Abstract
Summary: Endovascular treatment of carotid cavernous fistulas (CCFs) presents many technical difficulties and hazards, some unique to each patient. This report details some of the difficulties encountered in the treatment of a 63-year-old patient with a CCF and an ipsilateral internal carotid artery dissection. After failure of conventional techniques using a detachable balloon, complete closure of the CCF was achieved by transvenous coil embolization while the arterial lumen was protected by a nondetachable balloon catheter.
Posttraumatic carotid cavernous fistulas (CCF) most often develop in association with injury to the skull base, resulting in laceration of the internal carotid artery (ICA) (1–3). Spontaneous CCFs usually are related to rupture of an aneurysm of the cavernous segment of the ICA. The most serious complications and symptoms of a CCF are those associated with venous hypertension transmitted either to the eye or to the brain, depending on the available routes of venous drainage. Preferred treatment of CCFs in recent years has been predominantly by endovascular techniques. Ideally, endovascular treatment of a CCF aims to occlude the fistula while preserving flow in the parent carotid artery (3). In some situations, this can prove impossible or hazardous, and alternative endovascular techniques may have to be contrived. Transarterial occlusion of the fistula may be performed either with balloons or coils (4). Occasionally, it may be necessary to sacrifice the parent vessel. Transvenous access to the cavernous sinus for coil occlusion of the fistula is most often achieved via the inferior petrosal sinus, but can also be accomplished via the superior ophthalmic vein (5, 6).
This report describes a modification of endovascular techniques used to occlude a CCF in a patient in whom conventional endovascular techniques failed.
Technique
A 63-year-old man was involved in a motor vehicle accident, which resulted in severe head trauma. After the accident, he was densely paralytic on the left side of his body. A head CT scan showed extensive subarachnoid hemorrhage and multiple fractures of the skull base. He was transferred to our hospital, where cerebral angiography was performed within 8 hours of the accident. This study revealed an endoluminal dissection flap in the right ICA (Fig 1A). However, flow to the intracranial circulation across the dissection was prompt. No occluded intracranial vessels could be seen, but there was evidence of a fistula from the cavernous segment of the right ICA to the cavernous sinus. The rate of flow through the CCF was moderate at the time of the first angiogram, and because of the right hemispheric infarction and other injuries, a decision regarding treatment of the CCF was deferred.
fig 1.
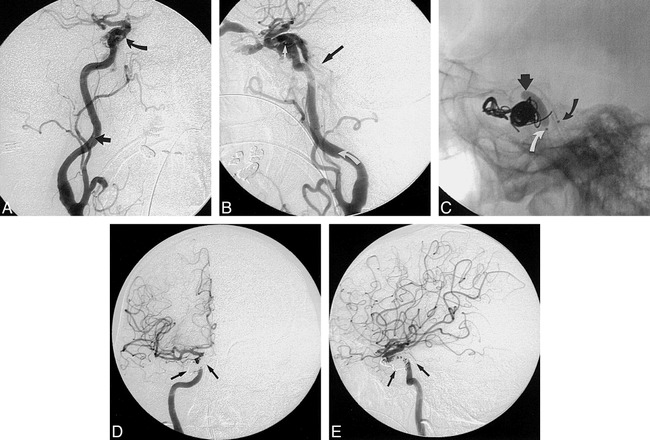
63-year-old man with a CCF and an ipsilateral ICA dissection.
A, Anteroposterior view of the right common carotid artery injection shows a spiral flap within the cervical ICA (straight arrow). Early opacification (curved arrow) of the cavernous sinus indicates the presence of a CCF.
B, Lateral view of the right ICA (treatment day 2) shows that the CCF is completely reopened. Artifact from the gold marker of the deflated latex balloon (straight white arrow) indicates that the balloon has not moved but is situated close to the carotid artery. The dissection flap of the ICA is well seen on this projection (curved white arrow). The inferior petrosal sinuses (black arrow) opacify promptly, indicating ease of transvenous access to the cavernous sinus via this route.
C, Lateral projection of a still image taken during coil deployment in the cavernous sinus. The Endeavor balloon (straight arrow) is inflated across the laceration of the ICA. A number of fibered and nonfibered GDCs have been deployed within the cavernous sinus via a two-marker microcatheter. The coils are beginning to assume a complex disposition in a 3D configuration around the ICA. The marker of the balloon catheter (curved white arrow) and the proximal marker of the double-marker microcatheter (curved black arrow) lie close together but within different anatomic structures, the ICA and inferior petrosal sinus, respectively.
D and E, Anteroposterior (D) and lateral (E) views of the right ICA injection after complete occlusion of the CCF with coils. The complex disposition of the coils (arrows) within the cavernous sinus denies a profile view of the carotid artery. Use of the nondetachable balloon within the arterial lumen during coil deployment preserved the integrity of the arterial lumen and prevented inadvertent compromise of the artery.
Over the subsequent 2 weeks, the proptosis, chemosis, and bruit increased significantly, although intraocular pressure remained within normal range. A decision was made to treat the CCF by endovascular techniques.
At the first treatment session, initial angiograms showed that the CCF had increased considerably in flow rate as compared with the images obtained 2 weeks previously. Venous drainage was through the ophthalmic veins and the petrosal sinuses. A long endoluminal dissecting flap was still evident in the right cervical ICA. The patient was heparinized to more than double the baseline activated clotting time (ACT). Through a 6F Envoy catheter (Cordis, Miami, FL) a #16 latex gold-valve balloon (Nycomed, France) was floated past the cervical ICA dissection and into the fistula site. The balloon was mounted on a red and black coaxial 2F/3F catheter system (Nycomed). Repeated attempts with balloon deflation and inflation were made to achieve a satisfactorily stable position for the balloon within the fistula. Unfortunately, the tear in the artery seemed to be so wide that complete occlusion required a volume of balloon inflation that resulted in unsatisfactory compromise of the parent vessel. A final run showed compromise of the ICA to a suboptimal degree, and it was decided to remove the #16 balloon. However, this proved impossible, because over the course of many deflations and inflations the valve had become unresponsive. Consequently, the balloon was detached in place, resulting in occlusion of the CCF and moderate compromise of the parent ICA. An attempt to augment the lumen of the parent artery was made by inflating a Solstice 3-mm balloon (MIS, Sunnyvale, CA) within the vessel alongside the latex balloon. Despite the degree of compromise of the parent vessel, flow to the right hemisphere seemed satisfactory. The patient was returned to the neurointensive care unit and continued on heparin therapy for a target partial thromboplastin time (PTT) of 40 to 60 seconds. Within a few hours of the procedure, the patient's eye was much improved in appearance. Chemosis and proptosis were improved considerably and the bruit was extinguished.
The following morning, the patient's eye appeared to have deteriorated overnight, and the bruit over the right eye had returned loudly. An assumption that the latex balloon had deflated prematurely was confirmed angiographically, while the metallic marker of the deflated latex balloon could still be seen immediately adjacent to the carotid artery (Fig 1B). Because of the extreme difficulties encountered during transarterial balloon placement on the previous day and the risks of transarterial catheterization across the right ICA dissection, a transvenous route of treatment was chosen on this occasion. The venous route to the cavernous sinus was catheterized with a Tracker 18 double-marker Turbo-Tracker (Target, Fremont, CA) and placed via the ipsilateral inferior petrosal sinus. Using electrolytically detachable coils (GDCs), an attempt to build a coil mesh within the cavernous sinus was confounded by prolapse of coils into the ICA. Furthermore, the ease with which this occurred caused concern that coil pressure might push the deflated latex balloon into the ICA and cause a distal embolus.
To protect the ICA and to facilitate coil placement within the cavernous sinus, a variation of the balloon reconstructive technique recently described (7) for aneurysm treatment was improvised. The patient was heparinized to two to three times baseline ACT. Through an introducer catheter in the right common carotid artery, an Endeavor nondetachable silicone balloon (Target) was floated past the cervical ICA dissection. An attempt to inflate this balloon at the fistula site was hampered by the sump of the CCF, which tended to draw the inflating balloon into the cavernous sinus completely. Therefore, the relatively straight Endeavor balloon was advanced in a deflated state past the arterial tear, partially inflated, and then pulled back across the fistula, inflating gently all the while, until complete coverage of the fistulous tear was obtained (Fig 1C). This allowed the first GDC, a 12 mm × 20 cm coil, to be deposited satisfactorily. The Endeavor balloon was then deflated to allow resumption of forward flow in the carotid artery, and the coil was detached. The procedure was then repeated with a number of standard-type GDCs, later switching to fibered GDCs. With each coil placement, the balloon within the carotid artery was inflated and deflated.
Use of the balloon during this procedure continued to be of critical value longer into the process than was originally anticipated. As the mesh of coils within the cavernous sinus became more complex and dense, it assumed a 3D configuration wrapped around the ICA. Therefore, it became increasingly difficult to see the ICA in profile during coil deposition. The inflated balloon within the carotid artery facilitated the safe deposition of coils in a 3D mesh around the ICA (Fig 1D and E). This resulted in complete elimination of flow through the CCF and satisfactory preservation of the ICA. No emboli were identified. The duration of carotid occlusion during each balloon inflation was less than a minute. After the second procedure, the patient's eye seemed improved again and the bruit was eliminated. He was maintained on heparin for 48 hours after the procedure for a target PTT of 40 to 60 seconds.
Discussion
This case illustrates some of the considerable difficulties that can be encountered during endovascular occlusion of a CCF, and demonstrates an improvisational technique that ultimately proved easier to execute than conventional methods. Detachable balloon maneuvering in the ICA can pose difficulties with satisfactory balloon placement, as was the case with this patient. The mounting of the balloon on the microcatheter delivery system can result in its premature or inadvertent detachment, with distal migration to the cerebral vasculature. In this patient, numerous attempts at satisfactory balloon deployment probably caused balloon migration on the microcatheter to the point where the valve became occluded and deflation was not possible. Occasionally, balloons can be encountered with incompetent valves. The balloon used in this case had been tested for valve competence for approximately 5 minutes before mounting it on the microcatheter. However, the integrity of the valve may have become compromised during the deployment process, or it may have been damaged at the time of inflating the Solstice balloon beside it in an attempt to augment the compromised lumen of the artery.
The technique of using an endoluminal balloon for protection and preservation of the ICA described in this case is a variation of the reconstructive balloon technique for embolization therapy of intracranial aneurysms described by others (7–9). In contrast to the first procedure, in which a variety of technical difficulties and problems were encountered, the second procedure was remarkably easy. The two difficulties in the second procedure related to crossing the dissection in the carotid artery and maintaining a stable position across the arterial rent with the balloon. Aggravation of the carotid dissection was avoided by floating the Endeavor balloon up the carotid artery in a semiinflated (ie, flow-directed) state. The technique for placing the balloon across the arterial tear also proved satisfactory.
The long-term outcome of the treatment described here ought to prove satisfactory. The mesh of coils within the cavernous sinus should present an interface to the parent vessel similar to that achieved with endovascular coil occlusion of intracranial aneurysms. Therefore, while there is some risk of acute thromboembolic complications after the procedure, this risk can be reduced with heparinization and antiplatelet therapy. Furthermore, this technique avoids some of the difficulties and delayed complications associated with CCF occlusion using detachable balloons. When water-soluble contrast material is used to inflate intravascular detachable latex balloons for CCF occlusion or other purposes, a delayed spontaneous deflation of the latex balloon over some weeks is expected. This results in a rate of pseudoaneurysm or pouch formation at the site of the healed CCF as high as 30% (3). With dense coil packing in the cavernous sinus, the likelihood of a pseudoaneurysm of the carotid artery with the coil technique should be less, probably similar to that found after endovascular coil treatment of an arterial aneurysm. Comparative disadvantages of the technique described here would include the increased cost of materials associated with the use of numerous coils in the place of a single balloon. Additionally, patients in whom this technique might be considered must be studied carefully at first to avoid coil occlusion of critical parenchymal veins afferent to the cavernous sinus. In this patient, the risks of thromboembolic complications from endovascular balloon navigation requiring heavy heparinization (7) had to be balanced with the risks of extreme anticoagulation in the setting of subacute cerebral infarction. However, the procedure was technically easy to execute and no thromboembolic complications were encountered.
Conclusion
For patients with a wide-necked fistula in whom placement of a single balloon, or multiple balloons, seems impossible or hazardous, use of a nondetachable endoluminal balloon for protection and preservation of the parent artery may prove to be a useful alternative.
Footnotes
Address reprint requests to Pearse Morris, MB, BCh.
References
- 1.Phadke RV, Kumar S, Sawlani V, Mazumdar B, Guijral RB. Traumatic carotid cavernous fistula: anatomical variations and their treatment by detachable balloons. Australas Radiol 1998;42:1-5 [DOI] [PubMed] [Google Scholar]
- 2.Desal H, Leaute F, Auffray-Calvier E, et al. Direct carotid-cavernous fistula: clinical, radiologic and therapeutic studies, apropos of 49 cases. J Neuroradiol 1997;24:141-154 [PubMed] [Google Scholar]
- 3.Lewis AI, Tomsick TA, Tew JM. Management of 100 consecutive direct carotid cavernous fistulas: results of treatment with detachable balloons. Neurosurgery 1995;36:239-244 [DOI] [PubMed] [Google Scholar]
- 4.Siniluoto T, Seppanen S, Kuurne T, Wikholm G, Leinonen S, Svendsen P. Transarterial embolization of a direct carotid cavernous fistula with Guglielmi detachable coils. AJNR Am J Neuroradiol 1997;18:519-523 [PMC free article] [PubMed] [Google Scholar]
- 5.Gioulekas J, Mitchell P, Tress B, McNab AA. Embolization of carotid cavernous fistulas via the superior ophthalmic vein. Aust N Z J Ophthalmol 1997;25:47-53 [DOI] [PubMed] [Google Scholar]
- 6.Irie K, Fujiwara T, Kuyama H, Nagao S, Ohkawa M. Transvenous embolization of traumatic carotid cavernous fistula with mechanical detachable coils. Minim Invasive Neurosurg 1996;39:28-30 [DOI] [PubMed] [Google Scholar]
- 7.Moret J, Cognard C, Weill A, Castaings L, Rey A. Reconstruction technique in the treatment of wide-neck intracranial aneurysms: long-term angiographic and clinical results. J Neuroradiol 1997;24:30-44 [PubMed] [Google Scholar]
- 8.Mericle RA, Wakhloo AK, Rodriquez R, Guterman LR, Hopkins LN. Temporary balloon protection as an adjunct to endosaccular coiling of wide-necked cerebral aneurysms: technical note. Neurosurgery 1997;41:975-978 [DOI] [PubMed] [Google Scholar]
- 9.Levy DI, Ku A. Balloon-assisted coil placement in wide-necked aneurysms: technical note. J Neurosurg 1997;86:724-727 [DOI] [PubMed] [Google Scholar]


