Abstract
Background:
Pregnancy anxiety predicts adverse developmental outcomes in offspring from infancy through late childhood, but studies have not examined associations with outcomes in early childhood, nor clarified ethnic or cultural variations in these processes.
Aims:
To examine differences in pregnancy anxiety and related concerns between non-Hispanic White women, Latina women who prefer to speak in English, and Latinas who prefer Spanish; (2) To test prospective associations between pregnancy anxiety and child negative affect and moderation by ethnicity and language preference, used as a proxy for acculturation.
Study design and methods:
This longitudinal study included 95 women (40 Non-Hispanic Whites, 31 Spanish-preference Latinas, and 24 English-preference Latinas). Language preference was provided at study entry. Pregnancy anxiety was assessed in the second and third trimesters of pregnancy with two standardized measures. Mothers reported child negative affect at age 4.
Results:
Spanish-preference Latinas had significantly more pregnancy-related anxiety about their health and safety in childbirth and concerning the medical system compared to English-preference Latinas and non-Hispanic White women. Adjusting for covariates, pregnancy anxiety in the second trimester, though not the third trimester, predicted significantly higher child negative affect in the full sample. A significant moderation effect indicated that the association was strongest among the lower acculturated Latinas, i.e., those who preferred Spanish.
Conclusion:
These results document higher risk for offspring associated with pregnancy anxiety in the second trimester especially among less acculturated Latina women, and suggest the need for culturally-sensitive screening tools and interventions to improve outcomes for Latina mothers and their children.
Keywords: pregnancy anxiety, prenatal anxiety, Latina mothers, child negative affect, ethnicity, acculturation
Introduction
Pregnancy anxiety is a context-specific form of anxiety rooted in fears and concerns regarding one’s current pregnancy [1–3]. This type of anxiety may reflect concerns about one’s own health, health of the developing fetus, the impending childbirth, hospital and health-care experiences, and/or parenting ability. Pregnancy anxiety is empirically distinct from general anxiety and stress and has been shown to be a better predictor of adverse birth and developmental outcomes [1] through fetal programing of the hypothalamic-pituitary-adrenal (HPA) axis and other mechanisms during pregnancy [4].
Prior studies have documented racial and ethnic disparities in the experience of pregnancy anxiety, such as higher levels among Latina and Black women compared to non-Hispanic white women [5]. Latina women are an understudied group and if they experience higher levels of pregnancy anxiety, the implications for their birth and child developmental outcomes deserve attention. While significant racial/ethnic differences in pregnancy anxiety have not been observed in all studies [6], inconsistencies across studies may be due to not taking into account factors related to acculturation, immigration status, perceived discrimination, and socioeconomic disadvantages.
Acculturation is the multi-dimensional process through which a person from one culture adopts the practices, values, and traits of another culture, and it may be important in understanding patterns of pregnancy anxiety among women residing in the U.S. The degree to which a woman has adopted U.S. cultural norms, values, and practices, in addition to their language preference, nativity, and immigration history, may contribute to variation in levels of pregnancy anxiety, particularly within the Latina population living in the U.S. Two studies with Mexican-origin women found that women who preferred to be interviewed in Spanish and those born outside the U.S. reported more pregnancy anxiety compared to more acculturated women (i.e., English-preference and U.S. born women) [7–8]. One of the studies examining specific pregnancy-related concerns found that less acculturated women had more concerns about labor and delivery, while more acculturated women were more worried about the baby’s development [7]. An earlier qualitative study on recently immigrated Latinas living in the U.S. further suggested that higher maternal mortality rates in their home countries may increase their concerns about labor and delivery even when in the U.S. because of past experiences [9]. Studies that investigate ethnic and cultural variations in specific worries and concerns about pregnancy can provide a better understanding of pregnancy anxiety and the risk posed to offspring within distinct sociocultural contexts that, until now, have been largely overlooked in the literature.
Several prospective studies have found that pregnancy anxiety increases risk for less favorable cognitive and motor outcomes in offspring from infancy through toddlerhood, independent of medical history, socioeconomic status, and postnatal stress [10–11]. Pregnancy anxiety also has been associated with offspring temperament and mental health outcomes including higher levels of negative affect in infants, toddlers, and 6-9-year-old children [12–15]. These associations are notable because negative affect in early in childhood is associated with risk for later mental health and behavior problems [16]. One study, for example, provided evidence that mean levels of pregnancy anxiety measured over the course of pregnancy predicted elevated emotional reactivity in infants at 6 months of age [12]. Another study identified early second trimester (13 to 17 weeks) as a sensitive period in which maternal pregnancy anxiety predicted more negative affectivity in children at 2 years, independent of sociodemographic factors, obstetric risk, and postnatal maternal stress [13]. These studies showed that only pregnancy anxiety, and not general state anxiety, was associated with child temperament outcomes [12–13]. Longitudinal cohort studies of children followed beyond toddler years have found that high levels of pregnancy anxiety over the course of pregnancy predicted impaired executive functioning [14] and greater anxiety [15] in 6- to 9-year-old children. Although some of these pregnancy anxiety studies included diverse samples with respect to participant ethnic, racial and cultural background and controlled for race/ethnicity in their analyses [13–14], none have examined ethnicity or culturally-related variables as hypothesized predictors or moderators of the processes linking pregnancy anxiety and developmental outcomes.
In sum, a growing body of prospective investigations document that pregnancy anxiety predicts adverse child outcomes. However, very few studies examine ethnic and cultural variations in pregnancy anxiety and findings are mixed. More studies are needed to examine these as moderators of the association between pregnancy anxiety and child temperament. The current study had two objectives: (1) To examine differences between non-Hispanic White, and Latina women of two acculturation groups (English-preference and Spanish-preference) in levels of second and third trimester pregnancy anxiety and specific types of concerns; (2) To prospectively test whether the associations between pregnancy anxiety and child negative affect at age 4 years are modified by maternal ethnicity or language preference, operationalized as a proxy for acculturation. Given the risks to mothers and infants associated with pregnancy anxiety, research increasing our understanding of ethnic and cultural variations may help elucidate distinct patterns predicting child outcomes.
Methods
Participants and Procedure
The “Preconception and Prenatal Stress: Pathways to Child Biology and Behavior Study” studied mother-child pairs from Washington, DC, Lake County, IL, and Eastern NC. These women were a subgroup of a larger Community Child Health Research Network (CCHN) study cohort. CCHN was a multi-site research network funded by the National Institutes of Child Health and Human Development. The research network’s purpose was to develop a better understanding of maternal child health disparities [17]. The present study includes a subsample of women from the original CCHN study who were from the three study sites participating in the follow-up and who became pregnant with a subsequent child over the follow-up period.
The current study includes 95 women, who were selected based on self-identification or ethnic identity as Latina/Hispanic (n = 55) or non-Hispanic White (NHW) (n = 40). Latina participants selected their language of preference as English (44%) or Spanish (56%) for participation in the study. All NHW participants selected English. See Table 1 for additional sample demographics. Trained interviewers collected data during structured in-home interviews scheduled in the second trimester (M = 20.36, SD = 4.84 gestational weeks) and third trimester (M = 32.96, SD = 3.94 gestational weeks) of pregnancy, and when children were 3.5 to 4.5 years old (M = 3.80, SD =.38 years). The study was approved by the Institutional Review Boards at each site and mothers provided written and informed consent for themselves and their child.
Table 1.
Sample Demographics (N = 95)
| N (%) | |
|---|---|
| Ethnicity | |
| Non-Hispanic White | 40 (33) |
| Latina | 55 (45) |
| Language Preference (within Latina) | |
| English | 24 (44) |
| Spanish | 31(56) |
| Nativity (within Latina) | |
| US-Born | 10 (18) |
| Foreign-Born | 45 (82) |
| M (SD) | |
| Maternal Age (Years at T3) | 33.72 (5.54) |
| Household Per Capita Income (T1) | $17,520 ($28,424) |
| Education (Years T1) | 12.6 (3.4) |
| Weeks Started Prenatal Care | 7.33 (4.41) |
| Child Sex | |
| Male | 42 (44) |
| Female | 53 (56) |
| Child Age (Years at T3) | 3.80 (.38) |
Note: T1 = 2nd trimester, T2 = 3rd trimester, T3 = child approximately 4 years old.
Measures
Demographic and Medical Variables.
Participants reported basic demographic information including date of birth, education, language preference, nativity (U.S. or foreign born), relationship status with child’s father (married/in a romantic relationship or not married/in a romantic relationship) and per capita household income as well as the timing of prenatal care initiation. Outcomes of pregnancy (birth weight and gestational age at birth) were obtained from medical records.
Language Preference.
Language preference is included in many acculturation measures [18] and has been found to explain most of variation in acculturation scores. In the present report, language preference was used as a proxy measure of acculturation with English-preference indicating more acculturation to U.S. culture and Spanish-preference indicating less acculturation.
Pregnancy Anxiety.
Two measures of pregnancy anxiety were administered in the present study. One was used to capture changes in anxiety about the current pregnancy over time, and the other was administered once to capture some of the specific concerns related to the pregnancy that a mother might be having.
The Pregnancy-Specific Anxiety Scale (PSAS) [19] measures feelings about a current pregnancy and was completed twice, in the second and third trimesters of pregnancy. The four items concerning fear and anxiety related to pregnancy (i.e., anxious or worried, concerned, afraid, panicky) are embedded in the 13-items scale that queries women to report how often they feel specific positive and negative emotions about being pregnant in the past week using a 5-point Likert scale ranging from 1 (Never) to 5 (Always). Responses to the four pregnancy anxiety items were averaged to compute the pregnancy anxiety scores. The measure is available in Spanish and English and has strong face validity and predictive validity [19]. In this sample, internal consistency estimates of reliability were acceptable and comparable in the Spanish-speaking and English-speaking subgroups in the 2nd (α = .72 and .74) and 3rd trimesters (α = .74 and .77).1
The Pregnancy-related Anxiety Scale (PRAS) was used to assess types of worries and concerns specific to pregnancy and the intensity of these concerns [20]2. Mothers completed this scale once during the third trimester. This 10-item instrument, published by Rini et al. (1999) [20], uses a 4-point Likert scale ranging from 1 (Not at all Never) to 4 (Very Much Almost all of the time). Items concern the extent to which women felt worried about childbirth, the health of the baby, and parenting without any time period specified. The measure has been validated in both English and Spanish and has demonstrated predictive validity [20]. Internal consistency reliability was acceptable to strong in the Spanish-speaking and English-speaking subgroups in this sample (α = .83 and .78).
Pregnancy-specific anxiety scores in the second trimester and third trimester were moderately associated (r = .60, p < .001) and both time points were associated with the other pregnancy anxiety measure, the PRAS (r = .35, p < .01 and r = .39, p < .01). A screener for general symptoms of anxiety (OASIS) was also administered prior to conception and scores on this were not significantly related to either pregnancy anxiety measure at any trimester (all p’s >.28) verifying that pregnancy anxiety is a distinct construct from general anxiety.
Depressive symptoms.
Depressive symptoms in mothers were measured using the Center for Epidemiologic Studies Depression Scale (CES-D) at the follow-up study visit scheduled when their child was approximately 4 years old [21]. The 9-item scale assesses how often mothers experienced depressive symptoms during the last 7 days on a scale ranging from 1 (rarely or none of the time) to 4 (most or all of the time). The measure is valid and reliable in English and Spanish [22]. Internal consistency reliability was high and comparable in the Spanish-speaking (α = .83) and English-speaking (α =.87) subgroups in this sample.
Child Negative Affect.
During home visits when the child was approximately 4 years old, mothers responded to the 36-item Very Brief version of the Children’s Behavior Questionnaire or CBQ [23]. The CBQ is widely used in developmental research and has demonstrated reliability, convergent validity, and predictive validity of social behavior across cultures [23]. The Negative Affectivity dimension of the scale includes 12 items to assess how frequently the child expresses of negative emotions such as anger/frustration and fear. Sample items include “[my child] is very difficult to soothe when s/he has become upset” and “[my child] gets quite frustrated when prevented from doing something s/he wants to do.” Internal consistency reliability was similar in the Spanish-speaking (α = .65) and English-speaking (α =.61) subgroups in this sample.
Data Analytic Plan
Multivariate outlier analyses, using DFFITS, DFBETAS, Cook’s distance as criteria, identified no influential cases. Concurrent maternal depression and child sex were covaried in all regression models. Other covariates considered were mothers and child demographic variables (i.e., mother age, income, education, nativity, relationship status, child sex, and child age) and birth outcome variables (birth weight, gestational age). Any covariates associated with either the predictors or outcomes at p < .10 were included in the models; although sex of child was not significant, we chose to include it in the model given evidence of its importance [24]. Per capita household income was marginally associated with lower child negative affect (r = −.19, p < .07) and was therefore also included as a covariate. No other demographic variables or birth outcome variables were related to pregnancy anxiety or negative affect study variables (all p-values > .13).
T-tests were used to examine ethnic differences (NHW vs. Latina) in pregnancy anxiety (measured with the PSAS and PRAS), and timing of prenatal care initiation. One-way ANOVA with Tukey’s LSD post-hoc comparisons were used to test for differences by language preference (NHW vs. Latina English-preference vs. Latina Spanish-preference). Any identified differences by ethnicity or language preference were followed up with item-level analyses. Ethnic and language preference differences in timing of prenatal care initiation were examined to rule out any explanation that differences in study variables could be due to differences in this aspect of care.
Regression models examined main effects of pregnancy-specific anxiety measured with the PSAS in the second and third trimesters on child negative affect scores, covarying for ethnicity, concurrent depression, income, and child sex. These analyses were conducted in order to test for the possibility that the second or third trimesters of pregnancy was a sensitive period. Moderation of significant associations between pregnancy-specific anxiety and child negative affect by ethnicity and/or language preference was tested by examining subgroup regression analyses within groups (NHW vs. Latina English-preference vs. Latina Spanish-preference). When findings were significant, effect sizes were examined.
Results
Differences by Ethnicity and/or Language Preference
Levels of pregnancy anxiety on the two measures did not differ between NHW and Latina women (all p-values > .25). When language preference was considered, there was a statistically significant difference in pregnancy-related anxiety (F = 3.16, p < .05; Table 2). Latina Spanish-preference mothers reported significantly more pregnancy anxiety on this measure compared to Latina English-preference mothers (M = 1.83, SD =.52 vs. M = 1.50, SD = .43) with NHW mothers in between (M = 1.67, SD = .39). Differences did not appear to be related to initiation or prenatal care, as all groups started their prenatal care early (M = 7.33 weeks). Item-level examination of showed that Latina Spanish-preference mothers had more concerns about the childbirth (i.e., “I’m afraid I will be harmed during the delivery” and “I am concerned about developing medical problems during the pregnancy”; F = 2.68, p = .08 and F = 2.72, p = .07), and the baby being harmed “i.e., “I’m worried that the baby could be abnormal”; F = 2.64, p = .08). NHW mothers had more worries about parenting (i.e., “I am concerned about taking care of a new baby”; F = 2.72, p = .07). There were no other significant or marginal post-hoc differences in individual items (Table 3).
Table 2.
Means of Study Variables by Acculturation Group
| Full Sample (N = 95) | Non-Hispanic White (n = 40) | Latina English-Preference (n = 24) | Latina Spanish-Preference (n = 31) | ANOVA F, p-value | |
|---|---|---|---|---|---|
| M (SD); Range | M (SD) | M (SD) | M (SD) | ||
| 2nd trimester Pregnancy-Specific Anxiety | 2.09 (.71); 1 – 3.75 | 1.96 (.81) | 2.48 (.68) | 1.99 (.50) | F = 2.52, p = .09 |
| 3rd trimester Pregnancy-Specific Anxiety | 1.67 (.46); 1 – 2.70 | 2.03 (.92) | 2.03 (.74) | 1.99 (.50) | F = .61, p = .54 |
| Pregnancy-Related Anxiety | 1.96 (.77); 1 - 5 | 1.67 (.39) | 1.50 (.43) | 1.83 (.52) | F = 3.16, p < .05 |
| Concurrent Maternal Depression | 14.67 (5.23); 9 – 34.71 | 14.31 (5.30) | 17.04 (6.41) | 13.31 (4.58) | F = 1.71, p = .19 |
| Prenatal Care (week started) | 7.33 (4.41); 0 - 21 | 7.62 (4.13) | 8.38 (4.07) | 5.90 (5.28) | F = .79, p = .46 |
| Child Negative Affect | 4.13 (.77); 2.17 – 6.33 | 4.12 (.90) | 4.40 (.56) | 3.94 (.69) | F = 2.51, p = .09 |
Table 3.
Item-level Analysis of the PRAS – Differences in Types of Concerns by Acculturation Group
| Non-Hispanic White (n = 40) | Latina English-Preference (n = 24) | Latina Spanish-Preference (n = 31) | ANOVA F, p-value | |
|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | ||
| I am confident of having a normal childbirth* | 3.13 (1.06) | 3.19 (.98) | 3.18 (1.01) | F = .02, p = .98 |
| I think my labor and delivery will go normally* | 3.18 (.80) | 3.50 (.63) | 3.53 (.62) | F = 1.50, p = .23 |
| I have a lot of fear regarding the health of my baby | 1.78 (.67) | 1.44 (.63) | 1.94 (1.03) | F = 1.77, p = .18 |
| I am worried that the baby could be abnormal | 1.61 (.72) | 1.19 (.40) | 1.71 (.85) | F = 2.64, p = .08 |
| I am afraid that I will be harmed during the delivery | 1.39 (.66) | 1.31 (.60) | 1.88 (1.05) | F = 2.68, p = .08 |
| I am concerned about how the baby is growing and developing inside of me | 1.61 (.58) | 1.75 (.86) | 1.71 (.77) | F = .20, p = .82 |
| I am concerned about losing the baby | 1.43 (.59) | 1.44 (.81) | 1.53 (.72) | F = .11, p = .90 |
| I am concerned about having a difficult labor | 1.83 (.78) | 1.81 (.98) | 2.06 (.97) | F = .42, p = .66 |
| I am concerned about taking care of a new baby | 1.87 (.87) | 1.44 (.73) | 1.35 (.61) | F = 2.72, p = .07 |
| I am concerned about developing medical problems during the pregnancy | 1.39 (.50) | 1.63 (.89) | 1.88 (.60) | F = 2.72, p = .07 |
Reverse-scored for full scale scoring
Maternal Pregnancy-Specific Anxiety and Child Negative Affect
Higher maternal pregnancy-specific in the second trimester was associated with higher scores on child negative affect at age 4 (r = .36, p < .01). When co-varying ethnicity, income, concurrent depression, and child sex this effect remained (b = .35, β = .33, p < .05) (see Table 5). The effect size was small. Pregnancy-specific anxiety in the third trimester did not relate to child negative affect (r = .09, p = .46; Table 4), or predict negative affect in adjusted analyses (b = .05, β = .05, p = .63).
Table 5.
Model Results – Main Effects (N = 95)
| 2nd Trimester | 3rd Trimester | |
|---|---|---|
| Predictors | b (SE) | b (SE) |
| Pregnancy-Specific Anxiety | .35 (.15)* | .05 (.13) |
| Concurrent Depression | .00 (.02) | .02 (.02) |
| Income | −.01 (.00)† | −.01 (.00) |
| Sex (1=male, 2 = female) | −.06 (.15) | −.04 (.16) |
| Ethnicity (0 = NHW, 1= Latina) | −.16 (.17) | −.07 (.16) |
Note:
p < .10;
p < 05;
p < .01
Table 4.
Bivariate Correlations among Study Variables (N = 95)
| 2nd trimester Pregnancy-Specific Anxiety | 3rd trimester Pregnancy-Specific Anxiety | Pregnancy-Related Anxiety | Concurrent Maternal Depression | |
|---|---|---|---|---|
| 2nd trimester Pregnancy-Specific Anxiety | 1 | |||
| 3rd trimester Pregnancy-Specific Anxiety | .60** | 1 | ||
| Pregnancy-Related Anxiety | .35** | 39** | 1 | |
| Concurrent Maternal Depression | .45** | .33** | −.01 | 1 |
| Child Negative Affect | .36** | .09 | −.05 | .21** |
Note:
p < .05
p < .01
Subgroup regression models demonstrated significant language preference differences in the association between pregnancy-specific anxiety in the second trimester and child negative affect (see Figure 1). Adjusting for income, concurrent depression, and child sex, pregnancy-specific anxiety in the second trimester predicted higher negative affect in children of Latina Spanish-preference mothers (b =.88, β = .60, p = .004), a moderate-sized effect. In Latina English-preference and NHW mothers, associations between second trimester pregnancy-specific anxiety and child negative affect, were trending in a similar direction, but did not reach significance (b = .29, β = .38, p = .17 and b = .27, β = .24, p = 21, respectively).
Figure 1. Acculturation Differences in the Effect of Pregnancy-Specific Anxiety on Child Negative Affect.
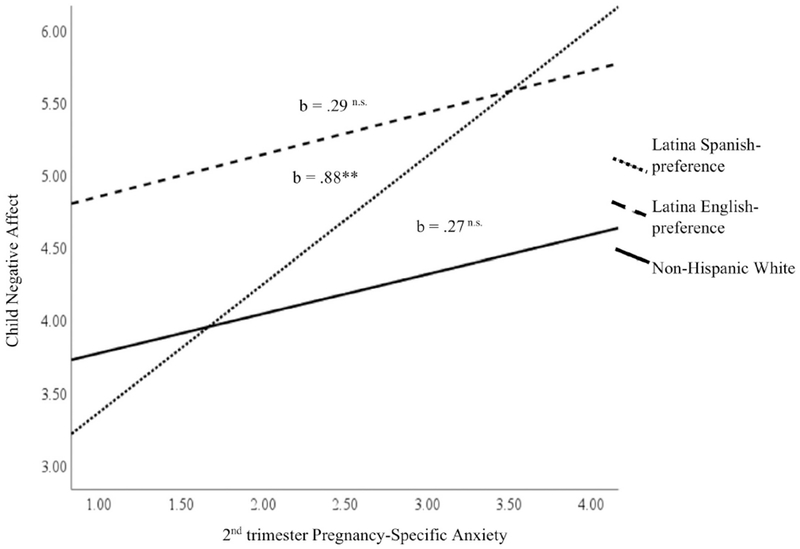
Note. ** < .01; n.s. non-significant
Discussion
The current study examined ethnic and acculturation variation in pregnancy anxiety and moderation of associations with an early childhood outcome. Maternal acculturation in the U.S. was measured using language preference, a common proxy for acculturation. We found that Latina women with Spanish-language preference, i.e., less U.S. acculturation, reported the most concerns related to their pregnancy and, in addition, the nature of their concerns differed. Findings further indicated that pregnancy-specific anxiety in the second (but not the third) trimester of pregnancy predicted negative affect in children at 4 years of age. This association was not moderated by ethnicity, but was moderated by acculturation, such that the association was strongest among women who preferred to be interviewed in Spanish (i.e., less acculturated Latina women). These effects were not explained by potential confounds, such as concurrent depressive symptoms, income, or child sex. Similar, but smaller associations were evident in non-Hispanic White women and more acculturated Latinas (i.e., those who preferred to be interviewed in English).
Consistent with two previous studies with U.S. residing Mexican and Mexican-American samples [7–8], Latina women in this study who preferred to be interviewed in Spanish reported more concerns about their pregnancy compared to Latina women who preferred English. This suggests that differences in pregnancy anxiety among Latinas in the U.S. may be related to level of acculturation, and related factors, and therefore only emerge when language preference and acculturation are considered. Our findings are also consistent with previous work demonstrating that pregnancy anxiety in less acculturated women tends to be driven by worries about interactions with the medical system as well as personal health and safety during the birth [9]. These differences were not explained by differential access to prenatal care because the groups initiated prenatal care at approximately the same time in their pregnancies.
Differences could relate to concerns about birth-related experiences in their home countries, uncertainties about the medical systems in the U.S., worries related to ability to obtain healthcare as an immigrant, and/or discrepancies in quality or consistency of such care. Previous literature studying general state anxiety in Latina women during pregnancy has pointed to acculturative stress as a salient factor predicting elevated levels early in pregnancy [25]. Acculturative stress, and the cumulative effects of multiple stressors, may also play a role in the intensity of pregnancy anxiety in Spanish-speaking women in this study, who may be earlier in the acculturation process and experiencing ongoing worries about personal safety and family security related to their immigration status in this country. This work highlights the need for future research on the effects of unique sources of distress for less-acculturated Latina women, such as immigration-related stress including deportation threat and border-crossing trauma.
Understanding the effects of maternal negative emotional experiences on the stress response system may help elucidate why pregnancy anxiety is associated with child negative affect, and why effect sizes were stronger for less acculturated Latina women. Uncontrollable stressors have been found to produce more exaggerated stress responses [26] compared to stressors within the individual’s control. Therefore, even if women endorse similar levels of pregnancy-specific anxiety, the types of things they worry about may differ in controllability (e.g. parenting versus labor) and differentially affect the extent to which the mother’s physiology is stress responsive in utero. Consistent with this, the less acculturated group worried more about pregnancy and childbirth complications, risks over which they likely did not feel they had much control. Conversely, non-Hispanic White mothers had more concerns about their ability to parent effectively, a skill they could theoretically more easily control and improve for example, by accessing social support or other resources). Therefore, the types of pregnancy-related concerns and the extent to which a pregnant woman feels efficacious in her ability to manage them appear to have implications for later child functioning and deserves further attention.
Pregnancy-specific anxiety in second trimester was associated with the greatest developmental risk among less acculturated Latina women. This lends support to translational work involving culturally-sensitive screening tools to identify women at risk, particularly early in the pregnancy, and effective resources to reduce concerns for this population. Screening regarding specific maternal worries could help tailor support and referrals accordingly. For example, if a mother expresses anxiety about childbirth, prenatal care providers can ensure the patient has access to birth preparation education in the preferred language and understands information provided. Providers may also offer additional opportunities to answer questions or communicate with family members.
The current findings add to previous work showing strong associations between second trimester pregnancy anxiety and adverse developmental outcomes [10,13]. Significant findings in the second trimester are notable because this is one sensitive period when the fetus is rapidly developing and appears to be at risk for later negative temperament, and less favorable cognitive, and mental health outcomes [10,13]. More research is needed to identify plausible mechanisms through which pregnancy anxiety may contribute to fetal programming and subsequent adverse developmental outcomes at this sensitive stage. One candidate mechanism involves HPA processes whereby increased cortisol secretion in pregnant women with higher in pregnancy anxiety [27] and higher placental corticotropin-releasing hormone (pCRH) in the maternal and fetal bloodstream [28] can adversely affect fetal development [29]. Another study linked prenatal anxiety with a downregulation of placental 11β-HSD2, the enzyme that metabolizes and essentially inactivates cortisol, resulting in more fetal exposure to maternal cortisol [30]. Although cortisol exposure is important to the fetus at later stages in the pregnancy (e.g., to prepare for delivery), excess exposure can be detrimental during critical stages in early fetal development when the fetus is meant to be protected from this hormone [1]. These disruptions to the fetal environment can result not only in changes in hormonal exposures, but also in epigenetic programming with effects throughout the life course [4].
Specific features of our study design and measures bear mention as they pertain to the findings. First, the sample size and modest main effect of pregnancy anxiety in the second trimester on child negative affect should be taken into account when evaluating the findings. However, the moderate effect size within the Spanish-speaking Latina subsample certainly warrants follow-up with larger samples. Second, pregnancy anxiety was not assessed in the first trimester, precluding the ability to test for earlier sensitive periods in pregnancy. Third, this study did not assess general anxiety during pregnancy limiting the ability to differentiate any effects from the associations with pregnancy anxiety, though the literature points to pregnancy anxiety as a strong and independent predictor of birth and developmental outcomes [1, 13]. Fourth, although measures were collected longitudinally over a fairly long time period, mother-report was used to assess both pregnancy anxiety and child negative affect, increasing the possibility of confounding effects due to self-report bias. Objective evaluations of child negative affect in future research would bolster confidence in the effects. Finally, using language preference as a proxy measure for acculturation is a possible weakness. Although this approach is commonly used [18], assessment of acculturation with validated multi-item measures might identify useful aspects of cultural value systems. Future research should also examine traditional cultural values that could amplify or reduce pregnancy anxiety in Latinas [7] or factors such as familism that might protect against adverse effects during the acculturation process.
In sum, we found that pregnancy-specific anxiety in the second trimester of pregnancy was related to child negative affect in early childhood especially for offspring of less acculturated Latina women, who tend to be more concerned about their health during pregnancy and their own safety during childbirth as compared to non-Hispanic white women and more acculturated Latina women. These findings highlight the need for effective support for expecting mothers experiencing high levels of pregnancy anxiety, particularly for Spanish-speaking Latina women, in order to reduce health disparities, improve mothers’ pregnancy experience, and promote better developmental outcomes in children years later.
Highlights.
Less acculturated U.S. Latinas worry about their health and safety in childbirth
Non-Hispanic White women in the U.S. worry more about their future parenting
Pregnancy anxiety in 2nd trimester increases risk for child negativity at age 4
Pregnancy anxiety risk for children is highest among less acculturated Latinas
Acknowledgments
Funding Sources: The CCHN is supported through cooperative agreements with the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD; U HD44207, U HD44219, U HD44226, U HD44245, U HD44253, U HD54791, U HD54019, U HD44226-05S1, U HD44245-06S1, R03 HD59584, 5R01HD072021-05) and the National Institute for Nursing Research (NINR; U NR008929). Nicole E. Mahrer was supported by the National Institute of Mental Health (5 T32 MH015750; Christine Dunkel Schetter).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: None Declared
References
- [1].Dunkel Schetter C, Psychological science on pregnancy: Stress processes, biopsychosocial models, and emerging research issues, Annu. Rev. Psychol 62 (2011) 531–558. doi: 10.1146/annurev.psych.031809.130727. [DOI] [PubMed] [Google Scholar]
- [2].Guardino CM, Dunkel Schetter C, Understanding pregnancy anxiety: Concepts, correlates, and consequences, Zero to Three. 34 (2014) 12–21. https://eric.ed.gov/?id=EJ1125704 (accessed May 19, 2019). [Google Scholar]
- [3].Huizink AC, Mulder EJH, Robles De Medina PG, Visser GHA, Buitelaar JK, Is pregnancy anxiety a distinctive syndrome?, Early Hum. Dev 79 (2004) 81–91. doi: 10.1016/j.earlhumdev.2004.04.014. [DOI] [PubMed] [Google Scholar]
- [4].Vaiserman AM, Epigenetic programming by early-life stress: Evidence from human populations, Dev. Dyn 244 (2015) 254–265. doi: 10.1002/dvdy.24211. [DOI] [PubMed] [Google Scholar]
- [5].Campos B, Dunkel Schetter C, Abdou CM, Hobel CJ, Glynn LM, Sandman CA, Familialism, social support, and stress: Positive implications for pregnant Latinas., Cult. Divers. Ethn. Minor. Psychol 14 (2008) 155–162. doi: 10.1037/1099-9809.14.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Parker Dominguez T, Dunkel Schetter C, Glynn LM, Hobel C, Sandman CA, Racial differences in birth outcomes: The role of general, pregnancy, and racism stress., Heal. Psychol 27 (2008) 194–203. doi: 10.1037/0278-6133.27.2.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Campos B, Schetter CD, Walsh JA, Schenker M, Sharpening the focus on acculturative change: ARSMA-II, stress, pregnancy anxiety, and infant birthweight in recently immigrated latinas, Hisp. J. Behav. Sci 29 (2007) 209–224. doi: 10.1177/0739986307300841. [DOI] [Google Scholar]
- [8].Fleuriet KJ, Sunil TS, Perceived social stress, pregnancy-related anxiety, depression and subjective social status among pregnant Mexican and Mexican American women in South Texas, J. Heal. Care Poor Underserved. 25 (2014) 546–561. doi: 10.1353/hpu.2014.0092. [DOI] [PubMed] [Google Scholar]
- [9].Scrimshaw SC, Zambrana RE, Dunkel Schetter C, Issues in Latino women’s health: Myths and challenges, in: Ruzek SB, Oleson VL, Clarke AE (Eds.), Women’s Heal. Complexities Differ, Ohio University Press, 1997, pp. 329–347. [Google Scholar]
- [10].Huizink AC, Robles De Medina PG, Mulder EJH, Visser GHA, Buitelaar JK, Psychological measures of prenatal stress as predictors of infant temperament, J. Am. Acad. Child Adolesc. Psychiatry. 41 (2002) 1078–1085. doi: 10.1097/00004583-200209000-00008. [DOI] [PubMed] [Google Scholar]
- [11].Davis EP, Sandman CA, The timing of prenatal exposure to maternal cortisol and psychosocial stress is associated with human infant cognitive development, Child Dev. 81 (2010) 131–148. doi: 10.1111/j.1467-8624.2009.01385.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Nolvi S, Karlsson L, Bridgett DJ, Korja R, Huizink AC, Kataja E-L, Karlsson H, Maternal prenatal stress and infant emotional reactivity six months postpartum., J. Affect. Disord 199 (2016) 163–70. doi: 10.1016/j.jad.2016.04.020. [DOI] [PubMed] [Google Scholar]
- [13].Blair MM, Glynn LM, Sandman CA, Davis EP, Prenatal maternal anxiety and early childhood temperament, Stress. 14 (2011) 644–651. doi: 10.3109/10253890.2011.594121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Buss C, Davis EP, Hobel CJ, Sandman CA, Maternal pregnancy-specific anxiety is associated with child executive function at 69 years age, Stress. 14 (2011) 665–676. doi: 10.3109/10253890.2011.623250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Davis EP, Sandman CA, Prenatal psychobiological predictors of anxiety risk in preadolescent children, Psychoneuroendocrinolo 37 (2012) 1224–1233. doi: 10.1016/j.psyneuen.2011.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Dougherty LR, Klein DN, Durbin CE, Hayden EP, Olino TM, Temperamental positive and negative emotionality and children’s depressive symptoms: A longitudinal prospective study from age three to age ten, J. Soc. Clin. Psychol 29 (2010) 462–488. doi: 10.1521/jscp.2010.29.4.462. [DOI] [Google Scholar]
- [17].Ramey SL, Schafer P, DeClerque JL, Lanzi RG, Hobel C, Shalowitz M, Chinchilli V, Raju TNK, The Preconception Stress and Resiliency Pathways Model: A multi-Level framework on maternal, paternal, and child health disparities derived by community-based participatory research, Matern. Child Heal. J 19 (2015) 707–719. doi: 10.1007/s10995-014-1581-1. [DOI] [PubMed] [Google Scholar]
- [18].Thomson MD, Hoffman-Goetz L, Defining and measuring acculturation: A systematic review of public health studies with Hispanic populations in the United States, Soc. Sci. Med 69 (2009) 983–991. doi: 10.1016/j.socscimed.2009.05.011 [DOI] [PubMed] [Google Scholar]
- [19].Roesch SC, Dunkel Schetter C, Woo G, Hobel CJ, Modeling the types and timing of stress in pregnancy, Anxiety StressCoping. 17 (2004) 87–102. doi: 10.1080/1061580031000123667. [DOI] [Google Scholar]
- [20].Rini CK, Dunkel Schetter C, Wadhwa PD, Sandman CA, Psychological adaptation and birth outcomes: The role of personal resources, stress, and sociocultural context in pregnancy, Heal. Psychol 18 (1999) 333–345. doi: 10.1037/0278-6133.18.4.333. [DOI] [PubMed] [Google Scholar]
- [21].Santor DA, Coyne JC, Shortening the CES-D to improve its ability to detect cases of depression, Psychol. Assess 9 (1997) 233–243. doi: 10.1037/1040-3590.9.3.233. [DOI] [Google Scholar]
- [22].Grzywacz JG, Hovey JD, Seligman LD, Arcury TA, Quandt SA, Evaluating short-form versions of the CES-D for measuring depressive symptoms among immigrants from Mexico, Hisp. J. Behav. Sci 28 (2006) 404–424. doi: 10.1177/0739986306290645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Rothbart MK, Ahadi SA, Hershey KL, Fisher P, Investigations of temperament at three to seven years: The children’s behavior questionnaire, Child Dev. 72 (2001) 1394–1408. doi: 10.1111/1467-8624.00355. [DOI] [PubMed] [Google Scholar]
- [24].Putnam SP, Gartstein MA, Rothbart MK. Measurement of fine-grained aspects of toddler temperament: The Early Childhood Behavior Questionnaire. Infant Behav.Dev 29 (2006) 386–401. doi: 10.1016/j.infbeh.2006.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Preciado A, D’Anna-Hemandez K. Acculturative stress is associated with trajectory of anxiety symptoms during pregnancy in Mexican-American women. J Anxiety Disord. 48 (2017) 28–35. doi: 10.1016/j.janxdis.2016.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Peters ML, Godaert GLR, Ballieux RE, Brosschot JF, Sweep FCGJ, Swinkels LMJW, Van Vliet M, Heijnen CJ, Immune responses to experimental stress: Effects of mental effort and uncontrollability, Psychosom. Med 61 (1999) 513–524. doi: 10.1097/00006842-199907000-00016. [DOI] [PubMed] [Google Scholar]
- [27].Kane HS, Dunkel Schetter C, Glynn LM, Hobel CJ, Sandman CA, Pregnancy anxiety and prenatal cortisol trajectories, Biol. Psychol 100 (2014) 13–19. doi: 10.1016/j.biopsycho.2014.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Ramos IF, Guardino CM, Mansolf M, Glynn LM, Sandman CA, Hobel CJ, Dunkel Schetter C, Pregnancy anxiety predicts shorter gestation in Latina and non-Latina white women: The role of placental corticotrophin-releasing hormone, Psychoneuroendocrinology. 99 (2019) 166–173. doi: 10.1016/j.psyneuen.2018.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Davis EP, Glynn LM, Schetter CD, Hobel C, Chicz-Demet A, Sandman CA. Corticotropin-releasing hormone during pregnancy is associated with infant temperament. Dev. Neurosci 27 (2005) 299–305. doi: 10.1159/000086709. [DOI] [PubMed] [Google Scholar]
- [30].O’Donnell KJ, Bugge Jensen A, Freeman L, Khalife N, O’Connor TG, Glover V, Maternal prenatal anxiety and downregulation of placental 11β-HSD2, Psychoneuroendocrinology. 37 (2012) 818–826. doi: 10.1016/j.psyneuen.2011.09.014. [DOI] [PubMed] [Google Scholar]


