Abstract
Summary: Distal aneurysms of the cerebellar arteries are associated with a poor prognosis, as surgery or embolization with GDCs is very difficult. We report our experience with a new therapeutic method involving intraaneurysmal injection of glue. Three aneurysms were catheterized with a flow-guided microcatheter, and glue was slowly injected into the aneurysms. In two cases, treatment resulted in total occlusion of the aneurysm with preservation of the parent artery. In one case, the aim was to occlude both the aneurysm and parent artery.
Aneurysms in the distal cerebellar arteries are rare (1–5). The ability to treat them surgically depends on the location of the aneurysm, but surgery is considered difficult and is associated with a rather high morbidity/mortality rate (4, 5). Embolization with Guglielmi detachable coils (GDCs, Target Therapeutics, Fremont, CA) may be difficult or impossible because of the distal location of the aneurysm or because of the unfavorable ratio between the size of the aneurysm and the size of the parent vessel. We propose a new method to occlude such aneurysms by means of intraaneurysmal injection of glue.
Case Reports
Case 1
A 39-year-old man sought medical attention for frequent headaches. MR imaging disclosed a right posterior inferior cerebellar artery (PICA) aneurysm. Findings at neurologic examination were normal. Cerebral angiography confirmed a distal PICA aneurysm at the telovelotonsillar (cranial loop) bifurcation of the PICA, in its hemispheric and vermian branches (Fig 1A). Subtracted rotational angiography revealed a wide aneurysmal neck. Initially, endovascular treatment with GDCs was considered; however, we anticipated several problems with that technique. First, we thought it would be difficult to catheterize the aneurysm with the microcatheter we normally use for this purpose, the Tracker 10 (Target Therapeutics), owing to the very distal location of the aneurysm. Second, because of the great width of the aneurysmal neck and the small diameter of the parent artery, occlusion of the aneurysm with GDCs would most likely have resulted in protrusion of the coils, resulting in occlusion of the distal hemispheric branch of the PICA. Consequently, we decided on endovascular treatment with injection of glue.
fig 1.
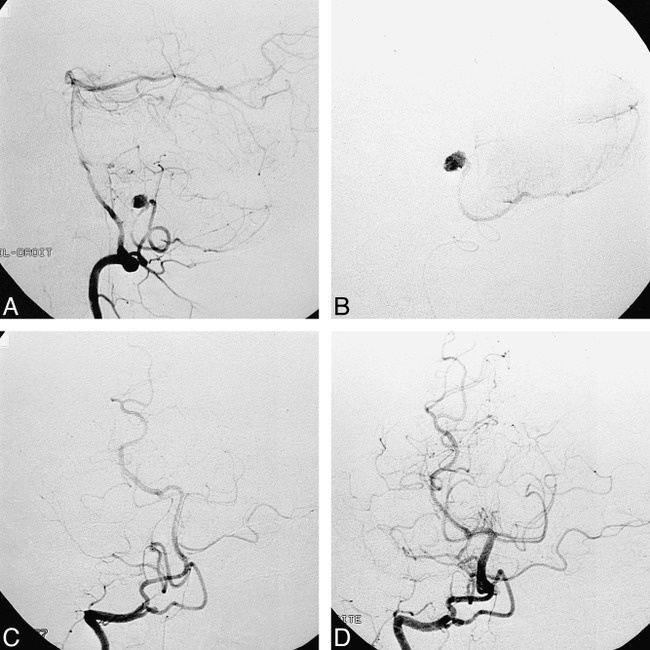
Case 1: 39-year-old man.
A, Right vertebral injection, lateral view, shows aneurysm located at the telovelotonsillar segment (cranial loop) bifurcation of the PICA in its hemispheric and vermian branches.
B, Intraaneurysmal contrast injection, lateral view, shows opacification of the aneurysm and progressive filling of the hemispheric branch.
C, Postembolization right vertebral injection, anteroposterior view, shows occlusion of the aneurysm with a small remnant at the level of the neck.
D, 7-month follow-up right vertebral injection, anteroposterior view, shows complete occlusion of the aneurysm, with no visible neck remnant. The distal PICA appears normal.
A 6F guiding catheter was introduced, with its tip placed in the right vertebral artery. Through the guiding catheter, the distal PICA was catheterized with a flow-guided Magic 1.8F microcatheter (Balt Extrusion, Montmorency, France) directed by a 0.010F microguidewire (Terumo, Tokyo, Japan). The tip of the microcatheter was gently introduced into the aneurysm. Slow injection of contrast material caused the neck of the aneurysm to become well defined (Fig 1B) and enabled progressive filling of the aneurysm as well as further opacification of the distal PICA. This close control of flow inside the aneurysm encouraged us to proceed with the injection of glue. A mixture of 1 mL Histoacryl (Braun, Melsungen, Germany) and 2 mL iodized oil (Lipiodol, Andre Guerbert, Aulnay sous Bois, France) was prepared in a 3-mL Luer-Lok syringe and injected into the aneurysm very slowly. Control angiography showed occlusion of the aneurysm with preservation of the parent artery and normal flow in the distal hemispheric branch. A small remnant of the aneurysm was seen at the level of the neck (Fig 1C). Upon waking from anesthesia, the patient was asymptomatic and was discharged 3 days later. Follow-up angiography at 7 months showed complete occlusion of the aneurysm with no visible neck remnant (Fig 1D). The patient is scheduled for a 2-year follow-up angiogram to confirm the stability of the result.
Case 2
A 38-year-old woman presented with sudden severe occipital headaches. On admission, she was drowsy and had marked neck stiffness but was otherwise without neurologic deficits (Hunt and Hess grade II). A CT scan showed subarachnoid hemorrhage with blood in the fourth ventricle. Cerebral angiography revealed an aneurysm located at the telovelotonsillar segment of the PICA (Fig 2A). Endovascular treatment by glue injection was considered preferable to GDC embolization because of the very distal location of the aneurysm.
fig 2.
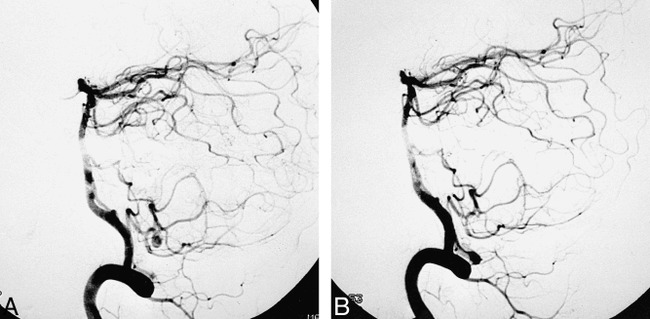
Case 2: 38-year-old woman.
A, Right vertebral injection, lateral view, shows aneurysm located at the telovelotonsillar segment bifurcation of the PICA, in its hemispheric and vermian branches.
B, Postembolization right vertebral injection, lateral view, shows complete occlusion of the aneurysm with normal-appearing distal PICA.
The tip of a Magic 1.8F microcatheter was gently placed inside the aneurysm. Slow injection of diluted contrast material allowed good control of flow within the aneurysm, with slow opacification of the aneurysmal sac and secondary filling of the distal PICA. By slowly injecting 0.2 mL of a mixture of one third Histoacryl and two thirds Lipiodol, we obtained complete occlusion of the aneurysm with preservation of the parent artery (Fig 2B). The patient rapidly recovered after the procedure. A 3-month follow-up angiogram showed persistent total occlusion of the aneurysm and a normal-appearing distal PICA. The patient is scheduled for a 2-year follow-up angiogram to confirm the stability of the result.
Case 3
A 44-year-old woman had sudden onset of headaches associated with mild left-sided hypoesthesia and varying degrees of consciousness. On admission, she was stuporous with a left-sided cerebellar syndrome and a stiff neck (Hunt and Hess grade III). A CT scan showed diffuse subarachnoid hemorrhage. Cerebral angiography revealed a wide-necked aneurysm located distally in the hemispheric branch of the right superior cerebellar artery (Fig 3A). Significant stagnation of contrast medium was noted within the aneurysm, with delayed filling of the distal segment of the artery. Severe vasospasm of the basilar artery was also noted.
fig 3.
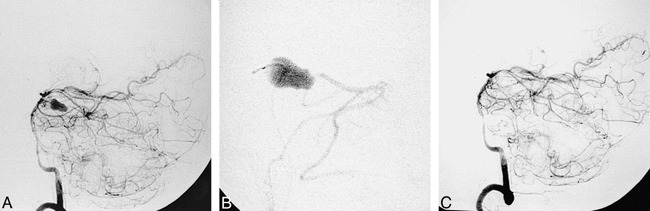
Case 3: 44-year-old woman.
A, Left vertebral injection, lateral view, shows distal aneurysm in the hemispheric branch of the right SCA.
B, Intraaneurysmal contrast injection, lateral view, shows opacification of the aneurysm. Note absence of an aneurysmal neck and filling of the distal branch.
C, Postembolization left vertebral injection, lateral view, shows occlusion of the aneurysm and parent artery. Proximal SCA segment is not opacified owing to spasm caused by withdrawal of the microcatheter.
Owing to the distal location and wide neck of the aneurysm, the therapeutic strategy in this case was to occlude both the aneurysm and the parent vessel by glue injection. To achieve microcatheterization of the distal superior cerebellar artery and the aneurysm, we first slowly injected 150 mg of papaverine intraarterially through the microcatheter (Magic 1.8F), which was positioned in the basilar artery. Thereafter, microcatheterization of the aneurysm was performed with ease. The wide neck of the aneurysm was well defined by the intraaneurysmal contrast injection (Fig 3B). Slow injection of 0.4 mL of a mixture of one third Histoacryl and two thirds Lipiodol enabled complete occlusion of the aneurysm as well as of the parent artery (Fig 3C). Upon waking from general anesthesia, the patient was clinically unchanged. Eight hours later, she had a slight left-sided hemiparesis, which completely resolved within 3 days.
Discussion
Aneurysms located in the distal intracranial vessels are rare. Distal aneurysms represent approximately 7% to 9% of anterior cerebral artery aneurysms, 2% to 7% of middle cerebral artery aneurysms, and 5% of posterior cerebral artery aneurysms (6). Aneurysms of the distal superior cerebellar artery (SCA) and PICA are rare. Locksley et al (1), in a series of 2349 intracranial aneurysms, found six aneurysms of the SCA (0.3%) and 11 of the PICA (0.5%). Gacs et al (2), in a surgical series of 910 vertebrobasilar aneurysms, reported six distal aneurysms of the SCA (0.7%) and eight aneurysms of the PICA (0.9%).
The poor prognosis in patients with ruptured intracranial aneurysms of the posterior circulation was documented in 1995 by Schievink et al (6). In their series, the 48-hour survival rate was 32% for aneurysms of the posterior circulation and 77% for aneurysms of the anterior circulation. The 30-day survival rate was 11% and 53%, respectively.
Outcome after surgery, depending on the location of the aneurysm, has been reported by several investigators. Andoh et al (5) analyzed 15 cases of aneurysms on the distal PICA (12 cases disclosed by subarachnoid hemorrhage), the majority of them located at the telovelotonsillar segment. They reported good recovery in 10 patients (67%) and a fair result in one patient (7%). Three patients (20%) died, and recurrent bleeding occurred in three patients. Nishizaki et al (3), in a review of the surgical literature, reported good results in 82% of the cases and a fair result in 8%; 10% of the patients died as a result of the procedure. Gacs et al (2) reported 16 patients with distal cerebellar aneurysms, all of whom were in good clinical condition when they underwent surgery. The final outcome was considered excellent or good in 11 cases (69%) and poor in four cases (25%). One patient died during surgery for two PICA aneurysms associated with an arteriovenous malformation (AVM).
Since the introduction of GDCs, endovascular treatment has become the standard method of managing aneurysms considered to be unclippable. Today, it is generally believed that ruptured or unruptured aneurysms in the posterior circulation may be treated with GDCs, with a low morbidity/mortality risk as compared with surgery. The main limitation to this treatment is the morphology of the aneurysm: the presence of a wide neck being the most important limitation. The remodeling technique, introduced by Moret et al (7), has extended the indication for endovascular treatment of intracranial aneurysms without increasing the risk incurred by the procedure. The technique consists of the temporary inflation of a balloon in front of the neck of the aneurysm during deposition of every coil. Despite these new techniques, some aneurysms still remain untreatable with GDCs.
In our three cases of distal cerebellar artery aneurysms, we judged GDC treatment to be unsuitable for several reasons. Microcatheterization with a Tracker 10 would have been impossible or very difficult, at least in cases 1 and 2. The aneurysms in these cases were located at the telovelotonsillar segment of the PICA, and acute loops of the proximal PICA would most likely have made microcatheterization impossible. Moreover, coil embolization would probably have caused occlusion of the parent artery, considering the broad neck of the aneurysm relative to the small diameter of the parent artery (8). In case 3, the absence of an aneurysmal neck made selective treatment with GDCs impossible. Considering these likely problems in using GDCs, we therefore decided to try to occlude these aneurysms with glue.
Microcatheterization was performed with the use of a flow-guided microcatheter (Magic 1.8F) directed by a 0.010F microguidewire (Terumo). In each case, the procedure was easy and rapid. The tip of the microcatheter, which was shaped with steam, was placed inside the microcatheter and kept there. The microcatheter was slowly pushed over the wire, with the tip never coming in contact with the aneurysmal wall. With this technique, catheterization of the aneurysmal sac is completely atraumatic. The aim of embolization in each case was initially to occlude the aneurysm and the parent artery in front of the aneurysmal neck. Otherwise, the proximal portion of the PICA/SCA, as well as the perforating arteries arising from these arterial segments, would remain patent and the distal segments of the SCA/PICA would be retrogradely vascularized from the very rich pial collateral circulation. In cases 1 and 2, the slow injection of contrast material inside the aneurysm allowed us to obtain progressive filling of the aneurysm. This good control of flow inside the aneurysm encouraged us to glue only the aneurysm and to try to preserve the parent artery. The glue solution (a mixture of 1 mL Histoacryl and 2 mL Lipiodol) was injected very slowly with a 3-mL Luer-Lok syringe, resulting, in all cases, in complete occlusion of the aneurysm with preservation of the parent artery and normal flow in the distal hemispheric branches. In case 3, a superselective injection of contrast material confirmed what we had noted earlier, that is, the absence of an aneurysmal neck. We therefore decided to occlude the parent artery as well by intentionally spilling glue from the sac of the aneurysm into the parent artery.
Several authors have reported the results of experimentally occluded aneurysms using cyanoacrylate, either by direct puncture of the aneurysm or by an endovascular approach (9, 10). The major drawback reported in these studies has been the large number of distal embolizations of cyanoacrylate into normal vessels. Fox et al (11) reported the results from three patients with cerebral aneurysms who were treated with isobutyl 2-cyanoacrylate combined with calibrated-leak balloons. All treatments resulted in major infarction and death. Szikora et al (12) reported good results from the injection of N-hexyl-cyanoacrylate in experimental aneurysms under the protection of a stent previously deposited in the parent artery. The stent allowed good control of the blood flow inside the aneurysms and thus safer filling of glue inside the aneurysm.
In our cases, the aim was initially to occlude both the aneurysm and the parent artery. Nonetheless, from the superselective contrast studies in cases 1 and 2, we found that we had good control of the blood flow inside the aneurysms and hence changed our strategy to aim at selective occlusion of the aneurysm only.
The mixture of glue we used, one third Histoacryl and two thirds Lipiodol, is what we now frequently use when embolizing brain AVMs. It allows us to inject the glue mixture slowly and with good control of the polymerization. As when embolizing direct fistulas in cases of brain AVMs, the tip of the microcatheter should be in contact with the wall of the aneurysm (the vessel in cases of AVMs). Because of this contact, the first drop of glue will stick to the wall. Very slow injection of the glue will allow the collected mass to progress along and stick to the entire wall of the aneurysm, thus, enabling complete filling of the aneurysm while preserving the parent artery.
The technique allows easy and safe catheterization of an aneurysm using a flow-guided microcatheter, the tip of which is flexible and therefore atraumatic. The risk of rupture of the aneurysm during embolization is extremely low, primarily because the glue is injected very slowly into the aneurysm and secondarily because no manipulation is required as compared with the GDC technique.
We would expect even fewer problems in the long term regarding compaction of the intraaneurysmal device with glue as compared with coils. However, this has to be further analyzed in larger series.
The two major drawbacks of the technique are distal migration of glue to normal arteries and reflux of glue into the feeding pedicle. The first may be avoided by establishing control of flow inside the aneurysm.
We advocate the use of this technique only in cases of very distally located aneurysms in small arteries, in which accidental occlusion of the parent artery at the level of the aneurysmal neck would not be critical because of good collateral circulation. Reflux of glue into the feeding pedicle has to be avoided by injecting the glue very slowly. A small reflux of glue in our case 3 was the probable cause for the slight left-sided hemiparesis observed 8 hours after the procedure; however, this completely resolved within 3 days.
Conclusion
Occlusion of intracranial aneurysms of the distal cerebellar arteries by means of intraaneurysmal injection of glue may be a safe and efficient alternative to surgery or endovascular treatment with GDCs. Control of blood flow within the aneurysm is essential in order to preserve the parent artery and avoid reflux of glue into the feeding pedicle. Significant experience and skill in glue injection of brain AVMs is mandatory for obtaining perfect control of the procedure. Further experimental studies will be needed to assess whether occlusion of aneurysms, whatever their location, with glue can become an established therapeutic approach. Gaining control of intraaneurysmal blood flow will be a critical factor in widening the indications for the technique.
Footnotes
Address reprint requests to Christophe Cognard, MD, Service de Neuroradiologie, Hopital Purpan, Place du Dr Baylac, 31059 Toulouse Cedex, France.
References
- 1.Locksley HB. Report on the cooperative study of intracranial aneurysms and subarachnoid hemorrhage, section V, part 1: natural history of subarachnoid hemorrhage, intracranial aneurysms and arterio-venous malformations; based on 6368 cases in the cooperative study. J Neurosurg 1966;25:219-239 [DOI] [PubMed] [Google Scholar]
- 2.Gacs G, Vinuela F, Fox AJ, Drake CG. Peripheral aneurysms of the cerebellar arteries: review of 16 cases. J Neurosurg 1983;58:63-68 [DOI] [PubMed] [Google Scholar]
- 3.Nishizaki T, Tamaki N, Nishida Y, Fujita K, Matsumoto S. Aneurysms of the distal postero inferior cerebellar artery: experience with three cases and review of the literature. Neurosurgery 1985;16:829-832 [DOI] [PubMed] [Google Scholar]
- 4.Spallone A, De Santis S, Giuffre R. Peripheral aneurysms of the anterior inferior cerebellar artery: case report and review of literature. Br J Neurosurg 1995;9:537-541 [DOI] [PubMed] [Google Scholar]
- 5.Andoh T, Itoh T, Yoshimura S,, et al. Peripheral aneurysms of the posterior inferior cerebellar artery: analysis of 15 cases. No Shinkei Geka 1992;20:683-690 [PubMed] [Google Scholar]
- 6.Schievink WI, Wijdicks EF, Piepgras DG, Chu-Pin Chu, O'Fallon M, Whisnant JP. The poor prognosis of ruptured intracranial aneurysms of the posterior circulation. J Neurosurg 1995;82:791-795 [DOI] [PubMed] [Google Scholar]
- 7.Moret J, Cognard C, Weill A, Castaings L, Rey A. The “remodelling technique” in the treatment of wide neck intracranial aneurysms. Intervent Neuroradiol 1997;3:21-35 [DOI] [PubMed] [Google Scholar]
- 8.Chaloupka JC, Putman M, Awad IA. Endovascular therapeutic approach to peripheral aneurysms of the superior cerebellar artery. AJNR Am J Neuroradiol 1996;17:1338-1342 [PMC free article] [PubMed] [Google Scholar]
- 9.Sheptak PE, Zanetti PH, Susen AF. The treatment of intracranial aneurysms by injection of a tissue adhesive. Neurosurgery 1977;1:25-29 [DOI] [PubMed] [Google Scholar]
- 10.Kerber CW, Cromwell LD, Zanetti PH. Endovascular treatment with cyanoacrylate. Neurosurgery 1985;16:13-17 [PubMed] [Google Scholar]
- 11.Fox AJ. Detachable calibrated leak balloon with IBCA/NBCA for treatment of aneurysm. AJNR Am J Neuroradiol 1992;13:1452-1453 [Google Scholar]
- 12.Szikora I, Guterman LR, Standard SC, Wakhloo AK, Hopkins LN. Endovascular treatment of experimental aneurysms with liquid polymers: the protective potential of stents. Neurosurgery 1996;38:339-347 [DOI] [PubMed] [Google Scholar]


