Abstract
Background & objectives:
Comprehension and process of consent are important for persons with mental illness as they may not be impaired in considering research participation. The American Psychiatric Association developed a detailed Cultural Formulation Interview (CFI). The present study was a part of field testing of CFI, aimed to standardize cultural information affecting the patients’ management in India. This paper describes the process and conclusions from the consent-seeking process of this study.
Methods:
The purpose and procedures about field trial of the CFI were introduced and the patient and caregiver were requested for participation. Consent process was carried out step by step, by reading out the consent form to the first new patient of the day in the psychiatry outpatients department of a tertiary care hospital in north India, inviting questions followed by the ‘comprehension’ questions. The entire process was audiotaped without any personal identifiers. The process was repeated if not comprehended.
Results:
A total of 67 patients consented, 11 refused and majority were educated more than secondary school. Some concerns shown by the patients and caregivers included risk of participation, loss or benefits of participation, privacy, etc. All types of mentally ill patients participated in the study.
Interpretation & conclusions:
Translations of consent forms used simple words, consonant with understanding of the potential participants. Patients’ belief that participating in this long process would improve their care, and serve humanity, influenced their decision to participate. Except for intoxication and severe psychosis, patients could understand and comprehend issues around consent. Main issues were confidentiality and culture. Our experience in the psychiatry OPD refutes the commonly held belief that mentally ill persons lack comprehension and ability to consent.
Keywords: Comprehension, cultural formulation interview, debriefing, informed consent, mental illness
Comprehension and capacity to consent is a part of the consent process. Performing an assessment of decision-making capacity to consent to participate in research should be determined to decide who signs the consent1. Others advocate the use of feedback procedures2. Assessment of a patient's competence remains an essential part of the consent process3. While the primary responsibility of ensuring that the individual has really understood what his/her responsibilities as a research subject will be, is that of the investigator, in India, the law permits the caregiver of a patient who is unable to provide consent, to consent on his/her behalf1. Comprehension of duties as a research subject is as important as consenting especially for persons whose decisional capacity is impaired due to mental illness.
All mentally ill people may not be impaired in considering research participation and determining whether to participate or not. Mentally ill individuals suffer from a spectrum of disorders with varying degrees of disability of understanding and cognition. Several different factors, including illness variables, cognitive capacity and education, may affect comprehension4. Capacity and comprehension may change among patients with serious mental illnesses such as schizophrenia, over time, generally related to better neuropsychological test performance5. In a study conducted in China, patients with schizophrenia, after one week of training, showed enhanced competence for consent and scored higher than controls on the Understanding and Appreciation subscales of Chinese Mandarin MacArthur Competence Assessment Tool-Clinical Research6. Cultural issues and beliefs also play a major role in clinical expression, help-seeking, treatment adherence and outcome. However, the role of cultural factors in severe mental illnesses has not received appropriate attention from mental health professionals7.
In the Diagnostic and Statistical Manual of Mental Disorders (DSM IV)8, cultural factors affecting help-seeking were described in narrative form. For the DSM 5th edition, the American Psychiatric Association (APA)8 developed a detailed Cultural Formulation Interview (CFI). Consisting of 13 main questions, some with subsections, the CFI aims to standardize information about cultural factors which may affect the patients’ management. The CFI has been field tested in different parts of the world9. This study was conducted with an aim to field test CFI in India. This paper describes the process and conclusions from the consent-seeking process in a psychiatry outpatients department (OPD) in north India.
Material & Methods
The study was conducted in the outpatient section of the department of Psychiatry at the Atal Bihari Vajpayee Institute of Medical Sciences (ABVIMS), Dr. Ram Manohar Lohia Hospital (RMLH), a tertiary care postgraduate teaching hospital in New Delhi, India, with a patient catchment area from all over the country, in particular the neighbouring north Indian States of Rajasthan, Haryana, Himachal Pradesh, Uttarakhand and Bihar. The consent form, in association with all participating centres of the study, was drafted at the New York State Psychiatric Institute and translated at RMLH into Hindi9. The consent form was followed by a series of questions designed to test comprehension of research process. For uniformity, all consent forms were read, explained and comprehension tested at the end in the outpatient's department. The consent process, CFI interview itself, psychiatric interview thereafter and subsequent debriefing interviews were all audiotaped after due informed consent, without any personal identifiers. The tapes, with no names or personal identifiers, were stored and analysed for results (Figure). Newly registered patients at the Psychiatry Outpatient Department were included in this study. There were no exclusion criteria except patient's refusal to participate.
Figure.
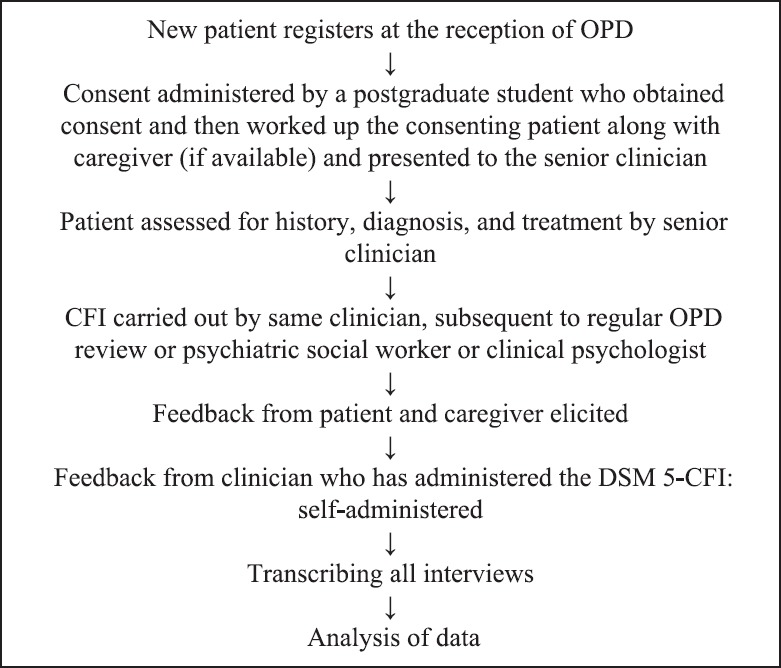
Flowchart of Cultural Formulation Interview (CFI) field study procedures. OPD, outpatient department; DSM 5, Diagnostic and Statistical Manual of Mental Disorders, 5th edition.
To increase variability and encompass wider viewpoints, all mental health professionals of the department, psychiatrists, clinical psychologists and psychiatric social workers, conducted the CFI interview subsequent to consent after rigorous training sessions. All CFI interviewers were assigned five patients each, while there was no restriction on the number of consent interviews per interviewer.
The participants were not paid, and the study procedures took extra time (almost 4 h in all), consisting of audiotaped consent, comprehension, psychiatric interview, CFI interview and debriefing of patient and caregiver. Only one patient was recruited per day by one interviewer. Before the study began, members of the department of Psychiatry were sensitized to the role of cultural factors in psychiatry through a series of lectures. Two workshops of 2 h duration, including a specially prepared video for the CFI, were conducted.
On the assigned day of field testing, a postgraduate student informed the first new patient about the study. He/she introduced the DSM 5-CFI through a brief standard introduction and requested consent for CFI participation8. In case the patient refused, the next new patient was asked. If the patient (usually accompanied by a family member) had agreed to participate, detailed consent process was started step by step. The consent was audiotaped. The consent form was read paragraph by paragraph, inviting the patient and caregiver if present, to ask questions at each step. The CFI was followed by the ‘comprehension’ questions. If the participant could not answer these questions the first time, the consent was read out again, and the participant was questioned again. If the patient could not comprehend after three readings, he/she was informed that he/she could not participate in this research. The procedure of the study is illustrated in the Figure. Feedback from clinicians who conducted CFI was taken. The consent audiotapes formed the material for the present study. The study protocol was examined and approved by the Institutional Ethics Committee of ABVIMS, RMLH, New Delhi.
Results
A total of 67 patients (39 male, 28 female) consented for the study and 11 refused. The majority of participants were educated to a higher level than secondary school. Concerns shown by those who refused included potential risks of participation, loss or benefits of participation, issue of privacy, etc. Patients diagnosed with diverse psychiatric disorders participated in the study. Final data analysis was conducted on 67 participants of whom seven were subsequently diagnosed with psychosis. This number was too small for separate analysis. A majority of patients (57%, n=38) were accompanied by caregivers who also consented and participated in the procedures. More than half (64%) patients were married, spoke Hindi as a primary language (88%), earned their own living or lived with parents or spouse and belonged to Delhi (Table I).
Table I.
Demographic and clinical details of participants (n=67)
| Variable | Frequency (%) |
|---|---|
| Gender | |
| Male | 39 (58.2) |
| Female | 28 (41.8) |
| Education | |
| Illiterate | 2 (3) |
| Primary | 10 (14.9) |
| Middle | 7 (10.4) |
| Secondary | 15 (22.4) |
| Senior secondary | 18 (26.9) |
| College | 15 (22.4) |
| Marital status | |
| Ever married* | 43 (64.2) |
| Never married | 24 (35.8) |
| Primary language** | |
| 1 | 54 (80.6) |
| 2 | 3 (4.5) |
| 3 | 5 (7.5) |
| 4 | 5 (7.5) |
| Income source*** | |
| 1 | 25 (37.3) |
| 2 | 16 (23.9) |
| 3 | 23 (34.3) |
| 4 | 3 (4.5) |
| Income# | |
| 0 | 5 (7.5) |
| 1 | 10 (14.9) |
| 2 | 14 (20.9) |
| 3 | 13 (19.4) |
| 4 | 8 (11.9) |
| 5 | 4 (6) |
| 6 | 3 (4.5) |
| 7 | 10 (14.9) |
| State of birth | |
| NCR | 27 (40.3) |
| Bihar | 13 (19.4) |
| UP | 8 (6) |
| Others | 19 (34.3) |
| Diagnosis | |
| Adjustment disorder | 4 |
| Anxiety | 8 |
| Substance dependence | 8 |
| Depression | 21 |
| Bipolar disorder | 7 |
| Conversion-dissociation | 4 |
| Rule out neurological disorder | 2 |
| Mental retardation | 1 |
| Obsessive-compulsive disorder | 8 |
| Psychosis or schizophrenia | 4 |
*Includes two divorced and one widowed; **Hindi/Hindi and English/Hindi and regional language/regional language; ***Self/spouse/parents/I choose not to answer; #Nil/up to 50,000/50,001-100,000/100,001-150,000/150,001-200,000/ 20,001-250,000/250,001-300,000/above 300,001 per year
Most participants were accompanied by their male/female caregivers during consent process except two female and 10 male participants. Seven relatives actively consented in the consent process, asking questions and receiving answers (Table II). Consent was provided or countersigned by caregiver for one participant suffering from mania and for four suffering from psychosis. One child was accompanied by his parents, where his father provided consent. Three participants required repetition of consent more than once, based on replies of their comprehension test. One male participant asked for a copy of his electronic audio consent, apart from the written consent form which was provided to all and one female participant consulted her husband on phone before consenting. Four potential participants left during or immediately after the consent process, as they were pressed for time. For four other participants, consent was administered in English. Questions and queries raised during the consent process are presented in Table II. From participants’ queries (Table II), it was evident that, although the consent form incorporated all study procedures which were repeatedly read out to them with pauses for questions, doubts remained which were clarified. Most queries were about the risk of participation, loss or benefits of participation and procedures of the study recording storing of study data and confidentiality. Only one of the 67 participants, during the last part of the study (debriefing) observed that the consent process was lengthy.
Table II.
Questions raised by the participants and caregivers during their consent process
| 1. Why are you audio taping my interview? |
| 2. How will you keep my audio tape privately? |
| 3. What is the meaning of diagnostic (‘naidanik’ in Hindi)? |
| 4. I could not understand ‘pure Hindi’, when you read consent form. |
| 5. What kind of harm has generally occurred during this kind of participation? |
| 6. For treatment, do we need to participate in this process? |
| 7. What kind of risk will be there for me if I participate or not? |
| 8. Why will you destroy my audiotapes after 15 years? |
| 9. What is the meaning of ‘Bhagidari’ (Participation) over here? |
| 10. Is signature important on consent form? |
| 11. Is blood test must for this participation? |
| 12. One caregiver asked about research and record keeping of participants? Who and How? |
| 13. Do I need to come again and again for this? |
| 14. Caregiver: Is there any harm in participation? |
| 15. ‘If privacy is breached, I could be spotted’. |
| 16. Could I continue my duty while taking medication? |
| 17. What is ‘clinical evaluation’? Why were 10 questions asked to me? Do I need to reply, in what way and to whom? |
| 18. What is the purpose of audio tape? |
| 19. Privacy of participations, how will it be ensured? |
| 20. What is ‘Emotional Injury’? |
| 21. Clear my confusion about difference between research and treatment. |
| 22. What is the meaning of background (‘prushtabhoomi’ in Hindi) and culture? |
Discussion
In the present study, it was found that a random group of new psychiatry outpatients could comprehend and intelligently participate in a research study to validate an important tool which would eventually benefit all such patients. These patients could understand and question the consent process. Participation in a research process is a matter of choice and not a compulsion and this should be clearly spelt out in the consent form. Capacity to consent implies competence in assessing the choices put forth. However, capacity to consent may vary widely among psychiatry patients, deemed the most seriously ill and compromised10. Specific guidelines for psychiatric patients may fulfil this need10. Further, cognitive therapy may improve self-reflectiveness and ability to comprehend implications of treatment11. Even seriously ill psychiatric inpatients may be able to understand and reason about the choices presented to them5. Patients with schizophrenia may also be deemed competent unless a clinical evaluation opines them clearly unfit for consent12. Capacity to consent may also change over time, which may be associated with better performance on neuropsychological tests5.
Consent forms are usually lengthy, dense documents incorporating several headings, subheadings, procedures and finally the signature13,14. The procedure becomes more difficult when translation needs to be done. Efforts were made to use simple Hindi words in translation. However, it was tried to keep difficult words to a minimum but some were unavoidable. This was in accordance with consent form guidelines that Informed Consent Form translations must be performed to a patient's level of understanding15,16.
Consent is a relatively novel concept for the majority of Indian patients, many of whom travel long distances for psychiatric consultation at a tertiary care centre due to paucity of mental health services17. This study did not provide any monetary compensation to participants, but their belief that participating in this long process would improve their care formed the basis of their decision to participate. Patients perceive consent form differently and there is discrepancy in consent procedures in different centres18. The right to refuse to participate in research is an inalienable right of the participant. Most refusals occurred before the consent was administered, mainly because patients did not have time. Their refusal was respected. The (informed consent) process must also allow the respondent to decline participation without being subject to intimidation, coercion, or being unduly influenced by incentives that could be viewed as coercive19. According to Mfutso-Bengo et al20, the reasons for refusing consent include “failure to follow traditional customs, lack of study benefits, superstition, poor informed consent procedures, ignorance of health research, fear of strangers, lack of cultural sensitivity, poor timing, and previous bad research experience”. Our informed consent procedures were as open and non-coercive as possible, even for this no-risk study.
Patients from urban areas and of comparatively higher socio-economic status were more concerned with treatment and not willing to prolong consultation through participation. This appeared to be an individual opinion as a wide variety of patients from different backgrounds were enrolled in the study. Refusal to participate in schizophrenia patients was determined by age and level of education in a study by Kim et al21 as younger and better-educated patients tended to decline participation in a risky study. Confidentiality of information is a major issue in obtaining consent for participation in research and this has been extensively studied in psychiatry patients22,23.
Participants found the audiotape a curious part of the research and almost all remarked on it. Some were worried about the audiotaping and wanted information on exactly who would be able to access their tapes. Some refusals were due to audiotaping of the entire consent-taking procedure, because people were reluctant to have their voice audiotaped. In clinical trials in India, the Central Drugs Standard Control Organization (CDSCO) under the Ministry of Health and Family Welfare, Government of India, has made audiotaping of consent compulsory24. It was reassuring to note that audiotaping did not interfere materially with the consent process.
During debriefing at the end, all participants were satisfied with CFI procedures and happy with the time given to them. None complained about being interviewed again and again. Some caregivers held strong beliefs about religious leaders and quickly consented on hearing the word ‘sanskriti’ (culture). They seemed more interested when told about the cultural aspect of the study and its relation to mental illness.
In conclusion, our study showed that it was possible to obtain proper consent, even in a busy psychiatry OPD and make the patients understand the procedures of the study. Altruism was a major, but not the only, factor in their consenting to the prolonged procedure. Participants, at some level, also expected extra attention to their symptoms and for the doctor to provide more personalized treatment, due to the detailed discussion of their condition that the CFI protocol required. Patients with major mental illnesses such as bipolar disorder, schizophrenia and depression were enrolled. It was found that except for intoxication and gross excitement due to psychosis, patients could understand and comprehend issues around consent. Even in psychosis, there is a wide variety of cognitive ability that at least for some issues, patients can take their own decisions25,26. An unanticipated benefit of this study was the extra training that participating residents received consent taking.
Acknowledgment
Authors acknowledge the members of the dedicated Cultural Formulation Interview (CFI) team (Drs Mahima Malhotra, Rahul Saha, Rohit Verma, Ashutosh Gupta, Satabdi Chakraborty, R.P. Beniwal, Mina Chandra, Shekhar Yadav, Satyam, Sreeja, Sapna, Sunita, Kapila Garg, Atul Rai) for their efforts in conducting CFI. Authors also thank all patients and their families for sincere participation.
Footnotes
Financial support & sponsorship: The first author (SND) acknowledges the American Psychiatric Association, USA, for funding. The second and third authors (NNM & TB) thank the Fogarty International Center, the NIH Office of the Director Office of Behavioral and Social Science Research and the National Center for Chinese and Alternative Medicine, of NIH (R01TW008289) and Training Grant for Psychiatric Genetics in India (Grant #5D43 TW006167), for financial support. Funding agencies had no role in the design and conduct of the study
Conflicts of Interest: None.
References
- 1.Simpson C. Decision-making capacity and informed consent to participate in research by cognitively impaired individuals. Appl Nurs Res. 2010;23:221–6. doi: 10.1016/j.apnr.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 2.Stiles PG, Poythress NG, Hall A, Falkenbach D, Williams R. Improving understanding of research consent disclosures among persons with mental illness. Psychiatr Serv. 2001;52:780–5. doi: 10.1176/appi.ps.52.6.780. [DOI] [PubMed] [Google Scholar]
- 3.Henwood S, Wilson MA, Edwards I. The role of competence and capacity in relation to consent for treatment in adult patients. Br Dent J. 2006;200:18–21. doi: 10.1038/sj.bdj.4813118. [DOI] [PubMed] [Google Scholar]
- 4.Candilis PJ, Fletcher KE, Geppert CM, Lidz CW, Appelbaum PS. A direct comparison of research decision-making capacity: Schizophrenia/schizoaffective, medically ill, and non-ill subjects. Schizophr Res. 2008;99:350–8. doi: 10.1016/j.schres.2007.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aydin Er R, Sehiralti M. Comparing assessments of the decision-making competencies of psychiatric inpatients as provided by physicians, nurses, relatives and an assessment tool. J Med Ethics. 2014;40:453–7. doi: 10.1136/medethics-2012-100928. [DOI] [PubMed] [Google Scholar]
- 6.Wang X, Yu X, Appelbaum PS, Tang H, Yao G, Si T, et al. Longitudinal informed consent competency in stable community patients with schizophrenia: A one-week training and one-year follow-up study. Schizophr Res. 2016;170:162–7. doi: 10.1016/j.schres.2015.11.019. [DOI] [PubMed] [Google Scholar]
- 7.Viswanath B, Chaturvedi SK. Cultural aspects of major mental disorders: A critical review from an Indian perspective. Indian J Psychol Med. 2012;34:306–12. doi: 10.4103/0253-7176.108193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington DC: American Psychiatric Association; 2013. [Google Scholar]
- 9.Lewis-Fernández R, Aggarwal NK, Lam PC, Galfalvy H, Weiss MG, Kirmayer LJ, et al. Feasibility, acceptability and clinical utility of the cultural formulation interview: Mixed-methods results from the DSM-5 international field trial. Br J Psychiatry. 2017;210:290–7. doi: 10.1192/bjp.bp.116.193862. [DOI] [PubMed] [Google Scholar]
- 10.Jain S, Kuppili PP, Pattanayak RD, Sagar R. Ethics in psychiatric research: Issues and recommendations. Indian J Psychol Med. 2017;39:558–65. doi: 10.4103/IJPSYM.IJPSYM_131_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Raffard S, Fond G, Brittner M, Bortolon C, Macgregor A, Boulenger JP, et al. Cognitive insight as an indicator of competence to consent to treatment in schizophrenia. Schizophr Res. 2013;144:118–21. doi: 10.1016/j.schres.2012.12.011. [DOI] [PubMed] [Google Scholar]
- 12.Hostiuc S, Rusu MC, Negoi I, Drima E. Testing decision-making competency of schizophrenia participants in clinical trials. A meta-analysis and meta-regression. BMC Psychiatry. 2018;18:2. doi: 10.1186/s12888-017-1580-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jhanwar VG, Bishnoi RJ. Comprehensibility of translated informed consent documents used in clinical research in psychiatry. Indian J Psychol Med. 2010;32:7–12. doi: 10.4103/0253-7176.70517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Christopher PP, Foti ME, Roy-Bujnowski K, Appelbaum PS. Consent form readability and educational levels of potential participants in mental health research. Psychiatr Serv. 2007;58:227–32. doi: 10.1176/ps.2007.58.2.227. [DOI] [PubMed] [Google Scholar]
- 15.Indian Council of Medical Research. Ethical Guidelines for Biomedical Research on Human Participants: Indian Council of Medical Research. 2006 [Google Scholar]
- 16.Mathur R, editor. National Ethical Guidelines for Biomedical and Health Research Involving Human Participants. New Delhi: Director-General Indian Council of Medical Research; 2017. [DOI] [PubMed] [Google Scholar]
- 17.GBD 2015. Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rajesh DR, Singh A, Chopra M, Dingh GP, Venkteshan M, Bhardwaj A. Patient's awareness, attitude, understanding and perceptions towards legal nature of informed consent. J Indian Acad Forensic Med. 2013;35:40–3. [Google Scholar]
- 19.Aguilera-Guzmán RM, Mondragón BL, Icaza MM, Elena M. Ethical considerations in community interventions: The pertinence of informed consent. Salud Ment. 2008;31:129–38. [Google Scholar]
- 20.Mfutso-Bengo J, Masiye F, Molyneux M, Ndebele P, Chilungo A. Why do people refuse to take part in biomedical research studies. Evidence from a resource-poor area? Malawi Med J. 2008;20:57–63. doi: 10.4314/mmj.v20i2.10958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim JH, Kim D, Park SH, Nam J. Accept or refuse?. A pilot study of patients’ perspective on participating as imaginary research subjects in schizophrenia. Psychiatry Investig. 2009;6:66–71. doi: 10.4306/pi.2009.6.2.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Al Alawi M, Al Sinawi H, Al Maqbali M, Al Hatmi H. Perception of stigma among attendees of tertiary care psychiatric clinic in Oman. Int J Pub Health Safe. 2016;1:108. [Google Scholar]
- 23.Kumari S, Banerjee I, Majhi G, Chaudhury S, Singh AR, Verma AN. Felt stigma and self-esteem among psychiatric hospital outdoor and community camp attending patients. Med J DY Patil Univ. 2014;7:550–7. [Google Scholar]
- 24.Central Drugs Standard Control Organization. Draft guidelines on audio-visual recording of informed consent process in clinical trial. New Delhi: Ministry of Health & Family Welfare, Government of India; 2014. [accessed on November 5, 2018]. Available from: https://www.iscr.org/wp-content/ uploads/2019/04/Draft_guide_lines_on_Audio-Visual_ Recording_of_ICF_in_clinical_trial_dated_9-January-20 14._57.pdf . [Google Scholar]
- 25.Capdevielle D, Raffard S, Bayard S, Garcia F, Baciu O, Bouzigues I, et al. Competence to consent and insight in schizophrenia: Is there an association?. A pilot study. Schizophr Res. 2009;108:272–9. doi: 10.1016/j.schres.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 26.Palmer BW, Dunn LB, Depp CA, Eyler LT, Jeste DV. Decisional capacity to consent to research among patients with bipolar disorder: Comparison with schizophrenia patients and healthy subjects. J Clin Psychiatry. 2007;68:689–96. doi: 10.4088/jcp.v68n0505. [DOI] [PubMed] [Google Scholar]


