Abstract
Summary: Neurologic complications associated with inferior petrosal sinus sampling for adrenocorticotropic hormone in the diagnosis of Cushing syndrome are rare. Previously reported complications include brain stem infarction and pontine hemorrhage. We report a case of venous subarachnoid hemorrhage with subsequent acute obstructive hydrocephalus occurring during inferior petrosal sinus sampling for Cushing syndrome.
Inferior petrosal sinus (IPS) sampling for adrenocorticotropic hormone (ACTH) plays an important role in the assessment of patients with Cushing syndrome. The test is accurate in localizing the source of ACTH, particularly after ovine corticotrophin-releasing hormone (oCRH) stimulation (1). One initial report by Miller and Doppman (2) described the procedure as low risk, with no major complications in a series of 335 patients. Subsequently, several investigators, including Miller et al (3), reported the occurrence of neurologic complications after IPS sampling (4, 5). These included transient brain stem symptoms, pontine hemorrhage, and brain stem infarction. We now report a case of venous subarachnoid hemorrhage, which, to our knowledge, is the first reported occurrence during IPS sampling.
Case Report
A 62-year-old woman had a 2-year history of clinical characteristics and physical appearance strongly suggestive of Cushing syndrome, including obesity, proximal muscle weakness, facial plethora, hypertension, depression, diabetes mellitus, and osteoporosis. Serum cortisol and serum ACTH were elevated. There was suppression on high-dose but not low-dose dexamethasone. Because of the marked elevation of baseline ACTH levels and the failure of extensive MR and CT examinations to locate the source of its production, IPS sampling was undertaken.
IPS sampling for ACTH was performed via a bilateral femoral vein approach. A 5.8F catheter was positioned in each internal jugular vein. After the administration of 4000 U of heparin, a Tracker 18 microcatheter (Target Therapeutics, Fremont, CA) was positioned into a channel of the left IPS. To position the microcatheter within the right IPS, however, an anomalous IPS/condylar vein complex joining the right internal jugular vein in the mid-cervical region had to be catheterized. Catheter position was confirmed with hand injection of contrast material and digital subtraction angiography. Sampling for ACTH before and after administration of oCRH was performed in standard fashion (2).
Before the procedure, the patient reported a mild headache and nasal congestion. Approximately 20 minutes into the procedure, during catheter placement, her systolic blood pressure rose to 190 mm Hg, and elevation persisted through the duration of the procedure, measuring 170 to 180 mm Hg (average baseline blood pressure, 140 mm Hg systolic). She also stated that her headache increased during the procedure. Over the course of 3.75 hours, the patient received a total of 100 μg fentanyl and 10 mg midazolam. She was drowsy after the procedure but oriented and without neurologic deficits. Owing to her decreased mental status she was transferred to a monitored care area for close observation. After arrival, she was noted to be restless and oriented only to person. Within the next 2 hours, her mental status deteriorated further and she became unresponsive.
Physical examination revealed minimal flexion in response to noxious stimuli, spontaneous respirations, and reactive 2-mm pupils. Her Glasgow Coma Scale score was 5. No improvement was noted after administration of naloxone and flumazenil. An emergency CT study of the head showed extensive subarachnoid and intraventricular hemorrhage mixed with contrast material and acute obstructive hydrocephalus (Fig 1).
fig 1.
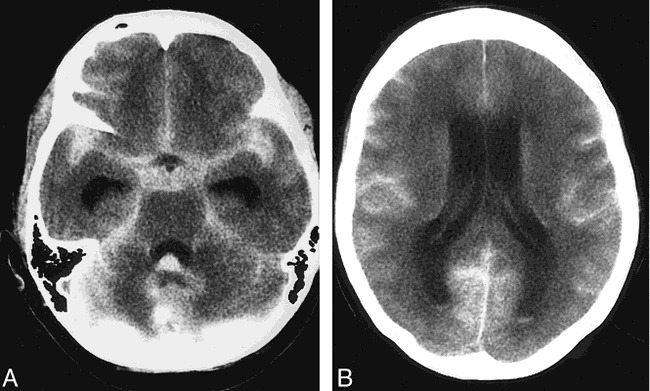
62-year-old woman with venous subarachnoid hemorrhage after IPS sampling.
A and B, CT scans of the head performed approximately 2.5 hours after IPS sampling show generalized ventriculomegaly. There is diffuse subarachnoid hemorrhage mixed with residual intravenous contrast material bilaterally. A small amount of blood and contrast material is seen in the dependent portions of the lateral and fourth ventricles.
The patient was emergently intubated and hyperventilated. A percutaneous external ventricular drain was placed in the right lateral ventricle. During placement, intracranial pressure was noted to be markedly elevated. Shortly after placement of the ventricular drain the patient's condition began to improve. She was extubated on the following day. Her mental status continued to improve. A cerebral angiogram showed no evidence of intracranial aneurysm or vascular malformation. The ventricular drain was removed 11 days after IPS sampling. However, 10 days later (21 days after IPS sampling), she experienced difficulty with walking and cognition. A head CT study was performed, which showed ventriculomegaly consistent with communicating hydrocephalus. A ventriculoperitoneal shunt was then placed.
The patient underwent a transsphenoidal exploration. No tumor was identified. Because the IPS showed elevated ACTH on the right, the patient had a hemihypophysectomy on the right. No tumor was found on frozen section, and a total hyposectomy was subsequently performed. The patient's cortisol levels were still elevated 1 month later and a bilateral adrenalectomy was performed.
After approximately 2 months of hospitalization, the patient was discharged. She requires a walker for ambulation and has diplopia attributed to divergence insufficiency, which is adequately treated with a prism. A follow-up MR study showed small foci of T2 signal abnormalities in the middle cerebellar peduncles, right cerebellar hemisphere, basal ganglia, and periventricular white matter, and resolution of her hydrocephalus.
Discussion
Initially believed to be a procedure with little risk, IPS sampling has since been reported to have been associated with neurologic complications in several patients, all involving brain stem injury. These neurologic complications are rare, however, occurring in one (0.2%) of 508 patients undergoing IPS sampling in one large series (3). Our case of subarachnoid hemorrhage was the only neurologic complication in a series of 94 procedures (1.1%) at our institution.
Miller et al (3) described two cases of brain stem injury: a brain stem infarction and a pontine hemorrhage. In addition, these investigators described their experience with two cases of transient brain stem symptoms that had no lasting sequela. The only common factor among the complications was the use of a catheter designed specially for IPS sampling; nevertheless, it is uncertain what role, if any, the catheter played in causing the complications. There have been two additional reports of brain stem injury, one involving a brain stem infarction at the pontocerebellar junction in a 45-year-old woman (4) and the other involving brain stem infarction in a 14-year- old boy (5). In all these cases, it is postulated that temporary increase in venous pressure resulted in venous infarction.
Our case of a venous subarachnoid hemorrhage with subsequent acute hydrocephalus occurred with the use of Tracker 18 microcatheters positioned in the IPS. At our institution, a 5.8F catheter and Tracker 18 microcatheter system is currently used in IPS sampling. The 5.8F catheters remain in the internal jugular vein whereas the microcatheters are advanced into the IPS. Catheterization of the right IPS in this patient was difficult, in part because of an anomalous IPS/condylar vein complex that joined the internal jugular vein in the mid-cervical region, but we have experienced similar difficult catheterizations in the past, without sequela. The microcatheters were not wedged in the IPS and careful hand injection of contrast material was performed both before and after sampling, as is standard in all our cases. The 5.8F catheter and microcatheter system had been used uneventfully for approximately 4 years for bilateral IPS sampling in 59 procedures. However, in this case, we speculate that venous perforation may have occurred during placement of the microcatheter.
Vigilance for the subtle signs and symptoms of impending brain stem injury has been emphasized by previous investigators (3, 4). These signs and symptoms may occur at the time of catheterization and can include hemifacial paresthesias, dysarthria, difficulty swallowing, or elevation in blood pressure. However, venous SAH can have an insidious onset that is ambiguous until obstructive hydrocephalus occurs. The resultant decreased level of consciousness may be similar to that seen with the side effects of sedation, as our patient.
Conclusion
In addition to brain stem ischemia/hemorrhage, venous subarachnoid hemorrhage is a potential but remote complication of IPS sampling. The cases presented in the literature and our own experience suggest there are no factors that predict which patients will experience neurologic complications (3, 4).
Footnotes
Address reprint requests to John Huston III, MD, Department of Diagnostic Radiology, Mayo Clinic, 200 First St SW, Rochester, MN 55902.
References
- 1.Oldfield E, Doppman JL, Nieman L, et al. Petrosal sinus sampling with and without corticotorphin-releasing hormone for the differential diagnosis of Cushing's syndrome. N Engl J Med 1991;325:897-905 [DOI] [PubMed] [Google Scholar]
- 2.Miller DL, Doppman JL. Petrosal sinus sampling: technique and rationale. Radiology 1991;178:37-47 [DOI] [PubMed] [Google Scholar]
- 3.Miller DL, Doppman JL, Peterman SL, et al. Neurologic complications of petrosal sinus sampling. Radiology 1992;185:143-174 [DOI] [PubMed] [Google Scholar]
- 4.Sturrock ND, Jeffcoate WJ. A neurological complication of inferior petrosal sinus sampling during investigation for Cushing's disease: a case report. J Neurol Neurosurg Psychiatry 1997;62:527-528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seyer H, Frisch H, Fahlbusch R, et al. Raymond's syndrome following petrosal sinus sampling. Acta Neurochir (Wein) 1994;131:157-159 [DOI] [PubMed] [Google Scholar]


