Abstract
Background.
Multiple studies have demonstrated that when incorporated with conventional imaging modalities, cardiac F-18 PET/CT can aid in diagnosis of endocarditis and improve the sensitivity of the Duke Criteria. These studies used as their gold standard the opinion of an endocarditis team and were characterized by low percentages of patients who underwent surgery. We reviewed 4 years of surgically managed IE cases where F-18 cardiac PET/CT was used to aid diagnosis.
Methods.
Between July 2014 and December 2018, we retrospectively reviewed 68 surgically managed endocarditis cases to identify patients who underwent pre-operative PET scans.
Results.
Fourteen patients were identified who underwent F-18 cardiac PET/CT prior to surgical intervention. Nine cases were classified as possible endocarditis by Duke Criteria and 8 involved prosthetic valves. Twelve out of fourteen scans were interpreted as suggestive of or consistent with endocarditis based on FDG uptake. Twelve positive PETs were associated with either operative findings of infection and/or positive PCR testing on the excised valve. Two patients with negative scans were found to have non-infectious mobile masses intra-operatively, negative valve cultures and negative pathology.
Conclusion.
In a small cohort, F-18 FDG cardiac PET/CT correlated closely with intra-operative findings in patients with endocarditis and helped guide surgical decision-making. It could be considered for addition to the Duke Criteria in the American Heart Association endocarditis guidelines similar to European protocols.
Keywords: Infection, PET, Diagnostic, Prognostic application
INTRODUCTION
Infectious endocarditis (IE) is a disease process with significant morbidity and in-hospital mortality approaching 20%.1 Care for patients with infectious endocarditis is complicated by delays in diagnosis and the relatively low sensitivity (~ 70 to 80%) of existing diagnostic algorithms, particularly the Duke Criteria.2 In recent years, F-18fluorodeoxyglucose (FDG) cardiac positron emission tomography/computed tomography (PET/CT) has been identfied as a useful tool in detecting occult endocardial infections, particularly in the setting of prosthetic valves. Multiple prospective studies have demonstrated that when incorporated with conventional imaging modalities, such as echocardiography, FDG PET/CT can improve the sensitivity of the Duke Criteria from 27–38% to 91–97%.3,4 Overall, a 2017 meta-analysis of 13 papers reported a pooled sensitivity of 76.8% for diagnosis of IE.5 In part based on these findings, the 2015 European Society of Cardiology (ESC) endocarditis guidelines added FDG cardiac PET/CT to their IE diagnostic criteria.6 However, all previous studies have used as their reference standard for diagnosis the consensus opinion of an endocarditis team or the modified Duke Criteria. Many of these studies were characterized by a relatively low percentage of patients who underwent surgery. As a result, pathologic or operative confirmation of IE was not available from the majority of cases. To better understand the correlation between positive PET results and pathologic and operative findings, we reviewed 4 years of surgically managed IE cases at a tertiary care medical center where FDG cardiac PET/CT was used to aid diagnosis.
METHODS
Between July 1, 2014 and December 31, 2018 we retrospectively reviewed 68 surgically managed cases of endocarditis. Cases were identified using International Classification of Diseases (ICD) 9 and ICD-10 codes of patients who underwent surgical valve replacement for endocarditis as well as all patients who had FDG PET/CT scans protocoled for myocardial sarcoid or inflammation performed in the setting of clinical suspicion of endocarditis (Figure 1). Cases where FDG PET/CT was obtained only for suspicion of sarcoidosis were not included. Additional cases were identified through the registry of the institutional multidisciplinary endocarditis team which has been active since June, 2018. All patients with prosthetic valves who underwent FDG cardiac PET/CT imaging did so > 3 months after valve implantation. Patients who had FDG PET/CT testing without a myocardial suppression protocol were not included in this study. Images were acquired using a whole-body PET/CT scanner (Siemens Biograph mCT, Knoxville, TN). Rest myocardial perfusion images were obtained using 82Rb as previously described.7 All patients also underwent 36 hours of preparation for suppression of myocardial glucose uptake prior to PET/CT scan per a separately published protocol.8 A total of 30 IU/kg of UFH was administered as three boluses (10 IU/kg) at 10 minutes before and 5 and 20 minutes after FDG injection. FDG Images were acquired for 15 minutes in list mode using 3D ordered subset expectation maximization (3D-OSEM) according to manufacturer’s recommendations with 3 iterations and 24 subsets, matrix size of 128 × 128 and pixel size of 3.18 × 3.18 mm. Variables including pre-operative modified Duke Criteria,9 PET results, operative findings, valve culture, pathology (microscopic vs. gross examination) and polymerase chain reaction (PCR) testing were recorded.
Figure 1.
Identification of patients for inclusion in retrospective analysis.
Definition of terms
FDG cardiac PET/CT scans were interpreted as positive if the FDG uptake of the valve in question was greater than the blood pool FDG value. Operative findings were noted as being consistent with infection if the surgical documentation mentioned any of the following: signs of infection, abscess, purulent vegetations, fistula formation or leaflet destruction. All other findings were considered to be non-infectious. Valve cultures were considered positive if organisms were identified on gram stain or successfully cultured. Pathologic results were documented as consistent with IE if organisms were identified histologically or if the final pathologic report included endocarditis in the final diagnosis. Echocardiography was considered positive if it met any of the Duke Criteria for endocardial involvement (Figures 2, 3).
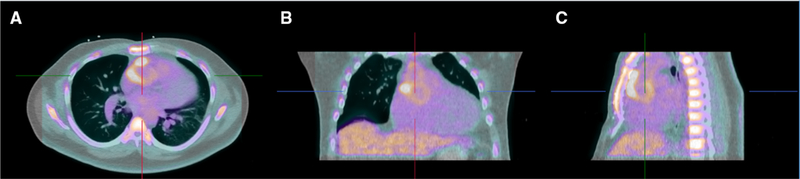
Figure 2.
18-FDG Cardiac PET/CT images from a patient with a native bicuspid aortic valve and 28 mm Gelweave ascending aortic/arch graft demonstrating increased FDG uptake (SUV 3.9) in the ascending aorta extending down to the aortic valve in axial (A) coronal (B) and sagittal (C) views.
Figure 3.
18-FDG Cardiac PET/CT demonstrating focal uptake in the region of the aortic valve (A). Short axis (B) and long axis (C) transesophageal echocardiogram images demonstrating a large vegetation on the left coronary cusp of the aortic valve.
RESULTS
Fourteen patients were identified who underwent FDG cardiac PET/CT prior to surgical intervention for presumed endocarditis. Nine (64.3%) cases were classified as possible endocarditis by Duke Criteria and the remaining 5 met definite endocarditis criteria (Table 1). Eight (57.1%) patients had prosthetic valves. Operative findings were consistent with infection in 11 (78.66%) patients. Of the remaining 3 cases, 1 was found to have a positive PCR test for Bartonella spp. from the excised valve suggesting the presence of bacterial DNA. The other 2 cases were determined to have a fractured prosthetic valve leaflet and a non-infectious thrombus, respectively. The most common infectious findings intra-operatively were purulent vegetations, seen in 6 patients. Abscesses were identified in 5 patients.
Table 1.
Pre-operative and intra-operative findings in 14 surgically managed endocarditis cases
| Organisms (n) | Duke criteria | Echo findings | PET results | Cardiac SUV max | Blood pool SUV |
|---|---|---|---|---|---|
| MSSA | Definite | Echolucent space posterior to the bioprosthetic AV | Positive | 6.8 | 2.0 |
| MSSA/MRSA | Possible | Native AV thickening | Positive | 5.6 | 1.8 |
| Staphylococcus epidermidis | Definite | Native AV vegetation | Positive | 2.1 | 2 |
| Staphylococcus lugdunensis/Citrobacter spp. | Possible | Bioprosthetic AV vegetation with abscess | Positive | 5.2 | 1.5 |
| Streptococcus mitis | Definite | Native AV vegetation with aortic root abscess | Positive | 3.1 | 1.2 |
| Streptococcus mutans | Definite | Normal bioprosthetic AV | Positive | 5.3 | 1.6 |
| Streptococcus bovis | Definite | Bioprosthetic AV vegetation | Positive | 6.2 | 1.6 |
| Streptococcus agalactiae | Possible | Native MV vegetation | Positive | 4.4 | 2.4 |
| Corynebacterium spp. | Possible | Native AV vegetation | Positive | 2.2 | 1.6 |
| Aggregatibacter spp. | Possible | Native AV cusp thickening | Positive | 3.9 | 1.2 |
| Culture negative | Possible | Bioprosthetic AV thickening | Positive | 3.3 | 2.5 |
| Culture negative | Possible | Bioprosthetic AV vegetation with severe Al | Positive | 5.4 | 2.8 |
| Culture negative | Possible | Calcified bioprosthetic MV | Negative | 1.9 | 1.4 |
| Culture negative | Possible | Bioprosthetic AV vegetation with severe AI | Negative | 1.8 | 1.7 |
| Organisms (n) | OR findings | Endocardial manifestations | OR culture | Pathology | Valve PCR |
| MSSA | Infection | Abscess/vegetations | GPCs | Not performed | N/A |
| MSSA/MRSA | Infection | Abscess | No growth | Dystrophic calcification | N/A |
| Staphylococcus epidermidis | Infection | Purulent vegetations | No growth | Not performed | Staphylococcus epidermidis |
| Staphylococcus lugdunensis/Citrobacter spp. | Infection | Abscess | Coag negative staph | Endocarditis | Enterobacteriaceae spp. |
| Streptococcus mitis | Infection | Abscess/vegetations | Strep mitis | Not performed | N/A |
| Streptococcus mutans | Infection | Abscess/vegetation | No growth | Not performed | Streptococcus mutans |
| Streptococcus bovis | Infection | Purulent vegetation | No growth | Not performed | N/A |
| Streptococcus agalactiae | Indeterminate | Leaflet destruction | No growth | Endocarditis | N/A |
| Corynebacterium spp. | Infection | Purulent vegetations | No growth | Endocarditis | |
| Aggregatibacter spp. | Infection | Abscess | No growth | Dystrophic calcification | N/A |
| Culture negative | Infection | Leaflet destruction | No growth | Dystrophic calcification | Granulicatella spp. |
| Culture negative | Non-infectious | Fractured leaflet | Not performed | Not performed | Bartonella spp. |
| Culture negative | Non-infectious | Fractured leaflet | Not performed | Not performed | N/A |
| Culture negative | Non-infectious | Thrombus | No growth | Not performed | N/A |
Twelve out of fourteen FDG cardiac PET/CT scans were interpreted as consistent with endocarditis. The two negative scans were performed in the patients ultimately found to have fractured leaflets and thrombus. All 12 positive PETs correlated with either operative findings of infection or positive microbiologic test for a positive predictive value of 100%. The remaining positive FDG PET/CT occurred in the patient who was ultimately found to have a positive valve PCR.
Pre-operatively, 12 patients underwent transthoracic echocardiography (TTE). Five TTEs met Duke Criteria for endocardial involvement, however, one of the positive TTEs was performed in the patient with a fractured leaflet. Four out of five positive TTEs correlated with operative findings consistent with infection. Transesophageal echocardiography was performed in 12 patients and was interpreted as positive in 7 patients, again with one of the positive results identified in a patient with non-infectious thrombus intra-operatively.
Valve cultures were performed in 12 cases and were positive in 3. Valve PCR was positive in 5 additional cases for combined sensitivity of valve culture and PCR of 67%. Of note, in 2 cases the valve PCR identified organisms that were not previously suspected preoperatively. Both patients received alterations in their treatment plans as a result of these findings. Pathologic review was consistent with endocarditis in 3 cases but notably was not completed in 7 cases.
DISCUSSION
FDG cardiac PET/CT is an emerging and increasingly utilized technology in patients with infectious endocarditis and when incorporated into the Modified Duke Criteria has been shown to improve their diagnostic sensitivity and specificity.4 However, previous studies have been limited by utilizing a consensus opinion of an endocarditis team, by a relatively small percentage of surgical cases as well as uncharacteristically low sensitivity of the Duke Criteria in their cohort. Our study is unique in that we have only incorporated surgical patients. Although there is little literature about the sensitivity and specificity of operative findings as they relate to pathologic review or valve culture, they are often used to guide medical decision-making in IE. While the presence of an abscess or purulent vegetations logically suggests the presence of infection even in the absence of positive culture or histology, these findings are not considered pathognomonic for endocarditis by the Duke Criteria. This is particularly relevant for two reasons. First, many patients have already received several days or weeks of antibiotic prior to surgery. Second, many excised valves are not sent for pathologic review. In our cohort, 29/68 (43%) reviewed cases were either not sent for microscopic review or only underwent a gross examination.
In this highly selected pilot study, FDG PET/CT using a protocol to suppress physiologic myocardial glucose uptake correlated very closely with operative findings. The only positive FDG PET/CT that did not have associated evidence of infection intra-operatively was later found to have a positive bacterial PCR from the excised prosthetic valve. Both patients with negative FDG PET/CT scans were later found to have non-infectious causes for their presentations. These findings suggest that in the setting of a clinical suspicion of endocarditis cardiac FDG PET/CT may be used to guide both medical and surgical decision-making. In the appropriate setting, a positive cardiac FDG PET/CT could be considered presumptive of endocarditis until proven otherwise.
The role of FDG PET/CT is particularly important in cases of prosthetic valve endocarditis where the sensitivity of TEE is decreased.10 The data from our cohort are consistent with the recommendations in the 2015 ESC guidelines to add cardiac FDG PET/CT to the diagnostic criteria for endocarditis in patients with prosthetic valves implanted for >3 months. This could be considered as an addition to the Modified Duke Criteria and incorporated into the AHA endocarditis guideline. The addition of operative findings to the Duke Criteria would also likely increase diagnostic sensitivity and are already being used in clinical practice.
An additional finding was the relatively low sensitivity of valve culture, which was increased considerably when valve PCR was incorporated. The improved sensitivity of valve PCR testing has previously been demonstrated, although there is little data regarding whether PCR findings change clinical management.11 Both patients who were found to have positive valve PCR results were treated with additional course of antibiotics post-operatively. However, it is unclear whether these results should be impacting medical decision-making and further research is needed on this topic.
Our study is limited by the small sample size of only 14 patients as well as by its retrospective nature. The findings of low sensitivity of both TTE and TEE may be the result of selection bias as patients with overt vegetations seen on echocardiography would be less likely to have a cardiac FDG PET/CT performed. Additionally, there is certainly a subset of patients who had positive cardiac PETs that did not undergo valve surgery. Among these individuals there are likely some who do not have endocarditis but are treated as such given their PET findings. However, this group is not captured by the parameters of our study. Despite this, our data supports that cardiac FDG PET/CT is an increasingly important modality in the diagnosis of a complex and highly morbid infectious disease.
NEW KNOWLEDGE GAINED
Cardiac FDG PET/CT correlates closely with intra-operative findings in IE. Universal PCR increased the microbiologic diagnosis when added to valve culture in surgically managed IE. The sensitivity of TEE for diagnosing vegetations may be over-estimated by the existing medical literature.
Supplementary Material
Disclosure
S. El-Dalati, R.L. Weinberg, A.B. Owczarczyk, C. Fagan, J. Riddell IV and S. Cinti have no conflicts of interest to disclose. V.L. Murthy has received consulting fees and stock options from Ionetix, Inc., owns stock in General Electric and Cardinal health, has a research grant from Siemens Medical Imaging, and has provided expert witness testimony on behalf of Jubilant Draximage. V. L. Murthy is supported by 1R01HL136685 from the National, Heart, Lung, Blood Institute and 1R01AG059729 from the National Institute on Aging.
Abbreviations
- PET
Positron emission tomography
- IE
Infectious endocarditis
- FDG
Fluorodeoxyglucose
- CT
Computerized tomography
- ICD
International statistical classifications of disease
- PCR
Polymerase chain reaction
Footnotes
Electronic supplementary material The online version of this article (https://doi.org/10.1007/s12350-019-01874-x) contains supplementary material, which is available to authorized users.
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bor DH, Woolhandler S, Nardin R, Brusch J, Himmelstein DU. Infective endocarditis in the U.S., 1998–2009: A nationwide study. Wertheim HFL, ed. PLoS ONE 2013;8(3):e60033. 10.1371/journal.pone.0060033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shrestha N, Shakya S, Hussain S, et al. Sensitivity and specificity of duke criteria for diagnosis of definite infective endocarditis: A cohort study. Open Forum Infect Dis 2017;4(1):S550–1. [Google Scholar]
- 3.Pizzi M, Roque A, Fernandez-Hidalgo N, et al. Improving the diagnosis of infective endocarditis in prosthetic valves and intracardiac devices With 18F-fluordeoxyglucose positron emission tomography/compute tomography angiography: Initial results at an infective endocarditis referral center. Circulation 2015;132(12):1113–26. [DOI] [PubMed] [Google Scholar]
- 4.Saby L, Laas O, Habib G, et al. Positron emission tomography/computed tomography for diagnosis of prosthetic valve endocarditis: Increased valvular 18F-fluorodeoxyglucose uptake as a novel major criterion. J Am Coll Cardiol 2013;61(23):2374–82. [DOI] [PubMed] [Google Scholar]
- 5.Mahmood M, Kendi AT, Ajmal S, et al. Meta-analysis of 18F-FDG PET/CT in the diagnosis of infective endocarditis. J Nucl Cardiol 2017;26(3):922–35. [DOI] [PubMed] [Google Scholar]
- 6.Habib, et al. 2015 ESC Guidelines for the management of infective endocarditis: The task force for the management of infective endocarditis of the European Society of Cardiology (ESC). Eur Heart J 2015;36(44):3075–128. [DOI] [PubMed] [Google Scholar]
- 7.Lee BC, Moody JB, Weinberg RL, et al. Optimization of temporal sampling for 82rubidium PET myocardial blood flow quantification. J Nucl Cardiol 2017;24:1517–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Larson S, Pieper J, Hulten E, et al. Characterization of a highly effective preparation for suppression of myocardial glucose utilization. J Nucl Cardiol 2019. 10.1007/s12350-019-01786-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li J, Sexton D, Mick N, et al. Proposed modifications to the duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 2000;30(4):633–8. [DOI] [PubMed] [Google Scholar]
- 10.Evangelista A, Gonzalez-Alujas MT. Echocardiography in infective endocarditis. Heart 2004;90:614–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shrestha N, Ledtke C, Wang H, et al. Heart valve culture and sequencing to identify the infective endocarditis pathogen in surgically treated patients. Ann Thorac Surg 2015;99:33–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.