Abstract
Background
Pilonidal sinus arises in the hair follicles in the buttock cleft. The estimated incidence is 26 per 100,000, people, affecting men twice as often as women. These chronic discharging wounds cause pain and impact upon quality of life. Surgical strategies centre on excision of the sinus tracts followed by primary closure and healing by primary intention or leaving the wound open to heal by secondary intention. There is uncertainty as to whether open or closed surgical management is more effective.
Objectives
To determine the relative effects of open compared with closed surgical treatment for pilonidal sinus on the outcomes of time to healing, infection and recurrence rate.
Search methods
For this first update we searched the Wounds Group Specialised Register (24/9/09); The Cochrane Central Register of Controlled Trials (CENTRAL) ‐ The Cochrane Library Issue 3 2009; Ovid MEDLINE (1950 ‐ September Week 3, 2009); Ovid MEDLINE(R) In‐Process & Other Non‐Indexed Citations (September 24, 2009); Ovid EMBASE (1980 ‐ 2009 Week 38); EBSCO CINAHL (1982 ‐ September Week 3, 2009).
Selection criteria
All randomised controlled trials (RCTs) comparing open with closed surgical treatment for pilonidal sinus. Exclusion criteria were: non‐RCTs; children aged younger than 14 years and studies of pilonidal abscess.
Data collection and analysis
Data extraction and risk of bias assessment were conducted independently by three review authors (AA/IM/JB). Mean differences were used for continuous outcomes and relative risks with 95% confidence intervals for dichotomous outcomes.
Main results
For this update, 8 additional trials were identified giving a total of 26 included studies (n=2530). 17 studies compared open wound healing with surgical closure. Healing times were faster after surgical closure compared with open healing. Surgical site infection (SSI) rates did not differ between treatments; recurrence rates were lower in open healing than with primary closure (RR 0.60, 95% CI 0.42 to 0.87). Six studies compared surgical midline with off‐midline closure. Healing times were faster after off‐midline closure (MD 5.4 days, 95% CI 2.3 to 8.5). SSI rates were higher after midline closure (RR 3.72, 95% CI 1.86 to 7.42) and recurrence rates were higher after midline closure (Peto OR 4.54, 95% CI 2.30 to 8.96).
Authors' conclusions
No clear benefit was shown for open healing over surgical closure. A clear benefit was shown in favour of off‐midline rather than midline wound closure. When closure of pilonidal sinuses is the desired surgical option, off‐midline closure should be the standard management.
Plain language summary
Healing by primary versus secondary intention after surgical treatment for pilonidal sinus
Pilonidal sinus is a very common disease of the buttock region which mostly affects young adults (men more than women) and for many with the disease, the condition can be painful and long‐lasting (chronic). The disease is thought to arise from ingrowing hair between the buttocks, which then becomes infected and forms into a "sinus" or tract. Patients with a pilonidal sinus usually present to their doctor with painful swelling around the buttock area, which may discharge pus‐like substance. This disease is usually treated by surgery. Surgeons agree that the area where the infection has developed should be completely incised and removed. However, surgeons have not agreed whether the resulting wound should be stitched closed or left open to heal without stitches. This review of the published literature found that patients who had their wounds closed with stitches healed faster and returned to work earlier than patients whose wounds were left unstitched and allowed to heal "naturally". However, the review also found that patients who had their wounds closed with stitches were more likely to get the disease again compared to those who did not have their wounds closed by stitches. This means that each type of surgical treatment has its advantages and disadvantages, and that the decision about which type of surgical wound to select should also be guided by the patient's own desired goals for treatment. The review also found that if a decision had been made to close the wound with stitches, then the best way to reduce the risk of the disease coming back and reduce other complications (such as infection), was to use a wound technique where the line of stitches was moved away from between the buttocks. Therefore one definitive recommendation from this systematic review is that where a decision has been made to close the sinus wound using stitches, this wound should not lie in the central area of the buttocks.
Background
Description of the condition
The term pilonidal sinus, 'pilus' meaning hair and 'nidal' meaning nest, was first used by Hodges in 1880 to describe an abnormal chronic tract between the buttocks (Werkgartner 2004). Pilonidal disease was termed 'jeep disease' during World War II because many military drivers were found to have the condition (Chinn 2003).
Pilonidal sinus is a disease that arises in the hair follicles of the natal cleft of the sacrococcygeal area (i.e. in the buttock cleft at the bottom of the backbone). It is a common disease with an estimated incidence of 26 per 100,000, affecting men twice as often as women (ratio 2.2 to 1.0) (Sondenaa 1995). The mean age of presentation is 21 and 19 years in men and women respectively (Notaro 2003). Many, but not all patients are hirsute, and an excess incidence has been reported in those who are moderately obese (Notaro 2003).
Originally thought to be a congenital condition, recent studies suggest that pilonidal sinus is an acquired disease that results from one or other of two aetiological mechanisms (causes)(Al‐Naami 2005). First, obstruction of the hair follicles can lead to follicle enlargement and rupture into the subcutaneous tissues causing abscess ‐ and ultimately chronic sinus ‐ formation. Secondly, broken hair can become inserted abnormally into the skin at the natal cleft, provoking a foreign‐body reaction; the subsequent infection results in cyst formation or sinus disease (Al‐Naami 2005).
Patients with pilonidal sinus often present with an acute painful swelling in the natal cleft associated with an abscess with, or without, the drainage of bloody purulent material (pus) from the sinus opening. Alternatively, they may present with a chronically discharging, and often painful, sinus tract. Irrespective of the mode of presentation, the painful nature of the condition causes significant morbidity and, although many tolerate symptoms for up to one year before seeking treatment, there is often a protracted loss of normal activity for these patients.
Description of the intervention
The 'ideal' therapy would be a quick cure that allowed patients to return to normal activity as soon as possible, with minimal pain and a low risk of complications such as recurrence or persistence of the sinus, and ongoing infection. The treatment of a pilonidal sinus‐related acute abscess is well established and consists of immediate drainage of the abscess followed by the slow process of healing by granulation (formation of new tissue in the sinus void). However, management of chronic pilonidal disease is variable, contentious and problematic. The principles of treatment require eradication of the sinus tract, complete healing of the overlying skin and prevention of recurrence. Non‐surgical treatments include the application of phenol, regular shaving and cryosurgery.
How the intervention might work
Surgical techniques are based on either incision, usually of an acute abscess, or excision of a chronic sinus tract. The surgical wound may be left to heal by secondary intention, that is, left open, packed and allowed to heal.
Alternatively, the wound is closed (healing by primary intention) either immediately after surgical treatment (primary wound closure), or after a delay. The best method of closure is a matter of conjecture. Methods can be broadly categorised as either midline closure techniques (with the wound lying within the natal cleft), or other techniques (where the wound is placed out with the midline, or the defect e.g. by using skin grafts or tissue flaps). See Appendix 4 for a glossary of terms.
Why it is important to do this review
There is no clinical consensus over the optimal management of pilonidal sinus. Advocates of open healing by secondary intention argue that this method reduces both wound tension and wound infection because free drainage can occur. Advocates of the surgical closure approach argue that healing is improved by eliminating the rolling action of the buttocks which can be achieved by flattening the gluteal crest. Furthermore, variations in current practice reflect the literature which describes a wide spectrum of outcomes reported for different open and closed surgical techniques for the treatment of pilonidal sinus. There is a need to compare open with closed techniques for the management of pilonidal sinus disease.
Objectives
To determine the relative effects of open surgical techniques compared with closed techniques for the management of pilonidal sinus disease on the outcomes of healing time, infection and rate of recurrence.
Methods
Criteria for considering studies for this review
Types of studies
RCTs comparing two or more surgical techniques that include healing by primary intention (i.e. wounds closed with sutures: closed wounds) or by secondary intention (i.e. wounds left open to heal: open wounds) for the treatment of non‐infected pilonidal sinus disease were included. All non‐randomised studies were excluded.
Types of participants
Any adult participant (over 14 years of age) undergoing surgery to treat pilonidal sinus disease. No distinction was made between new (initial presentation of the disease) and recurrent presentation of pilonidal sinus disease. Studies that included participants presenting with an abscess were excluded except where data could be extracted and analysed separately for those with and without pilonidal abscess.
Types of interventions
Any surgical intervention where wounds were either left open to heal or closed by sutures compared with another surgical intervention, for the treatment of pilonidal sinus disease, was considered eligible for inclusion. If primary surgical closure was used, these interventions were assigned to the "closed" healing group. These included studies comparing different types of surgical closure, e.g. midline versus alternative techniques. The open healing group included wounds that were left open to heal naturally by secondary intention. Trials comparing surgery with non‐surgical intervention were excluded.
Types of outcome measures
In order to be included in the review, studies had to provide data on at least one of the following primary or secondary outcomes:
Primary outcomes
Time to wound healing
Rate of surgical site infection (SSI)/proportion of infected wounds
Rate of recurrence or rate of re‐operation (there may be differences between how these are reported)
Secondary outcomes
Time to return to work (RTW)
Other complications and morbidity
Participant (patient) satisfaction
Cost
Length of hospital stay
Pain
Quality of life
Rate of change of wound volume
Wound healing rate (added post‐protocol)
Operative time (added post‐protocol)
Search methods for identification of studies
Electronic searches
For the first update of this review we searched the following databases:
Cochrane Wounds Group Specialised Register (Searched 24/9/09)
The Cochrane Central Register of Controlled Trials (CENTRAL) ‐ The Cochrane Library 2009 Issue 3
Ovid MEDLINE ‐ 1950 to September Week 3 2009
Ovid MEDLINE(R) In‐Process & Other Non‐Indexed Citations (September 24, 2009)
Ovid EMBASE ‐ 1980 to 2009 Week 38
EBSCO CINAHL ‐ 1982 to September Week 3 2009
We used the following search strategy on CENTRAL, developed in collaboration with the Cochrane Wounds Group Trial Search Co‐ordinator.
#1 MeSH descriptor Pilonidal Sinus explode all trees #2 pilonidal* #3 (pilonidal near/3 sinus*) #4 (pilonidal near/3 fistula*) #5 (pilonidal near/3 cyst*) #6 (pilonidal near/3 disease*) #7 (pilonidal near/3 abscess*) #8 natal near cleft #9 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8)
The search strategies for Ovid MEDLINE, Ovid EMBASE and EBSCO CINAHL can be found in Appendix 1, Appendix 2 and Appendix 3 respectively. The Ovid MEDLINE search was combined with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE: sensitivity‐ and precision‐maximizing version (2008 revision); Ovid format (Lefebvre 2008). The EMBASE and CINAHL searches were combined with the trial filters developed by the Scottish Intercollegiate Guidelines Network (SIGN) (SIGN 2009). No date or language restrictions were applied and translations of all relevant non‐English language papers were obtained using local resources.
Searching other resources
Handsearching journals We deemed handsearching of journals as unnecessary because all likely high‐yield publications were either included within the above search strategies or had already been handsearched and included in the Wounds Group Specialised Register. A list of journals currently being handsearched by The Cochrane Collaboration is available at the US Cochrane Center Handsearch master list page: http://apps1.jhsph.edu/cochrane/masterlist.asp.
We sent emails or letters to all authors of included studies requesting information on unpublished data and ongoing studies. We also searched the bibliographies of all included studies and review papers to identify other potentially suitable studies.
Data collection and analysis
Selection of studies
For the update of this review three review authors (AA/IM/JB) independently examined the titles and abstracts of articles identified in the searches as reporting potentially relevant trials. From this initial assessment, we obtained full versions of all potentially relevant articles. Any disagreements were resolved by discussion. We removed duplicate citations, although duplicate publications reporting data in more than one paper were obtained for full consideration.
Data extraction and management
We recorded the extracted data on data extraction forms. Two review authors (AA and IM) had independently developed and piloted the forms using three RCTs. The same review authors independently conducted full data extraction and disagreements were resolved by a third review author (JB).
Assessment of risk of bias in included studies
Two review authors independently undertook assessment of the risk of bias of each study as part of the data extraction process. Assessors were not blinded to the authors of individual trials. The review authors undertook appraisal of the risk of selection, performance, attrition and detection biases by assessing the following key items:
Sequence generation
Was the allocation sequence adequately generated e.g. coin toss, random number tables, computer generated? Recorded as yes, no or unclear.
Allocation concealment
Was allocation adequately concealed in a way that would not allow both the investigators and the participants to know or influence the intervention group before an eligible participants is entered into the study e.g. central randomisation, or sequentially numbered, opaque, sealed envelopes? Recorded as yes, no, or unclear.
Incomplete outcome data
Were incomplete outcome data adequately addressed? Incomplete outcome data essentially include: attrition, exclusions and missing data. If any withdrawals occurred, were they described and reported by treatment group with reasons given? Whether or not there were clear explanations for withdrawals and dropouts in treatment groups was recorded. An example of an adequate method to address incomplete outcome data is the use of intention to‐treat analysis (ITT). This key item was recorded as: yes, no, or unclear.
Selective outcome reporting
Are reports of the study free from suggestion of selective outcome reporting? This was interpreted as no evidence that statistically non‐significant results might have been selectively withheld from publication e.g. selective under reporting of data, or selective reporting of a subset of data. Recorded as yes, no, or unclear.
Other sources of bias
Was the study apparently free of other problems that could put it at a high risk of bias e.g. baseline imbalance, or the use of insensitive instrument to measure outcomes? Recorded as yes, no, or unclear.
Blinding
Details of blinding participants, personnel (surgeons) and outcome assessors were assessed. Recorded as yes, no, or not possible.
We completed a risk of bias table for each eligible study. We discussed any disagreement amongst all review authors to achieve a consensus. Quality assessment criteria was categorised as low, unclear or high risk of bias according to the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008). We presented assessment of risk of bias using a 'risk of bias summary figure', which presents all of the judgements in a cross‐tabulation of study by entry. This display of internal validity indicates the weight the reader may give the results of each study.
Assessment of heterogeneity
We investigated the following factors as potential causes of heterogeneity using the framework below:
Clinical diversity
For example: study location and setting, full characteristics of participants (e.g. age/sex/social class), co‐morbidity and treatments that participants may be receiving on entry to the trial. We considered how outcomes were measured, definitions of outcomes and the outcomes recorded. Depending upon how diverse these factors were across studies, we analysed these separately or presented them using a narrative approach.
Methodological diversity
For example: assessment of randomisation process, study quality and analytical method.
Statistical diversity
This was assessed by looking at the estimates of treatment effect in included studies and considering whether combining estimates would produce a meaningful overview. This was conducted using forest plots generated by the Cochrane RevMan software. The chi‐square test and I‐squared statistic were used, which examines the percentage of total variation across studies due to heterogeneity rather than due to chance (Higgins 2003). An I2 value of more than 50% would be considered at high risk of heterogeneity (Higgins 2008). This was taken into consideration and random effects models were used where appropriate as detailed in analysis text and graphs. Where data were too diverse for combining effect sizes or data seemed inappropriate to combine, data were summarised using a narrative approach.
Data synthesis
Quantitative data were entered into the Cochrane RevMan 5 program and analysed using Cochrane MetaView. For each outcome, summary estimates of treatment effect were calculated (with 95% Confidence Interval (CI)) for each comparison. For continuous outcomes, mean differences (MD) were calculated when appropriate. For dichotomous outcomes, relative risk (RR) or Peto odds ratio (OR) were calculated where appropriate. A Peto OR was used to calculate the effect estimates where the event rate was low and also where there were zero events.
Wound healing time and RTW were time to event data and analysed where appropriate using survival approaches (as described in the Cochrane Reviewer's Handbook version 5.0.1, Chapter 8). Where it was not appropriate to pool data, the results were presented narratively and in table format.
Subgroup analysis and investigation of heterogeneity
Studies were analysed by three surgical closure techniques: open healing, closed wound on the midline of the natal cleft (midline surgical closure) and closed wound using other off‐midline methods (closed other off‐midline). Closed 'other' included closure techniques lying off‐midline, including all plastic and advancement techniques where the surgical wound lies off the midline of the natal cleft.
Surgical techniques were assigned to the open healing group if the wound was allowed to heal either fully or partially by secondary intention. If the wound was closed by primary intention and the suture line lay in the midline of the natal cleft, surgical techniques were assigned to the closed (midline) group. Surgical techniques were assigned to closed (other) if the wound was closed by primary intention and the suture line lay off the midline of the natal cleft.
The following analyses were planned:
Open healing compared with closed wound (all)
Open healing compared with closed wound (midline)
Open healing compared with closed wound (other)
Closed wound (midline) compared with closed wound (other)
Closed wound (other) compared with closed wound (other) (added post‐protocol)
Results
Description of studies
Results of the search
For the initial review we undertook full bibliographic searches in February 2007. Two review authors (JB/IM) independently read a total of 1367 titles and abstracts and where discrepancies arose, a third review author (PMK) was consulted or the full paper was obtained for review. The first review retrieved 45 potential papers for full assessment, of which 18 studies were included and 26 studies were excluded. We were unable to trace one paper (Khalid 2001).
Searches were run in September 2009 for the updated review, a total of 67 citations were retrieved and screened by three review authors (AA,IM, JB), differences were resolved by discussion. A total of 16 trial reports were identified as needing assessment in full, one trial report was untraceable (Amorín 1989) and therefore was added to the Table of excluded studies. One paper was not identified by bibliographic searching but was retrieved when doing an author search (Sheikh 2007). Of the 16 potentially eligible trials, 8 new trials met the inclusion criteria (Al‐Salamah 2007; Ersoy 2009; Jamal 2009; Karakayali 2009; Kareem 2006; Nordon 2009; Sakr 2006; Sheikh 2007) and 8 studies were added to the Characteristics of excluded studies table. A total of 26 trials were included in the review.
Included studies
The trials included in the review were published between 1985 and 2009. Of the 26 trials included, 8 studies were from Turkey, 4 from the UK, 3 from Pakistan, and 2 from Egypt. The rest were from United Arab Emirates (UAE), Kingdom of Saudi Arabia (KSA), Kuwait, Iraq, Iran, Italy, Croatia, Denmark, and Norway. In term of geographical region, most studies have been conducted in Southern Europe (n=12) followed by the Middle East (n=7). The Norwegian study group published two papers on their participant cohort, one reporting short‐term outcome (Søndenaa 1992) and a follow‐up assessment of recurrence at four years postoperatively (Søndenaa 1996). These have been included as one trial (2 papers) as they contain the same participant cohort. SSI rate, recurrence, time of return to work, time to wound healing and other complications are reported in the 1992 paper and then recurrence only reported in the 1996 manuscript. Recurrence figures were used from the 1996 paper (representing the best length of follow‐up) whilst all other data were extracted from the 1992 report. No data were double‐counted.
A British group from Queen Alexander Hospital in Chichester published an abstract (Nordon 2005) and a paper (Nordon 2009) comparing off‐midline technique with another off‐midline technique. The abstract reported healing rate and RTW (Nordon 2005) and the published paper reported RTW, recurrence, and healing rate (Nordon 2009). Contact with the study authors revealed that the participants in the abstract were a subset of the same participants in the full publication; this RCT has been included as a single study.
Of the 26 included studies, 8 studies (Abu Galala 1999; Akca 2005; Hameed 2001; Karakayali 2009; Miocinovic 1999; Mohamed 2005; Sheikh 2007; Testini 2001) only recruited participants with new pilonidal sinus disease presentation. A similar number of studies recruited participants with new and recurrent pilonidal sinus (al‐Hassan 1990; Al‐Salamah 2007; Berkem 2005; Gencosmanoglu 2005; Jamal 2009; Kronborg 1985; Nordon 2009; Sakr 2006). One study (Cihan 2006) enrolled participants with only recurrence pilonidal sinus disease. Nine studies (Ersoy 2009; Ertan 2005; Fazeli 2006; Füzün 1994; Kareem 2006; Khawaja 1992; Rao 2001; Søndenaa 1992; Wright 2001) did not report whether they recruited participants with new or recurrent disease.
Overall, sample size within individual trials ranged from 26 to 380 participants and the total number of included participants was 2530. Of the studies that reported sex distribution, males represented 1825 (82%) of total participants. Four studies did not report details of age or sex distribution (Søndenaa 1992; Füzün 1994; Rao 2001; Wright 2001).
CHARACTERISTICS OF INTERVENTIONS
Of the 26 studies: 12 studies compared open wound healing with midline surgical closure (Al‐Salamah 2007; al‐Hassan 1990; Füzün 1994; Gencosmanoglu 2005; Hameed 2001; Kareem 2006; Khawaja 1992; Kronborg 1985; Miocinovic 1999; Mohamed 2005; Rao 2001; Søndenaa 1992); 5 trials compared open wound healing with closed wounds using non‐midline methods (other) (Fazeli 2006; Jamal 2009; Karakayali 2009; Sheikh 2007; Testini 2001); 6 studies compared closed (midline) with closed (other/off‐midline) (Abu Galala 1999; Akca 2005; Berkem 2005; Ertan 2005; Sakr 2006; Wright 2001) and 3 studies compared closed (other/off‐midline) with closed (other/off‐midline) (Cihan 2006; Ersoy 2009; Nordon 2009).
Open healing surgical techniques reported in the included studies were described, for example, as: wide excision, limited excision, marsupialisation (partial opposition of the wound edges leaving smaller area and thus wound to heal by secondary intention), Obeid's technique and other forms of postoperative packing of the wound as long as primary closure of the wound edges using sutures was not achieved.
Surgical techniques where wounds were closed on the midline included descriptions such as: midline closure, primary midline closure, and healing by primary intension. Closed wounds using off‐midline methods (other) included descriptions such as: rhomboid flap (also known as Limberg flap) (Abu Galala 1999; Akca 2005; Cihan 2006; Ersoy 2009; Ertan 2005; Karakayali 2009), V‐Y advancement flap (Berkem 2005), Bascom procedure (Nordon 2009; Wright 2001), Karydakis technique (Sakr 2006; Sheikh 2007) and z‐plasty (Fazeli 2006).
One study (Mohamed 2005) had three trial arms and participants were assigned to subgroups, where one arm was midline closure, therefore they were categorised as midline closure group. The second arm was wide excision and the third was limited excision, so for the purposes of this review both were combined, treated as one arm and categorised as open healing group.
See Appendix 4 for a glossary of terms.
CHARACTERISTICS OF OUTCOME MEASURES
Time to wound healing.
Full epithelialisation (healing) of the wound was considered as the definition of wound healing. Fifteen of the 26 studies reported time to wound healing; where data were reported by authors as units of weeks, these were converted into units of days. Few studies provided a specific definition of wound healing. The median value was used to summarize time to wound healing data in four of the 15 studies (Gencosmanoglu 2005; Kronborg 1985; Khawaja 1992; Rao 2001) and data are presented in Table 6. One study presented percentage data graphically therefore it was not possible to extract actual values for time to wound healing. An attempt was made to contact authors for data but no reply was received (Mohamed 2005). Ten studies (al‐Hassan 1990; Al‐Salamah 2007; Ertan 2005; Fazeli 2006; Hameed 2001; Kareem 2006; Jamal 2009; Karakayali 2009; Sheikh 2007; Søndenaa 1992) reported wound healing time as a continuous variable using mean (SD) values. Data on time to wound healing are presented in Table 6.
1. Time to wound healing (days).
| Study | Comparison | Experimental group | Control (closed) group | Sample Size E | Sample Size C | P value | Results format |
| Gencosmanoglu 2005 | Open vs closed (midline) | 79 (21, 112) | 14 (14, 63) | 73 | 69 | <0.001 | Median (range) |
| Kronborg 1985 | Open vs closed (midline) | 64 (17, 157) | 13 (7, 203) | 32 | 33 | nr | Median (range) |
| Rao 2001 | Open vs closed (midline) | 61 (34, 132) | 27 (24, 68) | 30 | 29 | <0.001 | Median (range) |
| Khawaja 1992 | Open vs closed (midline) | 41 (nr) | 14 (nr) | 23 | 23 | ‐23 (‐28, ‐20) | Median difference (95% CI) |
| al‐Hassan 1990 | Open vs closed (midline) | 91 (28‐546) | 10.3 (10‐15) | 40 | 42 | nr | Mean (range) |
| Hameed 2001 | Open vs closed (midline) | 70 (59‐91) | 14.5 (12‐21) | 20 | 23 | <0.05 | Mean (range) |
| Søndenaa 1992 | Open vs closed (midline) | 70 (28‐266) | 14 (14‐126) | 59 | 60 | <0.001 | Median (range) |
| Al‐Salamah 2007 | Open vs closed (midline) | 60.4 ± 6.2 (39‐87) | 14.5 ± 4.1 (10‐35) | 192 | 188 | <0.001 | Mean±SD (range) |
| Kareem 2006 | Open vs closed (midline) | 48.02 ± 11.34 (28‐63) | 19.95 ± 6.23 (14‐28) | 37 | 40 | <0.001 | Mean±SD (range) |
| Jamal 2009 | Open vs closed (off‐midline) | 120.08 ± 31.59 (60‐180) | 20.13±8.99 (15‐60) | 25 | 24 | nr | Mean±SD (range) |
| Karakayali 2009 | Open vs closed (off‐midline) | 43.8 ± 20.9 (15‐122) | 23.7 ± 11.2 (14‐96) | 70 | 70 | <0.001 | Mean±SD (range) |
| Sheikh 2007 | Open vs closed (off‐midline) | 46.83 (9.24) | 17.22 (7.56) | 13 | 13 | nr | Mean (SD) |
| Fazeli 2006 | Open vs closed (off‐midline) | 41 (20‐160) | 15.4 (10‐34) | 72 | 72 | <0.001 | Mean (range) |
| Ertan 2005 | Closed (midline) vs closed (off‐midline) | 15.7 (7‐38) | 10.3 (5‐22) | 50 | 50 | 0.001 | Mean (range) |
nr= not reported
It is not appropriate to analyse time‐to‐event data, such as time to healing, using methods for continuous outcomes (e.g. using mean times‐to‐event) as the relevant times are only known for the subset of participants who have experienced the event (e.g., healing). The most appropriate way of summarizing time‐to‐event data is to use methods of survival analysis and express the intervention effect as a hazard ratio. A hazard ratio is interpreted in a similar way to a risk ratio, as it describes how many times more (or less) likely a participant is to experience the event at a particular point in time if they receive the experimental rather than the control intervention. Inappropriate analysis of outcome data can introduce bias in the interpretation of the results. All studies reporting time to healing as an outcome report data as continuous (except Mohamed 2005 who reported it in graphical form)
Rate of surgical site infection (SSI)/proportion of wounds that became infected postoperatively.
The rate of SSI was reported by 17 studies (Abu Galala 1999; Akca 2005; Al‐Salamah 2007; Berkem 2005; Cihan 2006; Ersoy 2009; Ertan 2005; Fazeli 2006; Füzün 1994; Gencosmanoglu 2005; Hameed 2001; Jamal 2009; Karakayali 2009; Kareem 2006; Rao 2001;Sakr 2006; Sheikh 2007). Few studies gave a clear definition of SSI. Some studies reported other outcomes such as flap oedema, dehiscence and maceration and these were included in "Other complications and morbidity" outcome category.
Recurrence rate
All studies except one (Ersoy 2009) reported recurrence rate, therefore this was the most commonly reported outcome in the review. Recurrence was analysed based on the length of follow‐up (categorised as less than or more than one year) and the proportion of participants followed up (more than or less than 80%). As mentioned above, the Norwegian group published two papers (Søndenaa 1992; Søndenaa 1996) on the same participant cohort with follow‐up at one and four years. Only recurrence data at four years were included to prevent duplicate data entry. As with time to wound healing, recurrence could be analysed using time‐to‐event (e.g. survival) analysis, however none of the included trials reported individual data on time to recurrence.
Time to return to work
Time to RTW reported by 18 studies (Ertan 2005; Cihan 2006; Fazeli 2006; Testini 2001; al‐Hassan 1990; Abu Galala 1999; Nordon 2009; Søndenaa 1992; Füzün 1994; Sheikh 2007; Akca 2005; Al‐Salamah 2007; Sakr 2006; Ersoy 2009; Karakayali 2009; Gencosmanoglu 2005; Khawaja 1992; Kareem 2006) These data were either reported in days or converted into units of days (Table 7). Median (IQR/range) values were reported in 5 studies (Gencosmanoglu 2005; Nordon 2009; Akca 2005; Khawaja 1992; Ersoy 2009). One additional study by Wright 2001, was published as a conference abstract and although stated that RTW data were recorded, these were not reported in the abstract. All studies implied that all participants returned to work therefore this 'time to event' variable was presented using mean (SD) days.
2. Time to return work (days).
| Study | Comparison | Experimental group | Control group | SS E | SS_C | P value | Results format |
| al‐Hassan 1990 | Open vs closed (midline) | 28 (nr) | 14 (nr) | 50 | 46 | nr | Mean (SD) |
| Al‐Salamah 2007 | Open vs closed (midline) | 42.2 (5.3) | 15.6 (3.4) | 192 | 188 | <0.001 | Mean (SD) |
| Füzün 1994 | Open vs closed (midline) | 17.6 (12‐21) | 10.7 (9‐21) | 55 | 55 | <0.05 | Mean (range) |
| Kareem 2006 | Open vs closed (midline) | 35.51 (5.06) | 10.35 (2.72) | 37 | 40 | <0.0001 | Mean (SD) |
| Søndenaa 1992 | Open vs closed (midline) | 27.39 (36.82) | 15.4 (9.17) | 58 | 55 | <0.002 | Mean (SD) |
| Khawaja 1992 | Open vs closed (midline) | 42 (nr) | 19.5 (nr) | 23 | 23 | ‐22 (‐26, ‐17) | Median difference (95% CI) |
| Gencosmanoglu 2005 | Open vs closed (midline) | 3 (2, 8) | 21 (14, 63) | 73 | 69 | <0.001 | Median (range) |
| Karakayali 2009 | Open healing vs closed (off‐midline) | 11.2 (5.8) | 17.9 (9.3) | 70 | 70 | <0.001 | Mean (SD) |
| Sheikh 2007 | Open healing vs closed (off‐midline) | 8.15 (1.46) | 3.53 (1.33) | 13 | 13 | nr | Mean (SD) |
| Testini 2001 | Open vs closed (off‐midline) | 25.7 (11‐77) | 10.4 (5‐32) | 50 | 50 | <0.0001 | Mean (range) |
| Fazeli 2006 | Open vs closed (off‐midline) | 17.5 (nr) | 11.9 (nr) | 72 | 72 | <0.001 | Mean |
| Akca 2005 | Closed (midline) vs closed (off‐midline) | 19 (15, 20) | 9.5 (8, 12) | 100 | 100 | <0.001 | Median (IQR) |
| Ersoy 2009 | Closed (off‐midline) vs closed (off‐midline) | 15 (5‐45) | 14 (5‐46) | 50 | 50 | 0.346 | Median (range) |
| Nordon 2009 | Closed (off‐midline) vs closed (off‐midline) | 14 (7‐42) | 14 (3.5‐28) | 29 | 26 | nr | Median (range) |
| Abu Galala 1999 | Closed (midline) vs closed (off‐midline) | 14 (nr) | 23 (nr) | 22 | 24 | 0.0001 | Mean |
| Sakr 2006 | Closed (midline) vs closed (off‐midline) | 21‐28 | 21‐28 | 82 | 79 | nr | Range |
| Ertan 2005 | Closed (midline) vs closed (off‐midline) | 28.5 (14‐60) | 15.8 (7‐25) | 50 | 50 | 0.001 | Mean (range) |
| Cihan 2006 | Closed (off‐midline) vs closed (off‐midline) | 11.7 (0.45) | 9.3 (0.34) | 35 | 33 | 0.001 | Mean (SD) |
nr= not reported
Similarly time to return to work is also a type of time‐to‐event data and should not be analysed using methods for continuous outcomes.
Other complications and morbidity.
Other complications and morbidity outcome was reported by 14 studies (Ertan 2005; Cihan 2006; Fazeli 2006; Gencosmanoglu 2005; Testini 2001; al‐Hassan 1990; Jamal 2009; Hameed 2001; Søndenaa 1992; Akca 2005; Khawaja 1992; Kareem 2006; Sakr 2006; Sheikh 2007). Postoperative complications reported by studies included: bleeding, dehiscence, maceration, primary failure, hematoma, and flap oedema.
Participant satisfaction.
Participant satisfaction was reported in only two of the 26 trials (Ertan 2005; Mohamed 2005). A Turkish study used a VAS to assess participant satisfaction (Ertan 2005) and an Egyptian study reported satisfaction rate as 'satisfied or not satisfied' (Mohamed 2005).
Cost
One Pakistani study compared the cost of open versus closed midline repair (Hameed 2001). Although these cost values apply to the Pakistani health system, they were converted from rupees into Sterling (exchange rate based on 03/06/2009).
Length of hospital stay.
Length of hospital stay (LOS) was reported by 12 studies (Akca 2005; Fazeli 2006; Mohamed 2005; Testini 2001; al‐Hassan 1990; Hameed 2001; Jamal 2009; Karakayali 2009; Khawaja 1992; Füzün 1994; Al‐Salamah 2007; Sakr 2006), two of which were reported as median values (Table 8) (Akca 2005; Khawaja 1992). All data were converted into units of days. Reporting of this outcome varied across studies. Some study groups discharged participants after a standard period of time if no complications occurred (i.e. discharge was influenced by complications rate or complication dependent) (al‐Hassan 1990; Jamal 2009; Hameed 2001). In other centres, LOS was based on participant choice (Karakayali 2009).
3. Length of stay (days).
| Study name | Comparison | Experimental group | Control group | Sample size E | Sample size C | P value | Results format |
| al‐Hassan 1990 | Open vs closed (midline) | 3 (nr) | 3 (nr) | 50 | 46 | nr | Mean |
| Al‐Salamah 2007 | Open vs closed (midline) | 4.0 (1.1) | 3.6 (1.4) | 192 | 188 | <0.002 | Mean (SD) |
| Füzün 1994 | Open vs closed (midline) | 2.4 (1‐4) | 4.7 (3‐11) | 55 | 55 | <0.05 | Mean (range) |
| Kareem 2006 | Open vs closed (midline) | 4.27 (2.52) | 1 (0) | 37 | 40 | p<0.0001 | Mean (SD) |
| Mohamed 2005 | Open vs closed (midline) | 1.9 (1.1) | 3.76 (0.2) | 55 | 28 | <0.001 | Mean (SD) |
| Khawaja 1992 | Open vs closed (midline) | 3 (nr) | 1 (nr) | 23 | 23 | nr | Median |
| Fazeli 2006 | Open vs closed (off‐midline) | 1.76 (nr) | 2.86 (nr) | 72 | 72 | <0.001 | Mean |
| Jamal 2009 | Open vs closed (off‐midline) | 5.68 (1.25) | 4.04 (1.12) | 25 | 24 | <0.002 | Mean (SD) |
| Karakayali 2009 | Open vs closed (off‐midline) | 1.3 (0.5) | 1.6 (0.8) | 70 | 70 | 0.009 | Mean (SD) |
| Testini 2001 | Open vs closed (off‐midline) | 0.33 (0.17‐0.5) | 0.46 (0.13‐0.67) | 50 | 50 | nr | Mean (range) |
| Abu Galala 1999 | Closed (midline) vs closed (off‐midline) | 9 (nr) | 6 (nr) | 22 | 24 | <0.0001 | Mean |
| Ertan 2005 | Closed (midline) vs closed (off‐midline) | 4.6 (2‐14) | 3.4 (2‐8) | 50 | 50 | <0.005 | Mean (range) |
| Sakr 2006 | Closed (midline) vs closed (off‐midline) | 2.2 (0.4) | 2.7 (0.5) | 82 | 79 | >0.05 (ns) | Mean (SD) |
| Berkem 2005 | Closed (midline) vs closed (off‐midline) | 3 (2, 6) | 3 (2,7) | 16 | 18 | 0.62 | Median (range) |
| Cihan 2006 | Closed (off‐midline) vs closed (off‐midline) | 5.7 (0.6) | 3.6 (0.2) | 35 | 33 | <0.01 | Mean (SD) |
nr=not reported
Pain
Postoperative pain was reported as proportion or rate of participants experiencing pain and mean pain scores per group, respectively. Six studies reported mean/median pain scores (Ertan 2005; Akca 2005; Rao 2001; Wright 2001; Ersoy 2009) (Table 9) and one of these (Karakayali 2009) recorded pain before surgery, 1 week and 3 months after surgery (Table 10). The Turkish study by Karakayali 2009 used the McGill Pain Questionnaire (MPQ) and sub‐scores for present pain intensity (PPI), pain rating intensity (PRI) and VAS score (Table 10). Two studies reported rates of pain (Testini 2001; Søndenaa 1992). One study used a Verbal Rating System (VRS) to assess pain severity and presented graphical results, which were extracted and interpreted (Jamal 2009).
4. Pain score (median, range).
| Study | Comparison | Experimental group | Control group | SS_E | SS_C | P value |
| Rao 2001 Pain score day 4 | Open vs closed (midline) | 35 (0, 63) | 10 (0, 73) | 30 | 29 | <0.05 |
| Ersoy 2009 Pain score VAS | Closed (off‐midline) vs closed (off‐midline) | 4 (0‐10) | 4(0‐9) | 50 | 50 | 0.161 |
VAS = Visual Analogue Scale
ns= non‐significant
5. Karakayali trial: MPQ & VAS at 1 & 3 months (Mean ± SD).
| Scale and subscales | Open‐N=70 | Closure(off‐midline)‐N=70 | P‐value |
| Present Pain Intensity (PPI) 1 week 3months | 5.3 ± 2.9 1.0 ± 2.0 | 2.4 ± 1.3 0.3 ± 0.5 | <0.001 0.900 |
| Pain Rating Index (PRI) 1week 3 months | 5.3 ± 2.9 1.0 ± 2.0 | 9.4 ± 3.3 1.4 ± 2.4 | <0.001 0.298 |
| VAS (0=bad; 10=no pain) 1week 3months | 6.1 ± 1.7 8.8 ± 1.4 | 4.4 ± 1.9 8.8 ± 1.9 | <0.001 0.918 |
PPI= Present Pain Intensity; PRI= Pain Rating Index, VAS = Visual Analogue Scale
Quality of life
Ertan 2005 assessed quality of life using the SF‐36 questionnaire. Although the mean scores for each of the eight SF‐36 domains were reported, summary scores for physical and mental components were not reported (Table 11). As a result, tables of individual domains were not included in the analysis. Karakayali 2009 assessed quality of life preoperatively and 3 months postoperatively using the Cardiff Wound Impact Schedule (CWIS). This questionnaire has 33 items in four domains: physical functioning, well‐being, overall quality of life, and satisfaction with quality of life; higher scores indicate better quality of life. Scores are transformed from 0 to 100 however scores for overall quality of life and satisfaction with quality of life are scored from 0 to 10. The Karakayali 2009 study reported scores for different follow‐up periods (Table 12).
6. Ertan trial: SF‐36 Quality of life scores at 1 year (Mean (SD)).
| Item | Midline closure N=50 | Off‐midline N=50 | P value |
| General health perception | 71.1 (11.7) | 78.2 (14.1) | 0.008 |
| Physical functioning | 74.8 (12.9) | 77.6 (14.8) | ns |
| Social functioning | 87.3 (32.8) | 110.4 (33.8) | 0.001 |
| Role limitation physical | 42.5 (29.1) | 49.5 (41.1) | ns |
| Role limitation emotional | 57.3 (33.0) | 54.6 (44.5) | ns |
| Pain | 54.5 (14.0) | 67.5 (18.4) | 0.001 |
| Energy & vitality | 77.5 (16.8) | 72.9 (17.2) | ns |
| Mental health | 79.5 (12.3) | 77.6 (13.1) | ns |
ns=non‐significant
7. Karakayali: pre & post (3 months) QoL using Cardiff Wound Impact Schedule (Mean ± SD).
| Pre‐operative | P‐value | Post‐operative | P‐value | |||
| Open | Closed (off‐midline) | Open | Closed (off‐midline) | |||
| Physical‐functioning | 59.9±16.5 | 61.5±16.9 | 0.560 | 57.2±16.3 | 87.3±16.5 | <0.001 |
| Well‐being | 41.5±18.2 | 42.1±16.0 | 0.832 | 28.8±16.1 | 54.7±16.5 | <0.001 |
| Overall quality of life | 5.0±1.9 | 4.4±1.6 | 0.064 | 5.7±1.7 | 7.6±1.5 | <0.001 |
| Satisfaction with quality of life | 5.3±1.8 | 4.9±1.7 | 0.162 | 6.1±1.6 | 7.7±1.6 | <0.001 |
Rate of change of wound volume
Rate of change of wound volume was not reported in any included studies.
Wound healing rate
This outcome was analysed as the number of wounds reported healed within and beyond six months postoperatively. Wound healing rate was reported in 7 studies of the 26 included in the review (Testini 2001; al‐Hassan 1990; Kronborg 1985; Abu Galala 1999; Søndenaa 1992; Rao 2001; Sakr 2006). This outcome was analysed as the number of wounds reported as healed within and beyond six months postoperatively.
Operative time
This is outcome was added post‐protocol and was reported in 8 studies (Mohamed 2005; Hameed 2001; Jamal 2009; Karakayali 2009; Kareem 2006; Al‐Salamah 2007; Sakr 2006; Sheikh 2007). This outcome was analysed as continuous data (minutes).
Risk of bias in included studies
Two review authors independently undertook assessments of the risk of bias associated with the 26 trials during the data extraction process. The assessors were not blinded to study authors. Figure 1 presents a summary of risk of bias for individual studies using the five key domains described:
1.
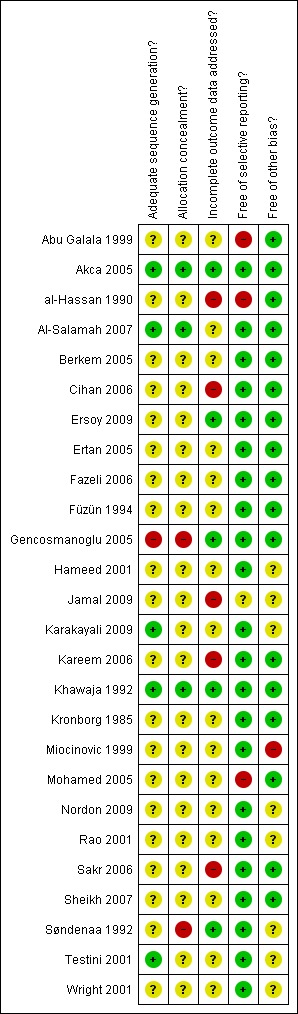
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Sequence generation
Allocation concealment
Incomplete outcome data adequately addressed
Evidence of selective outcome reporting
Evidence of other sources of bias
As with many surgical interventions, blinding of participants and surgeon to interventions is not possible. In general, this can sometimes apply to outcome assessors, particularly when they assess surgical outcomes that require visual inspection e.g. time to wound healing, postoperative complications and recurrence. However, outcomes such as pain, cost, participant satisfaction, self‐reported quality of life, and RTW can be assessed objectively. Nonetheless, a decision not to include blinding in the risk of bias criteria was reached.
Using the risk of bias criteria mentioned above, studies were classified accordingly to: (a) Low risk of bias ‐ (all key items suggested low risk of bias); (b) Unclear risk of bias ‐ (unclear risk of bias for one or more key items); or (c) High risk of bias ‐ (high risk of bias for one or more key items) according to the Cochrane Handbook version 5.0.1 (Higgins 2008). Figure 1 illustrates risk of bias data as recommended by The Cochrane Collaboration Higgins 2008. The symbol "+" indicates low risk of bias, "?" indicates unclear risk of bias, and "‐" indicates high risk of bias.
Out of the 26 studies, five studies used an adequate method of generating the randomisation sequence (Testini 2001; Karakayali 2009; Akca 2005; Khawaja 1992; Al‐Salamah 2007). However, allocation concealment was only adequately achieved in 3 studies (Akca 2005; Khawaja 1992; Al‐Salamah 2007). Similarly, only five studies adequately addressed incomplete outcome data (Gencosmanoglu 2005; Akca 2005; Søndenaa 1992; Khawaja 1992; Ersoy 2009). The majority of studies (22 out of 26) were free of selective outcome reporting; the four studies who were not free or were unclear were: Abu Galala 1999; al‐Hassan 1990; Jamal 2009; Mohamed 2005 and details are outlined in the risk of bias table.
Furthermore, two‐thirds (17 out of 26) were free of other biases, such as evidence of baseline imbalance or incorrect statistical analysis (Ertan 2005; Cihan 2006; Berkem 2005; Fazeli 2006; Mohamed 2005; Gencosmanoglu 2005; al‐Hassan 1990; Kronborg 1985; Abu Galala 1999; Akca 2005; Füzün 1994; Khawaja 1992; Kareem 2006; Al‐Salamah 2007; Sakr 2006; Ersoy 2009; Sheikh 2007).
Only two studies adequately fulfilled all risk of bias criteria and were considered to be at low risk of bias and thus of high methodological quality (Akca 2005;Khawaja 1992). Ten studies were considered to be at high risk of bias and poor methodological quality (Cihan 2006; Mohamed 2005; Gencosmanoglu 2005; al‐Hassan 1990; Abu Galala 1999; Jamal 2009; Søndenaa 1992; Miocinovic 1999; Kareem 2006; Sakr 2006). The remaining studies were graded as unclear risk of bias and thus of intermediate methodological quality.
Effects of interventions
Comparison of open wound healing with closed surgical technique (all techniques) for pilonidal sinus (Analysis 01)
In each outcome section, data from open wound healing compared with all closed techniques are presented first. This is followed by reporting of subgroup analyses where data are available: open healing vs. closed wound (midline); open vs closed (other).
Primary outcomes
Time to wound healing
Data were not pooled for time to wound healing due to the high statistical heterogeneity ( I2 = 97%). Data are presented in Table 6. Furthermore the data have not been analysed by survival methods and the mean time to healing data may give an inaccurate, and even biased, impression (since non‐healers do not contribute information). Most studies do not explicitly state that all participants achieved complete healing and therefore the time to healing data should be treated with caution.
Of the 13 studies incorporating 1421 participants reporting time to wound healing, 9 studies reported significantly faster (mean/median) time to wound healing after primary closure (Fazeli 2006; Gencosmanoglu 2005; Hameed 2001; Karakayali 2009; Søndenaa 1992; Rao 2001; Khawaja 1992; Kareem 2006; Al‐Salamah 2007). The other 4 studies (al‐Hassan 1990; Kronborg 1985; Jamal 2009; Sheikh 2007) reported similar results, though no formal statistical tests were reported. Only one study was of low risk of bias (Khawaja 1992).
Rate of surgical site infection/proportion of infected wounds (Analysis 1.1)
Ten studies (1231 participants) reported rate of SSI after open compared with closed (all) treatments (Al‐Salamah 2007; Fazeli 2006; Füzün 1994; Gencosmanoglu 2005; Hameed 2001; Jamal 2009; Karakayali 2009; Kareem 2006; Sheikh 2007; Søndenaa 1992). Heterogeneity was acceptable (I2 = 21%) therefore data were pooled using a fixed effect model. There was no significant difference in the rate of SSI between the two treatments (RR 1.31, 95% CI 0.93 to 1.85) (Analysis 1.1). The rate of SSI in most of the studies was low, except in three trials where infection rates were as high as 14%, 22% and 43% respectively (Fazeli 2006; Kareem 2006; Søndenaa 1992). Four of the 10 studies were at high risk of bias (Gencosmanoglu 2005; Jamal 2009; Kareem 2006; Søndenaa 1992). The rest were at unclear risk and none were graded as of high methodological quality (low risk of bias).
1.1. Analysis.
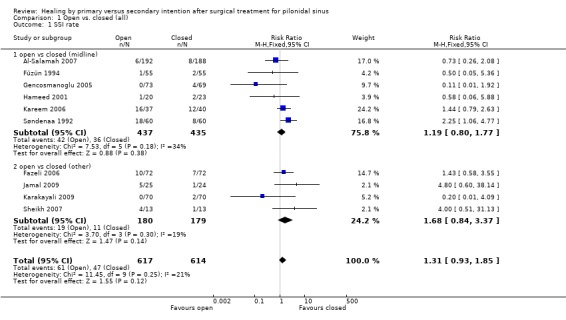
Comparison 1 Open vs. closed (all), Outcome 1 SSI rate.
Six studies (872 participants) compared open healing with midline closure (Al‐Salamah 2007; Füzün 1994; Gencosmanoglu 2005; Kareem 2006; Hameed 2001; Søndenaa 1992). No statistically significant difference was detected between the two treatment options when data were pooled (RR 1.19, 95% CI 0.80 to 1.77, I2 = 34%).
Three studies (59 participants) compared open healing with closed (other) treatment, z‐plasty (Fazeli 2006), Limberg flap (Jamal 2009) and Karydakis technique (Sheikh 2007). There was no significant difference in rate of postoperative SSI (RR 1.68, 95% CI 0.84 to 3.37, I2 = 19%).
Recurrence rate (Analysis 1.2)
Recurrence rate was the most commonly reported outcome with 16 studies comprising 1666 participants reporting recurrence, all of which had high follow up rates (i.e. greater than 80%) (Al‐Salamah 2007; al‐Hassan 1990; Fazeli 2006; Füzün 1994; Gencosmanoglu 2005; Hameed 2001; Jamal 2009; Karakayali 2009; Kareem 2006; Khawaja 1992; Kronborg 1985; Miocinovic 1999; Mohamed 2005; Sheikh 2007; Søndenaa 1992; Testini 2001). All studies but one (Mohamed 2005) followed participants for more than one year. Overall recurrence was uncommon with only 115 out of 1663 affected (6.9%).
Pooling the data from the 16 studies, using a fixed effect model showed that open healing by secondary intention was associated with significantly lower rates of recurrence than closed (all) wounds healing (RR 0.65, 95% CI 0.46 to 0.93, I2 = 17%) (Analysis 1.2). This means that open healing reduces the risk of recurrence by 35% when compared with any closed method. Seven of the studies were at high risk of bias (al‐Hassan 1990; Gencosmanoglu 2005; Jamal 2009; Kareem 2006; Miocinovic 1999; Mohamed 2005; Søndenaa 1992), one was of low risk of bias (Khawaja 1992) and the remainder were unclear with respect to their risk of bias.
1.2. Analysis.
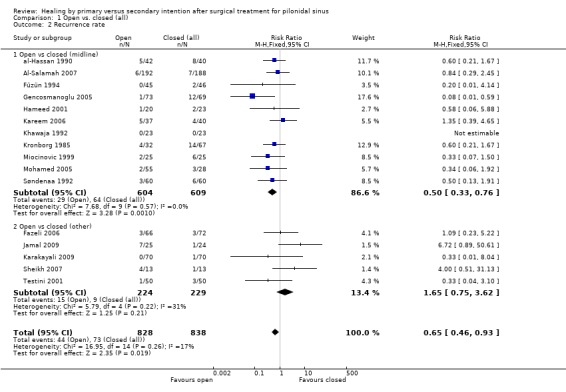
Comparison 1 Open vs. closed (all), Outcome 2 Recurrence rate.
When comparing open healing with midline closure, pooling the data from eleven trials (Mohamed 2005; Gencosmanoglu 2005; al‐Hassan 1990; Kronborg 1985; Hameed 2001; Søndenaa 1992; Füzün 1994; Khawaja 1992; Miocinovic 1999; Kareem 2006; Al‐Salamah 2007) showed a significantly lower recurrence rate after open technique (RR 0.50, 95% CI 0.33 to 0.76, I2 =0%).
There was no statistically significant difference in rates of recurrence between open and off‐midline surgical closure, demonstrated higher rate of recurrence in open surgery, although this difference was not statistically significant (RR 1.65, 95% CI 0.75 to 3.62, I2 = 31%). The off‐midline techniques used were: Karydakis flap (Testini 2001; Sheikh 2007 ); z‐plasty (Fazeli 2006); rhomboid excision and Limberg flap (Jamal 2009; Karakayali 2009).
Secondary outcomes
Time to return to work
Data were not pooled for time to return to work due to the high statistical heterogeneity ( I2 = 96%). Data are presented in Table 7.
Of the 11 studies (1729 participants) (al‐Hassan 1990; Al‐Salamah 2007; Fazeli 2006; Füzün 1994; Karakayali 2009; Kareem 2006; Søndenaa 1992; Sheikh 2007; Testini 2001; Khawaja 1992; Gencosmanoglu 2005 ) reporting time to return to work, 9 studies reported significant faster time to RTW (days mean/median) after primary closure (al‐Hassan 1990; Al‐Salamah 2007; Fazeli 2006; Füzün 1994; Kareem 2006; Søndenaa 1992; Sheikh 2007; Testini 2001; Khawaja 1992). Only two studies (Karakayali 2009; Gencosmanoglu 2005) favoured open wound healing over primary closure. This can be explained by the fact that both studies compared marsupialisation (involves partially opposing skin edges) with surgical closure, whilst the other studies which used open healing made no attempt to partially oppose the skin edges in the open healing wound group.
Time to return to work is a type of time‐to‐event data but has been inappropriately treated as continuous data (see discussion above in relation to time to healing). Of all studies, three were at high risk of bias (al‐Hassan 1990; Kareem 2006; Søndenaa 1992) and none were at low risk of bias.
Other complications and morbidity (Analysis 1.3)
Considering the clinical heterogeneity of this outcome (different complications pooled as one outcome) studies were pooled using a random effects model. Eleven studies (al‐Hassan 1990; Fazeli 2006; Hameed 2001; Gencosmanoglu 2005; Jamal 2009; Karakayali 2009; Kareem 2006; Khawaja 1992; Sheikh 2007; Søndenaa 1992; Testini 2001) reported complications and morbidity, other than recurrence or SSI, as an outcome. Pooling the data of 960 participants showed that no significant difference between open healing and primary surgical closure (all) (RR 0.70, 95% CI 0.34 to 1.46, I2 =50%) (Analysis 1.3). One study was at low risk of bias (Khawaja 1992) and five were at high risk of bias (al‐Hassan 1990; Gencosmanoglu 2005; Jamal 2009; Kareem 2006; Søndenaa 1992).
1.3. Analysis.
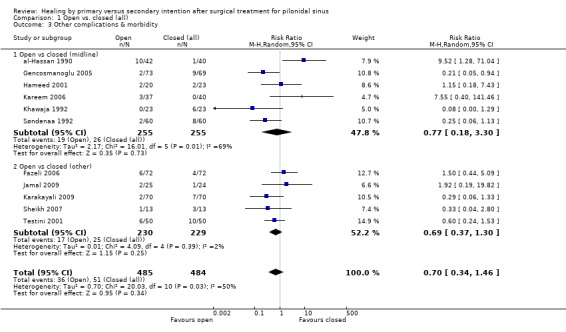
Comparison 1 Open vs. closed (all), Outcome 3 Other complications & morbidity.
Six studies (510 participants) reported complication rate when open healing was compared with midline primary closure. There was no significant difference in the rate of postoperative complications (RR 0.77, 95% CI 0.18 to 3.30, I2=69%). Only 5 studies (459 participants) compared open with closed off‐midline closure (z‐plasty, Karydakis flap, rhomboid excision and Limberg flap); no significant difference was demonstrated (RR 0.69, 95% CI 0.37 to 1.30, I2=2%) (Fazeli 2006; Jamal 2009; Karakayali 2009; Sheikh 2007; Testini 2001).
Participant satisfaction (Analysis 1.4)
One small study (n = 83; 3 arms) (Mohamed 2005) measured participant satisfaction as 'satisfied/not satisfied'. This study compared open healing with midline closure, where two (wide and limited excision) of the three arms were combined. Satisfaction was statistically significantly lower with open healing (RR 0.75, 95% CI 0.57 to 0.99) (Analysis 1.4). However, in the open group where there were two comparison arms, the satisfaction ratings were markedly different with 7/26 (27%) satisfied with wide excision and 27/29 (93%) satisfied with limited excision. The study was at high risk of bias.
1.4. Analysis.
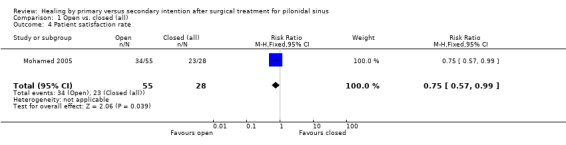
Comparison 1 Open vs. closed (all), Outcome 4 Patient satisfaction rate.
Cost (Analysis 1.5)
One study from Pakistan assessed cost (Hameed 2001). This study compared open healing with midline closure and found the latter to be significantly cheaper (MD 23.94 Rupees, 95% CI 0.73 to 47.15)(Analysis 1.5). After conversion to British Sterling the cost of open healing was £46.21 and closed technique £30.43 per participant. Although this study is unlikely to be generalisable to the developed world, it is the best estimate available from the literature. This study was at unclear risk of bias.
1.5. Analysis.
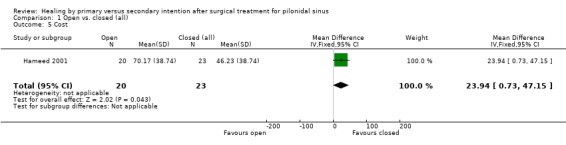
Comparison 1 Open vs. closed (all), Outcome 5 Cost.
Length of stay
Data were not pooled for length of hospital stay due to the high statistical heterogeneity ( I2 = 96%). Data are presented in Table 8.
LOS was recorded by 10 studies (1225 participants) (al‐Hassan 1990; Al‐Salamah 2007; Fazeli 2006; Füzün 1994; Jamal 2009; Karakayali 2009; Kareem 2006; Khawaja 1992; Mohamed 2005; Testini 2001), of which six used midline closure (al‐Hassan 1990; Al‐Salamah 2007; Füzün 1994; Kareem 2006; Mohamed 2005; ). Three of the 10 studies reported significantly longer hospital stay (mean/median) after open healing (Jamal 2009; Kareem 2006; Al‐Salamah 2007). However, four studies reported significantly longer hospital length of stay after closed healing (Füzün 1994Mohamed 2005Fazeli 2006; Karakayali 2009); the remainder of studies were unequivocal.
A possible explanation of the high heterogeneity is the variability in discharge criteria. Some discharge protocols were dependent on participant choice, others discharged participants when no postoperative complications occurred. Another explanation is that Testini 2001 carried out surgery as day cases whereas other studies admitted people as inpatients. Apart from Khawaja 1992 which was at low risk of bias, all studies were at unclear risk of bias, except four (al‐Hassan 1990; Jamal 2009; Kareem 2006; Mohamed 2005) which were at high risk of bias.
Pain (Analysis 1.6)
Postoperative pain was reported by six studies (Jamal 2009; Karakayali 2009; Kareem 2006; Rao 2001; Søndenaa 1992; Testini 2001). Rao 2001 found that the postoperative pain score on day 4 was significantly lower after midline closure than open healing (median VAS 10 (range 0‐73) vs. VAS score 35 (range 0‐63); P < 0.05) (Table 9).
The rate of pain was assessed by two studies (n=220) (Søndenaa 1992; Testini 2001). Pooling their data revealed no statistically significant difference (RR 1.13, 95% CI 0.45 to 2.80, I2=0%) (Analysis 1.6). Testini 2001 compared open healing with Karydakis technique and found similar rates of pain (6% and 4% respectively). Søndenaa 1992 compared open healing with midline closure and reported identical pain rates of 10%.
1.6. Analysis.
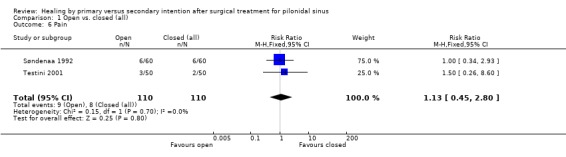
Comparison 1 Open vs. closed (all), Outcome 6 Pain.
Kareem 2006 found no statistically significant difference in the rate of severe pain between midline closure and open healing, although severe pain was more common in surgical closure than those with wounds that were left to heal openly: 3 (7.5%) vs. 2 (5.4%) participants.
Jamal 2009 used VRS to assess postoperative pain after comparing open wound healing with closed off‐midline (Limberg flap) and reported statistically significantly lower rates of severe pain after using the off‐midline technique. In the open healing group, 18/21 participants reported severe pain (score > 7/10), compared with 9/24 (38%) participants in the off‐midline group.
Karakayali 2009 used VAS and the McGill Pain Questionnaire (MPQ) subscales at 1 week and three months post operatively (Table 10). At one week, VAS scores were significantly higher (higher score = lower pain levels) for open technique (unroofing and marsupialisation) than for closed off‐midline (rhomboid excision and Limberg flap) but at 3 months, this difference was not statistically significant. Scores for the MPQ indicated significantly lower pain levels after open wound healing at 1 week but again, this difference was not statistically significant at 3 months.
Quality of life
Only one study reported QoL (Karakayali 2009) using the CWIS to compare pre and 3 month postoperative QoL in participants with open wound healing (unroofing and marsupialisation) to off‐midline closure (rhomboid excision and Limberg flap) (Table 12). Scores were similar for all major domains before surgery and significantly higher after off‐midline closure at 3 months postoperatively.
Rate of change of wound volume
No studies reported this outcome.
Wound healing rate (Analysis 1.7)
Five studies (474 participants) (al‐Hassan 1990; Kronborg 1985; Rao 2001; Søndenaa 1992; Testini 2001) reported wound healing rates after open healing compared with closed procedures. Data were pooled using a random effects model and there was no significant difference in the wound healing rate between the two methods (RR 0.94, 95% CI 0.85 to 1.04, I2 =79%) (Analysis 1.7). Two studies were at high risk of bias (al‐Hassan 1990Søndenaa 1992) and the rest were at unclear risk of bias.
1.7. Analysis.
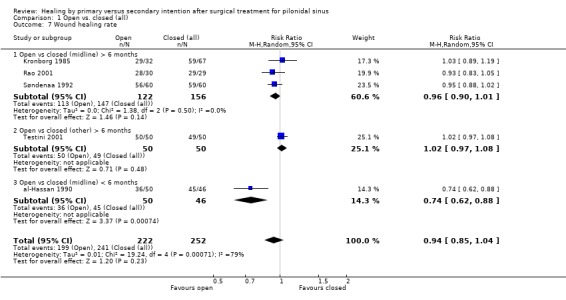
Comparison 1 Open vs. closed (all), Outcome 7 Wound healing rate.
Three studies (Kronborg 1985; Rao 2001; Søndenaa 1992) compared open healing with midline closure (time of the assessment more than 6 months) and found no difference in the wound healing rate (RR 0.96, 95% CI 0.90 to 1.01, I2 =0%). al‐Hassan 1990 assessed participants within six months and found that 98% of closed wounds had healed compared with only 72% of open wounds, this difference was statistically significant (RR 0.74, 95% CI 0.62 to 0.88).
The high heterogeneity between pooled data could be due to differences in the characteristics of participants at recruitment (e.g. presentation status) or difference in timing of participant follow‐up. Performing a sensitivity analysis showed that the high heterogeneity (I2 = 79%) was markedly reduced when only data from studies that assessed wound healing beyond 6 months were pooled. When data from al‐Hassan 1990 were omitted, the I2 reduced to 19% although this did not change the magnitude of the effect (RR 0.99, 95% CI 0.94 to 1.03).
Operative time
Data were not pooled for operative time due to the high statistical heterogeneity ( I2 = 94%). Data are presented in Table 13.
8. Operative time (minutes).
| Study name | Comparison | Experimental group | Control group | SS_E | SS_C | P value | Results format |
| Al‐Salamah 2007 | Open vs closed (midline) | 43 (5.1) | 58 (4.5) | 192 | 188 | <0.0001 | Mean (SD) |
| Kareem 2006 | Open vs closed (midline) | 14.77 (3.42) | 23.38 (5.18) | 20 | 23 | <0.0001 | Mean (SD) |
| Hameed 2001 | Open vs closed (midline) | 27 (nr) | 49 (nr) | 37 | 40 | <0.05 | Mean |
| Mohamed 2005 | Open vs closed (midline) | 54.8 (3.66) | 63 (4.6) | 55 | 28 | nr | Mean (SD) |
| Jamal 2009 | Open vs closed (off‐midline) | 35 (nr) | 60 (nr) | 25 | 24 | <0.004 | Mean |
| Karakayali 2009 | Open vs closed (off‐midline) | 53.1 (20.4) | 89.3 (31.0) | 70 | 70 | <0.001 | Mean (SD) |
| Sheikh 2007 | Open vs closed (off‐midline) | 25 (5) | 45 (10) | 13 | 13 | nr | Mean (SD) |
Seven studies (798 participants) (Al‐Salamah 2007; Hameed 2001; Jamal 2009; Karakayali 2009; Kareem 2006; Mohamed 2005; Sheikh 2007) compared the operative time between open healing and primary closure. All studies reported open healing to be quicker procedure than primary closure. Three studies were at high risk of bias (Mohamed 2005; Jamal 2009; Kareem 2006) and the rest were at unclear risk of bias.
One possible reason for the high levels of heterogeneity (I2 =94%) could be due to variation in the anaesthetic procedures used, e.g. three studies used general anaesthesia (Al‐Salamah 2007; Hameed 2001; Kareem 2006), one used general or spinal anaesthesia (Jamal 2009), one study used spinal anaesthesia only (Karakayali 2009), and one did not specify type of anaesthesia (Mohamed 2005).
Comparison of closed techniques with other closed surgical techniques for pilonidal sinus
Of the 26 studies included in the review, nine studies compared different types of surgical closure; six compared midline closure with off‐midline (Abu Galala 1999; Akca 2005; Berkem 2005; Ertan 2005; Sakr 2006; Wright 2001) and three compared closed off‐midline with another type of closed off‐midline surgery (Cihan 2006; Ersoy 2009; Nordon 2009).
Comparison of closed midline with closed off‐midline (Analysis 2)
Primary outcome
Time to wound healing (Analysis 2.1)
One Turkish study (Ertan 2005) compared time to wound healing after midline or rhomboid flap closure in 100 participants (closed other/off‐midline). Sutured midline wounds took significantly longer to heal compared with sutured off‐midline wounds (MD 5.4 days, 95% CI 2.3 to 8.5 days). Data are reported in Table 6 and Analysis 2.1. This study was at unclear risk of bias. All study participants were reported as achieving complete healing.
2.1. Analysis.
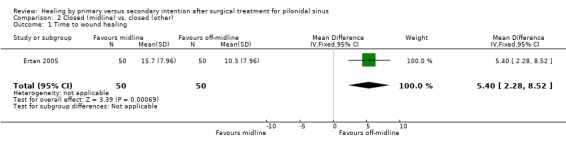
Comparison 2 Closed (midline) vs. closed (other), Outcome 1 Time to wound healing.
Rate of surgical site infection (SSI) (Analysis 2.2)
Five studies (541 participants) assessed postoperative rate of SSI (Abu Galala 1999; Akca 2005; Berkem 2005; Ertan 2005; Sakr 2006). Infection rates varied across the studies from 0% (Berkem 2005) to 20% (Ertan 2005). Pooling the trials using a fixed effect model showed rates of infection were statistically significantly higher after midline closure surgery (RR 3.72, 95% CI 1.86 to 7.42, I2 = 0%) (Analysis 2.2). One study was at low risk of bias (Akca 2005), and two were at high risk of bias (Abu Galala 1999; Sakr 2006).
2.2. Analysis.
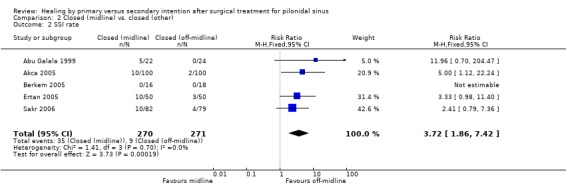
Comparison 2 Closed (midline) vs. closed (other), Outcome 2 SSI rate.
Recurrence rate (Analysis 2.3)
Six studies assessed recurrence rate of pilonidal sinus, providing data on 35 events in 574 participants (6.1%) (Abu Galala 1999; Akca 2005; Berkem 2005; Ertan 2005; Sakr 2006; Wright 2001). Results in the forest plot are grouped by length of follow‐up. A Peto OR was used to calculate the effect estimate due to a low event rate and specifically a high frequency of zero events in series. Pooled estimate showed the recurrence rate was significantly higher after midline closure than off‐midline (Peto OR 4.54, 95% CI 2.30 to 8.96, I2 = 33%) (Analysis 2.3). One study was at low risk of bias (Akca 2005), two were at high risk of bias (Abu Galala 1999; Sakr 2006) and the rest were at unclear risk of bias.
2.3. Analysis.
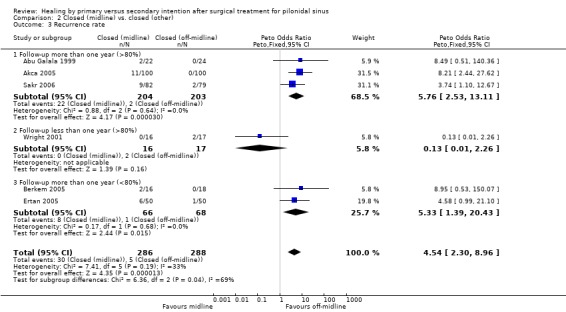
Comparison 2 Closed (midline) vs. closed (other), Outcome 3 Recurrence rate.
Of the six studies, one followed‐up participants for less than a year (Wright 2001) and found no statistically significant difference between the two techniques.
Secondary outcome
Time to return to work (Analysis 2.4)
Four studies reported time taken to RTW (Abu Galala 1999; Akca 2005; Ertan 2005; Sakr 2006). Two studies reported mean time to RTW (days) (Abu Galala 1999; Ertan 2005), one reported median (days) (Akca 2005), and one only reported the range in weeks (Sakr 2006). Due to the high heterogeneity between the two studies reporting mean values (Abu Galala 1999; Ertan 2005) (I2 = 95.6%) the data were not pooled (Table 7) (Analysis 2.4). Time to return to work is a type of time‐to‐event data and appears to have been inappropriately analysed as continuous data; these data should therefore be viewed with caution.
2.4. Analysis.
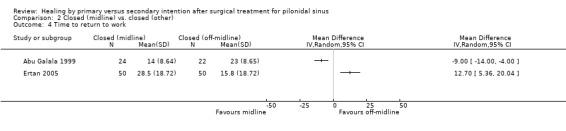
Comparison 2 Closed (midline) vs. closed (other), Outcome 4 Time to return to work.
The study by Abu Galala 1999 found that time to RTW took significantly longer after midline closure compared to off‐midline (mean 23 days vs. 14 days respectively). Ertan 2005 reported an opposing conclusion, whereby midline closure was associated with quicker return to work than off‐midline (mean 15.8 vs 28.5 days).
One Turkish study (Akca 2005) reported a significant longer period to RTW after midline closure when compared to off‐midline (rhomboid excision and Limberg flap) (median 19 vs. 9.5 days, respectively). However, an Egyptian study (Sakr 2006), which compared midline closure to off‐midline (Karydakis technique) found no difference between the two techniques (range of 3 to 4 weeks for both).
One study was at low risk of bias (Akca 2005) and two were at high risk of bias (Abu Galala 1999; Sakr 2006).
Other complications and morbidity (Analysis 2.5)
Three studies reported postoperative complications, other than SSI, in 461 participants (Akca 2005; Ertan 2005; Sakr 2006). Pooling using a random effects model (considering the nature of the outcome) showed there was a clear benefit demonstrated in off‐midline wounds compared with midline wounds (RR 4.42, 95% CI 1.51 to 12.99, I2 =15%) (Analysis 2.5). The study by Akca 2005 was at low risk of bias; the study by Ertan 2005 was at unclear risk of bias; and the study by Sakr 2006 was at high risk of bias.
2.5. Analysis.
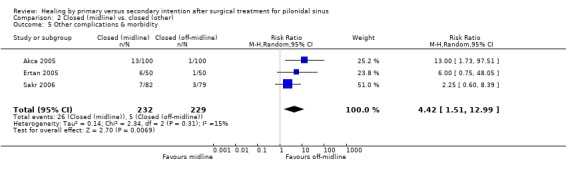
Comparison 2 Closed (midline) vs. closed (other), Outcome 5 Other complications & morbidity.
Participant satisfaction (Analysis 2.6)
A small but statistically significant preference was demonstrated for off‐midline closure compared with midline primary closure where satisfaction was measured using a 0‐10 VAS (Ertan 2005; 200 participants). However, a mean difference of 1 point on a VAS is unlikely to be translated into a meaningful clinical difference (off‐midline score = 7.4 (SD 1.4) vs. midline satisfaction score = 6.5 (SD 1.7); p<0.004) (Analysis 2.6).
2.6. Analysis.
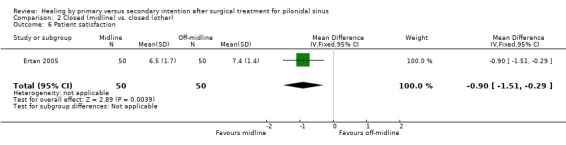
Comparison 2 Closed (midline) vs. closed (other), Outcome 6 Patient satisfaction.
Cost
No studies reported cost data.
Length of stay
Four studies reported length of hospital stay (341 participants) (Abu Galala 1999; Berkem 2005; Ertan 2005; Sakr 2006), Data were not pooled for LOS due to the high statistical heterogeneity ( I2 = 94%). Data are presented in Table 13. Hospital length of stay was significantly longer after midline closure compared with off‐midline closure in two studies (Abu Galala 1999; Ertan 2005); Two of the four studies were at high risk of bias (Abu Galala 1999; Sakr 2006).
A possible explanation for the high heterogeneity is the variation in discharge criteria, with one study (Abu Galala 1999) discharging participants when they were deemed "fit" for discharge, one discharging participants after drain removal (Sakr 2006) and the third study did not specify discharge criteria (Ertan 2005).
Pain (Analysis 2.7)
Pain was measured in two studies which compared midline and off‐midline closure (Ertan 2005; Wright 2001). Mean pain scores were estimable for the Turkish study (Ertan 2005) although no variance were reported for the UK trial which assessed the Bascom flap method (Wright 2001). Ertan 2005 showed significantly higher mean pain scores, measured using the SF‐36, after off‐midline closure (MD ‐13.00, 95% CI ‐19.41 to ‐6.59) (Analysis 2.7).
2.7. Analysis.
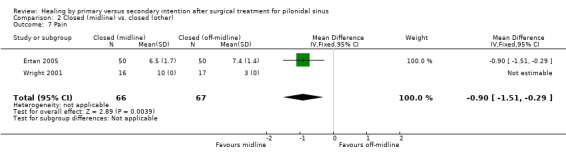
Comparison 2 Closed (midline) vs. closed (other), Outcome 7 Pain.
Quality of life
Although SF‐36 summary scores for overall QoL were not reported by Ertan 2005, the scores for each of the eight domains are presented in Table 11. Participants having the off‐midline Limberg flap had better scores for general health and social functioning although had more pain, less energy and vitality at one year after surgery.
Rate of change of wound volume
No studies reported this outcome.
Wound healing rate (Analysis 2.8)
Two studies compared wound healing rate beyond 6 months after midline and off‐midline closure (Abu Galala 1999; Sakr 2006). The first study Abu Galala 1999) found a significantly higher healing rate after off‐midline closure (RR 0.78; 95% CI 0.61 to 0.98) (Analysis 2.8). This study was at high risk of bias. The other study from Egypt (Sakr 2006) compared midline closure with off‐midline closure (Karydakis technique) and found that participants in both groups had healed by the 21st postoperative day; however, this study was at high risk of bias.
2.8. Analysis.
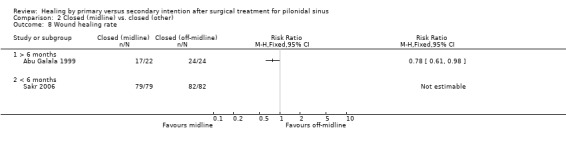
Comparison 2 Closed (midline) vs. closed (other), Outcome 8 Wound healing rate.
Operative time (Analysis 2.9)
Two studies (207 participants) reported mean operative time (Abu Galala 1999; Sakr 2006) however Abu Galala 1999 did not provide variance values so a meta‐analysis was not performed. The study by Sakr 2006 found that participants having off‐midline closure (Karydakis technique) had a longer operative time compared with those having midline closure (mean 45.2 vs. 40.1 minutes respectively). This finding was not statistically significant (Analysis 2.9).
2.9. Analysis.
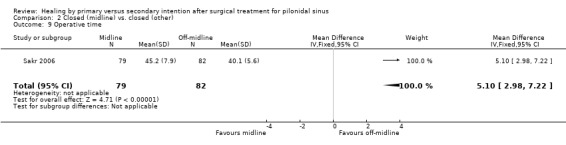
Comparison 2 Closed (midline) vs. closed (other), Outcome 9 Operative time.
Abu Galala 1999 found no difference in operative time between midline and off‐midline closure (Rhomboid flap), with the mean for both procedures reported as 55 minutes. Both studies (Abu Galala 1999; Sakr 2006) were at high risk of bias.
Comparison of closed other (classic rhomboid flap) with another type of closed other (modified rhomboid flap) for pilonidal sinus (Analysis 3)
Primary outcomes
Time to wound healing
Not reported.
Rate of surgical site infection (SSI) (Analysis 3.1)
A Turkish study (Cihan 2006) (68 participants) reported a lower SSI rate after asymmetrical modified Limberg (rhomboid) flap (3%) compared to classical Limberg (rhomboid) flap (23%) although this was not statistically significant (Analysis 3.1). This study was at high risk of bias.
3.1. Analysis.
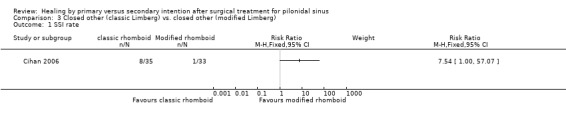
Comparison 3 Closed other (classic Limberg) vs. closed other (modified Limberg), Outcome 1 SSI rate.
Recurrence rate (Analysis 3.2)
The Turkish study (Cihan 2006) identified two participants with recurrence in the classical Limberg group (Peto OR 7.19. 95% CI 0.44 to 117.48) (Analysis 3.2).
3.2. Analysis.
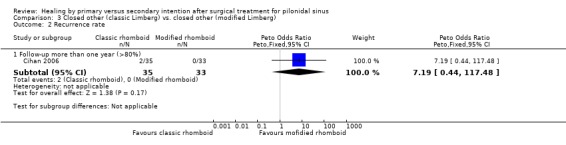
Comparison 3 Closed other (classic Limberg) vs. closed other (modified Limberg), Outcome 2 Recurrence rate.
Secondary outcomes
Time to return to work (Analysis 3.3)
Time off from work was subjectively defined by each patient as the period that lasted until the patient started to feel comfortable in carrying out his or her daily activities without further care. Cihan 2006 found a significant difference of two days in RTW between the two methods, favouring the modified Limberg flap (mean 9.3 days vs 11.4 days) (Analysis 3.3).
3.3. Analysis.
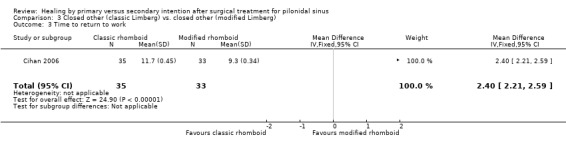
Comparison 3 Closed other (classic Limberg) vs. closed other (modified Limberg), Outcome 3 Time to return to work.
Other complications and morbidity (Analysis 3.4)
Cihan 2006 reported significantly higher postoperative complication rate after classical Limberg flap: authors reported that there were 16 participants with maceration and 8 with wound dehiscence although it is unclear whether some had both events (24/35; 69%). The event rate in participants having modified Limberg flap was (3/33, 10%) (Analysis 3.4).
3.4. Analysis.
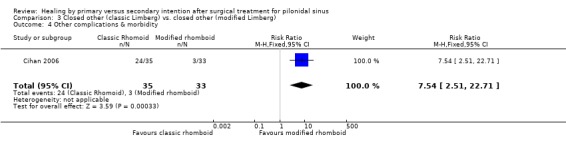
Comparison 3 Closed other (classic Limberg) vs. closed other (modified Limberg), Outcome 4 Other complications & morbidity.
Length of hospital stay (Analysis 3.5)
Cihan 2006 reported a significantly longer LOS after classical Limberg flap compared to modified Limberg flap (5.71 vs 3.61 days; P<0.01) (Table 8) (Analysis 3.5).
3.5. Analysis.
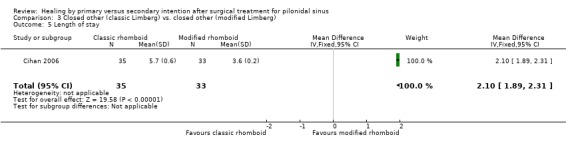
Comparison 3 Closed other (classic Limberg) vs. closed other (modified Limberg), Outcome 5 Length of stay.
The following secondary outcomes were not reported for this comparison:
Participant satisfaction, cost, pain, QoL, wound healing rate and operative time.
Comparison of closed other (classic rhomboid flap) with closed other (Karydakis technique) for pilonidal sinus (Analysis 4)
Primary outcomes
Time to wound healing
Not reported.
Rate of surgical site infection (SSI) (Analysis 4.1)
The Turkish study by Ersoy 2009 reported significantly higher infection rate after Karydakis technique (26%) compared with classical rhomboid flap (8%) (RR 3.25, 95%CI 1.14 to 9.29 Analysis 4.1). The study was at unclear risk of bias.
4.1. Analysis.
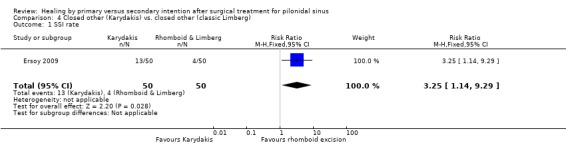
Comparison 4 Closed other (Karydakis) vs. closed other (classic Limberg), Outcome 1 SSI rate.
Recurrence rate
Not reported.
Secondary outcomes
Time to return to work
Ersoy 2009 found that it took slightly longer to RTW after Karydakis technique compared with classical rhomboid flap (median of 15 vs. 14 days). This was not statistically significant.
Pain
Ersoy 2009 reported that the median VAS pain score for participants treated with Karydakis technique was similar to the classical rhomboid flap group (median score 4 points in both groups).
The following secondary outcomes were not reported for this comparison:
Other complications and morbidity, participant satisfaction, cost, LOS, QoL, wound healing rate, and operative time.
Comparison of closed other (Simple Bascom) with closed other (Bascom Cleft Closure) for pilonidal sinus (Analysis 5)
Primary outcomes
The following primary outcomes were not reported for this comparison:
Time to wound healing and SSI rate.
Recurrence rate (Analysis 5.1)
The British study by Nordon 2009 reported a higher recurrence rate after simple Bascom compared with Bascom cleft closure technique (2 vs. 0 events) although no statistical tests were reported (Analysis 5.1). The study was at unclear risk of bias.
5.1. Analysis.
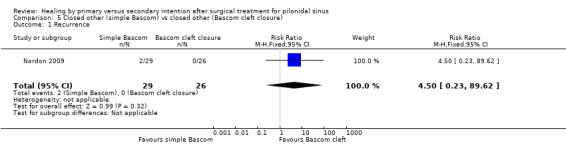
Comparison 5 Closed other (simple Bascom) vs closed other (Bascom cleft closure), Outcome 1 Recurrence.
Secondary outcomes
Time to return to work
Nordon 2009 reported similar median number of weeks to RTW after both surgical techniques (median of 2 weeks).
Wound healing rate (Analysis 5.2)
Nordon 2009 found that all the participants having Bascom cleft closure healed within 6 months compared with only 62% of participants in the simple Bascom group; no statistical tests were reported (Analysis 5.2). However, five participants in the simple Bascom group had failed to heal when assessed at median follow‐up of 36 months.
5.2. Analysis.
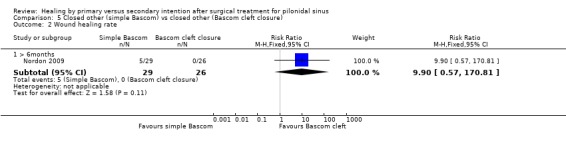
Comparison 5 Closed other (simple Bascom) vs closed other (Bascom cleft closure), Outcome 2 Wound healing rate.
The following secondary outcomes were not reported for this comparison:
Other complications and morbidity, participant satisfaction, cost, LOS, pain, QoL, and operative time.
Discussion
Summary of main results
Time to wound healing
It perhaps unsurprising that open surgical wounds that are left to granulate take longer to heal than surgically closed wounds. Interestingly, wounds closed on the midline of the natal cleft took longer to heal compared with wounds closed off‐midline, although this finding was based on a single study with 100 participants (Ertan 2005) having rhomboid excision or Limberg flap (off‐midline techniques). A more accurate approach to analysing time to wound healing would be to use survival analysis (e.g. Kaplan‐Meier) to account for each individual event out of the population at risk of developing the outcome over time. However most trialists appear not to have used this approach and this could not be corrected at the review stage since we did not have patient level data. Furthermore, high levels of heterogeneity led us to use a narrative rather than statistical approach to synthesise the evidence around this outcome. However even on a study by study basis, the inability of this approach to include unhealed patients may lead to biased estimates.
Surgical site infection
There were no statistically significant differences in infection rates between open wound healing and primary wound closure, regardless of suture line position. This is contrary to the general surgical consensus that open healing is more likely to result in fewer postoperative infections. However, when midline closure was compared with off‐midline, a statistically significant difference was found in favour of off‐midline closure. The superiority of the off‐midline technique was supported in a review by Petersen 2002. This narrative review included experimental and observational studies; Petersen 2002 reported an overall infection rate of 12.4% after midline closure and a range between 3.6 to 9.3% after off‐midline closure (depending on the type of off‐midline closure: asymmetric/oblique techniques, rhomboid flaps, VY‐advancement flaps, or z‐plasty). Our systematic review found similar results for midline wound closure when SSI rates were aggregated, giving a pooled rate of 13% (35/270). The similarity continued when SSI was investigated for off‐midline closure, with the pooled SSI rate being 3.3% in this review, which is similar to the lowest estimate reported by Petersen 2002.
Recurrence
Recurrence of pilonidal sinus was the most commonly reported outcome by all the included studies. Overall, this was a relatively rare outcome with only 7.0% (117/1666) of events occurring across all studies, with 5.3% (44/828) occurring after open healing compared to 8.7% (73/838) after closed (all) techniques.
Open healing was associated with a significantly lower recurrence rate than primary surgical closure (all techniques), with open technique reducing the risk of recurrence by 35% when compared with closed technique. The overall recurrence rate for all studies comparing midline with off‐midline closures was 6.1% (35/574). When these procedures were compared, off‐midline procedures were found to be associated with significantly fewer recurrences (10.5% vs. 1.7%). Petersen 2002 had similar findings, as they reported a higher recurrence rate with midline closure in comparison to off‐midline (9.4% compared with 1.5 to 2.4% depending on the type of the off‐midline closure). In our systematic review, one study compared recurrence following classic rhomboid flap (off‐midline technique) to modified rhomboid flap (another type of off‐midline technique). The study found that the former procedure resulted in more recurrences (Peto OR 7.19, 95% CI 0.44 to 117.48). However, meaningful interpretation of these data is difficult considering the very wide confidence interval.
Return to work
Pilonidal sinus disease is more common among young adults which means that the longer the convalescence period postoperatively, the less economically productive this group is. This makes the RTW outcome a very important factor in determining the optimal surgical procedure. In this review, a significant clinical advantage was found with primary wound closure (all) over open healing when RTW was investigated. This advantage was replicated when open healing was compared with midline closure and off‐midline independently, although this was not statistically significant for the latter comparison. Only two of nine studies (Gencosmanoglu 2005; Karakayali 2009) that compared open healing with closed techniques reported results that favoured open healing. This could be because only these two studies used marsupialisation, which opposes the edges of wounds resulting in smaller wounds, potentially promoting wound healing. The recent review by Lee 2008, also recommended marsupialisation as the initial primary surgery for patient with new pilonidal sinus disease. A more accurate approach to analysing time to return to work would be to use survival analysis and the inability to include unhealed patients in this analysis may lead to biased estimates.
Other complications and morbidity
No significant differences were found when open healing was compared with midline or off‐midline closure in relation to other postoperative complications. However, there was a statistically significant difference between midline and off‐midline closure, with the latter being associated with fewer complications and morbidity. This finding, in conjunction with lower SSI rates, lower recurrence rate and quicker wound healing time strongly suggest that off‐midline surgical closure is superior to midline closure.
Participant satisfaction
One study compared participant satisfaction after open healing with closed midline technique and found a statistically significant difference in favour of midline closure, although this finding should interpreted with caution as the study was at high risk of bias. When off‐midline closure was compared with midline, a statistically significant, although clinically non‐significant, difference was found in favour of off‐midline closure. This outcome was neglected by most pilonidal sinus studies, which warrants encouraging future trials to include patient preference and satisfaction with treatment.
Cost
Despite the potential economical impact of pilonidal sinus disease, there were no fully costed economic evaluation studies investigating either direct or indirect financial consequences. Only one study from Pakistan made an attempt to evaluate cost, although many could argue that the results are not generalisable to other health care settings (Hameed 2001). The study calculated costs associated with the operation, bed charges, dressings and income loss and found that primary midline closure was less costly than open healing. This is another outcome which is important to investigate in future studies.
Length of hospital stay
Due to the high level of heterogeneity, a pooled estimate was not calculated. The data from studies were variable and there were no consistent patterns observed. This was unexpected considering the common assumption that open wound healing requires more specialist wound care and is associated with longer time to return to usual activities. One possible explanation for the high heterogeneity could be due to variation in discharge criteria (complications dependent and/or participant preference) and/or the type of setting (inpatients or day case procedures).
Pain
There was little evidence of any difference between open healing and closed (all) techniques in terms of postoperative pain. In one study by Karakayali 2009, pain levels were significantly lower after open healing compared with closed (off‐midline) surgery at 1 week, however this difference diminished at 3 months. When midline closure was compared with off‐midline, higher pain scores were associated with the midline technique. This could be explained by the reduced tension that wound edges are put under when the suture line lies off‐midline. Of the 9 studies that assessed postoperative pain, five studies used a validated pain assessment tool (Akca 2005; Ersoy 2009; Ertan 2005; Jamal 2009; Karakayali 2009) such as VAS, MPQ, or pain domain within the SF‐36. Of all studies, only one study specified the timing of the postoperative pain assessment (Karakayali 2009), conducted at 1 week and 3 months. The lack of data regarding the time of assessment by the majority of studies makes difficult to differentiate whether pain reported was acute or chronic (>3 months).
Quality of life
Health‐related QoL was under‐reported, with only 2 of 26 studies assessing postoperative QoL. One study (Karakayali 2009) showed that off‐midline closure (rhomboid excision and Limberg flap) was associated with better postoperative quality of life compared with open healing. Another study (Ertan 2005) compared the same off‐midline technique (rhomboid excision and Limberg flap) with midline closure. It reported that participants had less pain, more energy and better mental health when they were managed with midline closure, although they had worse general health and social functioning.
Wound healing rate
There were no evidence of any difference between open healing and primary closure when wound healing rate was investigated beyond 6 months. Using the finding of only one study (al‐Hassan 1990), which was at high risk of bias, there was a significant difference between open wound healing compared with off‐midline closure within 6 months of follow‐up; this was in favour of off‐midline closure (RR 0.74, 95% CI 0.62, 0.88). Two studies compared midline with off‐midline closure, both at high risk of bias: one examined healing rate beyond 6 months (Abu Galala 1999), and favoured off‐midline closure; the other examined healing rate within 6 months and found no difference between the two treatments (Sakr 2006).
Operative time
Operative time was significantly shorter after an open approach compared with closed surgery. This significant difference was more marked when open healing was compared with closed off‐midline technique than when open healing was compared with closed midline technique. This could be due to the fact that off‐midline techniques are more technically challenging than the midline closure techniques. Therefore, operative time could potentially be reduced by increasing surgical experience. However, none of the studies provided data about surgeon experience, thus investigating the validity of this theory remains to be seen in future studies.
Overall completeness and applicability of evidence
A formal sensitivity analysis was not performed across all outcomes (e.g. by methodological quality). The review only included studies that recruited participants with new onset or recurrent pilonidal sinus disease and rejected those with an abscess at presentation. No attempt was made to conduct a sensitivity analysis for this clinical variable or for severity of disease because studies were often unclear in reporting data on clinical subgroups. In surgical RCTs, blinding of participants, surgeons and outcome assessors can be difficult, and in many circumstances impossible. Hence the findings from this surgical review should be interpreted with caution, as bias may exist from the lack of blinding.
Quality of the evidence
Only two studies were graded as low risk of bias, having satisfied all five domains in the risk of bias assessment. The high proportion of studies graded as high or unclear risk of bias raises some doubt and uncertainty about the results produced. Of the 26 studies, five studies used an adequate sequence generation method and only three used an appropriate allocation concealment method. Reporting of attrition, exclusions and missing data was generally poor, with only five studies appropriately reporting these factors. Failure to address or report the main risk of bias criteria contributes to the potential uncertainty of the results generated by this review. Empirical studies investigating the impact of failure to address the three main risk of bias criteria (sequence generation, allocation concealment and reporting of incomplete data) have varied in their findings and failed to demonstrate consistent results (Als‐Nielsen 2004; Pildal 2007; Schultz 1995; Wood 2008). However, studies published pre‐CONSORT (Moher 2001) were less likely to have provided explicit details on study methodology or considered factors that may increase risk of bias.
Potential biases in the review process
Surgical techniques were grouped into open healing and primary surgical closure and closed techniques were grouped into midline and off‐midline closure. Within each group there were variations in the surgical techniques used: for example, the amount of tissue excised; depth of incision; type of suture material and suturing technique used. This is one of the known flaws when attempting to aggregate data in any meta‐analysis. Nonetheless, a compromise like this is necessary to produce meaningful comparisons.
Care was taken to distribute similar surgical techniques into the appropriate groups. However, there were still variations in the techniques included in each group, therefore inference about the superiority of specific techniques within each group is not appropriate using these data. This means that the conclusions presented here are based on broad group superiority (open healing vs closed midline vs closed off‐midline) rather than a particular surgical technique (Bascom, Karydakis, or Limberg flaps). A narrative approach was taken when analysing studies that investigated a particular off‐midline technique with another off‐midline technique, as grouping these different surgical techniques seemed methodologically and clinically inappropriate.
A potential way to reduce bias is to blind outcome assessors when assessing objective outcome measures, for example, RTW, pain, satisfaction, self‐reported quality of life and cost. Of all the studies included in this review, only one study (Karakayali 2009) reported that outcome assessors were blinded for two surgical outcomes: postoperative pain and QoL. Furthermore, many studies failed to appropriately define surgical outcomes and studies used different methods to assess similar outcomes, some of which seemed not to be the most appropriate or valid method e.g. telephone interviewing or postal questionnaires to assess sinus recurrence. Future studies should define outcomes consistently and use standard assessment tools.
Formal assessment for publication bias (e.g. using funnel plots) was not performed. Twenty‐four studies were original reports of primary outcomes, two were was published as conference abstracts only and one group reported recurrence data at four years post‐operatively in a second update publication. No language restrictions were applied to the search strategy.
Agreements and disagreements with other studies or reviews
A follow‐up of at least 3 to 5 years has been suggested to produce valid conclusions about the incidence of recurrent pilonidal sinus disease (Aldean 2005; Allen‐Marsh 1990; Doll 2007). Therefore, assessing recurrence in a study population within one year of surgery may not represent the true population recurrence rate. In our analysis, only one study (Wright 2001) assessed recurrence within a year of surgery. This could have potentially led to a misleading conclusion. However, in a sensitivity analysis where the study data for Wright 2001 were removed, this did not significantly change the direction or magnitude of the overall effect size. Another point worth considering is that the low recurrence rate found in this systematic review may represent an underestimate of the true recurrence. Firstly, most of the studies had a mean follow up of less than 3 years which is shorter than the recommended follow up for pilonidal sinus surgery. Secondly, some studies used postal questionnaires or telephone interviewing to follow up participants, either as the only assessment method or in an attempt to follow up those who failed to attend outpatient clinics. So there is a possibility that participants with macroscopic asymptomatic recurrence disease were not detected.
Authors' conclusions
Implications for practice.
This review is a systematic review of the surgical treatment options available for pilonidal sinus disease. It found clear benefits associated with the off‐midline surgical closure over the midline closure technique, in a study at medium risk of bias. This is supported by the fact that most surgical outcomes showed a significant difference (or at the least a difference) in favour of off‐midline surgical closure. Based on current evidence, where surgical closure technique is favoured over open healing, an off‐midline technique should be the standard surgical option.
The evidence around surgical closure compared with open healing is less clear. Whilst surgically closed sinuses appear to heal more quickly they are more likely to recur. Furthermore most of the studies which reported time to healing analysed it inappropriately and th impact of this is unclear.Thus choosing between the two treatment options should be based on patient and surgeon preferences. Ideally, surgeons should explain both techniques during the preoperative consultation and inform participants about the advantages and disadvantages of each approach and discuss the desired goals of therapy. As with any surgical technique, surgeon experience and confidence in performing the technique should be part of the decision equation.
Implications for research.
The lack of full economic evaluations of surgical techniques in pilonidal sinus surgery is very surprising, considering that the disease is a common condition that affects young adults. Future should incorporate economic analysis so that healthcare providers can make informed decisions about which technique is more efficient, effective and cost‐effective.
Future trials of pilonidal sinus surgery should be adequately powered, possibly using multiple centres for recruitment and should incorporate valid methods to assess surgical outcomes. The primary outcomes for inclusion in future studies include time to wound healing analysed by survival methods, as well as SSI rate and sinus recurrence. Future trials should be conducted in accordance with nominated trial centres of excellence and adhere to standards recommended in the CONSORT guidelines. Long‐term follow‐up with detailed clinical assessment should be conducted to detect the true rate of recurrence.
What's new
| Date | Event | Description |
|---|---|---|
| 8 December 2010 | Amended | Contact details updated. |
History
Protocol first published: Issue 4, 2006 Review first published: Issue 4, 2007
| Date | Event | Description |
|---|---|---|
| 15 June 2010 | Amended | Contact details updated. |
| 22 October 2009 | New search has been performed | The review has been updated, a new search undertaken and an additional 8 studies have been included. Although the overall conclusions of the review have not changed, the aggregated values for most outcomes have changed. |
| 22 October 2009 | New citation required but conclusions have not changed | A new author has joined the review team as first author. |
| 14 August 2007 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
The authors would like to acknowledge the contribution of the peer referees, Wounds Group Editors (Nicky Cullum, Andrew Jull, Liz McInnes, Gill Worthy) and referees (Magnus Agren, Anne Marie Bagnall, Shirley Mankell, Nikki Stubbs). We would also like to thank the copy editors, Elizabeth Royle and Margaret Carver, and the contribution and advice of Sally Bell‐Syer (Managing Editor) and Ali Baba Akbari Sari and Ruth Foxlee (Trial Search Coordinators). The updated review was reviewed by Wounds Group Editors Gill Worthy and Dirk Ubbink.
Appendices
Appendix 1. Ovid MEDLINE search strategy
1 exp Pilonidal Sinus/ 2 pilonidal$.tw. 3 (pilonidal adj3 sinus$).mp. 4 (pilonidal adj3 fistula$).mp. 5 (pilonidal adj3 cyst$).mp. 6 (pilonidal adj3 disease$).mp. 7 (pilonidal adj3 abscess$).mp. 8 natal cleft.tw.
Appendix 2. Ovid EMBASE search strategy
1 exp Pilonidal Sinus/ 2 pilonidal$.tw. 3 (pilonidal adj3 sinus$).mp. 4 (pilonidal adj3 fistula$).mp. 5 (pilonidal adj3 cyst$).mp. 6 (pilonidal adj3 disease$).mp. 7 (pilonidal adj3 abscess$).mp. 8 natal cleft.tw. 9 or/1‐8
Appendix 3. EBSCO CINAHL search strategy
S9 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 S8 TI natal cleft or AB natal cleft S7 TI pilonidal N3 abscess* or AB pilonidal N3 abscess* S6 TI pilonidal N3 disease* or AB pilonidal N3 disease* S5 TI pilonidal N3 cyst* or AB pilonidal N3 cyst* S4 TI pilonidal N3 fistula* or AB pilonidal N3 fistula* S3 TI pilonidal N3 sinus* or AB pilonidal N3 sinus* S2 TI pilonidal or AB pilonidal S1 (MH "Pilonidal Cyst")
Appendix 4. Glossary of terms
Bascom procedure: an off‐midline surgical technique. The main incision is a lateral one which is developed deep under the skin so that the cavity is entered and excised. Tiny incisions are made to excise each of the individual pits down into the cavity. The resulting cavity can either be closed inside or left open whilst the lateral wound is always closed.
Bascom cleft closure: an off‐midline surgical technique that involves debridement of the diseased area after an off‐midline excision of the skin above the diseased area. A flap is mobilized from the opposite side of the wound, moving the sutures line away from the midline, which then covers the cleaned area.
Classical rhomboid (Limberg) flap: an off‐midline surgical technique. The diseased area is cut away in a rhomboid shape with an area of surrounding normal tissue. Then an adjacent rhomboid flap is moved to fill the rhomboid defect and sutured. The area from which the rhomboid flap was cut is closed in a straight line which can be achieved without difficulty as this skin is looser.
Karydakis technique: an off‐midline surgical technique that involves cutting away the diseased area in an elliptical shape which is centred on one side or the other of the wound. A flap from the side of the wound that involves the midline is raised and brought over the midline to cover the defect. The flap is then sutured to the other side of the wound.
Marsupialisation: an open surgical technique. The pilonidal sinus is excised with a surrounding area of normal tissue, the edges of the wound are then stitched closed together but not completely closed so that the resulting wound is smaller. Sutured in this way, the cyst remains open and can drain freely.
Modified rhomboid (Limberg) flap: this technique is similar to the classical rhomboid technique, however the end part of the suture line is moved to the side of the midline.
V‐Y advancement flap (related to midline): an off‐midline surgical technique. The diseased area is cut away, creating a defect that is closed with a “V” shaped full thickness flap. The technique of raising the flap is similar to that of a rhomboid flap only the shape is different. When the space left by the flap is closed the sutures form a Y shape.
Z‐Plasty: This is an off‐midline surgical technique where the whole diseased area is removed. This is followed by the skin flaps being cut in a Z‐shape and moved to fill the excised diseased area.
Data and analyses
Comparison 1. Open vs. closed (all).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 SSI rate | 10 | 1231 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [0.93, 1.85] |
| 1.1 open vs closed (midline) | 6 | 872 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.80, 1.77] |
| 1.2 open vs closed (other) | 4 | 359 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.68 [0.84, 3.37] |
| 2 Recurrence rate | 16 | 1666 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.46, 0.93] |
| 2.1 Open vs closed (midline) | 11 | 1213 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.33, 0.76] |
| 2.2 Open vs closed (other) | 5 | 453 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.65 [0.75, 3.62] |
| 3 Other complications & morbidity | 11 | 969 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.34, 1.46] |
| 3.1 Open vs closed (midline) | 6 | 510 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.18, 3.30] |
| 3.2 Open vs closed (other) | 5 | 459 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.37, 1.30] |
| 4 Patient satisfaction rate | 1 | 83 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.57, 0.99] |
| 5 Cost | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | 23.94 [0.73, 47.15] |
| 6 Pain | 2 | 220 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.45, 2.80] |
| 7 Wound healing rate | 5 | 474 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.85, 1.04] |
| 7.1 Open vs closed (midline) > 6 months | 3 | 278 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.90, 1.01] |
| 7.2 Open vs closed (other) > 6 months | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.97, 1.08] |
| 7.3 Open vs closed (midline) < 6 months | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.62, 0.88] |
Comparison 2. Closed (midline) vs. closed (other).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Time to wound healing | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | 5.40 [2.28, 8.52] |
| 2 SSI rate | 5 | 541 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.72 [1.86, 7.42] |
| 3 Recurrence rate | 6 | 574 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 4.54 [2.30, 8.96] |
| 3.1 Follow‐up more than one year (>80%) | 3 | 407 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 5.76 [2.53, 13.11] |
| 3.2 Follow‐up less than one year (>80%) | 1 | 33 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.13 [0.01, 2.26] |
| 3.3 Follow‐up more than one year (<80%) | 2 | 134 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 5.33 [1.39, 20.43] |
| 4 Time to return to work | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5 Other complications & morbidity | 3 | 461 | Risk Ratio (M‐H, Random, 95% CI) | 4.42 [1.51, 12.99] |
| 6 Patient satisfaction | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.51, ‐0.29] |
| 7 Pain | 2 | 133 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.51, ‐0.29] |
| 8 Wound healing rate | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 > 6 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 ≺ 6 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Operative time | 1 | 161 | Mean Difference (IV, Fixed, 95% CI) | 5.10 [2.98, 7.22] |
Comparison 3. Closed other (classic Limberg) vs. closed other (modified Limberg).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 SSI rate | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2 Recurrence rate | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 2.1 Follow‐up more than one year (>80%) | 1 | 68 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.19 [0.44, 117.48] |
| 3 Time to return to work | 1 | 68 | Mean Difference (IV, Fixed, 95% CI) | 2.40 [2.21, 2.59] |
| 4 Other complications & morbidity | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.54 [2.51, 22.71] |
| 5 Length of stay | 1 | 68 | Mean Difference (IV, Fixed, 95% CI) | 2.1 [1.89, 2.31] |
Comparison 4. Closed other (Karydakis) vs. closed other (classic Limberg).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 SSI rate | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.25 [1.14, 9.29] |
Comparison 5. Closed other (simple Bascom) vs closed other (Bascom cleft closure).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Recurrence | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.5 [0.23, 89.62] |
| 2 Wound healing rate | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 > 6months | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 9.9 [0.57, 170.81] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Abu Galala 1999.
| Methods | RCT, unblinded. | |
| Participants | 46 participants. 37 men, 9 women, Mean age 22.5 years. New sinus presentation only. | |
| Interventions | Closed midline (midline primary closure) vs. closed off‐midline (rhomboid flap) | |
| Outcomes | SSI rate, recurrence rate, RTW, LOS, % healed wounds. | |
| Notes | Complete follow‐up at 18 months. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "Randomly allocated". No information about randomisation method. |
| Allocation concealment? | Unclear risk | Quote: "allocated by a system of sequentially numbered sealed envelopes". No information about whether envelopes were opaque. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | No data reported on exclusions, attrition or missing data. |
| Free of selective reporting? | High risk | Element of selective under‐reporting. Data on time to complete wound healing were reported for closed off‐midline group but not for the midline closure group. |
| Free of other bias? | Low risk | |
Akca 2005.
| Methods | RCT, unblinded. | |
| Participants | 200 participants. 168 men, 32 women. Mean age 27 years range 15‐60. New sinus presentation. | |
| Interventions | Midline closure (excision and primary closure) vs. off‐midline closure (rhomboid excision and Limberg flap). | |
| Outcomes | SSI rate, recurrence rate, RTW, other complications, LOS, pain score. | |
| Notes | 100% follow‐up at 2 years. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "Randomly allocated....Computer generated table of random numbers". |
| Allocation concealment? | Low risk | Quote: "The randomization was carried out by an independent computer consultant". |
| Incomplete outcome data addressed? All outcomes | Low risk | No participants were lost to follow up. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
al‐Hassan 1990.
| Methods | RCT, unblinded. | |
| Participants | 96 participants. 68 men, 28 women. Mean age 23 years (range 13‐52). Both de novo and recurrent sinuses. | |
| Interventions | Midline closure (primary closure) vs. open healing. | |
| Outcomes | Healing time, recurrence, RTW, other complications, % initial healing. | |
| Notes | Complete follow up for at least one year; <80% drop out by 2 years. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "participants were randomised .... by taking a card from a sealed envelope". No information about the method of randomisation. |
| Allocation concealment? | Unclear risk | Quote: "...by taking a card from a sealed envelope". No information about whether envelopes were sealed or sequential. |
| Incomplete outcome data addressed? All outcomes | High risk | After randomisation, 4 participants were excluded from the closure group as closure was not possible. No information about the method of analysis used (e.g. intention to treat analysis). |
| Free of selective reporting? | High risk | Element of selective under reporting. Not enough information provided to incorporate time to wound healing data. |
| Free of other bias? | Low risk | |
Al‐Salamah 2007.
| Methods | RCT, unblinded. | |
| Participants | 380 participants. 355 men, 25 women. Mean age 22.6 years. New and recurrence sinuses. | |
| Interventions | Midline closure (simple excision with closure) vs open healing (simple excision without closure). | |
| Outcomes | Healing time, SSI, recurrence, RTW, , operating time. | |
| Notes | Follow up of 100% at a mean of 35.75 months. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "an equal number of envelopes with those two options were available in the operating room...Nurse mixed the envelopes". |
| Allocation concealment? | Low risk | Quote: "closed envelope randomisation...Opaque envelopes". |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Appropriately described valid reasons for exclusion. No information on attrition or missing data. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Berkem 2005.
| Methods | RCT, unblinded. | |
| Participants | 34 patients. 32 men, 2 women. Mean age 24.5 years (range 16‐44). New and recurrent sinuses. | |
| Interventions | V‐Y advancement flap, off mid‐line vs midline. | |
| Outcomes | SSI, Recurrence, LOS. | |
| Notes | 100% follow‐up at 12 months, 56% at 2 years. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "...participants were randomised into two groups". |
| Allocation concealment? | Unclear risk | Not reported. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | No information on exclusion, attrition or missing data. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Cihan 2006.
| Methods | RCT, unblinded | |
| Participants | 68 participants. 58 men, 10 women. Mean age 28.4 (range 17‐43). Recurrence presentation only. | |
| Interventions | Off‐midline closure (classic Limberg flap) vs. Off‐midline closure (modified Limberg flap). (off‐midline v. off‐midline). | |
| Outcomes | SSI, recurrence, RTW, other complications, LOS. | |
| Notes | Follow up for 2 years, no dropouts described. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "The randomization of the patients into groups was done in such a way that every other patients with pilonidal disease was assigned to the group a modified method of treatment". |
| Allocation concealment? | Unclear risk | Not reported. |
| Incomplete outcome data addressed? All outcomes | High risk | Two participants from the total number of participants (n=70) could not be fully followed up so they were excluded from analysis. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Ersoy 2009.
| Methods | RCT, unblinded. | |
| Participants | 82 participants. 68 men, 14 women. Mean age 26.8 years. Not clear if new or recurrence presentation. | |
| Interventions | Karydakis procedure vs Rhomboid excision and classic Limberg (off‐midline vs off‐midline). | |
| Outcomes | SSI, time to return to activity, time to return to driving, Pain (VAS), wound dressing time, oral analgesia need, difficulty of defecation count. | |
| Notes | follow up 100% at 30 days. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "patients were randomized according to their admission protocol number". |
| Allocation concealment? | Unclear risk | Not reported. |
| Incomplete outcome data addressed? All outcomes | Low risk | |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Ertan 2005.
| Methods | RCT, unblinded. | |
| Participants | 100 participants. 91 men, 9 women. Mean age 27.2 years (range 17‐47). Unclear whether recurrence or new presentation. | |
| Interventions | Midline closure (primary midline closure) vs. off‐midline closure (rhomboid excision & Limberg flap). | |
| Outcomes | Healing time, SSI, recurrence, RTW, other complications, QOL, pain. | |
| Notes | Follow‐up of 65% at one year. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | "Balanced randomisation" |
| Allocation concealment? | Unclear risk | Not reported. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | No information on exclusion or missing data. Attrition was described, but no explanation of reasons for drop out or how were they dealt with in the analysis. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Fazeli 2006.
| Methods | RCT, unblinded. | |
| Participants | 144 participants. 123 men, 21 women. Mean age 25.6 years. Unclear whether recurrence or new presentation. | |
| Interventions | Open healing (excision and healing by secondary intention) vs. off‐midline closure (z‐plasty). | |
| Outcomes | Time to healing, SSI, recurrence, RTW, other complications, hospital stay. | |
| Notes | Mean follow up of 22 months, complete in z‐plasty group, 6 drop‐outs in open group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "Randomized clinical trial". |
| Allocation concealment? | Unclear risk | Not reported. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Study reported missing data, but no information on how they were incorporated into the analysis. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Füzün 1994.
| Methods | RCT, unblinded. | |
| Participants | 110 participants. Age & sex details not reported. Unclear whether recurrence or new presentation. | |
| Interventions | Open healing (obeid excision and semi‐open packing) vs. midline closure (excision and primary midline closure). | |
| Outcomes | SSI, recurrence, RTW, LOS. | |
| Notes | Follow up of 83% at mean of 23 months. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "..were randomly assigned" |
| Allocation concealment? | Unclear risk | Not reported. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | No information on exclusions, attrition or missing data. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Gencosmanoglu 2005.
| Methods | RCT, unblinded. | |
| Participants | 151 participants. 131 men, 11 women. Median age 25.5 years (range 16‐49). New presentation & recurrence. | |
| Interventions | Open healing (modified lay‐open marsupialisation) vs. midline closure (primary midline closure). | |
| Outcomes | Healing time, SSI, recurrence, RTW, other complications rate. | |
| Notes | 100% follow up at 2 years. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | "..randomly allocated to two groups according to the initial letter of their surname (A‐M, group A; N‐Z, group B)" |
| Allocation concealment? | High risk | No concealment possible because sequence predicted by surname. |
| Incomplete outcome data addressed? All outcomes | Low risk | All participants were followed up. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Hameed 2001.
| Methods | RCT, unblinded | |
| Participants | 43 participants. 34 men, 9 women. Mean age 23.7 years (range 17‐33). New presentation only. | |
| Interventions | Open healing (wide excision open) vs. midline closure (primary midline closure). | |
| Outcomes | Healing time, SSI, recurrence, other complications, cost. | |
| Notes | 88% follow up at 3 years. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "The patients were randomised". |
| Allocation concealment? | Unclear risk | Not reported. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Reported that two participants opted for primary closure despite randomisation. No information on how they were incorporated into the analysis (e.g. whether they used intention to treat analysis or not). |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Unclear risk | Participants were followed in outpatient clinic. However, when it was impractical they were followed by a telephone call or a questionnaire. The study did not report the number of participants for each assessment method or whether this was applied to all or some outcomes. |
Jamal 2009.
| Methods | RCT, unblinded. | |
| Participants | 49 participants. 45 men, 4 women. Mean age 26.44 years. New and recurrence sinuses. | |
| Interventions | Open healing (open excision and secondary healing) vs off‐midline closure (rhomboid excision and classic Limberg flap). | |
| Outcomes | Healing time, recurrence, SSI, operating time, pain, other complications. | |
| Notes | Follow up of about 92% at 18 months average. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "Blocked randomization was used". No information of the process of selection (e.g. random number table, or computer random number generation) |
| Allocation concealment? | Unclear risk | Not reported. |
| Incomplete outcome data addressed? All outcomes | High risk | Exclusion criteria were cases with incomplete participant data and participants who were lost to follow up. |
| Free of selective reporting? | Unclear risk | Element of under reporting: Not enough information to extract operative time. |
| Free of other bias? | Unclear risk | All participants were operated under general or spinal anaesthesia. No information on the number of participants who had general or spinal anaesthesia by intervention. |
Karakayali 2009.
| Methods | RCT, unblinded. | |
| Participants | 140 participants. 118 men, 22 women. Mean age 23.8 years. New sinuses only. | |
| Interventions | Open healing (unroofing & Marsupialisation) vs off‐midline closure (rhomboid excision and classic Limberg flap). | |
| Outcomes | healing time, SSI, RTW, other complications, QOL, pain, operative time, time to sitting without pain, time to return to daily activities without pain, time to walk with out pain. | |
| Notes | Patients were follow up for a mean of 15 months. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "computer generated table of random numbers, we randomly assigned participants..". |
| Allocation concealment? | Unclear risk | Not reported. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | All participants in both groups were followed up on an outpatient basis until the healing was complete. No information about exclusion, attrition, or missing data. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Unclear risk | The study used telephone or outpatient appointments to assess further recurrence after data analyses but numbers by method were not specified. |
Kareem 2006.
| Methods | RCT, unblinded. | |
| Participants | 77 participants. 59 men, 18 women. Mean age 25.9 years. unclear if new or recurrent sinuses. | |
| Interventions | Open healing (excision and healing by secondary intention) vs midline closure (primary midline closure). | |
| Outcomes | healing time, recurrence, RTW, other complications, operating time. | |
| Notes | 92% follow up at a mean of 4 years. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "patients were randomised in 2 groups". |
| Allocation concealment? | Unclear risk | Not reported. |
| Incomplete outcome data addressed? All outcomes | High risk | Quote: "Seven cases (two cases from group A and 5 cases from group B) were excluded from the study as they were lost to follow up". |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Khawaja 1992.
| Methods | RCT, unblinded. | |
| Participants | 46 participants. 36 men, 10 women. Age and sex details not reported. Unclear whether recurrence/new sinuses presentation. | |
| Interventions | Open healing vs. primary midline closure. | |
| Outcomes | Healing time, recurrence at 6 and 12 months, RTW, other complications, LOS out‐patient visits. | |
| Notes | 100% follow up at 2 years | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "Randomly allocated to a treatment group by a system of sequentially numbered opaque sealed envelopes". |
| Allocation concealment? | Low risk | "opaque sealed envelopes" |
| Incomplete outcome data addressed? All outcomes | Low risk | Study used intention to treat analysis |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Kronborg 1985.
| Methods | RCT, unblinded. | |
| Participants | 99 participants. 80 men, 19 women. Median ages 23/25/28 years (range 15‐52). New and recurrence presentation. | |
| Interventions | Open healing vs. primary midline closure vs. primary midline closure with antibiotics. | |
| Outcomes | Healing time, recurrence. | |
| Notes | 3 groups, 2 closed groups combined. 95% follow up at 3 years. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "Balanced randomisation" |
| Allocation concealment? | Unclear risk | Not reported. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | At 3 years follow up, 4 participants who did not complete follow up. No information about how they were incorporated into the analysis. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Miocinovic 1999.
| Methods | Quasi RCT with 3 comparisons. Unblinded. Data extracted from 2 arms | |
| Participants | 100 participants. 82 men, 18 women. Mean age 23.7 years (SD 5.2). Only data for 50 participants included. New sinus presentation only. | |
| Interventions | Open healing (excision and open healing) vs. midline closure (primary midline closure). | |
| Outcomes | Recurrence. | |
| Notes | Although 100 participants studied, only used open v. closed data for sub‐set of 50 randomised with new presentation. Follow up 100% at 12 months. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "Randomized prospective study". |
| Allocation concealment? | Unclear risk | Not reported. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | No information on exclusions, attrition, or missing data. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | High risk | Groups were not comparable at baseline with respect to recurrence status. |
Mohamed 2005.
| Methods | RCT unblinded. | |
| Participants | 83 participants. 68 men, 15 women. Mean age 26.6 years (range 19‐31). New presentation. | |
| Interventions | Open wide excision vs. open limited excision vs. wide excision and primary midline closure. | |
| Outcomes | Healing time, recurrence pain, satisfaction, LOS. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "Randomly assigned". |
| Allocation concealment? | Unclear risk | Quote: "closed envelope randomisation". No mention if they were opaque. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | No information on exclusions, attrition, or missing data. |
| Free of selective reporting? | High risk | Selective under reporting: not enough information about time to wound healing include within a meta analysis. Data presented in a graph. |
| Free of other bias? | Low risk | |
Nordon 2009.
| Methods | RCT, unblinded | |
| Participants | 55 participants. 37 men, 18 women. Mean age 27 years. New and recurrence presentation. | |
| Interventions | Off‐midline closure (Simple Bascom) vs. off‐midline closure ( Bascom's Cleft Closure). | |
| Outcomes | Recurrence, RTW, wound healing rate | |
| Notes | 91% follow up at a mean of 36 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "Patients were randomized". |
| Allocation concealment? | Unclear risk | Quote: "Patients were randomized by sequentially numbered sealed envelopes". No mention if they were opaque. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | No information on exclusions, attrition, or missing data. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Unclear risk | It appears that before randomisation, participants were excluded from the study if they were not available for follow‐up evaluation. No information about the number of participants who were excluded or their characteristics. |
Rao 2001.
| Methods | RCT, unblinded. | |
| Participants | Sex and age not reported. 59 participants. Unclear whether new or recurrence presentation. | |
| Interventions | Open Healing (open and marsupialisation) vs. midline closure (primary closure). | |
| Outcomes | Healing time, pain, LOS, healing rate. | |
| Notes | No follow up details. Abstract only. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "Patients were randomly assigned". |
| Allocation concealment? | Unclear risk | Not reported. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | No information on exclusions, attrition, and missing data. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Unclear risk | Limited information because restricted to oral abstract. |
Sakr 2006.
| Methods | RCT, unblinded | |
| Participants | 161 participants. 138 men, 23 women. Mean age 24.6 years. New and recurrence presentation. | |
| Interventions | Off‐midline closure (Karydakis procedure) vs. midline closure (standard midline closure) | |
| Outcomes | SSI , recurrence, return to normal activities, other complications rate, operative time, healing rate. | |
| Notes | 94.4% follow up at a mean of 30.4 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not reported |
| Allocation concealment? | Unclear risk | Quote: "patients who were categorized, using the closed method..". |
| Incomplete outcome data addressed? All outcomes | High risk | Participants lost to follow up (n=9) were not included in the study analysis. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Sheikh 2007.
| Methods | RCT, unblinded. | |
| Participants | 26 participants. 25 males, 1 female. Mean age not reported, range 17 to 42 years. States that complex recurrence cases excluded. | |
| Interventions | Open healing (wide excision and open wound) vs. off‐midline closure (Karydakis procedure). | |
| Outcomes | Healing time, SSI, recurrence, RTW, other complications, operative time. | |
| Notes | Mean follow‐up 14 months. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Participants were "randomized". |
| Allocation concealment? | Unclear risk | Not reported |
| Incomplete outcome data addressed? All outcomes | Unclear risk | No information of exclusions, attrition and missing data. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Søndenaa 1992.
| Methods | RCT, unblinded. | |
| Participants | 120 participants, sex and age not reported. Unclear whether new or recurrence presentation. | |
| Interventions | Open healing vs. primary midline closure. | |
| Outcomes | Healing time, SSI, other complications, pain, RTW, recurrence, pain. | |
| Notes | 96% follow up at 1 year. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "Method of treatment was decided by opening envelopes from a stack of 120 that had been randomised and closed but not sealed". |
| Allocation concealment? | High risk | |
| Incomplete outcome data addressed? All outcomes | Low risk | Median of 4.2 years follow up, 113 returned a questionnaire investigating long term outcomes. the 7 that did not respond were contacted by a phone call. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Unclear risk | The study used questionnaires and phone calls to investigate long term clinical outcome (recurrence). Data by each method were not reported. |
Testini 2001.
| Methods | RCT unblinded. | |
| Participants | 100 participants,: 69 men, 31 women. Mean age 23 years (range 15‐64). New presentation sinus only | |
| Interventions | Open healing vs. off‐midline closure (Karydakis technique). | |
| Outcomes | Healing time, recurrence, RTW, complications, pain. | |
| Notes | 100% follow up at 3 years. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "The generation of random sequences of allocation was achieved using a coin". |
| Allocation concealment? | Unclear risk | Not reported. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | No information on exclusions, attrition, and missing data. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Unclear risk | Follow up performed at outpatient visit or telephone but not data by method were reported. |
Wright 2001.
| Methods | RCT, unblinded. | |
| Participants | 33 participants, sex and age not reported. Unclear whether new or recurrence presentation. | |
| Interventions | Primary midline closure vs. off‐midline closure (Bascom technique). | |
| Outcomes | Healing rate, RTW, pain, LOS. | |
| Notes | Abstract lacking in data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "this is a randomised comparison of Bascom". |
| Allocation concealment? | Unclear risk | Not reported. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | No information on exclusions, attrition, and missing data. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Unclear risk | Limited data because it was a poster abstract. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Amorín 1989 | Unable to trace |
| Awad 2007 | Methodology and interventions did not satisfy inclusion criteria |
| Baier 2002 | Fully translated: retrospective, not a clinical trial |
| Bascom 2002 | Case study |
| Christensen 1985 | Paper translated: participant group contained acute abscess |
| Collazo 1994 | RCT stopped prior to endpoints being reached: 11 participants only: poor description of results and outcomes |
| De Falco 2007 | Paper translated: retrospective cohort study |
| Duxbury 2003 | Interventions did not satisfy inclusion criteria |
| Faltz 1990 | Translated: interventions did not satisfy inclusion criteria |
| Golz 1980 | Case series description without comparison group |
| Gupta 2004 | Interventions did not satisfy inclusion criteria |
| Gupta 2005 | Interventions did not satisfy inclusion criteria |
| Hell 1971 | Translated: unclear study design |
| Hodgson 1981 | Poor methodology: inadequate description of results: large losses to follow up |
| Hollingworth 1992 | Series of letters |
| Hosseini 2006 | Included participants with acute abscess |
| Khalid 2001 | Unable to trace |
| Maniscalco 2001 | Paper translated: retrospective cohort study |
| Mann 1987 | Case series |
| Marks 1985 | Not an RCT: interventions did not satisfy inclusion criteria |
| Morrison 1985 | Large proportion of cases were pilonidal abscesses |
| Notaras 1970 | Review article |
| Oncel 2002 | Interventions did not appear to satisfy inclusion criteria: attempt to contact author: no reply |
| Ortiz 1977a | Interventions did not appear to satisfy inclusion criteria: attempt to contact author: no reply |
| Ortiz 1977b | Spanish language version of Ortiz 1977a |
| Petersen 2002 | Review article |
| Reidler 1978 | Translated: retrospective review |
| Sturniolo 1984 | Translated: not a clinical trial |
| Søndenaa 2002 | Intervention is antibiotic usage |
| Søreide 2009 | Review article |
| Watson 2005 | Letter |
| Werkgartner 2004 | Editorial |
| Wienart 2004 | Review article |
Differences between protocol and review
One new outcome has been added: operation time. This has been added post‐protocol.
One major difference from the original review is the change to the assessment of risk of bias. Based on the updated Cochrane Handbook, we adhered to recommendations in Chapter 8 and have altered the quality criteria accordingly. We have removed the original Table 6 and replaced with Figure 1 which presents a methodological quality summary for each included study.
Contributions of authors
The original protocol was written by IM and JB. PMK conceived the study & advised on clinical aspects. IM and JB wrote the original review. AA, IM and JB extracted data and wrote the updated review.
Sources of support
Internal sources
Not specified, Not specified.
External sources
-
Medical Research Council, UK.
JB was funded by the MRC from 2005 to 2007.
Declarations of interest
None declared
Edited (no change to conclusions)
References
References to studies included in this review
Abu Galala 1999 {published data only}
- Abu Galala KH, Salam IM, Abu Samaan KR, Ashaal YI, Chandran VP, Sabastian M, et al. Treatment of pilonidal sinus by primary closure with a transposed rhomboid flap compared with deep suturing: a prospective randomised clinical trial. European Journal of Surgery 1999;165(5):468‐72. [DOI] [PubMed] [Google Scholar]
Akca 2005 {published data only}
- Akca T, Colak T, Ustunsoy B, Kanik A, Aydin S. Randomized clinical trial comparing primary closure with the Limberg flap in the treatment of primary sacrococcygeal pilonidal disease. British Journal of Surgery 2005;92(9):1081‐4. [DOI] [PubMed] [Google Scholar]
al‐Hassan 1990 {published data only}
- al‐Hassan HK, Francis IM, Neglén P. Primary closure or secondary granulation after excision of pilonidal sinus?. Acta Chirurgica Scandinavica 1990;156(10):695‐9. [PubMed] [Google Scholar]
Al‐Salamah 2007 {published data only}
- Al‐Salamah S, Hussain M, Mirza S. Excision with or without primary closure for Pilonidal sinus disease. Journal of the Pakistan Medical Association 2007;57(8):388‐91. [PubMed] [Google Scholar]
Berkem 2005 {published data only}
- Berkem H, Topaloglu S, Ozel H, Avsar FM, Yildiz Y, Yuksel BC, et al. V‐Y advancement flap closures for complicated pilonidal sinus disease. International Journal of Colorectal Disease 2005;20(4):343‐8. [DOI] [PubMed] [Google Scholar]
Cihan 2006 {published data only}
- Cihan A. Superiority of asymmetric modified Limberg flap for surgical treatment of pilonidal disease. Diseases of the Colon and Rectum 2006;49:244. [DOI] [PubMed] [Google Scholar]
Ersoy 2009 {published data only}
- Ersoy E, Devay A, Doganay B, Özdoğan M, Gündoğdu RH. Comparison of short‐term results after Limberg and Karydakis procedures. Colorectal Disease 2009;11(7):705‐710. [DOI] [PubMed] [Google Scholar]
Ertan 2005 {published data only}
- Ertan T, Koc M, Gocmen E, Aslar AK, Keskek M, Kilic M. Does technique alter quality of life after pilonidal sinus surgery?. American Journal of Surgery 2005;190(3):388‐92. [DOI] [PubMed] [Google Scholar]
Fazeli 2006 {published data only}
- Fazeli MS, Adel MG, Abaschi AH. Comparison of outcomes in Z‐plasty and delayed healing by secondary intention of the wound after excision of the sacral pilonidal sinus: Results of a randomized, clinical trial. Diseases of the Colon and Rectum 2006;49(12):1831‐6. [DOI] [PubMed] [Google Scholar]
Füzün 1994 {published data only}
- Füzün M, Bakir H, Soylu M, Tansu, T, Kamak E, Harmancioglu O. Which technique for treatment of pilonidal sinus ‐‐ open or closed?. Diseases of the Colon and Rectum 1994;37(11):1148‐50. [DOI] [PubMed] [Google Scholar]
Gencosmanoglu 2005 {published data only}
- Gencosmanoglu R, Inceoglu R. Modified lay‐open (Incision, Curettage, Partial lateral wall excision and Marsupialization) versus Total Excision with Primary Closure in the treatment of chronic sacrococcygeal pilonidal sinus. International Journal of Colorectal Disease 2005;20(5):415‐22. [DOI] [PubMed] [Google Scholar]
Hameed 2001 {published data only}
- Hameed KK. Outcome of surgery for chronic natal cleft pilonidal sinus: A randomized trial of open compared with closed technique. Journal of College Surgeons and Physicians Pakistan 2001;11(1):32‐5. [Google Scholar]
Jamal 2009 {published data only}
- Jamal A, Shamim, M, Hashim F, Quershi, M. Open excision with secondary healing versus rhomboid excision with Limberg transposition flap in the management of Sacrococcygeal Disease. Journal of the Pakistan Medical Association 2009;59(3):157‐60. [PubMed] [Google Scholar]
Karakayali 2009 {published data only}
- Karakayali F, Karagllue E, Karabulut Z, Oksuz E, Moray G, Haberal M. Unroofing and Marsupialization vs. Rhomboid Excision and Limberg Flap in Pilonidal Disease: A Prospective, Randomized, Clinical Trial. Disease of the Colon and Rectum 2009;52(3):496‐502. [DOI] [PubMed] [Google Scholar]
Kareem 2006 {published data only}
- Kareem T. Surgical treatment of chronic sacrococcygeal pilonidal sinus Open method versus primary closure . Saudi Medical Journal 2006;27(10):1534‐7. [PubMed] [Google Scholar]
Khawaja 1992 {published data only}
- Khawaja HT, Bryan S, Weaver PC. Treatment of natal cleft sinus: a prospective clinical and economic evaluation. BMJ 1992;304(6837):1282‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kronborg 1985 {published data only}
- Kronborg O, Christensen K, Zimmermann‐Nielsen C. Chronic pilonidal disease: a randomized trial with a complete 3‐year follow‐up. British Journal of Surgery 1985;72(4):303‐4. [DOI] [PubMed] [Google Scholar]
Miocinovic 1999 {published data only}
- Miocinovic M, Horzic M, Bunoza D. The treatment of pilonidal disease of the sacrococcygeal region by the method of limited excision and open wound healing. Acta Medica Croatica 1999;54(1):27‐31. [PubMed] [Google Scholar]
Mohamed 2005 {published data only}
- Mohamed HA, Kadry I, Adly S. Comparison between three therapeutic modalities for non‐complicated pilonidal sinus disease. The Surgeon: Journal of the Royal Colleges of Surgeons of Edinburgh and Ireland 2005;3(2):73‐7. [DOI] [PubMed] [Google Scholar]
Nordon 2009 {published data only}
- Nordon I, Senapti A, Cripps NP. Bascom's operation versus cleft closure for the treatment of chronic pilonidal sinus; a prospective randomised controlled trial. Colorectal Disease 2005;7(1):38. [Google Scholar]
- Nordon IM, Senapati A, Cripps NPJ. A prospective randomized controlled trial of simple Bascom's technique versus Bascom's cleft closure for the treatment of chronic pilonidal disease. American Journal of Surgery 2009;197(2):189‐92. [DOI] [PubMed] [Google Scholar]
Rao 2001 {published data only}
- Rao M, Zawislak W, Gilliland R. A prospective randomised trial comparing two treatment modalities for chronic pilonidal sinus (ABSTRACT). Colorectal Disease 2001;3(1 Suppl 1):Oral 102. [DOI] [PubMed] [Google Scholar]
Sakr 2006 {published data only}
- Sakr M, Habib M, Shaheed A. Assessment of Karydakis Technique as Compared With Midline Closure For the Management of Chronic Pilonidal Sinus. Journal of Pelvic Medicine and Surgery 2006;12(4):201‐6. [Google Scholar]
Sheikh 2007 {published data only}
- Sheikh MR, Khalid MA, Rehman SU. Outcome of surgery for pilonidal sinus: Karydakis versus open procedure. Pakistan Journal of Surgery 2007;23(3):202‐4. [Google Scholar]
Søndenaa 1992 {published data only}
- Søndenaa K, Andersen E, Søreide JA. Morbidity and short term results in a randomised trial of open compared with closed treatment of chronic pilonidal sinus. European Journal of Surgery 1992;158(6‐7):351‐5. [PubMed] [Google Scholar]
- Søndenaa K, Nesvik I, Andersen E, Søreide JA. Recurrent pilonidal sinus after excision with closed or open treatment: final result of a randomised trial. European Journal of Surgery 1996;162(3):237‐40. [PubMed] [Google Scholar]
Testini 2001 {published data only}
- Testini M, Piccinni G, Miniello S, Venere B, Lissidini G, Nicolardi V, et al. Treatment of chronic pilonidal sinus with local anaesthesia: A randomized trial of closed compared with open technique. Colorectal Disease 2001;3(6):427‐30. [DOI] [PubMed] [Google Scholar]
Wright 2001 {published data only}
- Wright DM, Anderson JH, Molloy RG. A randomised trial of the Bascom procedure vs. primary closure for pilonidal sinus. Colorectal Disease 2001;3(1 Suppl 1):Poster 185. [Google Scholar]
References to studies excluded from this review
Amorín 1989 {published data only}
- Amorín J, Villani D, Ruiz R, Salinas A. Resection and primary closure vs simple curetage in the treatment of pilonidal sinus.. Revista Venezolana de Cirugía 189;42(1):138‐141. [Google Scholar]
Awad 2007 {published data only}
- Awad M, Saad K, Tolba A, Gharib O. A simple novel technique for closure of simple and complex pilonidal sinus with either simple (tongue‐shaped) or bilobed rotation flap. Indian J Plast Surg 2007;40(1):47‐50. [Google Scholar]
Baier 2002 {published data only}
- Baier PK, Baumgartner U, Furtwangler A, Holzinger F, Schoffel U, Baier PK, et al. Therapy of the pilonidal sinus ‐ Primary wound closure or open wound after excision. Zentralblatt fur Chirurgie 2002;127(4):310‐4. [DOI] [PubMed] [Google Scholar]
Bascom 2002 {published data only}
- Bascom J, Bascom T. Failed pilonidal surgery: new paradigm and new operation leading to cures. Archives of Surgery 2002;137:1146‐50. [DOI] [PubMed] [Google Scholar]
Christensen 1985 {published data only}
- Christensen K, Kronborg O, Zimmermann‐Nielsen C, Olsen H. Incision or primary suture in acute pilonidal abscesses. A prospective randomized study. Ugeskrift for Laeger 1985;147(44):3479‐81. [PubMed] [Google Scholar]
Collazo 1994 {published data only}
- Collazo E, Luna M. Obeid's technique for treatment of pilonidal sinus. Diseases of the Colon and Rectum 1994;37(7):731‐2. [DOI] [PubMed] [Google Scholar]
De Falco 2007 {published data only}
- Falco M, Ragusa M, Oliva G, Miranda A, Giudicianni C, Sperlongano P, et al. Surgical treatment of sinus pilonidalis by Dufourmentel's flap technique. Il Giornale Di Chirugia 2007;28(3):93‐7. [PubMed] [Google Scholar]
Duxbury 2003 {published data only}
- Duxbury MS, Blake SM, Dashfield A, Lambert AW. A randomised trial of knife versus diathermy in pilonidal disease. Annals of the Royal College of Surgeons of England 2003;85(6):405‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Faltz 1990 {published data only}
- Faltz HC, Brieler HS. Therapy of Sinus pilonidalis. Zentralblatt Fur Chirurgie 1990;115:1205. [Google Scholar]
Golz 1980 {published data only}
- Golz A, Argove S, Barzilai A. Pilonidal sinus disease: comparison among various methods of treatment and a survey of 160 patients. Current Surgery 1980;37(2):77‐85. [PubMed] [Google Scholar]
Gupta 2004 {published data only}
- Gupta PJ. A randomized study between excision and marsupialization and radiofrequency sinus excision in sacro‐coccygeal pilonidal disease. Current Surgery 2004;61(3):307‐12. [DOI] [PubMed] [Google Scholar]
Gupta 2005 {published data only}
- Gupta PJ. Radiofrequency sinus excision: better alternative to marsupialization technique in sacrococcygeal pilonidal sinus disease. Journal of the National Medical Association 2005;97(7):998‐1002. [PMC free article] [PubMed] [Google Scholar]
Hell 1971 {published data only}
- Hell E, Zimmermann G, Boeckl O. Pilonidal disorder (pilonidal cyst) and its treatment. Die Medizinische Welt. 1971;6:230‐2. [PubMed] [Google Scholar]
Hodgson 1981 {published data only}
- Hodgson WJ, Greenstein RJ. A comparative study between Z‐plasty and incision and drainage or excision with marsupialization for pilonidal sinuses. Surgery, Gynecology and Obstetrics 1981;153(6):842‐4. [PubMed] [Google Scholar]
Hollingworth 1992 {published data only}
- Hollingworth J, Hegarty DM, Kaufman HD. Treatment of natal cleft sinus. BMJ 1992;305(6848):311‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hosseini 2006 {published data only}
- Hosseini S, Banazadeh A, Rivaz M, Sabet B, Mosallae M, Purahmad M, et al. The comparison between drainage, delayed excision and primary closure with excision and secondary healing in management of pilonidal abscess. International Journal of Surgery 2006;4(4):228‐31. [DOI] [PubMed] [Google Scholar]
Khalid 2001 {published data only}
- Khalid K. Outcome of surgery for chronic natal cleft pilonidal sinus: a randomized trial of open compared with closed technique. Journal of the College of Physicians and Surgeons Pakistan 2001;11(1):32‐5. [Google Scholar]
Maniscalco 2001 {published data only}
- Maniscalco L, Speranza G, Maniscalco A. The pilonidal sinus: Which management?. Chirurgia Torino 2001;14(2):81‐3. [Google Scholar]
Mann 1987 {published data only}
- Mann CV, Springall R. 'D' excision for sacrococcygeal pilonidal sinus disease. Journal of the Royal Society of Medicine 1987;80(5):292‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Marks 1985 {published data only}
- Marks J, Harding KG, Hughes LE, Ribeiro CD. Pilonidal sinus excision ‐ healing by open granulation. British Journal of Surgery 1985;72:637‐40. [DOI] [PubMed] [Google Scholar]
Morrison 1985 {published data only}
- Morrison PD. Is Z‐plasty closure reasonable in pilonidal disease?. Irish Medical Journal 1985;154(3):110‐12. [DOI] [PubMed] [Google Scholar]
Notaras 1970 {published data only}
- Notaras MJ. A review of three popular methods of treatment of postanal (pilonidal) sinus disease. British Journal Surgery 1970;57(12):886‐90. [DOI] [PubMed] [Google Scholar]
Oncel 2002 {published data only}
- Oncel M, Kurt N, Kement M, Colak E, Eser M, Uzun H. Excision and marsupialization versus sinus excision for the treatment of limited chronic pilonidal disease: a prospective, randomized trial. Techniques in Coloproctology 2002;6(3):165‐9. [DOI] [PubMed] [Google Scholar]
Ortiz 1977a {published data only}
- Ortiz HH, Marti J, Sitges A. Pilonidal sinus: a claim for simple track incision. Diseases of the Colon and Rectum 1977;20(4):325‐8. [DOI] [PubMed] [Google Scholar]
Ortiz 1977b {published data only}
- Ortiz H, Martí J, Sitges A. Pilonidal sinus. Comparative study of three surgical techniques. Cirugía Española 1977;31(5):413‐8. [Google Scholar]
Petersen 2002 {published data only}
- Petersen S, Koch R, Stelzner S, Wendlandt TP, Ludwig K. Primary closure techniques in chronic pilonidal sinus: a survey of the results of different surgical approaches. Diseases of the Colon and Rectum 2002;45(11):1458‐67. [DOI] [PubMed] [Google Scholar]
Reidler 1978 {published data only}
- Riedler L, Weimann S, Steiner E. Operative therapy of the pilonidal sinus; 115 control patients [Beitrag zur operativen therapie des Sakraldermoids.]. Zentralblatt fur Chirugurgie 1978;103(21):1410‐15. [PubMed] [Google Scholar]
Sturniolo 1984 {published data only}
- Sturniolo G, Carditello A, Bonavito G, Martolotta M, Saitta E. [Evaluation of the results of different types of surgical intervention for pilonidal fistula] [Valutazione dei risultati dei differenti tipi di intervento chirurgico per fistola pilonidale]. Minerva Chirugica 1984;39(17):1161‐4. [PubMed] [Google Scholar]
Søndenaa 2002 {published data only}
- Søndenaa K, Diab R, Nesvik I, Gullaksen FP, Kristiansen RM, Saebø A, Kømer H. Influence of failure of primary wound healing on subsequent recurrence of pilonidal sinus. combined prospective study and randomised controlled trial. The European Journal of Surgery ‐ Acta Chirurgica 2002;168(11):614‐8. [DOI] [PubMed] [Google Scholar]
Søreide 2009 {published data only}
- Søredie K. The best surgical technique for chronic pilonidal disease‐is this question still open or closed?. Nature Clinical Practice Gastroenterology and Hepatology 2008;6(1):20‐22. [DOI] [PubMed] [Google Scholar]
Watson 2005 {published data only}
- Watson A, Cheetham M. Randomized clinical trial comparing primary closure with the Limberg flap in the treatment of primary saccrococcygeal pilonidal disease. British Journal Surgery 2005;92:1455. [DOI] [PubMed] [Google Scholar]
Werkgartner 2004 {published data only}
- Werkgartner. Invited commentary to "Knowledge‐based therapy of the pilonidal sinus". European Surgery 2004;36(6):170‐1. [Google Scholar]
Wienart 2004 {published data only}
- Wienart V. Knowledge‐based therapy of the pilonidal sinus. European Surgery 2004;36(3):166‐7. [Google Scholar]
Additional references
Al‐Naami 2005
- Al‐Naami MY. Outpatient pilonidal sinotomy complemented with good wound and surrounding skin care. Saudi Medical Journal 2005;26(2):285‐8. [PubMed] [Google Scholar]
Aldean 2005
- Aldean I, Shankar PJ, Mathew J, Safarani N, Haboubi NY. Simple excision and primary closure of pilonidal sinus: a simple modification of conventional technique with excellent results. Colorectal Disease 2005;7(1):81‐5. [DOI] [PubMed] [Google Scholar]
Allen‐Marsh 1990
- Allen‐Marsh, TG. Pilonidal Sinus: finding the right track of treatment. British Journal of Surgery 1990;77:123‐32. [DOI] [PubMed] [Google Scholar]
Als‐Nielsen 2004
- Als‐Nielsen B Gluud LL, Gluud C. Methodological quality and treatment effects in randomized trials: a review of six empirical studies. 12th Cochrane Colloquium. 2004:88‐9.
Chinn 2003
- Chinn BT. Outpatient management of pilonidal disease.. Sem Colon Rectal Surgery 2003;14:166‐72. [Google Scholar]
Doll 2007
- Doll D, Krueger CM, Schrank S, Dettmann H, Petersen S, Duesel W. Timeline of recurrence after primary and secondary pilonidal sinus surgery. Diseases of the Colon and Rectum 2007;50(10):1928‐34. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analysis. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT and Altman DG on behalf of the Cochrane Statistical Methods Group and the Cochrane Bias Methods Group (Editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 (updated September 2008).The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org.
Lee 2008
- Lee PJ, Raniga S, Biyani DK, Watson AJM, Faragher IG, Frizelle FA. Sacrococcygeal pilonidal disease. Colorectal Disease 2008;10(7):639‐50. [DOI] [PubMed] [Google Scholar]
Lefebvre 2008
- Lefebvre C, Manheimer E, Glanville J, on behalf of the Cochrane Information Retrieval Methods Group. Chapter 6: Searching for studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 (updated September 2008). The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org 2008.
Moher 2001
- Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel‐group randomised trials. The Lancet 2001;357:1191‐4. [PubMed] [Google Scholar]
Notaro 2003
- Notaro JR. Management of recurrent pilonidal disease. Seminars in Colon and Rectal Surgery 2003;14(4):173‐85. [Google Scholar]
Pildal 2007
- Pildal J, Hròbjartsson A, Jørgensen KJ, Hilden J, Altman DG, Gøtzsche PC. Impact of allocation concealment on conclusion drawn from meta‐analyses of randomized trials. International Journal of Epidemiology 2007;36:847‐57. [DOI] [PubMed] [Google Scholar]
Schultz 1995
- Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of the treatment effects in controlled trials. JAMA 1995;273:408‐12. [DOI] [PubMed] [Google Scholar]
SIGN 2009
- Scottish Intercollegiate Guidelines Network (SIGN). Search filters. http://www.sign.ac.uk/methodology/filters.html#random (accessed 8 April 2009).
Sondenaa 1995
- Sondenaa K. Andersen E. Nesvik I. Soreide JA. Patient characteristics and symptoms in chronic pilonidal sinus disease. International Journal of Colorectal Disease 1995;10(1):39‐42. [DOI] [PubMed] [Google Scholar]
Wood 2008
- Wood L, Egger M, Gluud LL, Schulz K, Juni P, Altman DG, et al. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta‐epidemiological study. BMJ 2008;336:601‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
McCallum 2008
- McCallum IJ, King PM, Bruce J. Healing by primary closure versus open healing after surgery for pilonidal sinus: systematic review and meta‐analysis. BMJ 2008;336(7649):868‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]


