Abstract
BACKGROUND AND PURPOSE: Radiologic evaluation of CSF leaks is a diagnostic challenge that often involves multiple imaging studies with the associated expense and patient discomfort. We evaluated the use of screening noncontrast high-resolution CT in identifying the presence and site of CSF rhinorrhea and otorrhea and compared it with contrast-enhanced CT cisternography and radionuclide cisternography.
METHODS: We retrospectively reviewed the imaging studies and medical records of all patients who were evaluated for CSF leak during a 7-year period. Forty-two patients with rhinorrhea and/or otorrhea underwent high-resolution CT of the face or temporal bone and then had CT cisternography and radionuclide cisternography via lumbar puncture. The results of the three studies were compared and correlated with the surgical findings in 21 patients.
RESULTS: High-resolution CT showed bone defects in 30 of 42 patients (71%) with CSF leak. High-resolution, radionuclide cisternography and CT cisternography did not show bone defects or CSF leak for 12 patients (29%) who had clinical evidence of CSF leak. Among the 30 patients with bone defects, 20 (66%) had positive results of their radionuclide cisternography and/or CT cisternography. For the 21 patients who underwent surgical exploration and repair, intraoperative findings correlated with the defects revealed by high-resolution CT in all cases. High-resolution CT identified significantly more patients with CSF leak than did radionuclide cisternography and CT cisternography, with a moderate degree of agreement.
CONCLUSION: Noncontrast high-resolution CT showed a defect in 70% of the patients with CSF leak. No radionuclide cisternography or CT cisternography study produced positive results without previous visualization of a defect on high-resolution CT. CT cisternography and radionuclide cisternography may be reserved for patients in whom initial high-resolution CT does not identify a bone defect or for patients with multiple fractures or postoperative defects.
CSF leak was first described by Galen in the second century as a normal, periodic release of CSF into the nose via the sella and ethmoid regions (1). This process was accepted as a physiological communication for many centuries until the late 1800s, when St. Clair Thompson described a series of patients with an abnormal, nontraumatic condition that he termed rhinorrhea (1). Since the 1940s, the interest in CSF rhinorrhea has grown, and most cases are related to trauma. Although most trauma-related CSF leaks resolve without intervention, persistent CSF leak may lead to meningitis or abscess and requires surgical repair. The goal of surgical therapy is repair of the dural defect contributing to the CSF leak.
Patients with CSF leaks present a diagnostic challenge to both clinician and radiologist. Preoperative assessment of patients with CSF rhinorrhea or otorrhea requires localization of an anatomic defect. Various combinations of planar tomography and CT, contrast-enhanced CT cisternography, and radionuclide cisternography, and, more recently, MR cisternography have been used in the diagnosis of these patients. Traditionally, radionuclide cisternography and contrast-enhanced CT cisternography have been the principal methods of evaluation. These techniques require injections into the intrathecal space, most often via lumbar puncture. Although cisternography has minimal inherent risks, such as infection and lumbar CSF leak, it significantly increases expense and adds patient discomfort. Radionuclide studies do not provide precise anatomic localization of CSF leaks.
In comparing CT results with operative findings for 13 patients, Lloyd et al (2) suggested that high-definition CT is all that is required for the effective demonstration of the site of CSF leak. This eliminates the need for lumbar puncture and provides anatomic localization of the defect. The patients in that report, however, did not undergo other imaging studies for comparison, and the number of patients was small. The purpose of our study was to compare high-resolution CT with radionuclide cisternography and contrast-enhanced CT cisternography for 42 patients with CSF leak. Imaging findings were then correlated with operative and clinical data.
Methods
During a 7-year period extending from October 1990 to October 1997, we examined 52 patients for CSF leak. The medical records and imaging studies of these patients were reviewed retrospectively, and 10 patients were excluded from our study because of incomplete imaging. Of these 10 patients, nine did not undergo radionuclide cisternography at the specific request of the referring physician and one did not undergo CT cisternography because there was no clinically active leak at the time of imaging. None of these 10 patients had positive CT cisternography or radionuclide cisternography results in the absence of a bone defect revealed by high-resolution CT. The 42 remaining patients were included in the final analysis.
The referring otolaryngologist confirmed CSF leak before imaging was performed. Fluid initially was sent for routine analysis of glucose (>30 mg/mL) and protein (>45 mg/dL), and a classic ring test using filter paper was conducted. Confirmation was also obtained by β-2-transferrin (τ transferrin) content in 24 patients after it became available at our institution (3). This protein is highly specific for human CSF and requires a small sample size. Before the patients with rhinorrhea underwent imaging, nasal pledgets were placed by an otorhinolaryngologist. Six pledgets were placed at the bilateral sphenoethmoidal recesses, beneath the bilateral middle turbinates, and at the level of the eustachian tubes. Imaging was performed during clinically active CSF leak, as reported by the patient. In all cases, high-resolution CT and contrast-enhanced CT cisternography/radionuclide cisternography were performed on the same day.
All patients initially underwent noncontrast high-resolution CT of the maxillofacial region or temporal bone. CT studies were performed in the axial and coronal planes using 1- to 3-mm-thick contiguous sections (1 mm in 18 patients, 2 mm in five patients, 3 mm in 19 patients). The field of view was 150 to 180 mm using a 512 × 512 matrix. A bone algorithm was used to enhance bone detail in all studies. Positive CT results consisted of visualization of a bone defect with adjacent extracranial fluid collection or mucosal thickening.
Patients then underwent fluoroscopy-guided lumbar puncture, and 3 to 6 mL of nonionic contrast medium was injected in combination with 1 to 2 mCi of 99mTc-DTPA. All patients were then placed in a prone kneeling or prone Trendelenburg position for 2 to 5 minutes to facilitate opacification of the cisterns. No other provocative maneuvers were used. The patients immediately underwent CT in the axial and coronal planes using parameters that were identical to those of the noncontrast examination. Radionuclide cisternography was performed approximately 3 hours after injection using anterior and lateral planar projections. The pledgets were removed, and net counts per minute were obtained. Simultaneous blood samples were also counted. A pledget-to-serum ratio was then calculated after adjusting for background for each pledget and was considered positive if equal to or greater than 1.5.
Two neuroradiologists retrospectively reviewed all the CT and radionuclide studies to confirm the findings. Interpretation was performed without knowledge of the clinical site of the CSF leak. The radionuclide cisternography results were considered positive if either scintigraphy or pledgets showed increased activity, and the side of CSF leak was determined whenever possible. Noncontrast high-resolution CT studies were evaluated independently to determine the presence of a bone defect. Contrast-enhanced CT cisternography examinations were then reviewed to identify extracranial contrast or pooling of contrast material at a fracture site with deformity of a local sulcus as described by Fagerlund and Liliequist (4). Hounsfield units were obtained from pre- and postcontrast CT scans in suspicious areas of fluid or soft-tissue opacity. An increase of 50% or greater revealed by contrast-enhanced CT cisternography was considered to be a positive result. Using this method, extracranial regions (ie, sinuses) of high density due to inspissated secretions were differentiated from contrast leak, and there was no disagreement regarding any of the cases between the two neuroradiologists. The results of both CT cisternography and radionuclide cisternography were evaluated for sufficient opacification and activity in the basilar cisterns, respectively. The results of the three studies were then compared.
Of the 42 patients, 21 underwent surgical repair of their CSF leak. The operative reports for these patients were reviewed and correlated with the imaging data. The site of CSF leak was determined intraoperatively by either direct visualization of a dural/bone defect or leakage of fluorescein (1 mL of intrathecal 5% fluorescein) administered at the time of surgery. The imaging findings were compared with the clinical side of leakage (left or right). In addition, clinical records were reviewed for follow-up visits and repeat imaging studies for those patients with normal results of their imaging studies despite laboratory evidence of CSF leak.
Clinical confirmation of CSF leak was evaluated using McNemar's test for 42 patients. Patients with positive results of their CT cisternography, radionuclide cisternography, or both tests were combined and considered a positive result. The percentage of bone defects revealed by high-resolution CT was then compared with this collective group of cisternograms. A simple κ coefficient was calculated to determine whether the results were beyond chance. High-resolution CT, radionuclide cisternography, and CT cisternography were then compared for the 21 surgical patients, and sensitivity was determined for each. Because there were no true-negative results for the patients in this surgical cohort, specificity was not determined.
Results
The study group consisted of 16 men and 26 women with an age range of 19 to 69 years. Of these 42 patients, 34 presented with rhinorrhea, six with otorrhea, and two with both rhinorrhea and otorrhea. A review of the clinical charts indicated that the precipitating events for CSF leak were postsurgical (23 cases), posttraumatic (nine cases), spontaneous (six cases), congenital (two cases), and of indeterminate nature (two cases). Of the patients who experienced surgery relating precipitating events, 11 had undergone previous paranasal sinus surgery, five had undergone mastoidectomies, and seven had undergone various neurosurgical procedures. The two congenital defects occurred in one patient with fibrous dysplasia and another patient with an encephalocele.
Of the 42 patients included in our study, 12 had normal findings at high-resolution CT and contrast-enhanced CT cisternography/radionuclide cisternography despite histories of CSF leak. None of these patients underwent subsequent imaging or intervention. Bone defects with adjacent extracranial fluid or mucosal thickening were identified for the remaining 30 patients, accounting for 71% of the group. For 10 of these 30 patients, the results of radionuclide cisternography and CT cisternography were normal, with a bone defect revealed by high-resolution CT being the only imaging finding (Fig 1). Four of these 10 patients underwent surgery and are included in the surgical patient group. There were no patients with abnormal cisternographic findings in whom a bone defect was not initially detected by high-resolution CT. The high-resolution CT section thickness, therefore, did not seem to make a difference regarding detection.
fig 1.
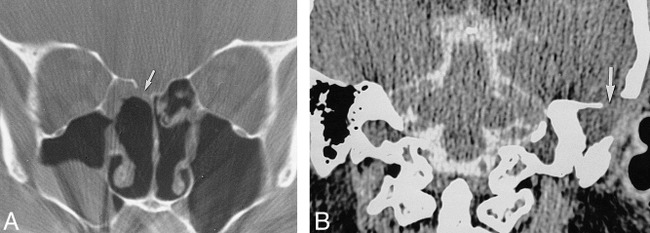
Two patients with bone defects on high-resolution CT and normal results of radionuclide cisternography and CT cisternography.
A, Coronal CT scan shows a defect (arrow) in the right cribriform plate with adjacent mucosal thickening.
B, Coronal CT scan of the temporal bone shows a large defect (arrow) in the tegmen mastoideum and mucosal thickening in the postsurgical mastoid bowl. No contrast accumulation is seen in the mastoid defect. Surgery confirmed the defect and leak in this patient.
All radionuclide cisternographic procedures were found to be of adequate technique, but four of 17 CT cisternographic procedures that produced negative results were noted to have poor contrast opacification of the basilar cisterns. Of the 30 patients with bone defects, 20 had positive cisternographic findings: seven at radionuclide cisternography, two at CT cisternography, and 11 on both studies (Figs 2–4). Twenty-one of 30 patients with bone defects underwent surgical exploration and repair, six experienced spontaneous resolution of their CSF leak, and three sought treatment elsewhere or were lost to follow-up.
fig 2.
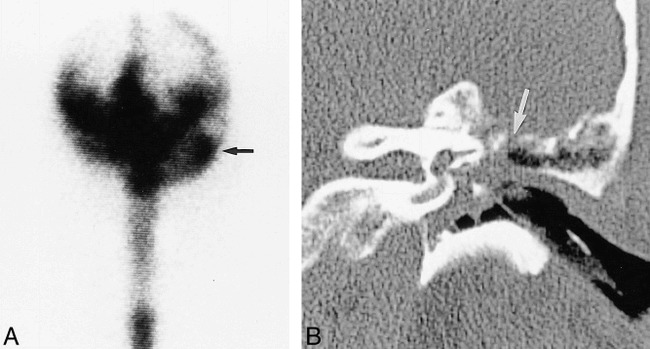
Patient with a defect revealed by CT and a leak revealed by radionuclide cisternography but not by CT cisternography.
A, Radionuclide cisternogram of the head, anterior planar view, shows an abnormal accumulation of radionuclide (arrow) in the left mastoid region.
B, Coronal CT scan of the temporal bone shows a defect (arrow) in the tegmen tympani with adjacent mucosal thickening. The bone and dural defect were confirmed at surgery.
fig 3.

Patient with a bone defect revealed by CT and a leak evident by CT cisternography but not by radionuclide cisternography.
A, Coronal CT scan of the face shows a large defect (straight arrow) in the right cribriform plate with adjacent mucosal thickening. Nasal pledgets can be seen within the nasal cavity (curved arrow).
B, Coronal CT cisternogram of the same region shows accumulation of contrast medium at the defect and extending into the ethmoidal sinus (arrow). The results of radionuclide cisternography and nasal pledgets were normal. There was no surgical confirmation.
fig 4.

Patient with a bone defect revealed by CT and positive results of radionuclide cisternography and CT cisternography.
A, Coronal CT scan of the face shows a defect (arrow) of the lateral sphenoidal sinus roof with mucosal thickening filling the sphenoidal sinus.
B, Coronal contrast-enhanced CT cisternogram shows contrast medium extending through the defect (arrow) and within the right sphenoidal sinus (curved arrow). The nasal pledgets indicated a leak in the region of the right sphenoethmoidal recess, although the cisternogram did not show abnormal accumulation of the radionuclide. The defect and CSF leak were confirmed at surgery.
Using McNemar's test, analysis of the 42 patients with CSF leak showed that high-resolution CT identifies bone defects in significantly more patients (P = .002) than radionuclide cisternography and/or CT cisternography detects leaks. A simple κ coefficient of .54 indicated moderate agreement that the results were beyond chance. There was a moderate degree of overlap between the tests. High-resolution CT and cisternography tended to miss the same patients with clinical evidence of CSF leak.
Surgical Patients
Twenty-one of 42 patients underwent surgical repair, all of whom had bone defects revealed by high-resolution CT. For 20 of 21 patients, the site of CSF leak was identified by direct visualization of a dural/bone defect or leakage of intrathecally administered fluorescein. In one patient, a bone defect was seen at surgery with no dural defect or fluorescein leak. The defect on the initial high-resolution CT scan correlated with the intraoperative defect for all 21 patients. In one patient, a subsequent CSF leak developed several years after surgery that was confirmed at a new site on imaging studies. The 21 surgical patients are summarized in Table 1.
TABLE 1:
Surgical patient summary

Four of these 21 surgical patients had bone defects revealed by high-resolution CT but had normal findings at radionuclide cisternography and CT cisternography (patients 1–4). Surgery was performed in these patients on the basis of the high-resolution CT findings alone and persistent clinical CSF leak. Clinical confirmation of CSF leak was obtained for three patients. In the fourth patient, no leak was observed at surgery, but the bone defect was confirmed (patient 4). This patient had clinical resolution of CSF leak after surgery. The remaining 17 surgical patients all had bone defects revealed by high-resolution CT; seven of the 17 patient had positive radionuclide cisternography results, one had positive CT cisternography results, and nine had positive results on both studies. The sensitivity of each examination was calculated for the 21 surgically proved cases as follows: high-resolution CT, 100%; radionuclide cisternography, 76%; and CT cisternography, 48%. Specificity was not determined because there were no true-negative results for the patients in this cohort.
Four patients with multiple bone defects revealed by high-resolution CT underwent surgical exploration (patients 13, 17, 18, and 21). For patient 13, all three imaging studies were positive. For patients 17 and 18, a leak was revealed by radionuclide cisternography but not by CT cisternography, whereas for patient 21, a leak was revealed by CT cisternography but not by radionuclide cisternography. CSF leak and bone defects were observed at surgery in all four patients, corresponding to the leak revealed by cisternography.
Nonsurgical Patients
For 21 of 42 patients, there was no surgical confirmation of either the visualized high-resolution CT defects or the CSF leak. Nine of 21 patients had bone defects at high-resolution CT. One patient also had positive CT cisternography results, and two patients had positive results of both radionuclide and CT cisternography (Table 2). In all nine patients, the side of the defect revealed by high-resolution CT corresponded to the side (left/right) of the clinical CSF leak. All nine patients experienced spontaneous resolution of their CSF leak with bed rest and/or lumbar drain.
TABLE 2:
Nonsurgical patient summary

Twelve of these 21 patients had normal findings at high-resolution CT and cisternography despite clinical evidence of CSF leak (Table 2). There was no common cause or clinical presentation within this group of patients. Medical records showed that for 11 of 12 patients, spontaneous resolution was noted at the time of the clinical follow-up examinations. One patient did not seek further treatment, so no follow-up records were available.
Two nonsurgical patients had multiple bone defects revealed by high-resolution CT (patients 26 and 27). Neither radionuclide cisternography nor CT cisternography revealed a leak for either of these patients. In patient 26, there was poor opacification of the basilar cisterns revealed by CT cisternography that may have accounted for the negative results. Both patients experienced spontaneous resolution of their CSF leak within 1 month of imaging.
Discussion
Radionuclide cisternography and contrast-enhanced CT cisternography are the mainstays of CSF leak evaluation. Simultaneous injection of radionuclide and CT contrast agents provides information regarding the presence and anatomic location of a CSF leak. Although the use of nasal pledgets to increase sensitivity is universally accepted, several more controversial methods of increasing sensitivity have been described, including head-hanging CT (5) and the overpressure technique (6, 7). Whenever possible, imaging should be performed with the patient in a position most likely to maximize CSF leakage (8).
In cases of large bone/dural defects, both portions of the examination may show a leak. Smaller defects often result in only one positive study, radionuclide cisternography or CT cisternography, leading to the conclusion that their combined use increases sensitivity (7). Cisternography, however, requires a lumbar puncture, which increases the patient's discomfort and expense, and, at most institutions, precisternography CT is also routinely performed for comparison with contrast-enhanced images, and therefore does not directly increase expense.
Because most CSF leaks are intermittent, the sensitivity of cisternography is dependent on the timing of the examination. Several authors have reported on the use of MR cisternography with sensitivity as high as 90% (9–12). MR cisternography eliminates lumbar puncture and does not seem to be dependent on active CSF leak. It is contraindicated in certain groups of patients (after aneurysm repair, retained metallic foreign bodies), and further clinical experience is necessary before MR cisternography gains widespread acceptance.
Indium-111–labeled DTPA also has been used to increase the sensitivity of radionuclide cisternography (13, 14). This requires patient compliance during subsequent imaging that is performed over a 2- to 3-day period. Glaubitt et al (13) reported detection of three delayed CSF leaks in 12 patients using 111In-DTPA but required imaging at 3, 6, 24, 48, and sometimes 72 hours after injection, and nasal pledgets were placed for 4 hours twice daily (13). The use of high-resolution CT as a screening technique for CSF leak may eliminate the need for lumbar puncture; reduce time, expense, and patient discomfort; and is not necessarily dependent on active CSF leak.
Left untreated, persistent CSF leak may result in recurrent meningitis. Although early investigators reported infection rates as high as 40% (15–17), recent data suggest an incidence of approximately 4% (1, 18). Surgery is aimed at closure of the defect, usually using pedicled or free mucosal grafts, or obliteration of a sinus, using muscle/fascia and fibrin glue (19). It is important to accurately identify the bone/dural defect responsible for CSF leakage for successful surgical intervention. The bone defects revealed by high-resolution CT must correspond to the site of CSF leak observed at surgery for this method to be acceptable. In our series, 21 of 42 patients underwent surgical exploration and all had confirmation of the defect revealed by high-resolution CT. In addition, 20 of these patients also had intraoperative visualization of CSF leak at this location.
CSF leak is not directly visible on noncontrast high-resolution CT scans. The question therefore arises as to whether a defect revealed by high-resolution CT correlates with the site of CSF leak. In our series, all patients underwent high-resolution CT before both cisternographic procedures. Of the 19 patients who had positive results at cisternography (radionuclide cisternography and/or CT cisternography), all had anatomic defects on high-resolution CT scans that corresponded to the site of leakage at surgery. There were, however, 11 patients with defects revealed by high-resolution CT but with no leak apparent at cisternography. Four of these patients underwent surgery, and the bone defect corresponded to the site of the high-resolution CT defect in each; three patients also had intraoperative confirmation of CSF leak at the site of the defect. The fourth patient had a very small defect observed at surgery but no intraoperative leak. Because CSF leaks are intermittent, cisternography should be performed during active leak to maximize sensitivity. Although attempts were made to examine all patients during active CSF leak, delays between high-resolution CT, CT cisternography, and radionuclide cisternography may have led to negative results on cisternograms. The small size of the defect in the fourth patient may have also limited detection of leakage at the time of surgery.
Cisternography may help confirm the site of CSF leak in patients with multiple cranial fractures. In our series, six patients had multiple bone defects revealed by high-resolution CT. CT cisternography localized the site of the leak in two of these patients. In two patients with normal CT cisternographic findings, surgery was performed on the basis of the most suspicious defect at high-resolution CT and correlation with radionuclide cisternography. Intraoperative fluorescein confirmed CSF leak at the defect identified on high-resolution CT in both cases. The remaining two patients with normal findings at radionuclide and CT cisternography experienced spontaneous resolution of their CSF leak. Although cisternography clearly assisted surgical planning for two patients, only six patients in our series had multiple defects. The additional information gained by performing cisternography, therefore, remains of questionable significance, and further study of this patient subset is needed.
Twelve patients had normal imaging findings, and all 12 experienced resolution of their CSF leak within 1 month of their imaging studies. It is possible that the bone defects in these patients were missed because of technical factors. In 10 of 12 patients, high-resolution CT was performed using 3-mm contiguous sections. It is possible that small bone defects are not visible at that resolution. We currently use 1-mm-thick high-resolution CT sections in all patients being evaluated for CSF leak to better identify small defects. Note, however, that there were no patients scanned with 3-mm sections in whom a leak was identified by radionuclide cisternography or CT cisternography in the absence of a defect revealed by high-resolution CT. In two patients, metallic artifacts from buckshot and dental hardware, respectively, may have interfered with the localization of bone defects. Only one of these 12 patients had 1-mm-thick high-resolution CT sections and no significant artifact. Despite the lack of an identifiable defect in these 12 patients, the CSF leak resolved in all patients without treatment.
Clinically symptomatic patients with normal imaging findings may best be treated conservatively by elevation of the head, avoidance of coughing, sneezing, and nose blowing, and the occasional administration of prophylactic antibiotic therapy (1). The CSF leak may often then spontaneously resolve.
Conclusion
High-resolution CT used initially to screen for CSF leak showed bone defects in 71% of the patients. There were no patients with positive results at CT cisternography or radionuclide cisternography who did not initially have bone defects revealed by high-resolution CT. There were, however, 10 patients with defects revealed by high-resolution CT in whom no leak was apparent by either radionuclide cisternography or CT cisternography. Twenty-one patients had confirmation of their defects at surgical exploration, and 20 of these patients had CSF leak observed at surgery that corresponded to the preoperative imaging findings. Our study suggests that high-resolution CT is a useful screening examination for the initial workup of CSF rhinorrhea or otorrhea. When the clinical and imaging findings coincide, further evaluation using CT cisternography and radionuclide cisternography is often unnecessary.
Footnotes
Presented at the annual meetings of the American Society of Head and Neck Radiology (recipient of the Radiologist-in-Training award), Phoenix, April 1998, and the American Society of Neuroradiology, Philadelphia, May 1998.
Address reprint requests to Jeffrey A. Stone, MD, Medical College of Georgia, Department of Radiology, 1120 15th St, Augusta, GA 30912.
References
- 1.Zlab MK, Moore GF, Daly DT, Yonkers AJ. Cerebrospinal fluid rhinorrhea: a review of the literature. Ear Nose Throat J 1992;71:314-317 [PubMed] [Google Scholar]
- 2.Lloyd MNH, Kimber PM, Burrows EH. Post-traumatic cerebrospinal fluid rhinorrhoea: modern high-definition computed tomography is all that is required for the effective demonstration of the site of leakage. Clin Radiol 1994;49:100-103 [DOI] [PubMed] [Google Scholar]
- 3.Oberascher G. A modern concept of cerebrospinal fluid diagnosis in oto- and rhinorrhea. Rhinology 1988;26:89-103 [PubMed] [Google Scholar]
- 4.Fagerlund M, Lilequist B. Intermittent cerebrospinal liquorrhea: cerebral computed tomography in the non-drop period. Acta Radiol 1987;28:189-192 [PubMed] [Google Scholar]
- 5.Rothfus WE, Deeb ZL, Daffner RH, Prostko ER. Head-hanging CT: an alternative for evaluating traumatic CSF rhinorrhea. AJNR AM J Neuroradiol 1987;8:155-156 [PMC free article] [PubMed] [Google Scholar]
- 6.Curnes JT, Vincent LM, Kowalsky RJ, McCartney WH, Staab EV. CSF rhinorrhea: detection and localization using overpressure cisternography with Tc-99m-DTPA. Radiology 1985;154:795-799 [DOI] [PubMed] [Google Scholar]
- 7.Piepgras U, Huber G. Simultaneous isotope and CT cisternography in the diagnosis and evaluation of cerebrospinal fluid rhinorrhea. Acta Radiol 1986;369(Suppl):290-291 [PubMed] [Google Scholar]
- 8.Di Chiro G, Ommaya AK, Ashburn WL, Briner WH. Isotope cisternography in the diagnosis and follow-up of cerebrospinal fluid rhinorrhea. J Neurosurg 1968;28:522-529 [DOI] [PubMed] [Google Scholar]
- 9.Eberhardt KEW, Hollenbach HP, Deimling M, Tomandl BF, Huk WJ. MR cisternography: a new method for the diagnosis of CSF fistulae. Eur Radiol 1997;7:1485-1491 [DOI] [PubMed] [Google Scholar]
- 10.El Gammal T, Sobol W, Wadlington VR, Sillers MJ, Crews C, Fisher WS III, et al. Cerebrospinal fluid fistula: detection with MR cisternography. AJNR Am J Neuroradiol 1998;19:627-631 [PMC free article] [PubMed] [Google Scholar]
- 11.Shetty PG, Shroff MM, Sahani DV, Kirtane MV. Evaluation of high-resolution CT and MR cisternography in the diagnosis of cerebrospinal fluid fistula. AJNR Am J Neuroradiol 1998;19:633-639 [PMC free article] [PubMed] [Google Scholar]
- 12.Eljamel MS, Pidgeon CN. Localization of inactive cerebrospinal fluid fistulas. J Neurosurg 1995;83:795-798 [DOI] [PubMed] [Google Scholar]
- 13.Glaubitt D, Haubrich J, Cordoni-Voutsas M. Detection and quantitation of intermittent CSF rhinorrhea during prolonged cisternography with 111In-DTPA. AJNR Am J Neuroradiol 1983;4:560-563 [PMC free article] [PubMed] [Google Scholar]
- 14.Schicha H, Voth E, Emrich D. Detection of occult and intermittent rhinorrhea using 111In-DTPA. 1985;11:76-79 [DOI] [PubMed] [Google Scholar]
- 15.Lewin W. Cerebrospinal fluid rhinorrhea in nonmissile head injuries. Clin Neurosurg 1966;52:237-252 [DOI] [PubMed] [Google Scholar]
- 16.Lewin W. Cerebrospinal fluid rhinorrhea in closed head injuries. Br J Surg 1954;42:1-18 [DOI] [PubMed] [Google Scholar]
- 17.Munro D. The modern treatment of craniocerebral injuries with special reference to the maximal permissible mortality and morbidity. N Engl J Med 1935;213:893-906 [PMC free article] [PubMed] [Google Scholar]
- 18.Eljamel MS, Fay PM. Acute traumatic CSF fistula: the risk of intracranial infection. Br J Neurosurg 1990;4:381-385 [DOI] [PubMed] [Google Scholar]
- 19.Wax MK, Ramadan HH, Ortiz O, Wetmore SJ. Contemporary management of cerebrospinal fluid rhinorrhea. Otolaryngol Head Neck Surg 1997;116:442-449 [DOI] [PubMed] [Google Scholar]


