Abstract
Introduction
Treat-and-extend (T&E) and pro re nata (PRN; ‘as needed’) regimens of intravitreal anti-vascular endothelial growth factor (VEGF) treatment have been found to reduce the injection burden on patients and improve the cost effectiveness of the treatment of macular edema. The aim of this study was to assess the effectiveness of a T&E regimen of aflibercept, in a clinical setting, in patients with diabetic macular edema (DME) who were either intravitreal anti-VEGF therapy naive or with minimal exposure to anti-VEGF (≤ 6 treatments) in the previous 12 months.
Methods
This prospective, single arm, open label study recruited patients with DME (macular thickness of ≥ 300 µm) and best-corrected visual acuity (BCVA) between 28-78 ETDRS letters. Participants received five loading doses of intravitreal aflibercept at 4-weekly intervals. BCVA measurements and macular optical coherence tomography were performed at each visit. If no disease activity was detected, treatment intervals were increased by 2 weeks to a maximum of 12 weeks. Outcome measures included: changes in BCVA and retinal anatomical measures (central foveal thickness [CFT] and central macular volume within 6 mm of the fovea [CSVol]) between baseline and 2 years, patient treatment intervals; and adverse events.
Results
Of the 36 patients who provided informed consent to participate in the study and were screened, 26 patients (eyes) were eligible to participate in the study. After regression analysis, adjustment for repeated measures, and significant covariates, the mean BCVA increased by 3.8 letters (95% confidence interval [CI] 1.1, 6.4) and the CFT and CSVol decreased by 127.2 µm (95% CI 91.7, 162.5) and 1.6 mm3 (95% CI 1.2, 2.0), respectively, over the course of the study. In the second year, 16 of the 25 patients still participating had their treatment intervals extended to 12 weeks. There was no evidence of any new adverse events that would require changes to the aflibercept safety profile.
Conclusion
For the majority of patients presenting with DME, a T&E regimen of aflibercept in the first 2 years of therapy is a practical alternative to PRN treatment with regular review.
Trial Registration
Australian New Zealand Clinical Trials Registry number, ACTRN12618000428268.
Funding
This investigator-initiated study was supported by Bayer Australia Ltd. who provided the study treatment and some financial assistance.
Keywords: Aflibercept, Anti-vascular endothelial growth factor, Clinical setting, Diabetic macular oedema, Treat and extend
Key Summary Points
| Why do this study? |
| Regular intravitreal injections of anti-vascular endothelial growth factor (VEGF) are currently the first-line treatment for centrally located diabetic macular edema (DME). |
| In clinical trials, treat and extend (T&E) and pro re nata (PRN; ‘as needed’) regimens of intravitreal anti-VEGF treatment have been found to reduce the injection burden on patients and improve the cost effectiveness of the treatment of macular edema. |
| The aim of this study was to assess the effectiveness of a T&E regimen of aflibercept, in a clinical setting, in patients presenting DME either intravitreal anti-VEGF therapy naive or with relapsed DME with minimal exposure (≤ 6 treatments) to anti-VEGF in the previous 12 months. |
| What did we learn? |
| At the end of 2 years, 75% of the participants remaining in the study had their treatment intervals extended to the maximum 12 weeks with no signs of disease activity, indicating that a T&E regimen of aflibercept is a practical alternative to PRN treatment with regular review. |
Introduction
Diabetes accounts for a significant burden of global chronic disease [1], with the ophthalmic complications of diabetic retinopathy (DR) and diabetic macular edema (DME) representing the commonest causes of early onset blindness worldwide [2]. More than 1.7 million (7%) Australians live with diabetes. The prevalence of the disease increases with age and is estimated to be threefold higher in aboriginal Australians than in Caucasian Australians [3]. In the 2015–16 National Eye Health Survey (NEHS) of Australian adults (> 40 years of age), 29% of those who self-reported diabetes also had DR; 8% had vision-threatening DR and 4% had clinically significant DME [4].
In the mid-1980s laser macular photocoagulation was recommended as the gold standard treatment for DME [5]. However, detection of high levels of vascular endothelial growth factor (VEGF) in eyes with macular edema secondary to microvascular disease (notably age-related macular degeneration, retinal vein occlusion and DME) [6] and a greater understanding of its role in the pathogenesis of these conditions resulted in the development of pharmaceutical agents targeting VEGF receptors [7, 8]. Furthermore, consistent evidence from clinical trials and clinical practice demonstrating the superiority of anti-VEGF treatment over laser treatment, particularly in cases where the efficacy outcome of interest was visual acuity rather than anatomical response [9–13], has resulted in the adoption of anti-VEGFs as first-line therapy for the treatment of macular edema.
In Australia, aflibercept (Eylea; Regeneron, Tarrytown, NY, USA) and ranibizumab (Lucentis®; Genentech, Inc., San Francisco, CA, USA) are the only anti-VEGF agents indicated for the treatment of DME. Both have been listed for re-imbursement on the Pharmaceutical Benefits Scheme for treatment of this disease since 1 October 2015. Prior to this listing, the VEGF inhibitor used to treat DME was off-label bevacizumab (Avastin™; Genentech, Inc., San Francisco, CA, USA). Bevacizumab and ranibizumab are both recombinant antibodies to VEGF-A (the latter is a small Fab antibody fragment which binds to all isoforms of VEGF-A), while aflibercept is a soluble recombinant human protein attached to the Fc portion of an immunoglobulin G molecule; it has a higher affinity for both VEGF-A and VEGF-B, as well as to placental growth factors PIGF-1 and PIGF-2 that have also been identified as being important in the pathogenesis of DME [14, 15].
In clinical trials and clinical practice treat and extend (T&E) and pro re nata (PRN; ‘as needed’) regimens of anti-VEGF treatment, in response to signs of disease activity, have been found to be beneficial in reducing the injection burden on patients and improving the cost effectiveness of treatment with little reduction in clinical outcomes [16].
The aim of this study, initiated prior to aflibercept being indicated for the treatment of DME in Australia, was to assess the effectiveness of a 2-year T&E regimen of aflibercept, in a clinical setting, in patients with DME with no history of intravitreal anti-VEGF therapy or in those with relapsed DME with minimal exposure (≤ 6 previous treatments) in the 12 months prior to screening.
Methods
Study Design
This study was an open-label, prospective, investigator-led interventional study in a clinic setting. Institutional ethics approval was obtained from the Tasmanian Health and Medical Research Ethics Committee (THMREC) prior to study commencement (Protocol Ref No: H0014556) and registered with the Australian New Zealand Clinical Trials Registry (ANZCTR; ACTRN12618000428268). Informed consent was obtained from all participants prior to enrollment, in accordance with Springer’s ethical policies. The study adhered to the tenets of the 1964 Declaration of Helsinki, as revised in 2013, and to the protocol approved by THMREC.
Participants
Patients aged > 18 years with type 1 or type 2 diabetes mellitus who presented for routine ophthalmologic examination and found to have DME with central macular involvement were invited to participate in the study. Eligible participants had a study eye that met the following criteria: a best-corrected baseline visual acuity (BCVA) of between 24 and 78 letters on the Early Treatment Diabetic Retinopathy Study (ETDRS) chart at 3 m; central retinal thickness within 1 mm of the fovea (CFT) of ≥ 300 µm by spectral domain-optical coherence tomography (OCT; Heidelberg Spectralis; Heidelberg Engineering Inc., Heidelberg, Germany); no anti-angiogenic drug treatment in the study eye in the preceding 120 days and in the previous 90 days in the fellow eye; no more than two macular laser photocoagulation treatments in the previous 6 months; no pan-retinal photocoagulation (PRP) or macular laser photocoagulation in the previous 90 days; no intra-ocular or peri-ocular corticosteroid treatment in the previous 120 days and no evidence of ocular or peri-ocular infection, active proliferative diabetic retinopathy, visually significant cataract, uncontrolled glaucoma, or other macular pathology (e.g., laser burns or scars, wet age-related macular degeneration, or macular holes) that might influence the outcomes of the study. Patients were also excluded if they had glycosylated serum hemoglobin (HbA1c) > 12% or any other unstable systemic medical condition at baseline. Diagnosis was confirmed by fluorescein angiogram, and only one eye was selected as the study eye. If the patient had two eyes with DME the most recently diagnosed eye was selected as the study eye.
Study Assessments
Assessments at each study visit included BCVA intra-ocular pressure (Icare; Tiolat Oy, Helsinki, Finland), OCT scans and slit lamp examination. At baseline and study completion, participants also underwent color fundus photography (CentreVue Digital Retinography System; Centervue S.p.A, Padova, Italy) and fluorescein angiography (Heidelberg Spectralis; Heidelberg Engineering Inc.) if indicated. At each follow-up visit, participants were asked about any adverse events and any changes in their health or medications. All serious adverse events were reported to the manufacturers and the local ethics committee.
Treatment Protocol
All participants were given five 4-weekly loading doses of 2 mg/0.05 mL aflibercept from single-use vials provided by Bayer Australia Ltd. (Pymble, NSW, Australia). The intravitreal injections were performed according to the regular procedure of each investigator using a 30-gauge needle inserted after local anesthesia and using aseptic technique. Post-injection, hand movement perception was confirmed, the eye was irrigated with saline, and artificial tear drops were administered if required.
After the first five monthly loading injections, treatment intervals were determined according to a T&E regimen, based on the presence of disease activity, i.e., a loss of ≥ 5 BCVA letters at any time during the study (considered by the treating physician to be attributable to disease activity) or persistent macular edema (macular thickness of ≥ 300 µm or increase in CFT of 50 µm). If none of these criteria were met, the participant’s injection interval was increased by 2 weeks until a maximum of 12-weekly dosing was attained. If either criteria were met, the injection interval decreased by 2 weeks (if > 4 weeks), or returned to 4 weeks (at the discretion of the investigator) until disease activity was minimized. Participants who experienced significant and rapid progression of disease or became unresponsive to aflibercept had the option to withdraw and have rescue therapy, such as, for example, laser photocoagulation therapy or intravitreal steroids.
Outcome Measures
The primary outcome measures were the mean change in BCVA and the proportion of participants with a change in BCVA of ≥ 5 and ≥ 10 letters between baseline and 2 years of follow-up. Secondary efficacy endpoints were the mean changes in CFT and central macular volume within 6 mm of the fovea (CSVol) between baseline and 2 years and the frequency of aflibercept injections over the course of the study.
Statistical Analysis
Statistical analyses were performed in the R statistical environment (R Development Core Team, 2014; R Foundation for Statistical Computing, Vienna, Austria). Continuous and categorical variables were summarized as means with standard deviation (SD) and frequencies (percentages), respectively, as appropriate. Mean changes in continuous variables were assessed using linear mixed models regression to account for the correlation in observations from the same individual over time. Predictors included in the full model for each outcome variable were visit, age, sex, intra-ocular pressure, treatment number, lens status, previous laser treatment (PRP), the number of PRP treatments, and baseline HbA1c. Final models for each outcome were generated using stepwise regression to eliminate non-significant variables. A binomial variable was also used to evaluate the effect of presenting with BCVA < 69 vs. ≥ 69 ETDRS letters at baseline. For all analyses p values of < 0.05 were considered to be statistically significant. The results of this study are presented in accordance with intention-to-treat analysis, with the outcome measures of three patients who did not complete the study carried forward.
Results
Baseline Characteristics
Of the 36 patients consented and screened, 26 (61% male) were eligible to participate in the study and completed the loading phase. Participant characteristics are presented in Table 1. Of the 26 eyes included in the study, nine of 14 right eyes and eight of 12 left eyes were phakic. At baseline, the mean BCVA was ETDRS 69.7 (range 59–78) letters and the mean CFT and CSVol were 416.6 (range 309–725) µm and 10.0 (range 7.4–13.5) mm3, respectively. Male participants had a slightly higher BCVA, with correspondingly lower CFT and CSVol, than female participants, but none of these differences were statistical significance.
Table 1.
Participant characteristics at baseline
| Participant characteristics | All | Males | Females |
|---|---|---|---|
| Patients, n (right eyes) | 26 (14) | 16 (9) | 10 (5) |
| Age, years | 67.4 (10.6) | 68.8 (9.9) | 62.2 (11.70 |
| Phakic:pseudophakic eyes, n | 9:17 | 6:10 | 3:7 |
| BCVA, EDTRS letters | 69.7 (6.2) | 70.9 (6.3) | 67.8 (5.6) |
| CFT, µm | 416.6 (121.3) | 404.4 (93.5) | 436.1 (157.1) |
| CSVol mm3 | 10.0 (1.6) | 10.0 (1.5) | 10.3 (1.5) |
| Diabetes mellitus type 1, n | 3 | 2 | 1 |
| Insulin treatment, n | 22 | 13 | 9 |
| Baseline HbA1c, % | 8.16 (1.32) | 7.8 (1.36) | 8.64 (1.17) |
| De novo ME, n | 15 | 11 | 4 |
| Diabetic retinopathy history, years | 4.1 (3.4) | 3.8 (3.0) | 4.7 (3.2) |
| Previous laser, n | 13 | 9 | 4 |
| Previous anti-VEGF, n | 7 | 4 | 3 |
Values in table are presented as the mean with the standard deviation (SD) in parenthesis, unless indicated otherwise
BCVA Best-corrected visual acuity measured after refraction using Early Treatment Diabetic Retinopathy Study (ETDRS) charts, CFT central retinal thickness within 1 mm of the fovea, CSVol central subfoveal volume within 6 mm of the fovea, HbA1c glycosylated hemoglobin, ME macular edema, n number of participants (eyes) in that category, VEGF vascular endothelial growth factor
Eighteen participants (12 male, 6 female) had a BCVA of ≥ 69 (mean 73.2, SD 3.4) letters, and eight participants (4 male, 4 female) had a BCVA of < 69 (mean 61.9, SD 2.7) letters, but there were no significant differences in mean CFT or CSVol of eyes with BCVA of < 69 letters and BCVA ≥ 69 letters: 394.4 (SD 81.4) vs. 426.4 µm (SD 134.4) and 9.72 (SD 1.4) vs. 10.3 mm3 (SD 1.72), respectively.
At baseline, 21 eyes (81.7%) had severe and five eyes had moderate DME [17], and review of fundal photographs indicated that 12 eyes had mild, eight had moderate, and six had severe non-proliferative diabetic retinopathy. Thirteen eyes had previously been treated with PRP and seven eyes previously treated with bevacizumab had a mean of 3.1 (SD 2.7) injections in the year prior to screening. Baseline HbA1c ranged from 6.2 to 11.1%, and although the majority of participants (22/26) were insulin dependent only three had type 1 diabetes.
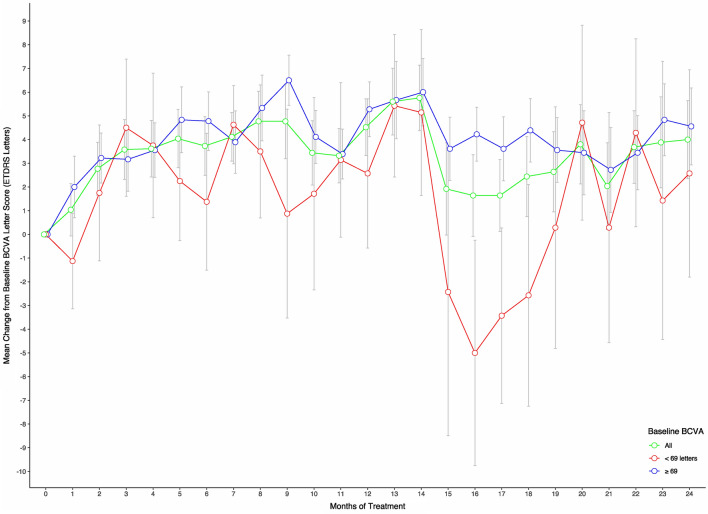
Visual Acuity
Mean BCVA and a summary of the change in BCVA over the course of the study are presented in Table 2. After 2 years of aflibercept treatment, the BCVA of 12 participants (46%) had improved by ≥ 5 letters and a further eight participants had maintained their baseline BCVA (Table 2). The mean change in BCVA at 6, 12, and 18 months and 2 years after adjustment for significant covariates, namely, age, sex, and baseline HbA1c, is presented for the overall study population in Table 3 and illustrated according to baseline BCVA (< 69 letters or ≥ 69 letters) in Fig. 1. The greatest improvements in vision were observed within the first few months of treatment. At 6 months, the mean improvement in visual acuity was 3.7 letters. Thereafter, BCVA varied in a see-saw pattern, being most evident in participants with a baseline BCVA of < 69 letters. Although the initial gains in vision were maintained throughout study duration, there was no additional significant improvement in BCVA between 6 months and 2 years (Table 3) and no statistically significant difference between the mean vision gained in eyes with BCVA ≥ 69 letters and those with BCVA < 69 letters at baseline (Fig. 1) or between naive participants and those with previous bevacizumab exposure.
Table 2.
Participant vision and retinal morphology over the study period
| BCVA and retinal morphology | Time post commencement of aflibercept treatment | |||
|---|---|---|---|---|
| 6 months | 1 year | 18 months | 2 years | |
| Mean number of BCVA letters | 73.5 (9.4) | 74.3 (9.4) | 72.3 (12.0) | 73.8 (10.7) |
| Change in number of BCVA (letters), n | ||||
| Gain of ≥ 15 letters | 0 | 0 | 0 | 1 |
| Gain of 10–14 letters | 5 | 6 | 2 | 6 |
| Gain of 5–9 letters, | 5 | 9 | 11 | 7 |
| Loss or gain of < 5 letters | 14 | 8 | 8 | 8 |
| Loss of 5–9 letters | 2 | 2 | 2 | 2 |
| Loss of ≥ 10 letters | 0 | 1 | 3 | 2 |
| Mean CFT, µm | 298.6 (58.7) | 295.4 (47.6) | 286.7 (42.6) | 290.1 (61.9) |
| Change in CFT, n | ||||
| Reduced by ≥ 50 μm | 16 | 15 | 16 | 15 |
| Reduced/increased by < 50 μm | 10 | 9 | 8 | 8 |
| Increased by ≥ 50 μm | 0 | 1 | 2 | 1 |
| Mean CSVol, mm3 | 8.7 (0.9) | 8.5 (0.8) | 8.5 (0.7) | 8.5 (0.8) |
| Change in CSVol, n | ||||
| Reduced by ≥ 1.0 mm3 | 15 | 15 | 16 | 15 |
| Reduced/increased by < 1.0 mm3 | 11 | 11 | 8 | 9 |
| Increased by ≥ 1.0 mm3 | 0 | 0 | 1 | 2 |
| Diabetic macular edema, n [17] | ||||
| Severe | 9 | 6 | 6 | 9 |
| Moderate | 11 | 7 | 4 | 1 |
| Mild | 4 | 7 | 8 | 5 |
| None | 2 | 6 | 8 | 11 |
Values in table are presented as the mean with the SD in parenthesis, unless indicated otherwise
n Number of participants (eyes) in that category
Table 3.
Mean changes in visual acuity and anatomical measures between baseline and follow-up, after adjustment for covariates
| Measures | Baseline to 6 months post commencement of aflibercept treatment | Baseline to 12 months post commencement of aflibercept treatment | Baseline to18 months post commencement of aflibercept treatment | Baseline to 24 months post commencement of aflibercept treatment | 6–12 months post commencement of aflibercept treatment | 12–24 months post commencement of aflibercept treatment |
|---|---|---|---|---|---|---|
| BCVA (EDTRS letters) |
3.73 [1.10, 6.36] p = 0.007 |
4.31 [1.64, 6.96] p = 0.002 |
2.23 [− 0.44, 4.88] p = 0.108 |
3.79 [1.12, 6.44] p < 0.001 |
0.57 [− 2.15, 3.30] p = 0.677 |
− 0.52 [− 3.26, 2.22] p = 0.708 |
| CFT (µm) |
− 117.96 [− 152.95, − 82.98] p < 0.001 |
− 121.68 [– 156.93, – 86.19] p < 0.001 |
− 130.72 [− 165.97, − 95.23] p < 0.001 |
− 127.20 [− 162.45, − 91.71] p < 0.001 |
− 3.76 [− 39.90, 32.50] p = 0.837 |
− 5.48 [− 42.00, 31.00] p = 0.837 |
| CSVol (mm3) |
− 1.36 [− 1.76, − 0.96] p < 0.001 |
− 1.60 [− 2.00, − 1.19] p < 0.001 |
− 1.57 [− 1.97, − 1.61] p < 0.001 |
− 1.60 [− 2.00, − 1.19] p < 0.001 |
− 0.24 [− 0.65, 0.17] p = 0.252 |
− 0.0024 [− 0.42, 0.42] p = 0.997 |
Values in table are presented as the mean with the 95% confidence interval given in square brackets
p significance test determined by linear mixed models regression: BCVA adjusted for repeated measures, patient age, sex, baseline HbA1c, and baseline BCVA; CFT and CSVol adjusted for repeated measures, patient age, sex, baseline HbA1c, and previous laser therapy
Fig. 1.
Change in best-corrected visual acuity (BCVA) Early Treatment Diabetic Retinopathy Scale (ETDRS) letter score over the course of the study for all participants and according to baseline BCVA. Change in BCVA was adjusted for repeated measures, patient age, sex, baseline glycosylated hemoglobin and baseline BCVA. Error bars indicate the standard deviation (SD)
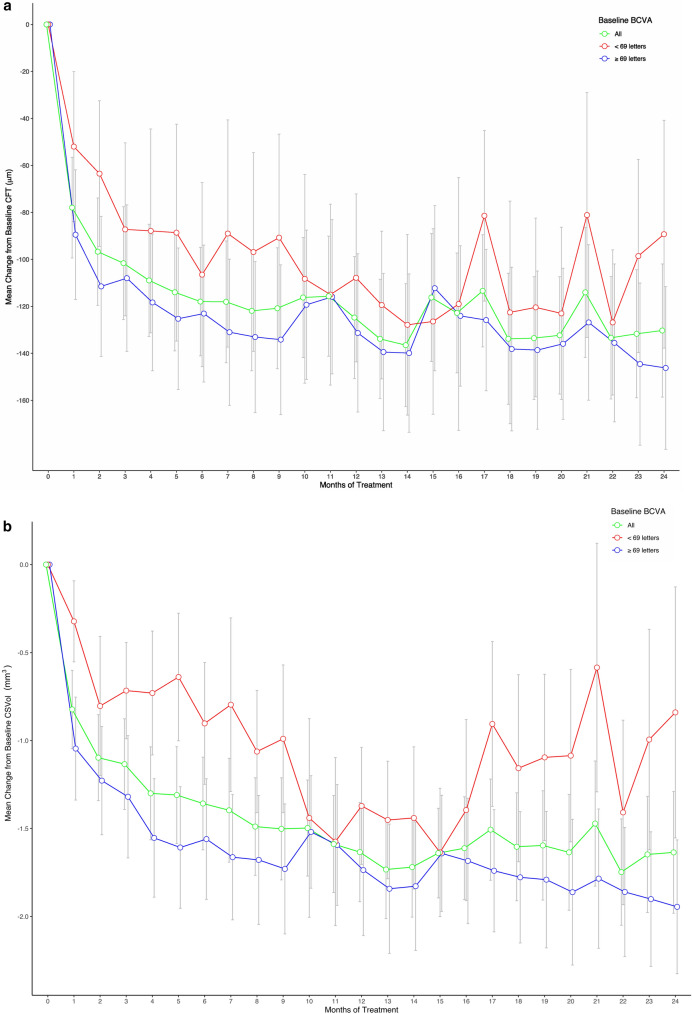
Anatomical Measures
Significant reductions in mean CFT were observed after one aflibercept injection, and at 6 months the proportion of participants with severe DME dropped to 34.6%; 57% of participants had a decrease in CFT of ≥ 50 µm (Table 1), and the mean CFT had decreased from 416.6 to 290.6 µm. The mean change in CFT, after adjustment for covariates (age, sex, and previous laser treatment), is presented in Table 3 and illustrated, according to baseline BCVA, in Fig. 2a. The mean reduction in CFT after 2 years of intravitreal aflibercept treatment was 127.2 (95% confidence interval 162.5, 91.5) µm, but although the mean CFT continued to decrease over the course of the study, the additional reduction of 10 µm after 6 months was not statistically significant (Table 3).
Fig. 2.
a Mean change in central retinal thickness within 1 mm of the fovea (CFT) over the course of 2 years of aflibercept treatment for all participants and according to baseline BCVA. b Mean change in central subfoveal volume within 6 mm of the fovea (CSVol) over the course of 2 years of aflibercept treatment, for all participants and according to baseline BCVA. CFT was measured by spectral domain-optical coherence tomography (Heidelberg Spectralis; Heidelberg Engineering Inc., Heidelberg, Germany). CFT and CSVol adjusted for repeated measures, patient age, sex, baseline glycosylated hemoglobin, and previous laser therapy. Error bars indicate the SD
At baseline the mean CFT of participants with a BCVA of < 69 letters was lower than that of participants with a BCVA of > 68 letters (Fig. 2a), but the differences between the two groups were not statistically significant at any time point, and the median change in CFT over the course of the study was similar in both groups (− 92.5 µm and − 80 µm respectively). Changes in CFT were accompanied by a significant reduction of 1.6 mm3 in CSVol, from 10.1 mm3 at baseline to 8.5 mm3 after 2 years (Tables 2, 3; Fig. 2b). On average, participants previously treated with PRP laser treatment or bevacizumab had reductions in CFT of 35 µm and 36 µm, respectively, greater than naive patients (p < 0.05).
Number and Frequency of Aflibercept Injections
Twenty-five patients completed 1 year and 23 completed 2 years of follow-up. In the first year: three participants had their follow-up/treatment interval extended to 12 weeks, four were extended to 10 weeks, six to 8 weeks and 6 weeks, while ten participants were maintained on a 4-weekly treatment regimen. In the second year, 18 of the remaining 25 participants (72%) had treatment intervals extended to > 8 weeks 16 at intervals of 12 weeks.
Of the 23 participants who completed the study, the mean number of injections administered at the end of the first year was 11.2 (median 11; SD 1.56). In the second year this was reduced to 6.9 (median 6; SD 3.2). There were no significant differences between the mean number of injections given to patients with BCVA ≥ 69 or < 69 letters at baseline.
Fifteen participants (5 female, 10 male) required bilateral anti-VEGF treatment over the course of the study (2 bevacizumab, 2 ranibizumab, and 11 aflibercept). Ten were diagnosed with clinically significant macular edema in their fellow eye at the same time as, or shortly after, commencing the study, but there were no statistically significant differences in any study outcomes between those receiving unilateral or bilateral anti-VEGF treatments.
Adverse Effects
Adverse events occurring over the course of the study are listed in Table 4.
Table 4.
Serious adverse events and non-serious adverse events observed/reported by more than one participant over the course of the study
| Ophthalmic events | Total number | Serious | Non-ophthalmic events | Total | Serious |
|---|---|---|---|---|---|
| Cataract | 6 | Cold/flu symptoms | 10 | 0 | |
| Visual disturbance (spots/floaters) | 6 | Hypo/hyperglycemia | 4 | 2 | |
| Subcutaneous hemorrhage | 7 | Chest infection | 4 | 2 | |
| Post-injection pain | 2 | Renal failure | 2 | 1 | |
| Stinging eyes | 2 | Allergy NOS | 2 | 1 | |
| Gastroenteritis | 2 | 1 | |||
| Vitreous hemorrhage | 2 | 2 | Cerebrovascular accident | 1 | 1 |
| Congestive cardiac failure | 1 | 1 | |||
| Myocardial infarction | 1 | 1 | |||
| Angina exacerbation | 1 | 1 | |||
| Hypocalcemia | 1 | 1 | |||
| Respiratory failure | 1 | 1 |
NOS Not otherwise specified
Participant Withdrawal
Two male participants failed to complete the study due to unrelated serious adverse events that resulted in death: One after only 7 months treatment due to complications of a viral lung infection; the second at 21 months when he developed congestive cardiac failure associated with a concomitant heart condition. In addition, a female resident of a nursing home withdrew at 23 months due to logistical issues (Table 4).
Other Adverse Events
The most commonly reported ophthalmic adverse events were progression of bilateral cataract, visual disturbance (spots/floaters), subconjunctival hemorrhage, and sticky/gritty eyes. Two participants developed vitreous hemorrhage in the second year of the study. but there were no instances of endophthalmitis or retinal detachment.
The most commonly reported non-ocular adverse events were respiratory tract infections and complications associated with concomitant disease, most commonly diabetes (unstable blood sugars and complications associated with diabetic renal disease) or cardiovascular disease. Two patients had thromboembolic events that led to hospitalization.
Discussion
This study has demonstrated that significant improvements in visual acuity and a reduction in DME severity are possible using a T&E regimen of aflibercept in routine clinical practice over a period of 2 years. Approximately 54% of participants improved their visual acuity by ≥ 1 line, and 69% had an improvement in the severity of their DME.
The observed improvement in participant visual acuity over 2 years (4 letters) was, however, lower than that observed in two pivotal large randomized clinical trials (VISTA and VIVID) [13] in which aflibercept was administered every 4 or 8 weeks after five monthly loading injections and the mean improvement in vision was 10.7 and 12.5 letters, respectively. Our results were similarly modest when compared to the Diabetic Retinopathy Clinical Research Network (DRCR.net) Protocol T study [18, 19], which compared the efficacy of aflibercept with ranibizumab and bevacizumab treatment for DME when all were used according to the same treatment regimen: six monthly loading injections followed by monthly follow-up visits for review and intravitreal injection and complete focal grid laser therapy as required. After 2 years, the mean BCVA of participants receiving aflibercept had improved by 12.8 letters compared to 10 letters and 12.3 letters for bevacizumab and ranibizumab, respectively [19].
A possible explanation for the lower improvement in mean BCVA observed in our participants may be the observation made by the DRCR investigators that the level of improvement in vision in patients treated with aflibercept over the course of 2 years was dependent on the baseline visual acuity score [19]. Although the baseline visual acuity inclusion criteria for this study was in accordance with those for the VIVID/VISTA [12] and DRCR.net Protocol T [19] trials (between 24 and 78 EDTRS letters), none of our participants had a baseline BCVA of < 50 letters. Mean baseline BCVA for the participants in our study was 70 letters overall (61 letters in those with BCVA < 69 letters) compared to 60 and 65 letters for the VISTA/VIVID [12] and DRCR.net Protocol T [19] trials, respectively. In addition, 50% of Protocol T participants had a visual acuity of < 69 letters at baseline compared to only 30% of our participants. Our study is therefore more prone to the ceiling effects limiting the total number of letters that may be gained by individual participants with baseline BCVA of ≥ 70 letters. The higher baseline BCVA in our participants is a likely consequence of our source population, who were patients attending clinic for regular ophthalmic review which facilitates earlier detection of visual decline and recommencement of treatment where appropriate. Patients recruited into large industry-funded clinical trials may be more likely to include those who might not be able to afford regular visits to an ophthalmology clinic and whose disease may have gone unchecked until study recruitment.
In contrast to the BCVA, mean baseline CFT and CSVol in this study were comparable to the aflibercept arm of Protocol T (CFT 416 [SD 121] µm and CSVol 10.1 [SD 1.6] mm3 vs. CFT 412 [SD 130] µm and CSVol 8.9 [SD 1.9] mm3, respectively) [19]. The change in CSVol was similar in the two studies (− 1.58 [SD 1.72] mm3 vs. − 1.7 [SD 1.6 ] mm3, respectively), but the mean improvement in CFT observed between baseline and 2 years was 50 µm less in all but two participants in our study, who were non-compliant with their 4-weekly injection schedule, with a reduced CFT.
At 2 years, previous exposure to PRP was associated with a greater reduction in CFT. However, although the current study protocol included focal laser therapy as a potential rescue measure, none of our participants with persistent severe DME (34.6%) were administered this treatment over the 2 years of the study as, with the exception of two patients (with reductions in BCVA of 9 and 11 letters), their vision was either maintained or improved. Over the 2 years of the Protocol T study, 31% of patients in the aflibercept arm had at least one session of focal grid laser therapy for persistent DME [19]. It is possible that if our participants had received treatment our outcomes may have been more comparable, although a post hoc analysis of Protocol T data suggested that any additional benefit of focal laser therapy was only apparent in participants with poor vision who were in the bevacizumab arm of the trial [20].
In a post hoc analysis, participants with anti-VEGF exposure prior to commencing the study had a greater reduction in CRT compared to naive participants. This is in contrast to the results of the VISTA [21] and Protocol T [19], where visual and anatomical outcomes of patients in the aflibercept arms of the study were independent of previous anti-VEGF exposure. Further investigation of this and other contributory factors that may be associated with better outcomes in previously treated patients was outside the scope of this study.
This study was initiated prior to the publication of the DRCR.net Protocol T trial that demonstrated the effectiveness of a PRN treatment schedule and before aflibercept was routinely available for the treatment of DME in Australia. The T&E regimen is regarded as a proactive, cautious approach to treatment which minimizes disease recurrence and reduces the number of patient visits to clinic [16]. In addition to freeing up clinic time for others, this regimen can make clinic visits less stressful for patients as they can anticipate the treatment and will be able to plan their visit (e.g., transport requirements) accordingly. In the current study, the median number of aflibercept treatments (11 (interquartile range [IQR] 10–12) in the first year and six (IQR 5–8.5) in the second year) was comparable to that observed in the Protocol T (9 (IQR 8–11) and 5 (IQR 2–7) in the first and second years, respectively). The downside of T&E regimens, however, is that patients are treated at pre-defined intervals and when treatment might be deemed unnecessary in a PRN regimen. Of the 12 participants who had their treatment intervals extended to 12 weeks, 11 continued to receive aflibercept treatment at 12-weekly intervals with no evidence of DME on the OCT scans. Such unnecessary treatments expose patients to increased risk of adverse events associated with intravitreal injection and would also make the cost of treatment more expensive than it need be. Therefore, physicians need to consider the risks and benefits of any treatment regimen to individual patients.
The weaknesses of this study include the lack of any comparator group and its sample size. As observed in other anti-VEGF T&E studies, the changes in visual acuity, CFT, and CSVol over the 2 years (Figs. 1, 2) fluctuated over time as participant treatment intervals were extended. Smaller sample size results in greater fluctuations as individual participant results have more weight over the sample. This was particularly evident among participants with a BCVA of < 69 letters, when our data was stratified according to baseline BCVA, where delays to treatment, caused by one patient’s non-compliance, had a negative effect on improvements previously observed.
This is the first 2-year prospective study of aflibercept for DME conducted in a routine clinical situation in patients with no or minimal recent exposure to anti-VEGF treatment. The few clinic-based prospective T&E studies conducted to date have investigated the efficacy of bevacizumab [22] or ranibizumab [23–25], but most prospective studies have concentrated on the outcomes of aflibercept treatment in patients non-responsive to other anti-VEGF treatments [26–29] or using loading followed by an 8-weekly regimen [30], with results similar to that observed in the VIVA/VISTA.
Conclusion
The results of this study indicate that a T&E regimen of aflibercept is effective and a practical alternative to a PRN treatment schedule for the majority of patients presenting with DME. Extension periods beyond 12 weeks should be employed to reduce patient overtreatment, but the latter is more likely in the third year of treatment and beyond.
Acknowledgments
We are grateful to the patients who participated in this study. Thanks also to Dr Guy Bylsma and Dr Andrew Traill who, along with Clinical Professor Nitin Verma and Professor Alex Hewitt, were Clinical Investigators on this study and provided advice on the study protocol in addition to identifying and caring for study participants.
Funding
This investigator-initiated study was supported by Bayer Australia Ltd. who provided the study treatment and some financial assistance but did not contribute to the study design, analysis, or preparation of this manuscript. No funding was received for the publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors criteria for authorship of this article, take responsibility for the integrity of the work as a whole, and have given their approval for publication of this version.
Disclosures
Beverley A. Curry, Paul G. Sanfilippo, Sarah Chan, Alexander W. Hewitt, and Nitin Verma have nothing to declare.
Compliance with Ethics Guidelines
Institutional ethics approval was obtained from the Tasmanian Health and Medical Research Ethics Committee (THMREC) prior to study commencement, Protocol Ref No: H0014556 and registered with the Australian New Zealand Clinical Trials Registry (ANZCTR), ACTRN12618000428268. Informed consent was obtained from all participants, prior to enrolment, in accordance with Springer’s ethical policies. The study adhered to the tenets of the 1964 Declaration of Helsinki, as revised in 2013, and to the protocol approved by THMREC.
Data Availability
The de-identified participant datasets analysed in preparation of this manuscript may be available from the corresponding author if a reasonable request is received and the research study proposed has ethical approval.
Footnotes
Enhanced Digital Features
To view enhanced digital features for this article go to 10.6084/m9.figshare.10247681.
Change history
12/22/2021
The license text was incorrectly structured. The article has been corrected.
References
- 1.International Diabetes Federation. Diabetes and Blindness due to DME. 2011. http://www.idf.org/sites/default/files/idf-europe/IDF%20Toolkit_Backgrounder_FINAL.pdf. Accessed 6 June 2014.
- 2.World Health Organization . Global status report on non communicable diseases 2012. Geneva: World Health Organization; 2014. [Google Scholar]
- 3.Australian Institute of Health and Welfare 2014. Cardiovascular disease, diabetes and chronic kidney disease: Australian facts: Prevalence and incidence. Cardiovascular, diabetes and chronic kidney disease series no. 2. Cat. no. CDK 2. Canberra: AIHW. http://www.aihw.gov.au/publication-detail/?id=60129549616.
- 4.Keel S, Xie J, Foreman J, von Wijngaarden P, Taylor H, Dirani M. The prevalence of diabetic retinopathy. The National Eye Health Survey. Ophthalmology. 2017;124:977–984. doi: 10.1016/j.ophtha.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 5.Early Treatment Diabetic Retinopathy Study Research Group Photocoagulation for diabetic macular edema: early treatment diabetic retinopathy study report No. 1. Arch Ophthalmol. 1985;103:1796–1806. doi: 10.1001/archopht.1985.01050120030015. [DOI] [PubMed] [Google Scholar]
- 6.Aiello LP, Avery RL, Arrigg PG, et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med. 1994;131:1480–1487. doi: 10.1056/NEJM199412013312203. [DOI] [PubMed] [Google Scholar]
- 7.Ciulla TA, Amador AG, Zinman B. Diabetic retinopathy and diabetic macular edema: pathophysiology, screening, and novel therapies. Diabetes Care. 2003;26(9):2653–2664. doi: 10.2337/diacare.26.9.2653. [DOI] [PubMed] [Google Scholar]
- 8.Ferrara N, Damico L, Shams N, Lowman H, Kim R. Development of ranibizumab, an anti-vascular endothelial growth factor antigen binding fragment, as therapy for neovascular age-related macular degeneration. Retina. 2006;26:859–870. doi: 10.1097/01.iae.0000242842.14624.e7. [DOI] [PubMed] [Google Scholar]
- 9.Mitchell P, Bandello F, Schmidt-Erfurth U, et al. The Restore study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology. 2011;118:615–625. doi: 10.1016/j.ophtha.2011.01.031. [DOI] [PubMed] [Google Scholar]
- 10.Rajendram R, Fraser-Bell S, Kaines A, et al. A 2-year prospective randomized controlled trial of intravitreal bevacizumab or laser therapy (BOLT) in the management of diabetic macular edema: 24-month data: report 3. Arch Ophthalmol. 2012;130:972–979. doi: 10.1001/archophthalmol.2012.393. [DOI] [PubMed] [Google Scholar]
- 11.Do DV, Nguyen QD, Boyer D, et al. One -year outcomes of the da Vinci Study of VEGF trap-eye in eyes with diabetic macular edema. Ophthalmology. 2012;119:1658–1665. doi: 10.1016/j.ophtha.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 12.Korobelnik J-F, Do DV, Schmidt-Erfurth U, et al. Intravitreal aflibercept for diabetic macular edema. Ophthalmology. 2014;121(11):2247–2254. doi: 10.1016/j.ophtha.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 13.Brown DM, Schmidt-Erfurth U, Do DV, et al. Intravitreal aflibercept for diabetic macular edema: 100-week results from the VISTA and VIVID studies. Ophthalmology. 2015;122:2044–2052. doi: 10.1016/j.ophtha.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 14.Papadopoulos P, Martin J, Ruan Q, et al. Binding and neutralization of vascular endothelial growth factor (VEGF) and related ligands by VEGF Trap, ranibizumab and bevacizumab. Angiogenesis. 2012;15:171–185. doi: 10.1007/s10456-011-9249-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rakic JM, Lambert V, Devy L, et al. Placental growth factor, a member of the VEGF family, contributes to the development of choroidal neovascularisation. Invest Ophthalmol Vis Sci. 2003;44(7):3186–3193. doi: 10.1167/iovs.02-1092. [DOI] [PubMed] [Google Scholar]
- 16.Freund KB, Korobelnik JF, Devenyi R, et al. Treat-and-extend regimens with anti-VEGF agents in retinal diseases: a literature review and consensus recommendations. Retina. 2015;35:1489–1506. doi: 10.1097/IAE.0000000000000627. [DOI] [PubMed] [Google Scholar]
- 17.Koleva-Georgieva DN, Sivkova NP. Types of diabetic macular edema assessed by optical coherence tomography. Folia Med. 2008;50:30–38. [PubMed] [Google Scholar]
- 18.Wells JA, Glassman AR, Ayala AR, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. Diabetic Retinopathy Clinical Research Network. N Engl J Med. 2015;372:1193–1203. doi: 10.1056/NEJMoa1414264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wells JA, Glassman AR, Ayala AR, et al. Diabetic Retinopathy Clinical Research Network. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema: two year results from a comparative effectiveness randomised clinical trial. Ophthalmology. 2016;123:1351–1359. doi: 10.1016/j.ophtha.2016.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jampol LM, Glassman AR, Bressler NM, et al. Diabetic retinopathy clinical research network anti-vascular endothelial growth factor comparative effectiveness trial for diabetic macular edema. Additional efficacy post hoc analyses of a randomized clinical trial. JAMA Ophthalmol. 2016;134(12):1429–1434. doi: 10.1001/jamaophthalmol.2016.3698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Do DV, Nguyen QD, Vitti R, et al. Intravitreal Aflibercept injection in diabetic macular edema patients with and without prior anti-vascular endothelial growth factor treatment. Outcomes from the Phase 3 program. Ophthalmology. 2016;123:850–857. doi: 10.1016/j.ophtha.2015.11.008. [DOI] [PubMed] [Google Scholar]
- 22.Sugimoto M, Ichio A, Nunome T, Kondo M. Two year result of intravitreal bevacizumab for diabetic macular edema using treat and extend protocol. Medicine. 2017;96:16. doi: 10.1097/MD.0000000000006406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Prunte C, Fajnkuchen F, Mahmood S, et al. Ranibizumab 0.5 mg treat-and-extend regimen for diabetic macular oedema:the RETAIN study. Br J Ophthalmol. 2016;100:787–795. doi: 10.1136/bjophthalmol-2015-307249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Payne JF, Wykoff CC, Lloyd-Clark W, Bruce BB, Brown DM. Randomized trial of treat and extend ranibizumab with and without navigated laser for diabetic macular edema. Ophthalmology. 2017;124:74–81. doi: 10.1016/j.ophtha.2016.09.021. [DOI] [PubMed] [Google Scholar]
- 25.Eichenbaum DA, Duerr E, Patel HR, Pollack SM. Monthly versus treat-and-extend ranibizumab for diabetic macular edema: a prospective, randomized trial. Ophthalmic Surg Lasers Imaging Retina. 2018;49:e191–e197. doi: 10.3928/23258160-20180221-07. [DOI] [PubMed] [Google Scholar]
- 26.Bahrami B, Hong T, Schlub TE, Chang AA. Aflibercept for persistent diabetic macular edema. Forty-eight-week outcomes. Retina. 2019;39(1):61–68. doi: 10.1097/IAE.0000000000002253. [DOI] [PubMed] [Google Scholar]
- 27.Călugăru D, Călugăru M. Conversion to aflibercept after prior anti-VEGF therapy for persistent diabetic macular edema. Am J Ophthalmol. 2016;168(2):290–291. doi: 10.1016/j.ajo.2016.05.015. [DOI] [PubMed] [Google Scholar]
- 28.Laiginhas R, Silva MI, Rosas V, et al. Aflibercept in diabetic macular edema refractory to previous bevacizumab: outcomes and predictors of success. Graefes Arch Clin Exp Ophthalmol. 2018;256:83–89. doi: 10.1007/s00417-017-3836-1. [DOI] [PubMed] [Google Scholar]
- 29.Chen Y-Y, Chang P-Y, Wang J-K. Intravitreal aflibercept for patients with diabetic macular edema refractory to bevacizumab or ranibizumab: analysis of response to aflibercept. Asia Pac J Ophthalmol. 2017;6:250–255. doi: 10.22608/APO.2016186. [DOI] [PubMed] [Google Scholar]
- 30.Polo RC, Sanchez CR, Guisado DMG, Luque MJD. Aflibercept for clinically significant diabetic macular edema: 12 month results in daily clinical practice. Clin Ophthalmol. 2018;12:99–104. doi: 10.2147/OPTH.S154421. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The de-identified participant datasets analysed in preparation of this manuscript may be available from the corresponding author if a reasonable request is received and the research study proposed has ethical approval.