Abstract
Summary: We report the CT and MR findings in two patients with multifocal meningioangiomatosis, neither of whom had a family history or stigmata of neurofibromatosis. All lesions were located in the cortical and subcortical areas and had round dense calcifications with eccentric cysts. The masses were associated with surrounding edema and gliosis.
Meningioangiomatosis is a rare, benign hamartomatous lesion found in the cerebral cortex and leptomeninges (1). Grossly and microscopically, it is characterized by cortical meningovascular proliferation and leptomeningeal calcification (2). Its pathogenesis has not been established; however, it is known to be associated with neurofibromatosis (NF) in nearly 50% of reported cases (3). In most reported cases, the mass lesion is solitary, although multiple lesions have occasionally been described. To our knowledge, though, multiple lesions with accompanying eccentric cysts have not been described on CT or MR studies. Accurate diagnosis of meningioangiomatosis is important because it is a benign, surgically correctable cause of seizures.
We report two cases of multifocal meningioangiomatosis.
Case Reports
Case 1
A 47-year-old woman had a 5-year history of headaches and generalized seizures. Precontrast CT scans showed multiple round calcified masses and eccentric cysts with edema in the left frontoparietal and right parietal lobes (Fig 1A and B). On T1-weighted MR images, the cyst was nearly isointense with CSF (Fig 1C). Proton density—and T2-weighted images revealed areas of dark signal intensity surrounded by areas of high signal intensity (Fig 1D and E). The central areas of dark signal intensity corresponded to the calcifications seen on CT scans. No significant mass effect was demonstrated. The patient underwent a left parietal craniotomy, and a calcified mass with cyst was totally removed; however, a small calcified mass in the right parietal lobe was not removed. There was no invasion of the overlying dura. The calcified mass was present in the cerebral cortex, and a cystic cavity was found in the subarachnoid space. Pathologic examination of the resected specimen showed multiple fragments of firm, whitish, calcified tissue, measuring 2.0 × 1.0 × 1.0 cm and 0.2 × 0.1 × 0.1 cm, respectively. Microscopically, the lesions consisted of extensive fibrillary calcification and proliferating vessels surrounded by meningothelial cells (Fig 1F). The patient has been free of seizures and headaches for the 15 months since surgery.
fig 1.
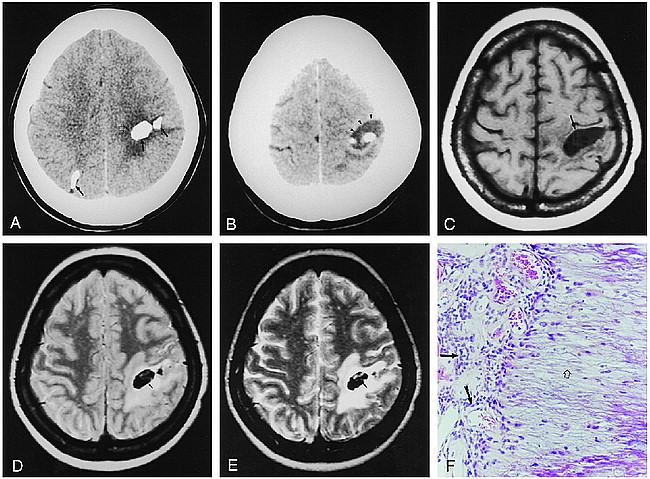
Case 1: 47-year-old woman.
A and B, Noncontrast CT scans show multiple round calcifications (solid arrows) and eccentric cysts (arrowheads) with moderate edema in the left frontoparietal (open arrow) and right parietal lobes.
C, On T1-weighted MR image (420/14/2 [TR/TE/excitations]), the cyst (arrow) is isointense with CSF; subtle, mottled dark signal intensity is also noted.
D and E, On proton density–weighted (2600/22/2) (D) and T2-weighted (2600/90/2) (E) images, the lesions have high signal intensity with central areas of low signal intensity (arrows).
F, Histopathologic specimen shows proliferating blood vessels surrounded by meningothelial cells (closed arrows) and fibrillary calcification (open arrow) (hematoxylin-eosin, original magnification ×100). This specimen was obtained from the cortex of the left parietal lobe.
Case 2
A 53-year-old man had a 2-year history of generalized seizures and headaches. Precontrast CT scans revealed dense round calcifications with eccentric cysts surrounded by edema in the left frontal and parietal lobes (Fig 2A). MR images of the brain showed heterogeneous areas of hypointense and isointense signal in the left frontal and parietal lobes on T1-weighted sequences (Fig 2B). The lesions showed irregular enhancement on contrast-enhanced T1-weighted images (Fig 2C and D). T2-weighted images revealed marked hypointensity corresponding to calcification and also revealed high signal intensity corresponding to cyst and edema (Fig 2E). The patient underwent left frontal and parietal craniotomies, and the calcified masses with cysts were totally removed. There was no involvement of the overlying dura. The calcified mass was located in the cerebral cortex and the cyst was in the subarachnoid space. The tumors were well demarcated, firm, whitish, and calcified. Microscopically, the lesions consisted of extensive fibrillary calcification and proliferating vessels surrounded by meningothelial cells. The patient has remained free of seizures and headaches during the 7 months since surgery.
fig 2.
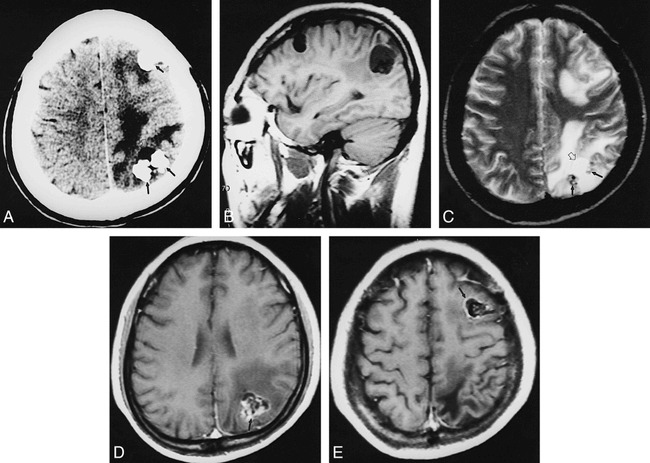
Case 2: 53-year-old man.
A, Noncontrast CT scan reveals multiple round calcifications (closed arrows) with eccentric cysts (open arrow) and moderate edema.
B, On T1-weighted image (420/14/2), the lesions show inhomogeneous hypo- and intermediate signal intensity in the left frontal and parietal lobes.
C, On T2-weighted image (2600/90/2), areas of heterogeneous signal intensity were noted in the left frontal and parietal lobes, caused by calcification (closed arrows), cyst (open arrow), and edema.
D and E, On contrast-enhanced T1-weighted image (420/14/2), the lesions show irregular enhancement (arrows).
Discussion
Meningioangiomatosis is a rare benign disorder characterized by the hallmarks of meningioma and angioma (4). It is a very slow-growing tumor (5) whose features have previously been reported (1–25). Meningioangiomatosis was first described by Bassoe and Nuzum in 1915 (6) as an incidental autopsy finding in a 15-year old boy; it was named by Worster-Drought et al in 1937 (1). Meningioangiomatosis primarily affects children and young adults, and seizures and/or headaches are the most common symptoms (2). It is associated with NF in nearly 50% of reported cases (3). A review of the literature suggests that meningioangiomatosis is strongly associated with NF2 rather than NF1 (7, 8).
Though its pathogenesis is unknown, three possible theories have been suggested (9): first, these lesions could represent a hamartoma; second, they could result from direct invasion of the brain tissue by a leptomeningeal meningioma; and third, they could represent a vascular malformation. Characteristics of meningioangiomatosis are leptomeningeal calcification and meningovascular proliferation interwoven with bands of fibrous connective tissue (10). The pathologic criteria for meningioangiomatosis may be summarized as follows: leptomeningeal proliferations of nodules, whorls, or bands of meningothelial cells (ie, arachnoidal cap cells exhibiting marked degenerative reactions, such as calcification, fibrocartilage, or bone formation) in association with sharply demarcated intracortical plaques of proliferating small vessels and perivascular cuffs of spindle-shaped fibroblastlike cells (4). The calcification patterns vary from faint psammomatous calcification to dense osteoid (5). Meningioangiomatosis affects the cerebral cortex in 90% of cases and usually occurs in the frontal or temporal lobes, but is rarely founded in the third ventricle, thalamus, cerebral peduncles (2), or brain stem (11). An association with meningioma or oligodendroglioma has occasionally been reported (12, 13).
Although multifocal cerebral lesions have been reported, meningioangiomatosis usually consists of well-demarcated solitary lesions (2, 14). Multifocal lesions or masses associated with cysts have not been described on either CT or MR studies. Our two patients with multifocal meningioangiomatosis were older than those in most reported cases and had no stigmata or family history of NF. On CT and MR examinations, the masses were composed mainly of dense round calcification and the cysts were eccentric to the mass. At surgery, the lesions were well demarcated and located superficially. Two lesions showed multiple calcifications with eccentric tumoral cysts. Cysts were also present in the subarachnoid spaces. It could be suggested that the mechanism of extratumoral cyst formation is the same as that of cystic meningioma, in which the cyst may form as the result of a ball-valve mechanism with the gradual accumulation of CSF in several sulci between the tumor and brain parenchyma (15).
Meningioangiomatosis is a benign lesion that does not become malignant (5). Its accurate diagnosis is important because total surgical removal is the treatment of choice, and the prognosis after surgery is excellent in most cases. The differential diagnosis of radiologic images (10, 25) includes meningioma, oligodendroglioma, granulomatous meningitis, and parasitic diseases.
Conclusion
Meningioangiomatosis is a benign cerebral lesion characterized by leptomeningeal calcification and meningovascular proliferation. It exhibits peripheral edema or gliosis on CT and MR imaging studies. It usually manifests as a solitary lesion; however, as we report, multifocal lesions or masses associated with cyst formation may be present.
Footnotes
Address reprint requests to Man-Soo Park, MD, Department of Radiology, Kang Nung Hospital, 415, Bangdong-Ri, Sacheon-Myon, Kangnung-Si, Kangwon-Do, 210–850, Korea.
References
- 1.Worster-Drought C, Dickson WEC, McMenemy WH. Multiple meningeal and perineural tumors with analogous changes in the glia and ependyma. Brain 1937;60:85-117 [Google Scholar]
- 2.Halper J, Scheithauer BW, Okazaki H, Laws ER. Meningioangiomatosis: a report of six cases with special reference to the occurrence of neurofibrillary tangles. J Neuropathol Exp Neurol 1986;45:426-446 [PubMed] [Google Scholar]
- 3.Tien RD, Osumi A, Oakes JW, Madden JF, Burger PC. Meningioangiomatosis: CT and MR findings. J Comput Assist Tomogr 1992;16:361-365 [PubMed] [Google Scholar]
- 4.Paulus W, Peiffer J, Roggendorf W, Schuppan D. Meningioangiomatosis. Pathol Res Pract 1989;184:446-452 [DOI] [PubMed] [Google Scholar]
- 5.Paringon CR, Graves VB, Megstrand LR. Meningioangiomatosis. AJNR Am J Neuroradiol 1991;12:549-552 [PMC free article] [PubMed] [Google Scholar]
- 6.Bassoe P, Nuzum F. Report of a case of central and peripheral neurofibromatosis. J Nerv Ment Dis 1915;42:785-796 [Google Scholar]
- 7.Stemmer-Rachamimov AO, Horgan MA, Taratuto AC, et al. Meningioangiomatosis is associated with neurofibromatosis 2 but not with somatic alterations of the NF2 gene. J Neuropathol Exp Neurol 1997;56:485-489 [DOI] [PubMed] [Google Scholar]
- 8.Sakaki S, Nakagawa K, Nakamura K, Takeda S. Meningioangiomatosis not associated with von Recklinghausen's disease. Neurosurgery 1987;20:797-801 [DOI] [PubMed] [Google Scholar]
- 9.Kasantikul V, Brown WJ. Meningioangiomatosis in the absence of Von Recklinghausen's disease. Surg Neurol 1981;15:71-75 [DOI] [PubMed] [Google Scholar]
- 10.Rubinstein LJ. Tumors of the central nervous system. In: Atlas of Tumor Pathology. Second series, fascicle 6. Washington DC: Armed Forces Institute of Pathology; 1972:252–307
- 11.Kollias SS, Crone KR, Ball WJ, Prenger EC, Ballard ET. Meningioangiomatosis of the brain stem: case report. J Neurosurg 1994;80:732-735 [DOI] [PubMed] [Google Scholar]
- 12.Blumenthal D, Berho M, Bloomfield S, Schochet SS Jr, Kaufman HH. Childhood meningioma associated with meningiomatosis: case report. J Neurosurg 1993;78:287-289 [DOI] [PubMed] [Google Scholar]
- 13.Lopez JI, Ereno C, Oleaga L, Areitio E. Meningioangiomatosis and oligodendroglioma in a 15-year-old boy. Arch Pathol Lab Med 1996;120:587-590 [PubMed] [Google Scholar]
- 14.Russell DS, Rubinstein LT. Pathology of Tumors of the Nervous System. 5th ed. Baltimore: Williams & Wilkins; 1989:777–779
- 15.Wasenko JL, Hochhauser L, Stopa EG, Winfield JA. Cystic meningioma: MR characteristics and surgical correlations. AJNR Am J Neuroradiol 1994;15:1959-1965 [PMC free article] [PubMed] [Google Scholar]
- 16.Kuzniecky R, Melanson D, Robitaille Y, Olivier A. Magnetic resonance imaging of meningioangiomatosis. Can J Neurol Sci 1988;15:161-164 [DOI] [PubMed] [Google Scholar]
- 17.Whiting DM, Awad IA, Miles J, Chou SS, Luders H. Intractable complex partial seizures associated with temporal lobe encephalocele and meningioangiomatosis: a case report. Surg Neurol 1990;34:318-322 [DOI] [PubMed] [Google Scholar]
- 18.Hozay J. Une angioneuromatose meningo-encephalique diffuse. Rev Neurol 1953;89:222-236 [PubMed] [Google Scholar]
- 19.Liu SS, Johnson PC, Sonntag VKM. Meningioangiomatosis: a case report. Surg Neurol 1989;31:376-380 [DOI] [PubMed] [Google Scholar]
- 20.Ogilvy CS, Chapman PH, Gray M, de la Monte SM. Meningioangiomatosis in a patient without von Recklinghausen's disease. J Neurosurg 1989;70:483-485 [DOI] [PubMed] [Google Scholar]
- 21.Kunishio K, Yamamoto Y, Sunani N, et al. Histopathologic investigation of a case of meningioangiomatosis not associated with von Recklinghausen's disease. Surg Neurol 1987;27:575-579 [DOI] [PubMed] [Google Scholar]
- 22.Rhodes RH, Davis RL. An unusual fibro-osseous component in intracranial lesions. Hum Pathol 1978;9:309-319 [DOI] [PubMed] [Google Scholar]
- 23.Jun C, Burdick B. An unusual fibro-osseous lesion of the brain. J Neurosurg 1984;60:1308-1311 [DOI] [PubMed] [Google Scholar]
- 24.Willson N, Kaufman MA, Bodansky SM. An unusual intracerebral connective tissue mass. J Neuropathol Exp Neurol 1977;36:373-378 [DOI] [PubMed] [Google Scholar]
- 25.Aizpuru RN, Quencer RM, Noenberg M, Altman N, Smirniotopoulos J. Meningioangiomatosis: clinical, radiologic and histopathologic correlation. Radiology 1991;179:819-821 [DOI] [PubMed] [Google Scholar]


