Abstract
Summary: A pulmonary embolus of acrylic cement was present in a 41-year-old woman with Langerhans' cell vertebral histiocytosis (LCH) after percutaneous vertebroplasty. Chest radiograph and CT confirmed pulmonary infarction and the presence of cement in the pulmonary arteries. She was treated with anticoagulants, and responded favorably. This rare complication occurred because perivertebral venous migration was not recognized during vertebroplasty. Adequate preparation of cement and biplane fluoroscopy are recommended for vertebroplasty.
Percutaneous vertebroplasty involves an injection of acrylic cement (polymethylmethacrylate [PMMA]) into a diseased vertebral body for partial vertebral body remodeling and lumbar pain relief (1). Complications are infrequent, and consist of local processes such as infection or cement leakage into the spinal canal or the perivertebral venous system (2, 3). Other complications usually are related to the initial vertebral disease rather than to the vertebroplasty technique itself (2–4). One case of lethal pulmonary embolism has been reported in the immediate postoperative period (4). In that case, pulmonary embolism was not related to the performance of vertebroplasty (no cement was evident on chest radiograph). We report a case of symptomatic pulmonary embolism caused by cement after percutaneous vertebroplasty.
Case Report
A 41-year-old woman was hospitalized for pain in the right lower chest, tachypnea, tachycardia, and hemoptysis. The chest pain started immediately after percutaneous vertebroplasty of L3 performed 10 days earlier for chronic lumbar pain and osteolysis secondary to LCH. Diagnosis of LCH was made 2 years earlier by surgical biopsy. Dyspnea did not develop until the third postoperative day, after the patient already had been discharged from the hospital.
Vertebroplasty was performed under general anesthesia by a unilateral transpedicular approach with a 10-gauge needle. The acrylic cement (Surgical Simplex [How Medica International Inc.; Shannon, Ireland]) had been prepared at room temperature (20° C) and opacified with 1 g of tungsten powder. Eight cc was injected under lateral fluoroscopic guidance.
Blood gas analysis revealed hypoxia (76 mm Hg oxygen) and hypocapnia (36 mm Hg pCO2). A chest radiograph revealed a consolidation in contact with the pleural surface in the middle lobe, associated with a right pleural effusion. Multiple tubular opacities corresponding to the course of vessels were also depicted opposite the opacity in the middle lobe (Fig 1A).
fig 1.
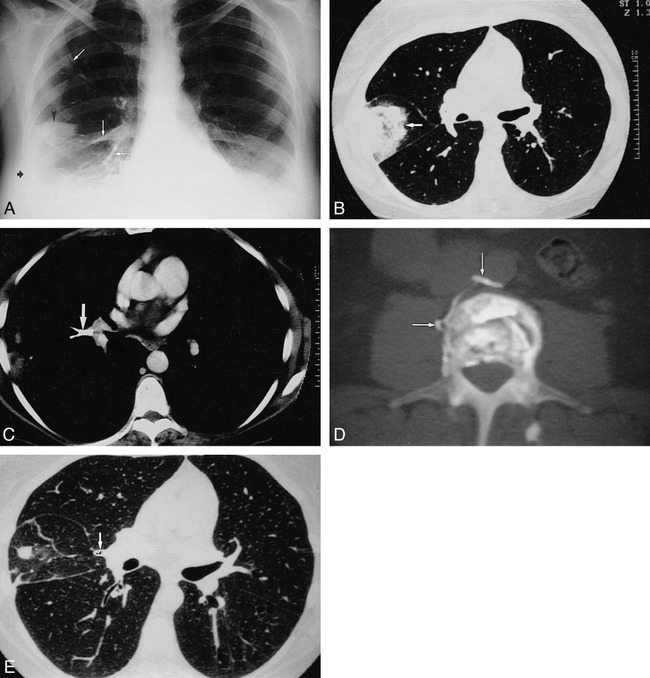
Chest radiograph and CT of 41-year-old woman with LCH after percutaneous vertebroplasty.
A, Chest radiograph shows pleural-based consolidation in the middle-lobe (arrow-head). Multiple high-density tubular opacities outlining pulmonary vessels (white arrows). Note a right pleural effusion (black arrow).
B, Chest CT scan at the level of bronchus intermedius shows characteristic appearance of pulmonary infarct in the middle lobe and pleural-based truncated cone consolidation (white arrow) between major and minor fissures.
C, Chest CT scan with soft tissue window settings. High-density intra-luminal cement (arrow) outlining the pulmonary artery and its bifurcation.
D, CT scan with bone settings at the level of vertebroplasty (L3) shows cement in right latero-vertebral vein draining in the vena cava (arrows).
E, Follow-up chest CT 1 month after vertebroplasty. Comparison with fig. 1B shows partial resolution of the pulmonary infarct in the middle lobe and persistence of cement in pulmonary artery (arrow).
Ventilation perfusion scanning revealed multiple perfusion defects in the right lung, predominantly in the middle and lower lobes. Doppler sonography of the legs was unremarkable. Thoracic CT revealed the characteristic appearance of pulmonary infarction of the middle lobe (Fig 1B). The presence of cement in the pulmonary arteries of the middle lobe and several segmental arteries of the superior and lower lobes confirmed a pulmonary embolism caused by cement (Fig 1C). CT showed the origin of the leak arose at the level of the vertebroplasty, revealing cement in a right laterovertebral vein draining into the inferior vena cava (Fig 1D). A small asymptomatic epidural leak was also observed. The patient was treated with anticoagulants and responded favorably, with regression of dyspnea and tachycardia and normalization of blood gases. Follow-up CT 1 month later revealed progressive resolution of the middle lobe infarction (Fig 1E).
Discussion
Although percutaneous vertebroplasty is considered only minimally invasive, complications can occur during the procedure. Cement leaks into the external vertebral venous plexuses have frequently been described. There is also a potential risk of cement migration into the inferior vena cava (4) and pulmonary embolism. Nevertheless, we failed to find any documented report of symptomatic pulmonary embolism caused by acrylic cement. This is probably because of the extremely rapid polymerization of the PMMA before it reaches the vena cava. Jensen et al (5) reported two patients with presumed embolization to the lungs that did not evince respiratory changes. Venous leaks can also occur toward the internal vertebral venous plexuses resulting in cord or nerve root compression (3). The great majority of these leaks are asymptomatic. Such leaks can be explained by the fluid consistency of the PMMA at the moment of injection. More extensive leaks may occur if the needle is positioned incorrectly, especially if the tip lies in a basivertebral vein. Gangi et al (6) recommended that the technique be performed under both CT and fluoroscopic guidance to verify needle positioning.
The pulmonary embolism in our patient may have been caused by insufficient polymerization of the PMMA at the time of injection, which allowed migration into the inferior vena cava and the pulmonary arteries. For this reason, the acrylic cement must be mixed to the consistency of paste (i.e. a stage of advanced polymerization) before injection so that the several difficult-to-evaluate factors that affect the polymerization rate (e.g. room temperature) can be better controlled. Good-quality lateral fluoroscopy is essential during injection. Detection of even minimal cement leakage into the perivertebral veins or behind the line of the posterior wall should be indications to halt the procedure immediately. In our case, pulmonary embolism occurred because perivertebral venous migration was not recognized. The cement was opacified only with tungsten powder. Jensen et al (5) recommend a barium/tungsten combination for adequate visualization of needle positioning and venous flow during fluoroscopy. Moreover, real-time detection of laterovertebral leakage remains difficult owing to overlap of the intravertebral cement. Biplane fluoroscopy or intermittent anteroposterior fluoroscopy could overcome this problem (5). The value of performing prior vertebral venography through the vertebroplasty needle is controversial. Jensen el al (5) found vertebrography to be of great use because it confirmed the needle position in the trabecular space and outlined the venous outflow pattern, showing where to look for PMMA migration. Some European authors (4, 6) have not performed vertebrography prior to vertebroplasty. Results appear doubtful to them because iodinated contrast agents have different physicochemical properties than PMMA, and nearly always diffuse into the venous plexuses. In addition, persistence of intravertebral opacifications could interfere with vertebroplasty.
Venous leaks are most frequent with highly vascular lesions (metastases of thyroid cancer, renal carcinoma, or vertebral angiomas). The main indications for vertebroplasty are osteolytic metastases, osteoporotic compression fractures, and vertebral hemangiomas. There are few reports in the literature of vertebroplasty for the treatment of LCH (7). These bone lesions are not histologically hypervascular, and it therefore seems difficult to attribute the lesion itself to the venous leak in our patient.
Nonetheless the literature does contain a report of a lethal pulmonary thromboembolism (4). A chest radiograph obtained in that case did not reveal any cement in the pulmonary arteries. By contrast, an acrylic cement embolism has been reported after hip replacement arthroplasty (8), although much more cement is used during arthroplasty than is required for vertebroplasty. In this study, however, these emboli detected by transesophageal sonography remained asymptomatic.
Interestingly, the vascular leak in our patient was not identified during the procedure, and diagnosis of pulmonary cement embolism was delayed. The lower chest pain felt immediately after the procedure was attributed to the vertebroplasty. It is not uncommon for patients to complain of local-regional pain 48 hours postoperatively, but discomfort usually subsides after nonsteroidal antiinflammatory drug administration. Misinterpretation of this patient's pain accounts for delay in diagnosis. Presence of chest pain should have suggested either a rib fracture or a pulmonary embolism, and a chest radiograph should have been taken immediately. The delayed onset of dyspnea that occurred after the patient had been discharged from the hospital may also explain the diagnostic delay. Furthermore, the embolism would probably have been diagnosed immediately if the patient had not been treated under general anesthesia. Several authors perform vertebroplasty under local anesthesia (3) or neuroanalgesia (5).
Anticoagulants appear to have been effective on the pulmonary infarction and clinical course of our patient, although it would be imprudent to recommend any therapeutic approach based on a single case. It would be interesting to perform a study with systematic chest radiographs after vertebroplasty in order to determine the incidence of pulmonary embolism caused by cement leakage and its impact on lung tissue.
Footnotes
Address reprint requests to B. Padovani, Department of Radiology, Hôpital Pasteur, BP 69 06002 Nice, Cedex 1, France.
References
- 1.Deramont H, Galibert R, Debussche-Depriester C. Percutaneous vertebroplasty with methylmethacrylate: technique, method, results. Abstract from the Radiological Society of North America, Chicago, 1990
- 2.Cotten A, Dewatre F, Cortet B, et al. Percutaneous vertebroplasty for osteolytic metastases and myeloma: effects of the percentage of lesion filling and the leakage of methyl methacrylate at clinical follow-up. Radiology 1996;200:525-530 [DOI] [PubMed] [Google Scholar]
- 3.Chiras J, Depriester C, Weill A, Sola-Martinez MT, Deramond H. Vertébroplasties percutanées. J Neuroradiol 1997;24:45-59 [PubMed] [Google Scholar]
- 4.Weill A, Chiras J, Simon JM, Rose M, Sola-Martinez T, Enkaoua E. Spinal metastases: indications for and results of percutaneous injection of acrylic surgical cement. . Radiology 1996;99:241-247 [DOI] [PubMed] [Google Scholar]
- 5.Jensen ME, Avery JE, Mathis JM, Kallmes DF, Cloft HJ, Dio JE. Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fractures: technical aspects. AJNR Am J Neuroradiol 1997;18:1897-1904 [PMC free article] [PubMed] [Google Scholar]
- 6.Gangi A, Kastler BA, Dietemann JL. Percutaneous vertebroplasty guided by a combination of CT and fluoroscopy. AJNR Am J Neuroradiol 1994;15:83-86 [PMC free article] [PubMed] [Google Scholar]
- 7.Cardon T, Hachulla E, Flipo RM, et al. Percutaneous vertebroplasty with acrylic cement in the treatment of a Langerhans cell vertebral histiocytosis. Clin Rheumatol 1994;13:518-521 [DOI] [PubMed] [Google Scholar]
- 8.Propst JW, Siegel LC, Schnittger I, Foppiano L, Goodman SB, Brock-Utne JG. Segmental wall motion abnormalities in patients undergoing total hip replacement: correlations with intraoperative events. Anesth Analg 1993;77:743-749 [DOI] [PubMed] [Google Scholar]


