Abstract
Summary: Contrast-bolus tracking in the carotid bifurcation was accomplished using an MR angiographic technique with a 3D turbo field-echo readout (TR/TE = 6/3, flip angle = 50°) modified by a keyhole scheme. Optimal visibility of the contrast bolus was achieved by digital subtraction from a reference volume. This technique reliably time-resolves the carotid arteries from the jugular veins.
The need for noninvasive imaging of the carotid arteries has provided fertile ground for the rapid development and application of different MR angiographic techniques (1–3). The commonly used time-of-flight (TOF) MR angiographic techniques suffer from artifacts related to intravoxel phase dispersion and to saturation of flow-related enhancement (4, 5).
Contrast-enhanced MR angiography, a technique in which contrast between intravascular lumen and extravascular tissues is achieved by injecting a T1-shortening agent into the bloodstream, has shown promise with regard to accurate representation of the vascular lumen and reduced sensitivity to TOF-related artifacts (6).
The need for fast contrast-enhanced 3D MR angiography is particularly important in carotid artery imaging to help time-resolve the arteries from the prominent adjacent jugular veins without cumbersome image postprocessing.
Although 3D MR techniques, in which the acquisition of the center of k-space is timed to coincide with the arrival of the contrast bolus in the imaging region of interest, have shown potential for routine cervical carotid artery imaging, they remain operator- and patient-dependent (7). More recently, improvements in MR imaging hardware and innovations in pulse design and k-space manipulation have allowed 3D time-resolved MR angiography with a reduced need for precise timing or to account for differences in intravascular transit times of the contrast bolus (8).
In this article, we describe a fast digital subtraction 3D MR angiographic technique for tracking a bolus of contrast material in the carotid bifurcation that can be implemented on a clinical MR unit with average gradient performance (non–echo planar). Also, we demonstrate the potential of this technique for time-resolving the carotid arteries from the jugular veins and for depicting carotid artery stenosis.
Methods
All carotid MR angiographic imaging was performed on a 1.5-T superconducting MR system with maximum gradient capability of 15 mTm−1 and a slew rate of 16.7 mTm−1·ms −1. MR angiograms were obtained with a standard quadrature neck coil operating in receive mode (Phillips Medical Systems; Shelton, CT).
First-pass contrast-bolus–tracking 3D MR angiography was implemented using a single-shot T1-weighted turbo field-echo readout technique (TR/TE = 6/2). Based on published computer simulation results, a nominal flip angle of 50° was chosen to optimize the angiographic contrast (7). A single volume was placed in the coronal plane with an FOV of 30 cm (40% rectangular) and a matrix of 102 × 256 (pixel size, 1.17 × 1.17 mm). The volume thickness was 5 cm divided into 20 5-mm-thick partitions (50% overcontiguous). A linear phase-encode profile order was implemented. The readout bandwidth was 450 Hz per pixel.
The acquisition was modified by a “keyhole” scheme that improved the temporal resolution in dynamic MR imaging by a factor of 2.2. A full sampling of k-space prior to intravenous bolus administration of 0.20 mmol/kg of gadopentetate dimeglumine was followed by truncated sampling limited to the segment of k-space sensitive to changes in image contrast (central 46 phase-encoded lines of k-space). Twenty dynamic volumes were generated (3.6 s/vol). Optimal visualization of the contrast bolus was achieved by image subtraction using the first image (full k-space sampling) as a reference.
Five patients (average age, 72 years) with narrowing at the carotid artery bifurcation demonstrated by 2D TOF MR angiography (22/7, 60° flip angle, 3-mm-thick sections) and five volunteers (average age, 34 years) were imaged using the first-pass contrast-bolus–tracking 3D MR angiographic technique. Informed consent was obtained from all volunteers.
The maximum-intensity projection (MIP) images generated from the first-pass contrast-bolus–tracking 3D MR angiographic technique were evaluated for the number of carotid bifurcations shown and the number of dynamic images that depicted only arterial structures. The degree of stenosis at the carotid bifurcations was compared using the MIP images generated from both MR angiographic techniques.
Results
First-pass contrast-bolus–tracking 3D MR an-giography adequately depicted both carotid bifurcations in each of the 10 subjects. In all 10 subjects there were at least two dynamic volumes in which the arteries of the head and neck were temporally resolved from the veins (Fig 1).
fig 1.
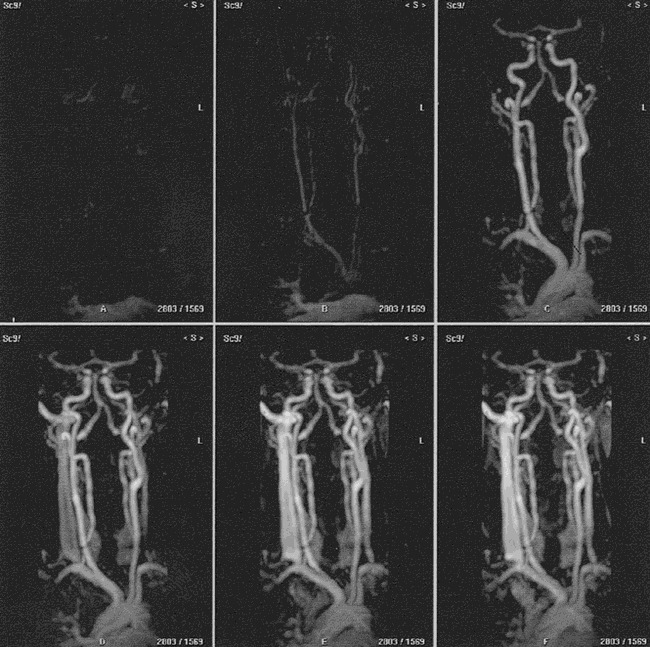
MIP projections of six of 20 temporally resolved volumes acquired from a male volunteer using subtracted 3D dynamic keyhole turbo field-echo MR angiography (TR/TE = 6/3, flip angle = 50°) show a coronal view of the vessels in the head and neck. The early phases show the aortic arch and major branches, the carotid arteries and bifurcations, and the vertebrobasilar arteries without interference from veins. The later phases show the arteries and the internal jugular veins
With regard to vessel-background contrast, MIP projections generated from the subtracted data set were judged superior to those generated from the nonsubtracted data set in all 10 subjects (Fig 2).
fig 2.

Rotated MIP projections of the eighth dynamic volume (arterial phase) acquired from a male volunteer using 3D dynamic keyhole turbo field-echo MR angiography (TR/TE = 6/3, flip angle = 50°). The nonsubtracted (top row) and the subtracted (bottom row) images show the aortic arch and major branches, the carotid arteries and bifurcations, and the vertebrobasilar arteries without interference from veins. Note the improved contrast between the arteries and background on the subtracted images
The rotated targeted MIP projections generated from the subtracted data set showed normal carotid bifurcations in all five volunteers (Fig 3).
fig 3.

Rotated targeted MIP projections of the ninth dynamic volume (arterial phase) acquired from a female volunteer using subtracted 3D dynamic keyhole turbo field-echo MR angiography (TR/TE = 6/3, flip angle = 50°) show a normal left carotid bifurcation without interference from veins.
The rotated targeted MIP projections generated from 2D TOF MR angiographic raw data showed narrowing in six carotid bifurcations (four on the left and two on the right side). The narrowing at the carotid bifurcation was judged to be mild in one, moderate in three, and severe in two.
Compared with 2D TOF MR angiography, the severity of the stenosis was less on the rotated targeted MIP projections generated from the contrast-bolus–tracking 3D MR angiographic technique in three carotid bifurcations (one mild and two moderate). In the remaining three, the severity of the stenosis was the same. In one patient, there was an apparent artifactual narrowing at the carotid bifurcation on the 2D TOF MR angiogram. On the contrast-bolus–tracking 3D MR angiogram, the same carotid bifurcation appeared normal (Fig 4).
fig 4.

A, MIP projection of the left carotid bifurcation acquired from a female patient with suspected moderate narrowing (arrow) using 2D TOF MR angiography (TR/TE = 22/7, flip angle = 60°).
B, The MIP projection acquired using subtracted 3D dynamic keyhole turbo field-echo MR angiography (TR/TE = 6/3, flip angle = 50°) shows a patent left carotid bifurcation.
Discussion
Turbo field-echo is a gradient-echo readout technique that allows fast imaging at very short TRs and TEs, before steady-state conditions are reached (both longitudinal and transverse) (9, 10). Characteristically, a flip angle sweep is implemented with gradual increase toward the chosen nominal flip angle. The nature of the flip angle sweep depends on the number of phase-encoding steps, the number of shots, the nominal flip angle, and the type of phase-encode profile order (linear versus centric). With turbo field-echo readout, nonuniform weighting of data along the phase-encode axis results from sampling at varying flip angles and at non–steady-state conditions.
Keyhole schemes also improve time resolution in dynamic imaging. This is achieved by sampling the high (responsible for image detail) and low (responsible for image contrast) spatial frequency data for the reference image and updating only the low spatial frequency data for the dynamic images. Combining the high spatial frequency data from the reference image with the low spatial frequency dynamic data sets results in a series of high-resolution dynamic images (11).
The combination of turbo field-echo readout and keyhole schemes allowed fast dynamic 3D MR imaging (3.6 seconds per dynamic volume) with adequate depiction of the carotid bifurcations and time separation of the arteries from veins in every patient examined. The adequate time separation of the arteries from the veins is due to the fact that the temporal resolution of this sequence approaches the lower limits of the published range of cerebral arteriovenous circulation time (12).
Like other contrast-enhanced MR angiographic techniques, 3D dynamic keyhole turbo field-echo MR angiography seems to be less sensitive to TOF-related artifacts (Fig 4). This is partially because contrast-enhanced MR angiography is less dependent than TOF MR imaging on the inflow of unsaturated spins for the production of the angiographic contrast.
Because of limited gradient speed on our MR scanner, relatively low spatial resolution is used to achieve dynamic imaging that is fast enough to reliably time-resolve the arteries from the veins. The relatively large partition thickness and pixel size can have a deleterious effect on image quality, particularly with regard to accurate representation of stenoses of subvoxel dimensions. Smaller voxel size, at the expense of longer acquisition time, combined with contrast-bolus detection techniques (such as fluoroscopic triggering) may allow higher resolution imaging of the carotid arteries without venous contamination.
On MR systems with fast imaging gradients (echo-planar capability), further reduction in acquisition time per dynamic image can be achieved owing to shorter TRs and TEs. This improvement in time resolution can be traded off for better in-plane spatial resolution, thinner partitions, or greater coverage (ie, larger 3D volume). High spatial- and time-resolution dynamic MR angiography will undoubtedly improve depiction of severe carotid stenosis and the string sign.
Further investigation is needed to study the effects of nonuniform weighting of data along the phase-encode axis and increased bandwidth considerations inherent to turbo field-echo readout as well as the effects of different keyhole schemes, including variable degrees of k-space truncation and the choice of reference image (before versus after the arrival of contrast material) on image quality (spatial resolution and signal-to-noise ratio).
Conclusion
Contrast-bolus–tracking digital subtraction 3D MR angiography using a combination of turbo field-echo readout and keyhole scheme techniques can reliably time-resolve carotid arteries from jugular veins. Also, it has the potential to more accurately represent vascular luminal narrowing as compared with TOF MR angiography.
Footnotes
Supported in part by a research grant from Philips Medical Systems, Shelton, CT.
Address reprint requests to Elias R. Melhem, MD, Department of Radiology, The Johns Hopkins Medical Institution, 600 N Wolfe St, Baltimore, MD 21287.
References
- 1.Mayberg MR, Winn HR. Endarterectomy for asymptomatic carotid artery stenosis: resolving the controversy. JAMA 1995;273:1459-1461 [PubMed] [Google Scholar]
- 2.Masaryk AM, Ross JS, DiCello MC, et al. 3DFT MR angiography of the carotid bifurcation: potential and limitations as a screening examination. Radiology 1991;179:797-804 [DOI] [PubMed] [Google Scholar]
- 3.Blatter DD, Bahr AL, Parker DL, et al. Cervical carotid MR angiography with multiple overlapping thin-slab acquisition: comparison with conventional angiography. AJR Am J Roentgenol 1993;161:1269-1277 [DOI] [PubMed] [Google Scholar]
- 4.Urchuk SN, Plewes DB. Mechanisms of flow-induced signal loss in MR angiography. J Magn Reson Imaging 1992;2:453-462 [DOI] [PubMed] [Google Scholar]
- 5.Lin W, Haake EM, Smith AS. Lumen definition in MR angiography.. J Magn Reson Imaging 1991;1:327-336 [DOI] [PubMed] [Google Scholar]
- 6.Prince MR, Yucel EK, Kaufman JA, et al. Dynamic gadolinium-enhanced three-dimensional abdominal MR angiography. J Magn Reson Imaging 1993;3:877-881 [DOI] [PubMed] [Google Scholar]
- 7.Levy RA, Prince MR. Arterial-phase three-dimensional-contrast MR angiography of the carotid arteries. AJR Am J Roentgenol 1996;167:211-215 [DOI] [PubMed] [Google Scholar]
- 8.Korosec FR, Frayne R, Grist TM, et al. Time-resolved contrast-enhanced 3D MR angiography. Magn Reson Med 1996;36:345-351 [DOI] [PubMed] [Google Scholar]
- 9.Norris DG, Bottcher U, Leibfritz D. A simple method of generating variable T1 contrast images using temporally reordered phase encoding. Magn Reson Med 1990;15:483-490 [DOI] [PubMed] [Google Scholar]
- 10.Holsinger AE, Riederer SJ. The importance of phase-encoding order in ultra-short TR snapshot MR imaging. Magn Reson Med 1990;16:481-488 [DOI] [PubMed] [Google Scholar]
- 11.Jones RA, Haraldseth O, Muller TB, et al. K-space substitution: a novel dynamic imaging technique. Magn Reson Med 1993;29:830-834 [DOI] [PubMed] [Google Scholar]
- 12.Levy RA, Maki JH. Three-dimensional contrast-enhanced MR angiography of the extracranial carotid arteries: two techniques. AJNR Am J Neuroradiol 1998;19:688-690 [PMC free article] [PubMed] [Google Scholar]


