Abstract
BACKGROUND AND PURPOSE: Thallium-201 single-photon emission computed tomography (SPECT) can be used to detect primary squamous cell carcinoma (SCCA) of the head and neck. Nevertheless, there have very few studies performed to evaluate the ability of thallium-201 to depict recurrent SCCA. The purpose of this study was to compare the ability of thallium-201 SPECT with CT to enable detection of recurrent SCCA of the upper aerodigestive tract.
METHODS: Thirty-three patients with a history of previously treated SCCA of the extracranial head and neck underwent thallium-201 SPECT imaging and contrast-enhanced CT. A neuroradiologist and nuclear medicine physician with knowledge of the primary site evaluated all thallium-201 studies for abnormal radiotracer uptake at the primary site. These results were correlated with histologic findings and clinical follow-up in all patients. All patients were followed up for a minimum of 2 years after completion of treatment. The McNemar test was used to determine statistical significance.
RESULTS: The diagnostic accuracy of thallium-201 SPECT was as follows: sensitivity, 88%; specificity, 94%; positive predictive value, 93%; and negative predictive value, 89%. The diagnostic accuracy of CT was as follows: sensitivity, 100%; specificity, 24%; positive predictive value, 55%; and negative predictive value, 100%. The diagnostic accuracy of thallium was superior to CT (P = .01).
CONCLUSION: Thallium-201 SPECT is superior to CT for differentiating recurrent tumor from post-treatment changes and may complement CT in the evaluation of previously treated SCCA of the extracranial head and neck.
One of the most challenging issues faced by clinicians and radiologists is the detection of recurrent tumor that has been treated previously for head and neck squamous cell carcinoma (HNSCCA). Surgery results in scarring and fibrosis that prevent complete evaluation of the primary site for recurrent tumor. This task is made more difficult if a reconstructive flap is used. In such patients, recurrences are often located deep to the flap and cannot be easily palpated. These anatomic distortions also compromise the ability of CT and MR imaging to depict early recurrence (1). Radiation therapy results in an inflammatory response (granulation tissue) in the tumor bed (2–4). In most sites, this inflammatory response progresses to fibrosis (scarring) within 3 to 4 months after completion of radiation therapy (2–4). An inflammatory response that occurs prior to scar formation is indistinguishable from tumor by imaging (5–8). The only findings diagnostic of recurrent tumor on CT or MR scans are: 1) presence of a focal mass in the location of a treated primary site; 2) lymph node metastases; 3) interval growth of a focal mass; or all three. Chemotherapy causes mucositis, erythema, and induration. Chemotherapy–associated changes also prevent thorough endoscopic evaluation and reduce the ability to detect accurately mucosal or submucosal tumor unresponsive to therapy (5, 6).
Accurate assessment of the status of a treated tumor is important, as early identification of recurrent HNSCCA increases the chances of successful salvage therapy. A delay in diagnosis allows tumors to enlarge and become incurable at the time of presentation (5, 6). Prompt detection may permit earlier salvage of small recurrences that might be unresectable when diagnosed at a more advanced stage (5, 6). An imaging technique that depicts accurately early recurrences has a potential to reduce patient morbidity and mortality.
Thallium-201 single-photon emission computed tomography (thallium-201 SPECT) has gained acceptance for detecting a variety of malignant tumors (9–13). Several investigators have studied the ability of thallium-201 SPECT to depict HNSCCA (14–18). Results suggest that HNSCCA is thallium-avid, and that thallium-201 SPECT accurately localizes the primary site prior to treatment as well as reveals clinically occult tumors (14–18). The degree of thallium uptake on pretreatment imaging also may be predictive of tumor response to nonsurgical organ preservation therapy (16). The purpose of our study was to determine if thallium-201 SPECT improves the diagnostic accuracy of differentiating recurrent HNSCCA from post-treatment changes as compared to CT findings. CT continues to be the preferred cross-sectional technique for evaluating recurrent tumor at many institutions because of its lower cost and easier access as compared with other imaging alternatives. Overall patient compliance is also better with spiral CT owing to shorter scan time (1 to 2 minutes) as opposed to the time required for MR imaging (30 to 45 minutes).
Methods
This is a prospective study that compared the ability of thallium-201 SPECT with that of CT for detecting recurrent HNSCCA. Thirty-three patients previously treated for HNSCCA underwent thallium-201 and contrast-enhanced CT. Patients were obtained from three institutions that performed thallium-201 SPECT to attempt to differentiate recurrent tumor from post-treatment changes (institution 1, 16 patients; institution 2, 11 patients; institution 3, 6 patients). All patients were treated with a combination of surgery, radiation therapy, and chemotherapy. The exact treatment regimen differed at each institution.
All patients had clinical symptoms of recurrent tumor at the primary site. The decision to image was made by the referring otolaryngology head and neck surgeon and was based on a combination of clinical symptoms and physical examination. Patient outcome was based on a combination of biopsy (n=16) and clinical follow-up (n=17). Presence of cervical lymph node metastases was not evaluated in this study.
All patients underwent contrast-enhanced CT and thallium-201 SPECT imaging. The interval between the two studies did not exceed 2 weeks. CT studies included contiguous sections (3-mm thickness, 16-cm field of view, and 512 × 512-mm matrix) obtained from the skull base to the thoracic inlet. CT studies were reconstructed in soft-tissue and bone algorithms. CT studies (primary site and nodes) were evaluated for the presence of recurrent tumor by one head and neck radiologist at the institution where the study was obtained. The imaging criteria used were the presence of a focal mass, asymmetric soft-tissue swelling, and distortion of the normal fascial planes. This radiologist was aware of the site of the primary tumor, and was asked to make a binary decision regarding whether the study was compatible with recurrent tumor at the primary site in a manner similar to Lapela et al (5).
Thallium-201 SPECT imaging was performed 10 minutes after the intravenous administration of 3 mCi of thallous chloride (half-life, 73 hours). Imaging was performed using multiheaded SPECT scanners equipped with low-energy all-purpose collimators. The type of scanner varied with each institution. Counts were collected over a 360° rotation with 128 stops at 10 seconds each. Images were reconstructed using a Butterworth filter with a cut-off frequency of 0.35 and an order of 9. The imaging matrix was 64 × 64 (6 mm per pixel). Images were oriented into 6-mm sections in transverse, coronal, and sagittal planes. Weighted planar reprojections (1 per exponential) of the SPECT data were created in multiple views (64 images). One nuclear medicine physician, at the institution where a study was performed, evaluated the thallium-201 SPECT studies for abnormal uptake, and was aware of primary tumor sites. This nuclear medicine physician was asked to make a binary decision as to whether or not the uptake at the known primary site was compatible with recurrent tumor. Asymmetric radiotracer uptake within the known primary site was interpreted as indicative of recurrent tumor. Quantitative analysis for distinguishing between post-treatment changes and recurrent tumor was not performed as part of this investigation (5, 19).
Results of the thallium-201 SPECT were recorded and compared with the CT interpretation. This information was conveyed to the referring otolaryngologist and the results were correlated with patient outcome. In this study, the readers were asked to make a binary decision as to whether or not the thallium-201 SPECT and CT studies were indicative of recurrent tumor at the primary site. A nonparametric grading scale (1+, no evidence of tumor; 2+, mild chance of tumor; 3+, equivocal; 4+, probable tumor; and 5+, definite tumor) was not used, as indeterminate interpretations would not benefit the otolaryngologist, radiation therapist, or medical oncologist. For these patients, the referring physicians were interested in the diagnostic accuracy of the study in determining whether or not tumor was present at the primary site.
The sensitivity, specificity, and positive and negative predictive values for identifying recurrent tumor were calculated for CT and thallium-201 SPECT. The McNemar test was used to compare directly the ability of the two diagnostic techniques to show recurrence.
Results
A summary of the results of the 33 patients who underwent both contrast-enhanced CT and thallium-201 SPECT is presented in Table 1. Twenty-six patients were men and seven were women. Average age of the patients was 60.1 years (range, 29–82 years).
TABLE 1:
Data summary
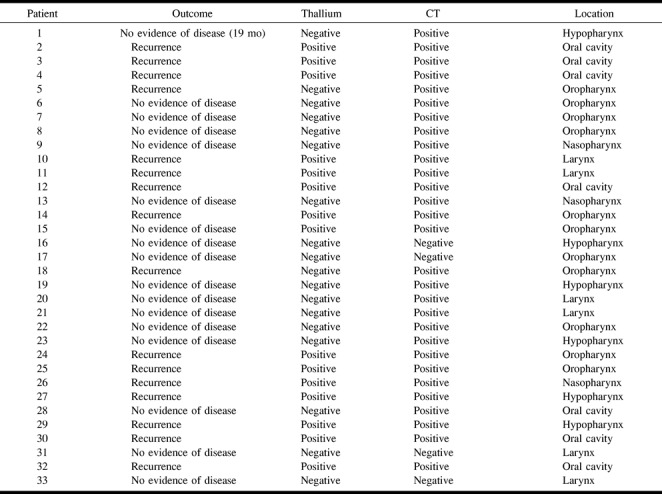
The primary tumor sites were as follows: oropharynx (n=11), oral cavity (n=7), hypopharynx (n=6), larynx (n=6), nasopharynx (n=3) (Table 1). Sixteen patients had histologically confirmed recurrent disease at the primary site. Seventeen patients had no evidence of disease based on clinical follow-up 2 years after completion of treatment. Sixteen of 17 patients who had no evidence of disease were followed up for 2 years after completion of treatment. One patient died of intercurrent disease 19 months after completion of treatment. Because there was no evidence of recurrent tumor at the primary site, this patient was categorized as having no evidence of disease.
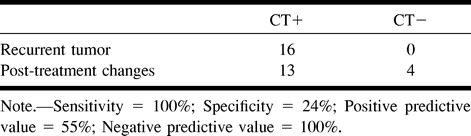
Results of CT for detection of recurrent tumor are summarized in Table 2. CT depicted all recurrent tumors (n=16), resulting in a sensitivity of 100%. Nevertheless, there were 13 false-positive studies. This resulted in a low specificity (24%) and positive predictive value (55%). CT findings were negative in four patients. None of these patients had recurrent tumor. Thus, there were no false-negative CT studies.
TABLE 2:
Diagnostic accuracy of CT for detecting recurrent tumor
Results of thallium-201 SPECT are summarized in Table 3. The average time between completion of treatment and thallium-201 SPECT was 6.4 months (range, 1.5–36 months). Thallium-201 SPECT accurately showed 14 of 16 recurrent tumors (Fig 1) and properly excluded disease in 16 of 17 patients (Fig 2). There were two false-negative studies and one false-positive study.
TABLE 3:
Diagnostic accuracy of thallium-201 SPECT for detecting recurrent tumor
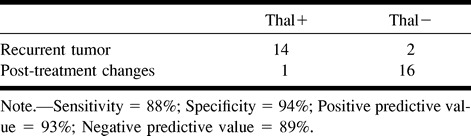
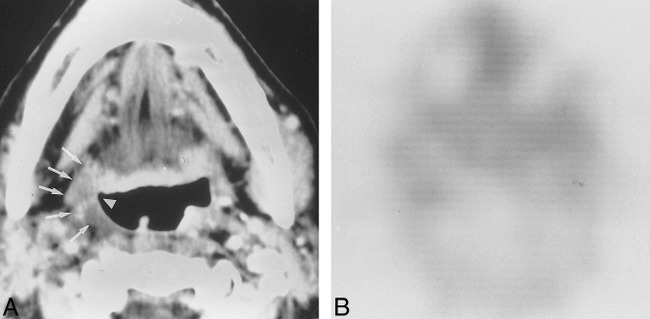
fig 1.
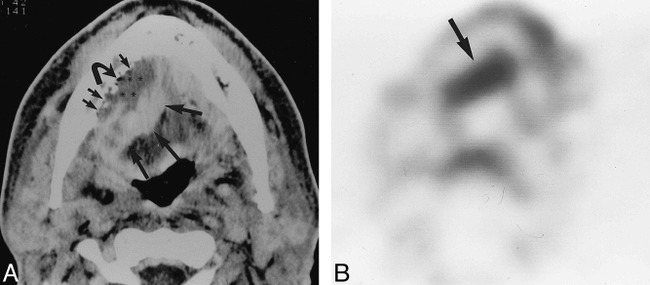
Correct identification of recurrent squamous cell carcinoma by Tl-201 SPECT.
A, Axial contrast-enhanced CT performed in a patient with a floor-of-mouth carcinoma 6 months after completion of combination radio- and chemotherapy. The study shows a heterogeneously enhancing mass that has soft-tissue (large straight arrows) and low-attenuation components (asterisk). Note erosion along the lingual cortex of the mandible (small straight arrows) and presence of gas (curved arrow). These findings were suspicious for recurrent tumor.
B, Axial thallium-201 SPECT obtained at the floor of mouth in the same patient illustrated in 1A. This study shows abnormal radiotracer uptake (arrow) in the region of the abnormality shown in 1A. Biopsy of this area revealed squamous cell carcinoma.
fig 2.
Correct exclusion of recurrent squamous cell carcinoma by Tl-201 SPECT.
A, Contrast-enhanced CT in a patient with a right-tonsil carcinoma previously treated with surgery and radiation therapy 14 months prior to this study. The patient presented with a right-sided nodal recurrence. This patient was a candidate for salvage surgery if no recurrent tumor was present at the primary site. Pretreatment studies were unavailable for comparison. CT shows an asymmetric soft-tissue mass involving the right tonsil (arrows). This is associated with asymmetry of the right glossotonsillar sulcus (arrowhead). Compare this to the normal appearance of the normal contralateral side.
B, Axial thallium-201 SPECT through the low oropharynx obtained in same patient illustrated in 2A shows no abnomal radiotracer uptake in the right tonsil. This patient has been followed up for over 2 years after completion of treatment and has no evidence of recurrent tumor at the primary site.
The McNemar test was used to compare sensitivity, specificity, and overall diagnostic accuracy of thallium-201 versus CT for properly distinguishing between recurrent tumor and post-treatment changes. CT and thallium-201 SPECT both had high sensitivity (100% and 88%, respectively) and negative predictive value (100% and 89%, respectively). CT revealed all 16 recurrent tumors, but because CT produced 12 more false-positive studies than thallium-201 SPECT, the specificity of CT was much lower than thallium-201 SPECT (24% vs 94%, respectively). The difference in sensitivity between CT and thallium-201 SPECT was not significant (P=.5); however, the specificity of thallium-201 SPECT was significantly higher than CT (P=.0005). As a result, the overall diagnostic accuracy of thallium-201 SPECT was superior to CT for detecting recurrent HNSCCA at the primary site (91% versus 61%, respectively; P=.01).
Discussion
Our results suggest that thallium-201 SPECT may help to differentiate recurrent HNSCCA from post-treatment changes at the primary site. It is commonly thought that the primary mechanism of thallium entry into the cell is linked to the sodium/potassium adenosinetriphosphatase (ATPase) pump in the cell membrane (9). This system actively transports potassium into the cell in exchange for sodium, thereby creating a high intracellular potassium concentration. Biologically, thallium is thought to act similarly to potassium and competes with potassium for intracellular transport across the cell membrane via the sodium/potassium ATPase system (9, 20–22). The reason for the elevated thallium-201 uptake in tumor has not been elucidated entirely, but is likely from the increased cellular proliferation of neoplastic cells as compared with adjacent normal tissue (9, 12, 13). Previous studies have suggested that areas of necrosis do not accumulate thallium-201 because of nonfunctioning of the ATPase cell membrane pump (12). This prevents active transport of thallium-201 into areas of necrosis. Thus, thallium-201 uptake appears to reflect the viability of the metabolic activity of tumor cells (12).
Our findings demonstrate that thallium-201 SPECT is more accurate than CT for distinguishing between tumor and non-neoplastic post-treatment changes. The difference in accuracy was based on the superior ability of thallium-201 SPECT to exclude tumor. Our results are consistent with those previously reported. Valdes-Olmes compared the effectiveness of thallium-201 SPECT with CT and MR imaging for detecting recurrent HNSCCA in 30 patients. They also reported a higher diagnostic accuracy for thallium-201 SPECT (sensitivity=93%, specificity=78%) when compared with CT/MR imaging (sensitivity=76%, specificity=30%) (18). The high sensitivity and low specificity of CT found in our study are also consistent with previous studies. Lapela et al reported CT findings with a sensitivity of 92% and a specificity of 50% for the detection of recurrent tumor (5).
We examined symptomatic patients who did not have prior cross-sectional imaging studies for comparison. It is highly likely that the diagnostic accuracy of CT would have been higher if the post-treatment studies could have been compared to baseline pretreatment CT (23). In our study, the majority of patients (n=31) did not have a pretreatment CT for comparison. Thus, our study was not intended to compare CT with thallium-201 SPECT for prospective treatment surveillance. Instead, we attempted to compare their abilities for assessing the difficult task of differentiating between recurrent tumor and post-treatment changes in symptomatic patients with distorted anatomy after treatment at one point in time.
The negative predictive value for CT was very high (100%). These findings indicate that CT is a reliable technique for excluding the presence tumor after treatment. Proper treatment surveillance with CT requires comparison of post-treatment imaging with a baseline pretreatment study. Complete radiographic response after treatment is indicative of local control (23). Further imaging surveillance may not be necessary for asymptomatic patients. Thallium-201 or other types of metabolic imaging may be helpful in patients with persistent residual masses present on post-treatment imaging or in patients who continue to be symptomatic but who have no residual disease detected on clinical exam or by imaging.
The high specificity of thallium-201 SPECT, compared with CT, help in the exclusion of tumor, and perhaps in avoidance of unnecessary biopsy. Our data suggest that thallium-201 SPECT may be used as an adjunct to CT for examining patients with previously treated HNSCCA who have suspicious CT findings but low clinical suspicion for recurrent tumor. Our results suggest that the high accuracy of a negative thallium-201 SPECT study may help prevent unnecessary biopsy in these patients. For patients presenting with clinical symptoms of recurrent tumor in whom CT findings are suspicious, biopsy of the suspicious region is desirable; the opportunity to perform surgical salvage may be lost if the diagnosis is delayed. Nonetheless, unnecessary biopsies should be avoided, if possible, as the trauma of multiple biopsies in irradiated tissues may result in a superimposed infection or perichondritis that may lead to frank cartilage necrosis, particularly in the larynx (4). Biopsy of necrotic tissue may cause these areas of necrosis to worsen and lead to a complete loss of function (4). Moreover, some biopsies require general anesthesia and, therefore, place a patient with an already compromised airway at greater risk. Risks are also increased with underlying cardiopulmonary disease, as is often the case with head and neck tumors. Additionally, false-negative biopsies may be attributed to sampling errors (5, 6). A negative biopsy result should be viewed with suspicion if there is a strong likelihood of recurrence on the basis of clinical or imaging findings. It is very likely that microscopic foci of tumor may not be revealed by thallium-201 SPECT, resulting in potentially false-negative studies. Thus, careful surveillance and repeat biopsies of the primary site may be necessary despite a negative thallium-201 SPECT study in patients who have a high clinical suspicion of recurrent HNSCCA.
The results of thallium-201 SPECT compare favorably with those previously reported for Technitium-99m-MIBI and 2-[F-18] fluoro-2-deoxy-D-glucose positron emission tomography (FDG PET) for differentiating recurrent HNSCCA from post-treatment changes (5, 6, 24, 25). Leitha at al reported a sensitivity and specificity of 95.3% and 78.4%, respectively, for the ability of Technitium-99m-MIBI to differentiate recurrent HNSCCA from post-treatment changes. (24) Fischbein et al reported a sensitivity and specificity of 100% and 64%, respectively, for the ability of FDG PET to distinguish properly between recurrent HNSCCA and nonmalignant post-therapy changes (25). Our investigation, coupled with other studies, suggests that thallium-201 SPECT may be an alternative form of metabolic imaging for detecting recurrent HNSCCA tumor at institutions where PET is not available (18). A direct comparison of thallium-201 SPECT and PET would be necessary, however, to compare properly the diagnostic accuracy of both techniques for detecting recurrent SCCA.
The primary disadvantage of thallium-201 imaging of the upper aerodigestive tract compared with FDG is the background uptake of thallium-201 by salivary and thyroid glands (14). Normal salivary gland activity has the potential to reduce the conspicuity of oral cavity and oropharynx tumors while thyroid uptake may reduce the ability to detect laryngeal tumors. This background thallium activity also may prevent identification of the full extent of primary tumor (14). In our series and those previously reported, the diagnostic accuracy of thallium-201 was not affected adversely by the normal background uptake. (18)
The registration between thallium-201 and CT was estimated by visual inspection. Automated or semiautomated techniques were not used in our study. Thus, there was no measure of the accuracy of our technique. Nonetheless, we found that the normal uptake in the parotid and submandibular gland was helpful in the attempt to identify the location of abnormal thallium-201 uptake. We believe that the diagnostic accuracy of thallium-201 may be improved further by SPECT/CT coregistration techniques. (24)
There are potential advantages of thallium-201 SPECT over FDG for imaging nasopharyngeal carcinoma and other skull base tumors. Unlike FDG, background uptake of thallium-201 by normal brain is low. Conspicuity of nasopharyngeal and skull base tumors may be reduced with FDG imaging, as these tumors are directly adjacent to normal brain FDG activity. Because of the low background activity of the normal brain, these tumors are well delineated with thallium-201 imaging. Our results also suggest that thallium-201 may be used to monitor response after completion of nonsurgical organ preservation therapy. FDG PET is unreliable for predicting treatment response when performed within 1 to 2 months after completion of radiation therapy. Greven et al reported a high incidence of false-negative studies when FDG PET was performed during this time interval (26). The cause of the false-negative studies is unknown but may arise from temporary cessation of glycolysis due to effects of radiation therapy. Thirteen of 33 patients in our study were imaged within 2 months after completion of radiation therapy. Six patients had uptake of tumor within the primary site and seven had no abnormal uptake. All six patients with persistent uptake had recurrent tumor at the primary site whereas the seven patients without uptake were controlled locally. Thus, our results suggest that thallium-201 may enable prediction of early primary site response.
It is true that thallium-201 SPECT imaging has lower resolution than can be achieved with FDG PET studies. Nevertheless, it should be noted that the degree of radiopharmaceutical uptake by the lesion and the resulting lesion-to-background contrast is especially critical in “hot spot” imaging; these factors may tend to offset the resolution disadvantage of thallium SPECT.
The studies in our series were qualitatively interpreted without the aid of quantification. Previous investigators have proposed that visual analysis of radionuclide images performed by experienced observers is sufficient for the detection of recurrent head and neck cancer (5, 18, 25). The use of visual analysis is further supported by the fact that HNSCCA has high thallium-201 uptake, as measured by quantitative methods (15, 16).
In summary, our results show that thallium-201 SPECT is more accurate than CT for differentiating recurrent HNSCCA from post-treatment changes. This diagnostic accuracy, combined with that found by other investigators, suggests that thallium-201 SPECT may be an alternative to FDG PET for detection of recurrent HNSCCA, using metabolic imaging with radiopharmaceuticals (5, 6, 18).
Footnotes
Address reprint requests to Suresh K. Mukherji, MD, Department of Radiology, 3324 Old Infirmary BC# 7510, University of North Carolina School of Medicine, Chapel Hill, NC 27599-7510.
References
- 1.Hudgins PA, Burson JG, Gussack GS, Grist WJ. CT and MR appearance of recurrent malignant head and neck neoplasms after resection and flap reconstruction. AJNR Am J Neuroradiol 1994;15:1689-1694 [PMC free article] [PubMed] [Google Scholar]
- 2.Manara M. Histologic changes of the human larynx irradiated with various technical therapeutic methods. Arch Ital Otolaryngol 1966;78:596-635 [PubMed] [Google Scholar]
- 3.Goldman JL, Cheren RV, Zak FG, et al. Hisopathology of larynges and radical neck specimens in combined radiation and surgery for advanced carcinoma of the larynx and hypopharynx. Ann Otol Rhinol Laryngol 1966;75:313-321 [Google Scholar]
- 4.Calcaterra TC, Stern F, Ward PH. Dilemma of delayed radiation injury of the larynx. Ann Otol Rhinol Laryngol 1972;81:501-507 [DOI] [PubMed] [Google Scholar]
- 5.Lapela M, Grenman R, Kurki T, et al. Head and neck cancer: detection of recurrence with PET and 2-[F-18]fluoro-2-deoxy-D-glucose. Radiology 1995;197:205-212 [DOI] [PubMed] [Google Scholar]
- 6.Anzai Y, Carroll WR, Quint DJ, et al. Recurrence of head and neck cancer after surgery or irradiation: prospective comparison of 2-deoxy-2-[F-18]fluoro-D-glucose PET and MR imaging diagnoses. Radiology 1996;200:135-141 [DOI] [PubMed] [Google Scholar]
- 7.Bronstein AD, Nyberg Schwartz AN, Shuman WP, Griffen BR. Soft tissue changes after head and neck radiation: CT findings. AJNR Am J Neuroradiol 1989;10:171-175 [PMC free article] [PubMed] [Google Scholar]
- 8.Glazer HS, Niemeyer JH, Balfe NM, et al. Neck neoplasms: mr imaging. II. posttreatment evaluation. Radiology 1986;160:349-354 [DOI] [PubMed] [Google Scholar]
- 9.Waxman A.D. Thallium-201 in nuclear oncology. In: Freeman LM, ed. Nuclear Medicine Annual 1991 New York: Raven Press, Ltd.; 1991;193-207
- 10.Carvalho PA, Schwartz RB, Alexander E, et al. Detection of recurrent gliomas with quantitative thallium-201/technitium-99m HMPAO single photon emission tomography. . J Neurosurg 1992;77:565-570 [DOI] [PubMed] [Google Scholar]
- 11.Schwartz RB, Caravalho PA, Alexander E, Loeffler JS, Folkherth R, Holman BL. Radiation necrosis vs high-grade recurrent glioma: differentiation by using dual-isotope SPECT with tl-201 and Tc-99m HMPAO. AJNR Am J Neuroradiol 1992;12:1187-1192 [PMC free article] [PubMed] [Google Scholar]
- 12.Elgazzar AH, Fernandez-ulloa , Silberstein EB. Tl-201 as a tumour-localizing agent: current status and future considerations. . Nucl Med Comm 1993;14:96-103 [DOI] [PubMed] [Google Scholar]
- 13.Ozcan Z, Burak Z, Ozcan C, et al. Is Tl-201 a reliable agent in tumour imaging? Nucl Med Comm 1996;17:805-809 [DOI] [PubMed] [Google Scholar]
- 14.Mukherji SK, Drane WE, Tart RP, Landau S, Mancuso AA. Comparison of thallium-201 and F-18 FDG SPECT uptake in squamous cell carcinoma of the head and neck. AJNR Am J Neuroradiol 1994;15:1837-1842 [PMC free article] [PubMed] [Google Scholar]
- 15.Nagamachi S, Hoshi H, Jinnouchi S, et al. Tl-201 SPECT for evaluating head and neck cancer. Ann Nucl Med 1996;10:105-111 [DOI] [PubMed] [Google Scholar]
- 16.Nagamachi S, Jinnouchi S, Flores LG, et al. The use of Tl-201 SPECT to predict the response to radiotherapy in patients with head and neck cancer. Nuc Med Comm 1996;17:935-942 [DOI] [PubMed] [Google Scholar]
- 17.Gregor T, Valdes-Olmes RA, Koops W, et al. Preliminary experience with thallous chloride Tl 201-labeled single photon emission computed tomography scanning in head and neck cancer. Arch Otolaryngol Head Neck Surg 1996;122:509-514 [DOI] [PubMed] [Google Scholar]
- 18.Valdes Olmos RA, Balm AJM, Hilgers FJM, et al. Tl-201 SPECT in the diagnosis of head and neck cancer. J Nucl Med 1997;38:873-879 [PubMed] [Google Scholar]
- 19.Mukherji SK, Drane WE, Mancuso AA, Parsons J, Mendenhall WM, Stringer SP. Occult primary tumors of the head and neck. Detection with 2-[F-18] fluoro-2-deoxy-D-glucose SPECT. Radiology 1996;199:761-766 [DOI] [PubMed] [Google Scholar]
- 20.Gehring PJ, Hammand PB. The interrelationship between thallium and potassium in animals. J Pharmacol Exp Ther 1967;155:187-201 [PubMed] [Google Scholar]
- 21.Lebowitz E, Greene MW, Greene R, et al. Thallium-201 for medical use I. J Nucl Med 1975;16:151-155 [PubMed] [Google Scholar]
- 22.Bradley-Moore PR, Lebowitz E, Greene MW, Atkins HL, Ansari AN. Thallium-201 for medical use II. biological behavior. J Nucl Med 1975;16:156-160 [PubMed] [Google Scholar]
- 23.Mukherji SK, Mancuso AA, Kotzur IM, Mendenhall W, Kubilis P, Lee R, Freeman D, Tart RP. Radiographic appearance of the irradiated larynx: part II: primary site response. Radiology 1994;193:149-154 [DOI] [PubMed] [Google Scholar]
- 24.Leitha T, Glaser C, Pruckmeyer M, et al. Technitium-99m-MIBI in primary and recurrent head and neck tumors: contribution of Bone SPECT image fusion. J Nucl Med 1998;39:1136-1171 [PubMed] [Google Scholar]
- 25.Fischbein NJ, Assar SA, Caputo GR, et al. Clinical utility of positron emission tomography with F-18 Fluorodeoxyglucose in detecting residual/recurrent squamous cell carcinoma of the head and neck. AJNR Am J Neuroradiol 1998;19:1189-1196 [PMC free article] [PubMed] [Google Scholar]
- 26.Greven KM, Williams DW, Keyes JW, et al. Distinguishing tumor recurrence from irradiation sequelae with positron emission tomography in patients treated for larynx cancer. Int J Radiation Oncology Biol Phys 1994;29:841-845 [DOI] [PubMed] [Google Scholar]


