Abstract
Objectives:
Missing teeth are routinely replaced with fixed dental prostheses (FDPs); thus, knowing the patient’s oral health–related quality of life (OHRQoL) after placement of FDP and factors affecting their quality of life in addition to their oral hygiene practices is important. This study aimed to measure OHRQoL with FDPs and oral hygiene practices of adults in Riyadh, Saudi Arabia.
Materials and Methods:
A survey was distributed in hard and soft copy forms. Target subjects were adults older than 18 years with FDP and living in Riyadh. The questionnaire contained four domains: demographic data, medical history, characteristics of the prostheses and oral hygiene practices, and Oral Health Impact Profile (OHIP)-14 questionnaire, which measures OHRQoL.
Results:
The study included 528 subjects. More than half of the participants (56.6%) had poor OHRQoL, which was associated with female gender, full-time employment, and low income. The presence of toothache, periodontal diseases, oral abscess, and broken teeth were all associated with poor OHRQoL. Participants with diabetes were also found to have poor OHRQoL. As for oral hygiene practices, 47% of subjects did not receive oral hygiene instructions after the placement of their FDP. It was also found that 53.4% of the study population brush only once daily.
Conclusion:
Many factors can have an influence on OHRQoL. Both dentist and patient awareness regarding postoperative oral hygiene instructions should be increased to ensure the durability of the prosthodontic appliances and improve patients’ OHRQoL.
Keywords: Fixed dental prostheses, oral hygiene practice, quality of life
Introduction
Fixed dental prostheses (FDPs) have been widely used for years.[1] Many studies have investigated the influence of FDP on the oral health.[2,3,4] It was found that despite the use of favorable mechanical design and biological material, dental plaque, and consequently, gingival inflammation will occur if proper oral hygiene measures were not applied.[5,6] It was found that the most common cause of single unit FDP failure was caries, which might be attributed to lack of good oral hygiene.[7] Achieving good plaque control requires individuals to comply and adhere to oral hygiene measures.[8] Frequent patients’ education and routine dental visits can motivate them and improve their oral health.[9]
Oral health is an integral part of the individual’s overall well-being, and it significantly affects the quality of life.[10] The World Health Organization defines oral health as “… a state of being free from any diseases and disorders that limit an individual’s capacity in biting, chewing, smiling, speaking, and psychosocial well-being.”[10] Therefore, the oral health–related quality of life (OHRQoL) is an important component of the quality of life, and multiple studies have shown its significance.[11,12] The OHRQoL is a multidimensional construct that includes physical, cognitive, emotional, and social aspects. Using the OHRQoL as an adjunctive method to define treatment outcomes instead of using the traditional criteria allows for a more comprehensive assessment that takes into consideration the social and emotional experience of the individual as well as physical functioning.[12,13] One of the most widely used instruments to assess the impact of oral health is the Oral Health Impact Profile (OHIP), which was proposed by Slade and Spencer[14] in 1994. The questionnaire studies four dimensions, which are oral function, orofacial pain, orofacial appearance, and psychosocial impact.[14]
There is a big gap in the literature regarding FDP epidemiology in terms of demographics, clinical characteristics, and patients’ OHRQoL with FDPs. Most studies focused on a specific type of prostheses and measured patients’ OHRQoL in relation to that specific type.[15,16] In addition, most studies in the literature did not explore the effect of oral hygiene practices of patients concerning FDP despite its significance.[15,16,17] Therefore, this study aimed to assess the OHRQoL of adults in Saudi Arabia about FDP to have an idea about the outcomes of this treatment modality and to identify oral hygiene practices to spot any relation between the two.
Materials and Methods
This is a cross-sectional observational analytical study of the relationship between quality of life and oral hygiene practice to the type of FDPs among adults in Riyadh, Saudi Arabia. The ethical approval was obtained from the institutional review board committee at King Abdullah International Medical Research Center, (RYD-18-419812-177162) before the study. The sample size was calculated by online sample size calculator for confidence level of 0.95% and confidence interval of 5 for Riyadh population. The sample size needed for this study was 350 participants.
The study was conducted using a self-administered, close-ended questionnaire. The questionnaire consisted of the following sections: first, sociodemographic data including gender, age, nationality, marital status, level of education, employment status, and family income. Second, the medical history of the participants such as the presence of any systemic conditions, habits such as smoking or tobacco use, and dental history such as the presence of toothache. Third, clinical information regarding the FDPs such as the duration of placement of most recent prosthesis, and information on oral hygiene practices such as the use of toothbrush, dental floss, and others, and frequency of their usage, and whether the participants received postoperative oral hygiene instruction or not. Fourth, the participants’ quality of life in relation to FDPs using OHIP-14 questionnaire, which is a validated questionnaire.[18] Respondents were asked to indicate on a four-point Likert scale how frequently they experienced each problem. OHIP had 14 questions divided into seven sections: functional section, physical pain section, psychological discomfort section, psychological disability section, handicap section, physical disability section, and social disability section. Each section, evaluating a particular component, had two questions (where the minimum score is 0, which means no impact on the quality of life, and the maximum score is 1, which means some impact on the quality of life). The overall score was calculated and graded on a two-point scale. Then, group I (0–6) scores were considered as a good quality of life, whereas group II (7–14) scores were considered as poor quality of life.
The data were collected by using both hard and electronic copy, and a consent form was provided as the first page of the questionnaire. The hard copy was distributed in both Arabic and English languages among patients attending King Abdulaziz Medical City outpatient dental clinics and King Saud bin Abdulaziz University for Health Sciences dental clinics. A soft copy was created using Google Forms (Google Forms, 2018; a free web-based survey generator). In the electronic form, the questions and options were kept as they were in the paper format to maintain the questionnaire integrity. The electronic questionnaire was distributed through social media platforms (Twitter and WhatsApp). Target subjects based on the inclusion criteria were all adults older than 18 years with FDP and living in the Riyadh region.
Statistical analysis: The data received were transferred in an Excel sheet, then coded and analyzed using IBM Statistical Package for the Social Sciences software, version 22.0 (IBM, Armonk, New York). Statistical analysis was descriptive statistics including numbers and percentages to compare the OHIP-14 and sociodemographic, medical history, oral hygiene practices, and clinical information regarding the fixed prostheses. Chi-square test was used to assess the relationship between other categorical parameters of demographic data, oral hygiene practice, and clinical information of the fixed prostheses in comparison to OHIP-14. All statistical tests were declared significant at a P value of 5% (0.05) (α value) or less along with confidence interval of 95% and a β value of 0.2.
Results
A total of 631 subjects participated in this study. After applying the inclusion and exclusion criteria, the total sample size was found to be 528 subjects.
The demographic data of the participants are presented in Table 1. In the sample, 43.4% (229) participants had good OHRQoL, whereas 56.6% (299) participants had poor OHRQoL. Table 2 shows the relationship between demographic characteristics and OHIP. An association was found between OHIP and gender where 84.6% of females and 15.4% of males had poor OHRQoL. Moreover, occupation appeared to play an important role in determining the quality of life. Full-time employees had higher OHIP scores indicating poor OHRQoL when compared to part-time employees. Another factor was family income where it was found that participants in the higher income group (>20,200 SR) had good OHRQoL when compared to the lower income group. Other demographic factors showed no significant relation with OHIP.
Table 1:
Demographic data
| Variables | Frequency | Valid percent | |
|---|---|---|---|
| Gender | Male | 102 | 19.3 |
| Female | 426 | 80.7 | |
| Total | 528 | 100.0 | |
| Age (in years) | <40 | 255 | 48.3 |
| 41–55 | 226 | 42.8 | |
| >56 | 47 | 8.9 | |
| Total | 528 | 100.0 | |
| Nationality | Saudi | 513 | 97.2 |
| Non-Saudi | 15 | 2.8 | |
| Total | 528 | 100.0 | |
| Social status | Single | 87 | 16.5 |
| Married | 405 | 76.7 | |
| Divorced | 17 | 3.2 | |
| Widow | 19 | 3.6 | |
| Total | 528 | 100.0 | |
| Education | Less HS | 29 | 5.6 |
| HS | 82 | 15.7 | |
| Bachelor’s | 307 | 58.8 | |
| More than bachelor’s | 104 | 19.9 | |
| Total | 522 | 100.0 | |
| Occupation | Employed FT | 257 | 48.8 |
| Employed PT | 19 | 3.6 | |
| Retired | 82 | 15.6 | |
| Not employed | 142 | 26.9 | |
| Student | 27 | 5.1 | |
| Total | 527 | 100.0 | |
| Family income | 0–8,699 SR | 103 | 19.7 |
| 8,700–11,999 SR | 60 | 11.5 | |
| 12,000–15,299 SR | 111 | 21.2 | |
| 15,300–20,159 SR | 106 | 20.2 | |
| >20,200 SR | 144 | 27.5 | |
| Total | 524 | 100.0 | |
| Total | 528 | 100.0 | |
HS = high school, FT = full time, PT = part time
Table 2:
Relationship between demographic characteristic and Oral Health Impact Profile (expressed as N [%])
| S. no. | Variable | Category | Good OHIP |
Poor OHIP |
Total | % | P value | ||
|---|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | ||||||
| 1. | Gender | Male | 56 | 24.5 | 46 | 15.4 | 102 | 19.3 | 0.009 |
| Female | 173 | 75.5 | 253 | 84.6 | 426 | 80.7 | |||
| 2. | Age | ≤40 years | 104 | 45.4 | 151 | 50.5 | 255 | 48.3 | 0.10 |
| 41–55 years | 98 | 42.8 | 128 | 42.8 | 226 | 42.8 | |||
| ≥56 years | 27 | 11.2 | 20 | 6.7 | 46 | 8.9 | |||
| 3. | Nationality | Saudi | 221 | 96.5 | 292 | 97.7 | 513 | 97.2 | 0.430 |
| Non-Saudi | 8 | 3.5 | 7 | 2.3 | 15 | 2.8 | |||
| 4. | Marital status | Single | 47 | 20.5 | 40 | 13.4 | 87 | 16.5 | 0.186 |
| Married | 167 | 72.9 | 238 | 79.6 | 405 | 79.7 | |||
| Divorced | 7 | 3.1 | 10 | 3.3 | 17 | 3.2 | |||
| Widow | 8 | 3.5 | 11 | 3.7 | 19 | 3.6 | |||
| 5. | Occupation | Employee (full time) | 103 | 45 | 155 | 51.8 | 258 | 48.9 | 0.010 |
| Employee (part time) | 6 | 2.6 | 13 | 4.3 | 19 | 3.6 | |||
| Retired | 45 | 19.7 | 37 | 12.4 | 82 | 15.5 | |||
| Unemployed | 57 | 24.9 | 85 | 28.4 | 142 | 26.9 | |||
| Student | 18 | 7.9 | 9 | 3 | 27 | 5.1 | |||
| 6. | Education | Less than high school | 13 | 5.7 | 16 | 5.4 | 29 | 5.5 | 0.802 |
| High school | 37 | 16.2 | 47 | 15.7 | 84 | 15.9 | |||
| Graduate | 129 | 56.3 | 180 | 60.2 | 309 | 58.5 | |||
| More than graduate | 50 | 21.8 | 56 | 18.7 | 106 | 20.1 | |||
| 7. | Income | 0–8,699 SR | 34 | 14.8 | 69 | 23.1 | 103 | 19.5 | 0.000 |
| 8,700–11,999 SR | 25 | 10.5 | 38 | 12.7 | 62 | 11.7 | |||
| 12,000–15,299 SR | 37 | 16.2 | 75 | 25.1 | 112 | 21.2 | |||
| 15,300–20,159 SR | 52 | 22.7 | 54 | 18.1 | 106 | 20.1 | |||
| >20,200 SR | 82 | 35.8 | 63 | 21.1 | 145 | 27.5 | |||
OHIP = Oral Health Impact Profile
Table 3 shows the relationship between clinical characteristics and OHIP. A significant association was found between OHRQoL and toothache, periodontal diseases, and oral abscess; in which, 71.28%, 70.05%, and 75.67% of the participants who reported to have toothache, periodontal diseases, and oral abscess, respectively, were also found to have poor OHRQoL.
Table 3:
Relationship between clinical characteristics and Oral Health Impact Profile (expressed as N [%])
| S. no. | Category | Variable | Category | Good OHIP |
Poor OHIP |
Total | P value | ||
|---|---|---|---|---|---|---|---|---|---|
| Number | % | Number | % | ||||||
| 1. | Do you currently have a toothache? | Yes | 56 | 24.5 | 139 | 46.5 | 195 | 0.000 | |
| 28.71 | 71.28 | ||||||||
| No | 173 | 75.5 | 160 | 53.5 | 333 | ||||
| 51.95 | 48.04 | ||||||||
| 2. | Duration of placement of most recent prosthesis? | Less than 1 Year |
52 | 22.7 | 80 | 26.8 | 132 | 0.216 | |
| 39.39 | 60.60 | ||||||||
| 1–5 years | 129 | 56.3 | 167 | 55.9 | 296 | ||||
| 43.58 | 56.41 | ||||||||
| 5–10 years | 18 | 7.9 | 28 | 9.4 | 46 | ||||
| 39.13 | 60.86 | ||||||||
| More than 10 years | 30 | 13.8 | 24 | 8 | 54 | ||||
| 55.55 | 44.44 | ||||||||
| 3. | Have you diagnosed with periodontal diseases? | Yes | 59 | 25.8 | 138 | 46.2 | 197 | 0.000 | |
| 29.94 | 70.05 | ||||||||
| No | 170 | 74.2 | 161 | 53.8 | 331 | ||||
| 51.35 | 48.64 | ||||||||
| 4. | Have you diagnosed with an oral abscess? | Yes | 18 | 7.9 | 56 | 18.7 | 74 | 0.000 | |
| 24.32 | 75.67 | ||||||||
| No | 211 | 92.1 | 243 | 81.3 | 454 | ||||
| 46.47 | 53.52 | ||||||||
| 5. | Do you have at least one broken tooth? | Yes | 81 | 35.4 | 156 | 52.2 | 237 | 0.000 | |
| 34.17 | 65.82 | ||||||||
| No | 148 | 64.6 | 143 | 47.8 | 291 | ||||
| 50.85 | 49.14 | ||||||||
Table 4 shows the relation between OHIP and systemic factors affecting the FDP. It was found that 70.7% of participants with diabetes had poor OHRQoL.
Table 4:
Relationship between systemic factors and Oral Health Impact Profile (expressed as N [%])
| S. no. | Variable | Category | Good OHIP |
Poor OHIP |
Total | P value | ||
|---|---|---|---|---|---|---|---|---|
| Number | % | Number | % | |||||
| 1. | What is your current smoking/tobacco use status? | Current smoker: more than one pack of cigarettes per day | 2 | 0.9 | 3 | 1 | 5 | |
| 40 | 60 | |||||||
| Current smoker: one or less pack of cigarettes per day | 8 | 3.5 | 8 | 2.7 | 16 | |||
| 50 | 50 | 0.933 | ||||||
| Current smoker: hookah | 8 | 3.5 | 14 | 4.7 | 22 | |||
| 36.36 | 63.636 | |||||||
| Past user of tobacco products | 8 | 3.5 | 9 | 3 | 17 | |||
| 47.05 | 52.94 | |||||||
| Never used tobacco products | 203 | 88.6 | 265 | 88.6 | 468 | |||
| 43.37 | 56.62 | |||||||
| 2. | Are you diagnosed with diabetes? | Yes | 22 | 9.6 | 53 | 17.7 | 75 | 0.008 |
| 29.33 | 70.66 | |||||||
| No | 207 | 90.4 | 256 | 82.3 | 453 | |||
| 45.69 | 56.51 | |||||||
| 3. | Are you diagnosed with hypertension? | Yes | 37 | 41.9 | 69 | 40.8 | 106 | 0.049 |
| 34.9 | 65.09 | |||||||
| No | 192 | 58.1 | 230 | 59.2 | 422 | |||
| 45.49 | 54.5 | |||||||
| 4. | Do you have any other systemic condition? | Yes | 52 | 22.7 | 66 | 22.1 | 118 | 0.862 |
| 44.06 | 55.93 | |||||||
| No | 177 | 77.3 | 233 | 77.9 | 410 | |||
| 43.17 | 56.83 | |||||||
OHIP = Oral Health Impact Profile
Approximately 47% of participants reported not receiving oral hygiene instructions after placement of their FDP. Participants who were instructed by their dentists about FDP maintenance and oral hygiene practice (54.6%) had higher percentage of good OHIP compared to those who did not receive any instructions; however the difference was not statistically significant.
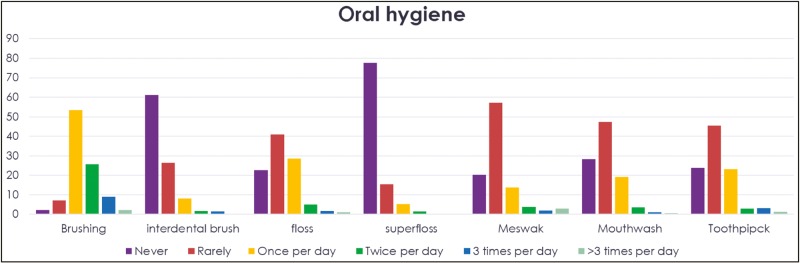
Figure 1 presents frequency distribution showing descriptive and inferential analysis of oral hygiene–related variables in the sample where it was found that most of the participants brush once daily (53.4%).
Figure 1:
Frequency of using oral hygiene aids among participants
Discussion
A significant association was found between OHRQoL and gender, where females had poor OHRQoL when compared to males. This could be explained by higher expectations and demands in females in comparison to males. On the contrary, Singh[19] found that there was no significant difference in FDP-related satisfaction levels between males and females in their sample.
In addition, occupation plays an important role in the OHRQoL. It was found that full-time employees had poor OHRQoL when compared to unemployed participants and students. No previous studies reported an association between occupation and OHRQoL; therefore, more studies are required to investigate this relation. Nevertheless, this could be explained by the busier schedules of full-time employees, which might lead to less attention to their oral health. Full-time employees must be educated through lectures and seminars provided at the workplace about the importance of oral hygiene and its effect on their lives. In addition, insurance, which includes preventive dental treatment, should be provided by their employers.
Another factor affecting OHRQoL was family income. It was found that participants with the income of 20,200 SR and higher had better OHRQoL. Studies with financial view indicated that FDPs are cost-effective.[20] This might suggest that higher income participants were able to afford better quality of FDP, which led to better OHRQoL. On the contrary, age, nationality, social status, and level of education showed no significant association, which is in agreement with a study conducted by Fischer et al.,[21] whereas Motallebnejad et al.[22] found that subjects with academic education had better oral health status due to the higher cultural level and better care of oral health. Goiato et al.[23] mentioned that there was an association between OHRQoL and social status, in which married people were more concerned about their FDP, suggesting that married people differ in their social attitudes. The association that was found between the demographic data and OHRQoL signifies the importance of keeping patient individualities in mind while deciding on a treatment plan.
In this study, toothache was related to poor OHRQoL. Similarly, Fischer et al.[21] found that pain had the biggest influence on the OHRQoL. Moreover, 70% of the participants with periodontal diseases and 75.7% of the participants with oral abscess had significantly less OHRQoL. Periodontal diseases and dental abscess are related to plaque and poor oral hygiene, which will affect the FDP in many ways, leading to poor OHRQoL; however, no other studies investigated this relation.
When linking OHRQoL with systemic factors, diabetes was found to be related with poor OHRQoL. In a study conducted by Pretnar et al.,[24] it was concluded that systemic diseases including diabetes and hypertension did not significantly affect the OHRQoL.
In this study, it was found that 47% of the participants denied receiving oral hygiene instructions after placement of their FDP. Although this was considered a large number, it was still less than what was found by other studies. For example, Geiballa et al.[25] found that 91.1% of their sample claimed that they did not receive oral hygiene instructions.
This study found that brushing was the most commonly used method for teeth cleaning, but most of the participants brushed their teeth only once a day. Furthermore, most of the participants rarely used other oral hygiene aids such as dental floss, mouthwash, and interdental brush despite their importance for FDP. It was also found that majority of the participants never used superfloss, which is an essential element for maintaining FDP. It is extremely important to increase the awareness of the population regarding oral hygiene practices to reduce the burden of oral diseases and to promote oral health. Therefore, giving postoperative instructions should be emphasized among practitioners to increase the life span of these prostheses and to improve patients’ OHRQoL. In addition, it was found that almost one-fifth of the participants did not attend any follow-up appointments. The long-term success of fixed prostheses was predominantly dependent on both the patient’s maintenance of effective home care of the health of the hard and soft tissues and on the dentists’ instructions and proper techniques.[26]
To the best of our knowledge, this was the first Saudi study to measure demographics, systemic diseases, oral hygiene practices, clinical characteristics of the prostheses, and follow-up appointments. In this cross-sectional study, OHIP questionnaire was not administered at various perception period difference (before and after placement of FDP), so the presence of other contributing factors such as price of treatment or procedural errors during fabrication and placement of the FDP cannot be excluded. Furthermore, the results of this study require a comparison with other studies on a different population to construct certain authentic and universal guidelines.
Conclusion
The results of this study showed that more than half of the study population had poor OHRQoL. Oral health status as well as systemic diseases had negatively affected patients’ quality of life. When fabricating FDP, it is essential for the success of the fixed prostheses to eliminate deteriorating oral factors. The medical condition of the patient should be kept under control for the general health of the patient and the success of dental treatment. One main finding of the study was that despite the importance of oral hygiene instructions after prostheses placement, large number of patients did not receive them; therefore, dentists’ awareness regarding providing postoperative instructions should be emphasized more to ensure the durability of the prosthodontic appliances and to improve patients’ OHRQoL. Practitioners should emphasize on the oral hygiene instructions and keep patients motivated.
Financial disclosure
This study was self-funded by the authors, with no source of funding to declare.
Conflict of interest:
There is no conflict of interest to declare.
Author contributions
All authors had contributed to study conception, data collection, data acquisition and analysis, data interpretation and manuscript writing. All the authors approved the final version of the manuscript for publication.
Ethical policy and institutional review board statement
The Institutional Review Board approval was obtained from King Abdullah International Medical Research Center, Riyadh, Kingdom of Saudi Arabia with IRB office reference number: IRBC/1894/18 in 25 October 2018.
Patient declaration of consent
Informed written consent forms were distributed to the participants asking their permission to be part of the study and publication of the data for research and educational purposes.
Data availability statement
The data that support the findings of this study are available on request from the author Raneem Bin Nafesah (Ralnafisa@gmail.com).
Acknowledgements
There are no non-author contributors. All contributions were done by the authors.
References
- 1.Kern J, Kern T, Wolfart S, Heussen N. A systematic review and meta-analysis of removable and fixed implant-supported prostheses in edentulous jaws: Post-loading implant loss. Clin Oral Implants Res. 2016;27:174–95. doi: 10.1111/clr.12531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Silness J, Gustavsen F, Mangersnes K. The relationship between pontic hygiene and mucosal inflammation in fixed bridge recipients. J Periodontal Res. 1982;17:434–9. doi: 10.1111/j.1600-0765.1982.tb01174.x. [DOI] [PubMed] [Google Scholar]
- 3.Kc Basnyat S, Sapkota B, Shrestha S. Oral hygiene and gingival health in patients with fixed prosthodontic appliances—A six month follow-up. Kathmandu Univ Med J (KUMJ) 2015;13:328–32. doi: 10.3126/kumj.v13i4.16832. [DOI] [PubMed] [Google Scholar]
- 4.Silness J, Ohm E. Periodontal conditions in patients treated with dental bridges. V. Effects of splinting adjacent abutment teeth. J Periodontal Res. 1974;9:121–6. doi: 10.1111/j.1600-0765.1974.tb00663.x. [DOI] [PubMed] [Google Scholar]
- 5.Valderhaug J, Heloe LA. Oral hygiene in a group of supervised patients with fixed prostheses. J Periodontol. 1977;48:221–4. doi: 10.1902/jop.1977.48.4.221. [DOI] [PubMed] [Google Scholar]
- 6.Tolboe H, Isidor F, Budtz-Jörgensen E, Kaaber S. Influence of oral hygiene on the mucosal conditions beneath bridge pontics. Scand J Dent Res. 1987;95:475–82. doi: 10.1111/j.1600-0722.1987.tb01963.x. [DOI] [PubMed] [Google Scholar]
- 7.Al Refai R, Saker S. Clinical and radiographic assessment of reasons for replacement of metal-ceramic fixed dental prostheses in patients referring to dental school. J Clin Exp Dent. 2018;10:e75–80. doi: 10.4317/jced.53850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ramsay DS. Patient compliance with oral hygiene regimens: A behavioural self-regulation analysis with implications for technology. Int Dent J Suppl Creating A Successful. 2000:304–11. doi: 10.1111/j.1875-595x.2000.tb00580.x. [DOI] [PubMed] [Google Scholar]
- 9.de Carvalho VF, Okuda OS, Bernardo CC, Pannuti CM, Georgetti MA, De Micheli G, et al. Compliance improvement in periodontal maintenance. J Appl Oral Sci. 2010;18:215–9. doi: 10.1590/S1678-77572010000300003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Petersen PE. The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century—The approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 2003;31:3–24. doi: 10.1046/j..2003.com122.x. [DOI] [PubMed] [Google Scholar]
- 11.Sischo L, Broder HL. Oral health-related quality of life: What, why, how, and future implications. J Dent Res. 2011;90:1264–70. doi: 10.1177/0022034511399918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bennadi D, Reddy CV. Oral health related quality of life. J Int Soc Prev Community Dent. 2013;3:1–6. doi: 10.4103/2231-0762.115700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Christie MJ, French D, Sowden A, West A. Development of child-centered disease-specific questionnaires for living with asthma. Psychosom Med. 1993;55:541–8. doi: 10.1097/00006842-199311000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- 15.Sato N, Koyama S, Mito T, Izumita K, Ishiko R, Yamauchi K, et al. Changes in oral health-related quality of life after oral rehabilitation with dental implants in patients following mandibular tumor resection. J Oral Sci. 2019;61:406–11. doi: 10.2334/josnusd.18-0234. [DOI] [PubMed] [Google Scholar]
- 16.AlZarea BK. Oral health related quality-of-life outcomes of partially edentulous patients treated with implant-supported single crowns or fixed partial dentures. J Clin Exp Dent. 2017;9:e666–71. doi: 10.4317/jced.53661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Filius MAP, Vissink A, Cune MS, Raghoebar GM, Visser A. Effect of implant therapy on oral health-related quality of life (OHIP-49), health status (SF-36), and satisfaction of patients with several agenetic teeth: Prospective cohort study. Clin Implant Dent Relat Res. 2018;20:592–7. doi: 10.1111/cid.12625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25:284–90. doi: 10.1111/j.1600-0528.1997.tb00941.x. [DOI] [PubMed] [Google Scholar]
- 19.Singh RK. A survey based evaluation and assessment of satisfaction and continuance of patients wearing fixed partial dentures. Int J Med Health Res. 2017;3:34–7. [Google Scholar]
- 20.Zou Y, Zhan D. Personal factors determining patient satisfaction with all-ceramic crown treatment for single anterior teeth. Int J Prosthodont. 2016;29:482–3. doi: 10.11607/ijp.4675. [DOI] [PubMed] [Google Scholar]
- 21.Fischer KR, Lindner I, Fickl S. Implant treatment in periodontally compromised subjects—Quality of life and patient satisfaction. Clin Oral Investig. 2016;20:697–702. doi: 10.1007/s00784-015-1561-x. [DOI] [PubMed] [Google Scholar]
- 22.Motallebnejad M, Mehdizadeh S, Najafi N, Sayyadi F. The evaluation of oral health-related factors on the quality of life of the elderly in Babol. Contemp Clin Dent. 2015;6:313–7. doi: 10.4103/0976-237X.161867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goiato MC, Torcato LB, Dos Santos DM, Moreno A, Antenucci RM, de Carvalho Dekon SF. Quality of life and satisfaction of patients wearing implant-supported fixed partial denture: A cross-sectional survey of patients from Araçatuba city, Brazil. Clin Oral Implants Res. 2015;26:701–8. doi: 10.1111/clr.12372. [DOI] [PubMed] [Google Scholar]
- 24.Pretnar T, Hren NI, Rener-Sitar K. Impact of systemic diseases on oral health related quality of life after implant-prosthodontic rehabilitation. Zdravniški Vestnik. 2014;83:436–45. [Google Scholar]
- 25.Geiballa GH, Abubakr NH, Ibrahim YE. Patients’ satisfaction and maintenance of fixed partial denture. Eur J Dent. 2016;10:250–3. doi: 10.4103/1305-7456.178313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ahuja S, Wicks R, Selecman A. Fabrication of new restorations with a consideration of oral hygiene. J Indian Prosthodont Soc. 2016;16:307–10. doi: 10.4103/0972-4052.158084. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the author Raneem Bin Nafesah (Ralnafisa@gmail.com).