ. Thermoregulation during exercise in individuals with spinal cord injuries. Sports Med. 2006;36:863–879. [DOI] [PubMed] [Google Scholar]
- [6].Price MJ. Preparation of paralympic athletes; environmental concerns and heat acclimation. Front Physiol. 2016;6:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Griggs KE, Stephenson BT, Price MJ, et al. Heat-related issues and practical applications for paralympic athletes at Tokyo 2020. Temperature. 2019:1–21. doi: 10.1080/23328940.2019.1617030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Mercer J. Glossary of terms for thermal physiology. Third edition. Revised by the commission for thermal physiology of the International Union of Physiological Sciences (IUPS thermal commission). Jap J Physiol. 2001;51:245–280. [PubMed] [Google Scholar]
- [9].Périard JD, Racinais S, Timpka T, et al. Strategies and factors associated with preparing for competing in the heat : a cohort study at the 2015 IAAF world athletics championships. Br J Sports Med. 2017;51:264–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Corbett J, Rendell RA, Massey HC, et al. Inter-individual variation in the adaptive response to heat acclimation. J Therm Biol. 2018;74:29–36. [DOI] [PubMed] [Google Scholar]
- [11].Gore CJ, Sharpe K, Garvican-Lewis LA, et al. Altitude training and haemoglobin mass from the optimised carbon monoxide rebreathing method determined by a meta-analysis. Br J Sports Med. 2013;47(Suppl 1):i31–i39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Wehrlin JP, Hallén J. Linear decrease in VO2max and performance with increasing altitude in endurance athletes. Eur J Appl Physiol. 2006;96:404–412. [DOI] [PubMed] [Google Scholar]
- [13].Ely MR, Cheuvront SN, Roberts WO, et al. Impact of weather on marathon-running performance. Med Sci Sports Exercise. 2007;39:487–493. [DOI] [PubMed] [Google Scholar]
- [14].Tyler CJ, Reeve T, Hodges GJ, et al. The effects of heat adaptation on physiology, perception and exercise performance in the heat: a meta-analysis. Sports Med. 2016;46:1699–1724. [DOI] [PubMed] [Google Scholar]
- [15].Pryor JL, Johnson EC, Roberts WO, et al. Application of evidence-based recommendations for heat acclimation: individual and team sport perspectives. Temperature. 2018;6:37–49. doi: 10.1080/23328940.2018.1516537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Daanen HAM, Racinais S, Périard JD. Heat acclimation decay and re-induction: a systematic review and meta-analysis. Sport Med. 2017;48:409–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Barwood MJ, Kupusarevic J, Goodall S. Repeated menthol spray application enhances exercise capacity in the heat. Int J Sports Physiol Perform. 2019;14:644–649. [DOI] [PubMed] [Google Scholar]
- [18].Corbett J, White DK, Barwood MJ, et al. The effect of head-to-head competition on behavioural thermoregulation, thermophysiological strain and performance during exercise in the heat. Sport Med. 2018;48:1269–1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].James CA, Hayes M, Willmott AGB, et al. Defining the determinants of endurance running performance in the heat. Temperature. 2017;4:314–329. doi: 10.1080/23328940.2017.1333189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Schmit C, Le Meur Y, Duffield R, et al. Heat-acclimatization and pre-cooling: a further boost for endurance performance? Scand. J Med Sci Sports. 2017;27:55–65. [DOI] [PubMed] [Google Scholar]
- [21].James CA, Richardson AJ, Willmott AG, et al. Short-term heat acclimation and precooling, independently and combined, improve 5 km running performance in the heat. J Strength Cond Res. 2018;32:1366–1375. [DOI] [PubMed] [Google Scholar]
- [22].Casadio JR, Kilding AE, Cotter JD, et al. From lab to real world: heat acclimation considerations for elite athletes. Sports Med. 2016;47:1467–1476. [DOI] [PubMed] [Google Scholar]
- [23].Garrett AT, Rehrer NJ, Patterson MJ. Induction and decay of short-term heat acclimation in moderately and highly trained athletes. Sport Med. 2011;41:757–771. [DOI] [PubMed] [Google Scholar]
- [24].Trangmar SJ, González-Alonso J. Heat, hydration and the human brain, heart and skeletal muscles. Sport Med. 2019;49:69–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Periard JD, Travers G, Racinais S, et al. Cardiovascular adaptations supporting human exercise-heat acclimation. Auton Neurosci. 2016;196:52–62. [DOI] [PubMed] [Google Scholar]
- [26].Taylor NA . Human heat adaptation. Compr Physiol. 2014;4:325–365. [DOI] [PubMed] [Google Scholar]
- [27].Sawka MN, Leon LR, Montain SJ, et al. Integrated physiological mechanisms of exercise performance, adaptation, and maladaptation to heat stress. Compr Physiol. 2011;1:1883–1928. [DOI] [PubMed] [Google Scholar]
- [28].Lei T-H, Mündel T. Humid heat stress affects trained female athletes more than does their menstrual phase. Temperature. 2018;5:202–204. doi: 10.1080/23328940.2018.1436394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Gibson OR, Taylor L, Watt PW, et al. Cross adaptation – heat and cold adaptation to improve physiological and cellular responses to hypoxia. Sports Med. 2017;47:1751–1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Corbett J, Neal RA, Lunt HC, et al. Adaptation to heat and exercise performance under cooler conditions: a new hot topic. Sports Med. 2014;44:1323–1331. [DOI] [PubMed] [Google Scholar]
- [31].Cramer MN, Jay O. Biophysical aspects of human thermoregulation during heat stress. Auton Neurosci. 2016;196:3–13. [DOI] [PubMed] [Google Scholar]
- [32].Buono MJ, Heaney JH, Canine KM. Acclimation to humid heat lowers resting core temperature. Am J Physiol. 1998;274:R1295–9. [DOI] [PubMed] [Google Scholar]
- [33].FDC M, Passos RLF, Fonseca MA, et al. Thermoregulatory efficiency is increased after heat acclimation in tropical natives. J Physiol Anthropol. 2010;29:1–12. [DOI] [PubMed] [Google Scholar]
- [34].Cotter JD, Patterson MJ, Taylor NA. Sweat distribution before and after repeated heat exposure. Eur J Appl Physiol Occup Physiol. 1997;76:181–186. [DOI] [PubMed] [Google Scholar]
- [35].Patterson MJ, Stocks JM, Taylor NAS. Humid heat acclimation does not elicit a preferential sweat redistribution toward the limbs. Am J Physiol Regul Integr Comp Physiol. 2004;286:R512–R518. [DOI] [PubMed] [Google Scholar]
- [36].Lorenzo S, Minson CT. Heat acclimation improves cutaneous vascular function and sweating in trained cyclists. J Appl Physiol. 2010;109:1736–1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Chinevere TD, Kenefick RW, Cheuvront SN, et al. Effect of heat acclimation on sweat minerals. Med Sci Sports Exercise. 2008;40:886–891. [DOI] [PubMed] [Google Scholar]
- [38].Sato F, Owen M, Matthes R, et al. Functional and morphological changes in the eccrine sweat gland with heat acclimation. J Appl Physiol. 1990;69:232–236. [DOI] [PubMed] [Google Scholar]
- [39].Kenefick RW, Cheuvront SN, Palombo LJ, et al. Skin temperature modifies the impact of hypohydration on aerobic performance. J Appl Physiol. 2010;109:79–86. [DOI] [PubMed] [Google Scholar]
- [40].González-Alonso J, Mora-Rodríguez R, Coyle EF. Stroke volume during exercise: interaction of environment and hydration. Am J Physiol Heart Circ Physiol. 2000;278:H321–30. [DOI] [PubMed] [Google Scholar]
- [41].Patterson MJ, Stocks JM, Taylor NAS. Whole-body fluid distribution in humans during dehydration and recovery, before and after humid-heat acclimation induced using controlled hyperthermia. Acta Physiol (Oxf). 2014;210:899–912. [DOI] [PubMed] [Google Scholar]
- [42].Greenleaf JE, Brock PJ, Keil LC, et al. Drinking and water balance during exercise and heat acclimation. J Appl Physiol. 1983;54:414–419. [DOI] [PubMed] [Google Scholar]
- [43].Eichna LW, Bean WB, Ashe WF, et al. Performance in relation to environmental temperature. Reactions of normal young men to hot, humid (simulated jungle) environment. Bull Johns Hopkins Hosp. 1945;76:25–58. [Google Scholar]
- [44].Funnell MP, Mears SA, Bergin-Taylor K, et al. Blinded and unblinded hypohydration similarly impair cycling time trial performance in the heat in trained cyclists. J Appl Physiol. 2019;126:870–879. [DOI] [PubMed] [Google Scholar]
- [45].Cheung SS, McGarr GW, Mallette MM, et al. Separate and combined effects of dehydration and thirst sensation on exercise performance in the heat. Scand J Med Sci Sports. 2015;25:104–111. [DOI] [PubMed] [Google Scholar]
- [46].Garrett AT, Goosens NG, Rehrer NJ, et al. Induction and decay of short-term heat acclimation. Eur J Appl Physiol. 2009;107:659–670. [DOI] [PubMed] [Google Scholar]
- [47].Nielsen B, Hales JR, Strange S, et al. Human circulatory and thermoregulatory adaptations with heat acclimation and exercise in a hot, dry environment. J Physiol. 1993. January 01; 460:467–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Lorenzo S, Halliwill JR, Sawka MN, et al. Heat acclimation improves exercise performance. J Appl Physiol. 2010;109:1140–1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Petersen CCJ, Portus MMR, Pyne DB, et al. Partial heat acclimation in cricketers using a 4-day high intensity cycling protocol. Int J Sports Physiol Perform. 2010;5:535–545. [DOI] [PubMed] [Google Scholar]
- [50].Gibson OR, Mee JA, Tuttle JA, et al. Isothermic and fixed intensity heat acclimation methods induce similar heat adaptation following short and long-term timescales. J Therm Biol. 2015;49–50:55–65. [DOI] [PubMed] [Google Scholar]
- [51].Kelly M, Gastin PB, Dwyer DB, et al. Short duration heat acclimation in Australian football players. J Sports Sci Med. 2016;15:118–125. [PMC free article] [PubMed] [Google Scholar]
- [52].Wingfield GL, Gale R, Minett GM, et al. The effect of high versus low intensity heat acclimation on performance and neuromuscular responses. J Therm Biol. 2016;58:50–59. [DOI] [PubMed] [Google Scholar]
- [53].Willmott AGB, James CA, Hayes M, et al. Heat acclimation attenuates the increased sensations of fatigue reported during acute exercise-heat stress. Temperature. 2019. doi: 10.1080/23328940.2019.1664370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Febbraio MA, Snow RJ, Hargreaves M, et al. Muscle metabolism during exercise and heat stress in trained men: effect of acclimation. J Appl Physiol. 1994;76:589–597. [DOI] [PubMed] [Google Scholar]
- [55].Racinais S, Wilson MG, Périard JD. Passive heat acclimation improves skeletal muscle contractility in humans. Am J Physiol Regul Integr Comp Physiol. 2017;312:R101–R107. [DOI] [PubMed] [Google Scholar]
- [56].Kuennen M, Gillum T, Dokladny K, et al. Thermotolerance and heat acclimation may share a common mechanism in humans. Am J Physiol Regul Integr Comp Physiol. 2011;301:R524–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Pugh JN, Kirk B, Fearn R, et al. Prevalence, severity and potential nutritional causes of gastrointestinal symptoms during a marathon in recreational runners. Nutrients. 2018;10:811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Pugh JN, Sage S, Hutson M, et al. Glutamine supplementation reduces markers of intestinal permeability during running in the heat in a dose-dependent manner. Eur J Appl Physiol. 2017;117:2569–2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Leon LR, Helwig BG. Heat stroke: role of the systemic inflammatory response. J Appl Physiol. 2010;109:1980–1988. [DOI] [PubMed] [Google Scholar]
- [60].Willmott AGB, Hayes M, James CA, et al. Once- and twice-daily heat acclimation confer similar heat adaptations, inflammatory responses and exercise tolerance improvements. Physiol Rep. 2018;6:e13936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Willmott AGB, Hayes M, Waldock KAM, et al. Short-term heat acclimation prior to a multi-day desert ultra-marathon improves physiological and psychological responses without compromising immune status. J Sports Sci. 2016;00:1–8. [DOI] [PubMed] [Google Scholar]
- [62].Costello JT, Rendell RA, Furber M, et al. Effects of acute or chronic heat exposure, exercise and dehydration on plasma cortisol, IL-6 and CRP levels in trained males. Cytokine. 2018;110:277–283. [DOI] [PubMed] [Google Scholar]
- [63].Guy J, Pyne DB, Deakin G, et al. Acclimation training improves endurance cycling performance in the heat without inducing endotoxemia. Front Physiol. 2016;7:318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].James CA, Richardson AJ, Watt PW, et al. Short-term heat acclimation improves the determinants of endurance performance and 5-km running performance in the heat. Appl Physiol Nutr Metab. 2017;42:285-294. [DOI] [PubMed] [Google Scholar]
- [65].Nadel ER, Pandolf KB, Roberts MF, et al. Mechanisms of thermal acclimation to exercise and heat. J Appl Physiol. 1974;37:515–520. [DOI] [PubMed] [Google Scholar]
- [66].Sawka MN, Young AJ, Cadarette BS, et al. Influence of heat stress and acclimation on maximal aerobic power. Eur J Appl Physiol Occup Physiol. 1985. January 01; 53:294–298. [DOI] [PubMed] [Google Scholar]
- [67].Pivarnik JM, Goetting MP, Senay LC. The effect of endurance training and heat acclimation on aerobic capacity blood volume and plasma testosterone. J Appl Sport Sci Res. 1987;1:33–35. [Google Scholar]
- [68].Lorenzo S, Minson CT, Babb TG, et al. Lactate threshold predicting time-trial performance: impact of heat and acclimation. J Appl Physiol. 2011;111:221–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Pandolf KB, Cadarette BS, Sawka MN, et al. Thermoregulatory responses of middle-aged and young men during dry-heat acclimation. J Appl Physiol. 1988;65:65–71. [DOI] [PubMed] [Google Scholar]
- [70].Yamada PM, Amorim FT, Moseley P, et al. Effect of heat acclimation on heat shock protein 72 and interleukin-10 in humans. J Appl Physiol. 2007;103:1196–1204. [DOI] [PubMed] [Google Scholar]
- [71].Chen T-I, Tsai P-H, Lin J-H, et al. Effect of short-term heat acclimation on endurance time and skin blood flow in trained athletes. Open Access J Sport Med. 2013;4:161–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Burk A, Timpmann S, Kreegipuu K, et al. Effects of heat acclimation on endurance capacity and prolactin response to exercise in the heat. Eur J Appl Physiol. 2012;112:4091–4101. [DOI] [PubMed] [Google Scholar]
- [73].Garrett AT, Creasy R, Rehrer NJ, et al. Effectiveness of short-term heat acclimation for highly trained athletes. Eur J Appl Physiol. 2012;112:1827–1837. [DOI] [PubMed] [Google Scholar]
- [74].Kenefick RW, Cheuvront SN, Elliott LD, et al. Biological and analytical variation of the human sweating response: implications for study design and analysis. Am J Physiol Integr Comp Physiol. 2012;302:R252–R258. [DOI] [PubMed] [Google Scholar]
- [75].Cheung SS, McLellan TM. Heat acclimation, aerobic fitness, and hydration effects on tolerance during uncompensable heat stress. J Appl Physiol. 1998. June 06; 84:1731–1739. [DOI] [PubMed] [Google Scholar]
- [76].Maher JT, Bass DE, Heistad DD, et al. Effect of posture on heat acclimatization in man. J Appl Physiol. 1972;33:8–13. [DOI] [PubMed] [Google Scholar]
- [77].Nielsen B, Strange S, Christensen NJ, et al. Acute and adaptive responses in humans to exercise in a warm, humid environment. Pflugers Arch. 1997;434:49–56. [DOI] [PubMed] [Google Scholar]
- [78].Racinais S, Périard JD, Karlsen A, et al. Effect of heat and heat-acclimatization on cycling time-trial performance and pacing. Med Sci Sports Exercise. 2015;47:601–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Castle P, Mackenzie RW, Maxwell N, et al. Heat acclimation improves intermittent sprinting in the heat but additional pre-cooling offers no further ergogenic effect. J Sports Sci. 2011;29:1125–1134. [DOI] [PubMed] [Google Scholar]
- [80].Sunderland C, Morris JG, Nevill ME. A heat acclimation protocol for team sports. Br J Sports Med. 2008;42:327–333. [DOI] [PubMed] [Google Scholar]
- [81].Buchheit M, Racinais S, Bilsborough J, et al. Adding heat to the live-high train-low altitude model: a practical insight from professional football. Br J Sports Med. 2013;47:i59–i69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Pethick WA, Murray HJ, McFadyen P, et al. Effects of hydration status during heat acclimation on plasma volume and performance. Scand J Med Sci Sports. 2019;29:189–199. [DOI] [PubMed] [Google Scholar]
- [83].Duvnjak-Zaknich DM, Wallman KE, Dawson BT, et al. Continuous and intermittent heat acclimation and decay in team sport athletes. Eur J Sport Sci. 2019;19:295–304. [DOI] [PubMed] [Google Scholar]
- [84].Racinais S, Buchheit M, Bilsborough J, et al. Physiological and performance responses to a training camp in the heat in professional Australian football players. Int J Sports Physiol Perform. 2014;9:598–603. [DOI] [PubMed] [Google Scholar]
- [85].Buchheit M, Voss SC, Nybo L, et al. Physiological and performance adaptations to an in-season soccer camp in the heat: associations with heart rate and heart rate variability. Scand J Med Sci Sports. 2011;21:e477–e485. [DOI] [PubMed] [Google Scholar]
- [86].Hellon RF, Jones RM, MacPherson RK, et al. Natural and artificial acclimatization to hot environments. J Physiol. 1956;132:559–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [87].Schmit C, Duffield R, Hausswirth C, et al. Pacing adjustments associated with familiarization: heat versus temperate environments. Int J Sports Physiol Perform. 2016;11:855–860. [DOI] [PubMed] [Google Scholar]
- [88].Rendell RA, Prout J, Costello J, et al. The effects of 10 days of separate heat and hypoxic exposure on heat acclimation and temperate exercise performance. Am J Physiol Integr Comp Physiol. 2017;313:R191–R201. [DOI] [PubMed] [Google Scholar]
- [89].Willmott AGB, Gibson OR, Hayes M, et al. The effects of single versus twice daily short term heat acclimation on heat strain and 3000 m running performance in hot, humid conditions. J Therm Biol. 2016;56:59–67. [DOI] [PubMed] [Google Scholar]
- [90].Lee BJ, Miller A, James RS, et al. Cross acclimation between heat and hypoxia: heat acclimation improves cellular tolerance and exercise performance in acute normobaric hypoxia. Front Physiol. 2016;7:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [91].Armstrong LE, Maresh CM, Keith NR, et al. Heat acclimation and physical training adaptations of young women using different contraceptive hormones. Am J Physiol Endocrinol Metab. 2005;288:E868–75. [DOI] [PubMed] [Google Scholar]
- [92].Brade C, Dawson B, Wallman K. Effect of precooling and acclimation on repeat-sprint performance in heat. J Sports Sci. 2013;31:779–786. [DOI] [PubMed] [Google Scholar]
- [93].DS K, DL C, WJ F, et al. Muscle metabolism during exercise in the heat in unacclimatized and acclimatized humans. J Appl Physiol. 1985;59:1350–1354. [DOI] [PubMed] [Google Scholar]
- [94].Pethick WA, Stellingwerff T, Lacroix MA, et al. The effect of a team sport-specific heat acclimation protocol on plasma volume in elite female soccer players. Sci Med Footb. 2018;2:16–22. [Google Scholar]
- [95].Scoon GSM, Hopkins WG, Mayhew S, et al. Effect of post-exercise sauna bathing on the endurance performance of competitive male runners. J Sci Med Sport. 2007;10:259–262. [DOI] [PubMed] [Google Scholar]
- [96].Zurawlew MJ, Mee JA, Walsh NP. Heat acclimation by post-exercise hot water immersion in the morning reduces thermal strain during morning and afternoon exercise-heat-stress. Int J Sports Physiol Perform. 2018;1–6. [DOI] [PubMed] [Google Scholar]
- [97].Zurawlew MJ, Mee JA, Walsh NP. Post-exercise hot water immersion elicits heat acclimation adaptations in endurance trained and recreationally active individuals. Front Physiol. 2018;9:1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [98].Zurawlew MJ, Walsh NP, Fortes MB, et al. Post‐exercise hot water immersion induces heat acclimation and improves endurance exercise performance in the heat. Scand J Med Sci Sports. 2015;26:745–754. [DOI] [PubMed] [Google Scholar]
- [99].Stevens CJ, Plews DJ, Laursen PB, et al. Acute physiological and perceptual responses to wearing additional clothing while cycling outdoors in a temperate environment: a practical method to increase the heat load. Temperature. 2017;4:414–419. doi: 10.1080/23328940.2017.1365108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [100].Ely BR, Blanchard LA, Steele JR, et al. Physiological responses to overdressing and exercise-heat stress in trained runners. Med Sci Sport Exerc. 2018;1.50:1285–1296. [DOI] [PubMed] [Google Scholar]
- [101].Willmott AGB, Gibson OR, James CA, et al. Physiological and perceptual responses to exercising in restrictive heat loss attire with use of an upper-body sauna suit in temperate and hot conditions. Temperature. 2018;5:162–174. doi: 10.1080/23328940.2018.1426949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [102].Taylor NAS. Principles and practices of heat adaptation. J Human Environ Syst. 2000;4:11–22. [Google Scholar]
- [103].Gibson OR, Willmott AGB, James C, et al. Power relative to body mass best predicts change in core temperature during exercise-heat stress. J Strength Cond Res. 2017;31:403–414. [DOI] [PubMed] [Google Scholar]
- [104].Daanen HAM, Jonkman AG, Layden JD, et al. Optimising the acquisition and retention of heat acclimation. Int J Sports Med. 2011;32:822–828. [DOI] [PubMed] [Google Scholar]
- [105].Gibson OR, Mee JA, Taylor L, et al. Isothermic and fixed-intensity heat acclimation methods elicit equal increases in Hsp72 mRNA. Scand J Med Sci Sports. 2015;25:259–268. [DOI] [PubMed] [Google Scholar]
- [106].Neal RA, Massey HC, Tipton MJ, et al. Effect of permissive dehydration on induction and decay of heat acclimation, and temperate exercise performance. Front Physiol. 2016;7:564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [107].Costa RJS, Crockford MJ, Moore JP, et al. Heat acclimation responses of an ultra-endurance running group preparing for hot desert-based competition. Eur J Sport Sci. 2012;14:1–11. [DOI] [PubMed] [Google Scholar]
- [108].Racinais S, Alonso JM, Coutts AJ, et al. Consensus recommendations on training and competing in the heat. Scand J Med Sci Sports. 2015;25:6–19. [DOI] [PubMed] [Google Scholar]
- [109].Fox RH, Goldsmith R, Kidd DJ, et al. Acclimatization to heat in man by controlled elevation of body temperature. J Physiol. 1963;166:530–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [110].Mee JA, Gibson OR, Doust JJH, et al. A comparison of males and females’ temporal patterning to short- and long-term heat acclimation. Scand J Med Sci Sports. 2015;25:250–258. [DOI] [PubMed] [Google Scholar]
- [111].Taylor NAS, Tipton MJ, Kenny GP. Considerations for the measurement of core, skin and mean body temperatures. J Therm Biol. 2014;46:72–101. [DOI] [PubMed] [Google Scholar]
- [112].Ruddock AD, Thompson SW, Hudson SA, et al. Combined active and passive heat exposure induced heat acclimation in a soccer referee before 2014 FIFA world cup. Springerplus. 2016;5:617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [113].Neal RA, Corbett J, Massey HC, et al. Effect of short-term heat acclimation with permissive dehydration on thermoregulation and temperate exercise performance. Scand J Med Sci Sports. 2015;26:875–884. [DOI] [PubMed] [Google Scholar]
- [114].Patterson MJ, Stocks JM, Taylor NAS. Sustained and generalized extracellular fluid expansion following heat acclimation. J Physiol. 2004;559:327–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [115].Armstrong LE, Hubbard RW, DeLuca JP, et al. Self-paced heat acclimation procedures. U.S.Army Res Inst Environ Med Natick (MA). 1986. [Google Scholar]
- [116].Fox R, Goldsmith R, Kidd D. Acclimatization of the sweating mechanism in man. J Physiol. 1961;157:56–57. [Google Scholar]
- [117].Pallubinsky H, Schellen L, Kingma BRM, et al. Thermophysiological adaptations to passive mild heat acclimation. Temperature. 2017;4:176–186. doi: 10.1080/23328940.2017.1303562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [118].Racinais S, Wilson MG, Gaoua N, et al. Heat acclimation has a protective effect on the central but not peripheral nervous system. J Appl Physiol. 2017;123:816–824. [DOI] [PubMed] [Google Scholar]
- [119].Shido O, Sugimoto N, Tanabe M, et al. Core temperature and sweating onset in humans acclimated to heat given at a fixed daily time. Am J Physiol. 1999;276:R1095–101. [DOI] [PubMed] [Google Scholar]
- [120].Mee JA, Peters S, Doust JH, et al. Sauna exposure immediately prior to short-term heat acclimation accelerates phenotypic adaptation in females. J Sci Med Sport. 2018;21:190–195. [DOI] [PubMed] [Google Scholar]
- [121].Beaudin AE, Clegg ME, Walsh ML, et al. Adaptation of exercise ventilation during an actively-induced hyperthermia following passive heat acclimation. Am J Physiol Regul Integr Comp Physiol. 2009;297:R605–14. [DOI] [PubMed] [Google Scholar]
- [122].Stanley J, Halliday A, D’Auria S, et al. Effect of sauna-based heat acclimation on plasma volume and heart rate variability. Eur J Appl Physiol. 2015;115:785–794. [DOI] [PubMed] [Google Scholar]
- [123].Shin YO, Lee JB, Min YK, et al. Heat acclimation affects circulating levels of prostaglandin E2, COX-2 and orexin in humans. Neurosci Lett. 2013;542:17–20. [DOI] [PubMed] [Google Scholar]
- [124].Brazaitis M, Skurvydas A. Heat acclimation does not reduce the impact of hyperthermia on central fatigue. Eur J Appl Physiol. 2010;109:771–778. [DOI] [PubMed] [Google Scholar]
- [125].Heathcote SL, Hassmén P, Zhou S, et al. Passive heating: reviewing practical heat acclimation strategies for endurance athletes. Front Physiol. 2018;9:1851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [126].Kanikowska D, Sato M, Sugenoya J, et al. No effects of acclimation to heat on immune and hormonal responses to passive heating in healthy volunteers. Int J Biometeorol. 2012;56:107–112. [DOI] [PubMed] [Google Scholar]
- [127].Fox RH, Goldsmith R, Hampton IF, et al. The nature of the increase in sweating capacity produced by heat acclimatization. J Physiol. 1964;171:368–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [128].Shapiro Y, Hubbard RW, Kimbrough CM, et al. Physiological and hematologic responses to summer and winter dry-heat acclimation. J Appl Physiol. 1981;50:792–798. [DOI] [PubMed] [Google Scholar]
- [129].Bradbury PA, Fox RH, Goldsmith R, et al. The effect of exercise of temperature regulation. J Physiol. 1964;171:384–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [130].Kissling LS, Akerman AP, Cotter JD. Heat-induced hypervolemia: does the mode of acclimation matter and what are the implications for performance at Tokyo 2020? Temperature. 2019;1–20. doi: 10.1080/23328940.2019.1653736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [131].Morton JP, Robertson C, Sutton L, et al. Making the weight: a case study from professional boxing. Int J Sport Nutr Exerc Metab. 2010;20:80–85. [DOI] [PubMed] [Google Scholar]
- [132].Crighton B, Close GL, Morton JP. Alarming weight cutting behaviours in mixed martial arts: a cause for concern and a call for action. Br J Sports Med. 2016;50:446–447. [DOI] [PubMed] [Google Scholar]
- [133].Khodaee M, Olewinski L, Shadgan B, et al. Rapid weight loss in sports with weight classes. Curr Sports Med Rep. 2015;14:435–441. [DOI] [PubMed] [Google Scholar]
- [134].Dawson B. Exercise training in sweat clothing in cool conditions to improve heat tolerance. Sports Med. 1994;17:233–244. [DOI] [PubMed] [Google Scholar]
- [135].Garvican-Lewis LA, Sharpe K, Gore CJ. Time for a new metric for hypoxic dose? J Appl Physiol. 2016;121:352–355. [DOI] [PubMed] [Google Scholar]
- [136].Regan JM, Macfarlane DJ, Taylor NA. An evaluation of the role of skin temperature during heat adaptation. Acta Physiol Scand. 1996;158:365–375. [DOI] [PubMed] [Google Scholar]
- [137].Chalmers S, Esterman A, Eston R, et al. Short-term heat acclimation training improves physical performance: a systematic review, and exploration of physiological adaptations and application for team sports. Sports Med. 2014;44:971–988. [DOI] [PubMed] [Google Scholar]
- [138].Spilsbury KL, Fudge BW, Ingham SA, et al. Tapering strategies in elite British endurance runners. Eur J Sport Sci. 2015;15:367–373. [DOI] [PubMed] [Google Scholar]
- [139].Mujika I, Padilla S, Pyne D, et al. Physiological changes associated with the pre-event taper in athletes. Sport Med. 2004. October 19; 34:891–927. [DOI] [PubMed] [Google Scholar]
- [140].Armstrong LE, Maresh CM. The induction and decay of heat acclimatisation in trained athletes. Sports Med. 1991;12:302–312. [DOI] [PubMed] [Google Scholar]
- [141].Garrett AT, Goosens NG, Rehrer NJ, et al. Short-term heat acclimation is effective and may be enhanced rather than impaired by dehydration. Am J Hum Biol. 2014;26:311–320. [DOI] [PubMed] [Google Scholar]
- [142].Aoyagi Y, McLellan TM, Shephard RJ. Interactions of physical training and heat acclimation. The thermophysiology of exercising in a hot climate. Sports Med. 1997. March 01;23:173–210. [DOI] [PubMed] [Google Scholar]
- [143].Périard JD, Racinais S, Sawka MN. Adaptations and mechanisms of human heat acclimation: applications for competitive athletes and sports. Scand J Med Sci Sports. 2015;25:20–38. [DOI] [PubMed] [Google Scholar]
- [144].Houmard JA, Costill DL, Davis JA, et al. The influence of exercise intensity on heat acclimation in trained subjects. Med Sci Sport Exercise. 1990. October 01 ;22:615–620. [DOI] [PubMed] [Google Scholar]
- [145].Reeve T, Gordon R, Laursen PB, et al. Impairment of cycling capacity in the heat in well-trained endurance athletes after high-intensity short-term heat acclimation. Int J Sports Physiol Perform. 2019;14:1058–1065. [DOI] [PubMed] [Google Scholar]
- [146].Gerrett N, Kingma BRM, Sluijter R, et al. Ambient conditions prior to Tokyo 2020 olympic and paralympic games: considerations for acclimation or acclimatization strategies. Front Physiol. 2019;10:414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [147].Willmott AGB, Hayes M, Waldock KAM, et al. Short-term heat acclimation prior to a multi-day desert ultra-marathon improves physiological and psychological responses without compromising immune status. J Sports Sci. 2017;35:2249–2256. [DOI] [PubMed] [Google Scholar]
- [148].Taylor NAS, Patterson MJ, Regan JM, et al. Heat acclimation procedures: preparation for humid heat exposure. Aeronaut. Marit Res Lab. 1997. [Google Scholar]
- [149].Reardon C, Tobin DP, Tierney P, et al. The worst case scenario: locomotor and collision demands of the longest periods of gameplay in professional rugby union. Maher B, editor. PLoS One. 2017. 12, e0177072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [150].Cunningham DJ, Shearer DA, Carter N, et al. Assessing worst case scenarios in movement demands derived from global positioning systems during international rugby union matches: rolling averages versus fixed length epochs. Sunderland C, editor. PLoS One. 2018. 13, e0195197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [151].Whitehead S, Till K, Weaving D, et al. The use of microtechnology to quantify the peak match demands of the football codes: a systematic review. Sport Med. 2018;48:2549–2575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [152].Maughan RJ, Otani H, Watson P. Influence of relative humidity on prolonged exercise capacity in a warm environment. Eur J Appl Physiol. 2012;112:2313–2321. [DOI] [PubMed] [Google Scholar]
- [153].Hayes M, Castle PC, Ross EZ, et al. The influence of hot humid and hot dry environments on intermittent-sprint exercise performance. Int J Sports Physiol Perform. 2014;9:387–396. [DOI] [PubMed] [Google Scholar]
- [154].Griefahn B. Acclimation to three different hot climates with equivalent wet bulb globe temperatures. Ergonomics. 1997;40:223–234. [DOI] [PubMed] [Google Scholar]
- [155].Tebeck ST, Buckley JD, Bellenger CR, et al. Differing physiological adaptations induced by dry and humid short-term heat acclimation. Int J Sports Physiol Perform. 2019;1–24. [DOI] [PubMed] [Google Scholar]
- [156].Buskirk ER. Temperature regulation with exercise. Exerc Sport Sci Rev. 1977;5:45–88. [PubMed] [Google Scholar]
- [157].Otani H, Kaya M, Tamaki A, et al. Effects of solar radiation on endurance exercise capacity in a hot environment. Eur J Appl Physiol. 2016;116:769–779. [DOI] [PubMed] [Google Scholar]
- [158].Wolf ST, Berry CW, Stanhewicz AE, et al. Sunscreen or simulated sweat minimizes the impact of acute ultraviolet radiation on cutaneous microvascular function in healthy humans. Exp Physiol. 2019;104:1136–1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [159].Horowitz M. Epigenetics and cytoprotection with heat acclimation. J Appl Physiol. 2016;120:702–710. [DOI] [PubMed] [Google Scholar]
- [160].Horowitz M. Lessons from gold mines. Temperature. 2017;4:107–108.doi: 10.1080/23328940.2017.1290571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [161].Gill N, Sleivert G. Effect of daily versus intermittent exposure on heat acclimation. Aviat Sp Environ Med. 2001;72:385–390. [PubMed] [Google Scholar]
- [162].Ronsen O, Haugen O, Hall�n J, et al. Residual effects of prior exercise and recovery on subsequent exercise-induced metabolic responses. Eur J Appl Physiol. 2004;92:498–507. [DOI] [PubMed] [Google Scholar]
- [163].Shido O, Sakurada S, Sugimoto N, et al. Ambient temperatures preferred by humans acclimated to heat given at a fixed daily time. Physiol Behav. 2001;72:387–392. [DOI] [PubMed] [Google Scholar]
- [164].Hobson RM, Clapp EL, Watson P, et al. Exercise capacity in the heat is greater in the morning than in the evening in man. Med Sci Sports Exercise. 2009;41:174–180. [DOI] [PubMed] [Google Scholar]
- [165].Alhadad SB, Tan PMS, Lee JKW. Efficacy of heat mitigation strategies on core temperature and endurance exercise: a meta-analysis. Front Physiol. 2019;10:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [166].Cramer MN, Jay O. Explained variance in the thermoregulatory responses to exercise: the independent roles of biophysical and fitness/fatness-related factors. J Appl Physiol. 2015;119:982–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [167].Smoljanic J, Morris NB, Dervis S, et al. Running economy, not aerobic fitness, independently alters thermoregulatory responses during treadmill running. J Appl Physiol. 2014;1451–1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [168].Gibson O, Taylor L, Watt P, et al. Hsp72 mRNA transcription, and sweat adaptations are greater post heat acclimation in trained vs. Untrained individuals. Eur Congr Sport Sci. 2016. [Google Scholar]
- [169].Kolka MA, Levine L, Stephenson LA. Use of an ingestible telemetry sensor to measure core temperature under chemical protective clothing. J Therm Biol. 1997;22:343–349. [Google Scholar]
- [170].Charkoudian N, Stachenfeld NS. Reproductive hormone influences on thermoregulation in women. Compr Physiol. 2014:4:793–804. [DOI] [PubMed] [Google Scholar]
- [171].T-H L, Mündel T. Humid heat stress affects trained female athletes more than does their menstrual phase. Temperature. 2018;5:202–204. doi: 10.1080/23328940.2018.1436394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [172].Lei T-H, Stannard SR, Perry BG, et al. Influence of menstrual phase and arid vs. humid heat stress on autonomic and behavioural thermoregulation during exercise in trained but unacclimated women. J Physiol. 2017;595:2823–2837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [173].Martin D, Sale C, Cooper SB, et al. Period prevalence and perceived side effects of hormonal contraceptive use and the menstrual cycle in elite athletes. Int J Sports Physiol Perform. 2018;13:926–932. [DOI] [PubMed] [Google Scholar]
- [174].Rechichi C, Dawson B, Goodman C. Athletic performance and the oral contraceptive. Int J Sports Physiol Perform. 2009;4:151–162. [DOI] [PubMed] [Google Scholar]
- [175].Tenaglia SA, McLellan TM, Klentrou PP. Influence of menstrual cycle and oral contraceptives on tolerance to uncompensable heat stress. Eur J Appl Physiol Occup Physiol. 1999;80:76–83. [DOI] [PubMed] [Google Scholar]
- [176].Stachenfeld NS, Silva C, Keefe DL. Estrogen modifies the temperature effects of progesterone. J Appl Physiol. 2000;88:1643–1649. [DOI] [PubMed] [Google Scholar]
- [177].Gagnon D, Kenny GP. Sex modulates whole-body sudomotor thermosensitivity during exercise. J Physiol. 2011;589:6205–6217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [178].Burrows M, Bird S. The physiology of the highly trained female endurance runner. Sport Med. 2000;30:281–300. [DOI] [PubMed] [Google Scholar]
- [179].Lei T, Cotter JD, Schlader ZJ, et al. On exercise thermoregulation in females: interaction of endogenous and exogenous ovarian hormones. J Physiol. 2019;597:71–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [180].Morton JP, Holloway K, Woods P, et al. Exercise training-induced gender-specific heat shock protein adaptations in human skeletal muscle. Muscle Nerve. 2009;39:230–233. [DOI] [PubMed] [Google Scholar]
- [181].Mee JA, Gibson OR, Tuttle JA, et al. Leukocyte Hsp72 mRNA transcription does not differ between males and females during heat acclimation. Temperature. 2016;3:549–556. doi: 10.1080/23328940.2016.1214336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [182].Kirby NV, Lucas SJE, Lucas RAI. Nine-, but not four-days heat acclimation improves self-paced endurance performance in females. Front Physiol. 2019;10:539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [183].Mee J, Peters S, Doust J, et al. Restricted sweat evaporation preceding short term heat acclimation accelerates adaption in females. Extrem Physiol Med. 2015;4:A112. [Google Scholar]
- [184].Lind A. Physiologic responses to heat. In: Licht S, editor. Medical climatology. Baltimore, MD: Waverly Press; 1964. p. 164–195. [Google Scholar]
- [185].Zurawlew MJ, Mee JA, Walsh NP. Post-exercise hot water immersion elicits heat acclimation adaptations that are retained for at least two weeks. Front Physiol. 2019;10:1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [186].Casadio JR, Kilding AE, Siegel R, et al. Periodizing heat acclimation in elite laser sailors preparing for a world championship event in hot conditions. Temperature. 2016;3:437–443. doi: 10.1080/23328940.2016.1184367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [187].Casadio JR, Kilding AE, Cotter JD, et al. From lab to real world: heat acclimation considerations for elite athletes. Sport Med. 2017;47:1467–1476. [DOI] [PubMed] [Google Scholar]
- [188].Pryor JL, Pryor RR, Vandermark LW, et al. Intermittent exercise-heat exposures and intense physical activity sustain heat acclimation adaptations. J Sci Med Sport. 2019;22:117–122. [DOI] [PubMed] [Google Scholar]
- [189].Pandolf KB, Burse RL, Goldman RF. Role of physical fitness in heat acclimatisation, decay and reinduction. Ergonomics. 1977;20:399–408. [DOI] [PubMed] [Google Scholar]
- [190].Weller AS, Linnane DM, Jonkman AG, et al. Quantification of the decay and re-induction of heat acclimation in dry-heat following 12 and 26 days without exposure to heat stress. Eur J Appl Physiol. 2007;102:57–66. [DOI] [PubMed] [Google Scholar]
- [191].Akerman AP, Tipton M, Minson CT, et al. Heat stress and dehydration in adapting for performance: good, bad, both, or neither? Temperature. 2016;3:412–436. doi: 10.1080/23328940.2016.1216255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [192].Pethick WA, Murray HJ, McFadyen P, et al. Effects of hydration status during heat acclimation on plasma volume and performance. Scand J Med Sci Sports. 2018;29:189–199. [DOI] [PubMed] [Google Scholar]
- [193].Mitchell JB, Grandjean PW, Pizza FX, et al. The effect of volume ingested on rehydration and gastric emptying following exercise-induced dehydration. Med Sci Sports Exercise. 1994;26:1135–1143. [PubMed] [Google Scholar]
- [194].Febbraio MA, Carey MF, Snow RJ, et al. Influence of elevated muscle temperature on metabolism during intense, dynamic exercise. Am J Physiol. 1996;271:R1251–5. [DOI] [PubMed] [Google Scholar]
- [195].Gibson OR, Turner G, Tuttle JA, et al. Heat acclimation attenuates physiological strain and the HSP72, but not HSP90α, mRNA response to acute normobaric hypoxia. J Appl Physiol. 2015;119:889–899. [DOI] [PubMed] [Google Scholar]
- [196].James CA, Richardson AJ, Watt PW, et al. Physiological responses to incremental exercise in the heat following internal and external precooling. Scand J Med Sci Sports. 2015;25:190–199. [DOI] [PubMed] [Google Scholar]
- [197].Morton RW, McGlory C, Phillips SM. Nutritional interventions to augment resistance training-induced skeletal muscle hypertrophy. Front Physiol. 2015;6:245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [198].Tipton KD, Wolfe RR. Protein and amino acids for athletes. J Sports Sci. 2004;22:65–79. [DOI] [PubMed] [Google Scholar]
- [199].Tipton KD, Witard OC. Protein requirements and recommendations for athletes: relevance of ivory tower arguments for practical recommendations. Clin Sports Med. 2007;26:17–36. [DOI] [PubMed] [Google Scholar]
- [200].Zuhl M, Dokladny K, Mermier C, et al. The effects of acute oral glutamine supplementation on exercise-induced gastrointestinal permeability and heat shock protein expression in peripheral blood mononuclear cells. Cell Stress Chaperones. 2015;20:85–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [201].Wischmeyer PE, Kahana M, Wolfson R, et al. Glutamine induces heat shock protein and protects against endotoxin shock in the rat. J Appl Physiol. 2001;90:2403–2410. [DOI] [PubMed] [Google Scholar]
- [202].Zuhl MN, Lanphere KR, Kravitz L, et al. The effects of oral glutamine supplementation on exercise induced gastrointestinal permeability and tight junction protein expression. J Appl Physiol. 2014; 116:183–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [203].Marshall H, Chrismas BC, Suckling CA, et al. Chronic probiotic supplementation with or without glutamine does not influence the eHsp72 response to a multi-day ultra-endurance exercise event. Appl Physiol Nutr Metab. 2017;42:876–883. [DOI] [PubMed] [Google Scholar]
- [204].Costa RJS, Gaskell SK, McCubbin A. Exertional-heat stress associated gastrointestinal perturbations during olympic sports: management strategies for athletes preparing and competing in the 2020 Tokyo olympic games. Temperature. 2019;1–31. doi: 10.1080/23328940.2019.1597676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [205].Evans GH, James LJ, Shirreffs SM, et al. Optimizing the restoration and maintenance of fluid balance after exercise-induced dehydration. J Appl Physiol. 2017;122:945–951. [DOI] [PubMed] [Google Scholar]
- [206].Guy J, Vincent G. Nutrition and supplementation considerations to limit endotoxemia when exercising in the heat. Sports. 2018;6:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [207].Thomas DT, Erdman KA, Burke LM. American college of sports medicine joint position statement. nutrition and athletic performance. Med Sci Sports Exercise. 2016;48:543–568. [DOI] [PubMed] [Google Scholar]
- [208].Bongers CCWG, Hopman MTE, Eijsvogels TMH. Cooling interventions for athletes: an overview of effectiveness, physiological mechanisms, and practical considerations. Temperature. 2017;4:60–78doi: 10.1080/23328940.2016.1277003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [209].Wegmann M, Faude O, Poppendieck W, et al. Pre-cooling and sports performance. Sport Med. 2012;42:545–564. [DOI] [PubMed] [Google Scholar]
- [210].Tyler CJ, Sunderland C, Cheung SS. The effect of cooling prior to and during exercise on exercise performance and capacity in the heat: a meta-analysis. Br J Sports Med. 2015;49:7–13. [DOI] [PubMed] [Google Scholar]
- [211].Ruddock A, Robbins B, Tew G, et al. Practical cooling strategies during continuous exercise in hot environments: a systematic review and meta-analysis. Sports Med. 2017;47:517–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [212].Stevens CJ, Taylor L, Dascombe BJ. cooling during exercise: an overlooked strategy for enhancing endurance performance in the heat. Sports Med. 2017;47:829–841. [DOI] [PubMed] [Google Scholar]
- [213].Choo HC, Nosaka K, Peiffer JJ, et al. Reliability of laser doppler, near-infrared spectroscopy and doppler ultrasound for peripheral blood flow measurements during and after exercise in the heat. J Sports Sci. 2017;35:1715–1723. [DOI] [PubMed] [Google Scholar]
- [214].Best R, Payton S, Spears I, et al. Topical and ingested cooling methodologies for endurance exercise performance in the heat. Sports. 2018;6:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [215].McNeely E. Practical aspects of precooling for competition in the heat. Strength Cond J. 2015;37:69–73. [Google Scholar]
- [216].Ross M, Abbiss C, Laursen P, et al. Precooling methods and their effects on athletic performance. Sport Med. 2013;43:207–225. [DOI] [PubMed] [Google Scholar]
- [217].Jones PR, Barton C, Morrissey D, et al. Pre-cooling for endurance exercise performance in the heat: a systematic review. BMC Med. 2012;10:166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [218].Dervis SM, Coombs GB, Chaseling GK, et al. A comparison of thermoregulatory responses to exercise between mass-matched groups with large differences in body fat. J Appl Physiol. 2016;120:615–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [219].Jay O, Bain AR, Deren TM, et al. Large differences in peak oxygen uptake do not independently alter changes in core temperature and sweating during exercise. Am J Physiol Regul Integr Comp Physiol. 2011;301:R832–41. [DOI] [PubMed] [Google Scholar]
- [220].Nybo L, Rasmussen P, Sawka MN. Performance in the heat-physiological factors of importance for hyperthermia-induced fatigue. Compr Physiol. 2014;4:657–689. [DOI] [PubMed] [Google Scholar]
- [221].Tyler CJ, Sunderland C, Cheung SS. The effect of cooling prior to and during exercise on exercise performance and capacity in the heat: a meta-analysis. Br J Sports Med. 2013;49:1–8. [DOI] [PubMed] [Google Scholar]
- [222].Schlader ZJ, Simmons SE, Stannard SR, et al. The independent roles of temperature and thermal perception in the control of human thermoregulatory behavior. Physiol Behav. 2011;103:217–224. [DOI] [PubMed] [Google Scholar]
- [223].Flouris AD, Schlader ZJ. Human behavioral thermoregulation during exercise in the heat. Scand J Med Sci Sports. 2015;25:52–64. [DOI] [PubMed] [Google Scholar]
- [224].Stevens CJ, Menthol: BR. A fresh ergogenic aid for athletic performance. Sport Med. 2017;47:1035–1042. [DOI] [PubMed] [Google Scholar]
- [225].Gibson OR, Wrightson JG, Hayes M. Intermittent sprint performance in the heat is not altered by augmenting thermal perception via L-menthol or capsaicin mouth rinses. Eur J Appl Physiol. 2019;119:653–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [226].Wilson T, Johnson S, Petajan J, et al. Thermal regulatory responses to submaximal cycling following lower-body cooling in humans. Eur J Appl Physiol. 2002;88:67–75. [DOI] [PubMed] [Google Scholar]
- [227].Parsons K. Human thermal environments: the effects of hot, moderate, and cold environments on human health, comfort, and performance. 3rd ed. Boca Raton, FL: CRC Press; 2014. [Google Scholar]
- [228].Casa DJ, Armstrong LE, Ganio MS, et al. Exertional heat stroke in competitive athletes. Curr Sports Med Rep. 2005;4:309–317. [DOI] [PubMed] [Google Scholar]
- [229].White AT, Davis SL, Wilson TE. Metabolic, thermoregulatory, and perceptual responses during exercise after lower vs. whole body precooling. J Appl Physiol. 2003;94:1039–1044. [DOI] [PubMed] [Google Scholar]
- [230].Siegel R, Maté J, Watson G, et al. Pre-cooling with ice slurry ingestion leads to similar run times to exhaustion in the heat as cold water immersion. J Sports Sci. 2012;30:155–165. [DOI] [PubMed] [Google Scholar]
- [231].Duffield R, Coutts AJ, Quinn J. Core temperature responses and match running performance during intermittent-sprint exercise competition in warm conditions. J Strength Cond Res. 2009;23:1238–1244. [DOI] [PubMed] [Google Scholar]
- [232].Minett GM, Duffield R, Marino FE, et al. Volume-dependent response of precooling for intermittent-sprint exercise in the heat. Med Sci Sport Exerc. 2011;43:1760–1769. [DOI] [PubMed] [Google Scholar]
- [233].Randall CA, Ross EZ, Maxwell NS. Effect of practical precooling on neuromuscular function and 5-km time-trial performance in hot, humid conditions among well-trained male runners. J Strength Cond Res. 2015;29:1925–1936. [DOI] [PubMed] [Google Scholar]
- [234].Sunderland C, Stevens R, Everson B, et al. Neck-cooling improves repeated sprint performance in the heat. Front Physiol. 2015;6:314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [235].Cuttell SA, Kiri V, Tyler C. A comparison of 2 practical cooling methods on cycling capacity in the heat. J Athl Train. 2016;51:525–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [236].Tyler CJ, Sunderland C. Neck cooling and running performance in the heat: single versus repeated application. Med Sci Sports Exercise. 2011;43:2388–2395. [DOI] [PubMed] [Google Scholar]
- [237].Castle PC, Macdonald AL, Philp A, et al. Precooling leg muscle improves intermittent sprint exercise performance in hot, humid conditions. J Appl Physiol. 2006;100:1377–1384. [DOI] [PubMed] [Google Scholar]
- [238].Webb P. Afterdrop of body temperature during rewarming: an alternative explanation. J Appl Physiol. 1986;60:385–390. [DOI] [PubMed] [Google Scholar]
- [239].Ramanathan NL. A new weighting system for mean surface temperature of the human body. J Appl Physiol. 1964;19:531–533. [DOI] [PubMed] [Google Scholar]
- [240].Kay D, Taaffe DR, Marino FE. Whole-body pre-cooling and heat storage during self-paced cycling performance in warm humid conditions. J Sports Sci. 1999;17:937–944. [DOI] [PubMed] [Google Scholar]
- [241].Price MJ, Maley MJ. The effects of pre-cooling on skin blood flow during exercise in the heat and subsequent performance. Extrem Physiol Med. 2015;4:A127. [Google Scholar]
- [242].Périard JD. Cardiovascular determinants involved in pacing under heat stress. Sports Med. 2013;43:643–645. [DOI] [PubMed] [Google Scholar]
- [243].Flouris AD. Functional architecture of behavioural thermoregulation. Eur J Appl Physiol. 2011;111:1–8. [DOI] [PubMed] [Google Scholar]
- [244].Villanova N, Azpiroz F, JR M. Perception and gut reflexes induced by stimulation of gastrointestinal thermoreceptors in humans. J Physiol. 1997;502(1):215–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [245].Ihsan M, Landers G, Brearley M, et al. Beneficial effects of ice ingestion as a precooling strategy on 40-km cycling time-trial performance. Int J Sports Physiol Perform. 2010;5:140–151. [DOI] [PubMed] [Google Scholar]
- [246].Ross MLR, Garvican-Lewis LA, Jeacocke NA, et al. Novel precooling strategy enhances time trial cycling in the heat. Med Sci Sport Exerc. 2011;43:123–133. [DOI] [PubMed] [Google Scholar]
- [247].Morris NB, Coombs G, Jay O. Ice slurry ingestion leads to a lower net heat loss during exercise in the heat. Med Sci Sports Exercise. 2016;48:114–122. [DOI] [PubMed] [Google Scholar]
- [248].Zimmermann M, Landers G, Wallman KE, et al. The effects of crushed ice ingestion prior to steady state exercise in the heat. Int J Sport Nutr Exerc Metab. 2017;27:220–227. [DOI] [PubMed] [Google Scholar]
- [249].Tan PMS, Lee JKW. The role of fluid temperature and form on endurance performance in the heat. Scand J Med Sci Sports. 2015;25:39–51. [DOI] [PubMed] [Google Scholar]
- [250].Onitsuka S, Nakamura D, Onishi T, et al. Ice slurry ingestion reduces human brain temperature measured using non-invasive magnetic resonance spectroscopy. Sci Rep. 2018;8:2757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [251].Naito T, Iribe Y, Ogaki T. Ice ingestion with a long rest interval increases the endurance exercise capacity and reduces the core temperature in the heat. J Physiol Anthropol. 2017;36:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [252].Morris NB, Jay O. To drink or to pour: how should athletes use water to cool themselves? Temperature. 2016;3:191–194. doi: 10.1080/23328940.2016.1185206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [253].Chaen Y, Onitsuka S, Hasegawa H. Wearing a cooling vest during half-time improves intermittent exercise in the heat. Front Physiol. 2019;10:711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [254].Maroni T, Dawson B, Dennis M, et al. Effects of half-time cooling using a cooling glove and jacket on manual dexterity and repeated-sprint performance in heat. J Sports Sci Med. 2018;17:485–491. [PMC free article] [PubMed] [Google Scholar]


