Abstract
BACKGROUND AND PURPOSE: Because it diminishes the stiffness of the intervertebral disk, disk degeneration results in abnormal motions of the spine. Therefore, disk degeneration associated with back pain may indicate spinal fusion. The purpose of this study was to correlate the MR appearance and stiffness of lumbar intervertebral disks.
METHODS: Eighty-two lumbar spinal segments were imaged with MR. The intervertebral disks were classified as: 1) normal, 2) having transverse or concentric tears of the annulus fibrosus if MR imaging showed only these changes, 3) having radial tears of the annulus fibrosus if MR imaging showed high-intensity zones in the annulus fibrosus or reduced signal intensity in the disk characteristic of radial tears, or 4) having advanced degeneration if MR imaging showed markedly reduced height, large osteophytes, or both. The rotation occurring from the application of a 6.6-Newton-meter (Nm) moment of axial rotational torque was measured kinematically. Average stiffness, in Nm/degree, was calculated as the ratio of the torque to the rotation.
RESULTS: Stiffness averaged 7.0 Nm/degree for the normal group; 1.9 Nm/degree for the disks with concentric or transverse tears; 1.7 Nm/degree for disks with radial tears; and 3.1 Nm/degree for disks with advanced degeneration. The differences were statistically significant.
CONCLUSION: Concentric, transverse, and radial tears of the intervertebral disk indicate reduced stiffness of the intervertebral disk and increased motions for a unit of applied torque. The most severely reduced stiffness was found in disks with radial tears of the annulus fibrosus. With collapse of the disk space, stiffness increases.
One of the indications for spinal fusion is degenerative instability, which is diagnosed on the basis of characteristic pain and neurologic deficits and evidence of abnormal motions at one or more spinal levels (1). Criteria for diagnosing instability are still controversial (2). The criteria for abnormal motion are not established. The motions of the lumbar spine are often assessed with flexion and extension radiographs, but the reliability of these studies is questioned (3). Investigators have attempted to identify the MR appearances of the intervertebral disk that predict degenerative instability. In one study, decreased signal intensity in the vertebral endplates on T1-weighted images was a good predictor of a clinical diagnosis of instability (4). In another study, tears of the annulus fibrosus were fairly sensitive and highly specific predictors of the clinical diagnosis of instability (5). Because disk stiffness cannot be measured in these clinical studies, instability is inferred from clinical findings and flexion/extension radiographs.
The purpose of this study was to correlate the morphologic characteristics of the intervertebral disk revealed by MR imaging with the stiffness of the intervertebral disk measured biomechanically. Diminished stiffness in a motion segment defines instability in biomechanical studies. As stiffness in the disk diminishes, a unit of force or torque produces more motion in the segment and more stress in the adjoining connective tissues. Cadaver lumbar motion segments, that is, an intervertebral disk with the two attached vertebrae, were used in this study so that both stiffness and morphologic disk characteristics could be assessed accurately. Specifically, the purpose was to determine if diminished stiffness of the intervertebral disk can be predicted by evidence of concentric, transverse, or radial tears that MR imaging reveals in the annulus fibrosus (6) or by diminished intervertebral disk height.
Methods
Cadavers ranging from 49 to 87 years (average age, 74 years) at time of death were acquired through the Body Donation Program. Bodies with metastatic disease, spinal trauma, or spinal surgery were excluded. Within 48 hours of death, the lumbar motion segments were harvested (7), sealed in plastic bags, and stored at −20° C until the biomechanical tests were performed. Eighty-two motion segments were harvested consisting of a T12-L1, L1-L2, L2-L3, L4-L5, or L5-S1 disk and the two adjacent vertebrae. Between 10 and 16 segments were harvested for each level.
The motion segments were thawed at room temperature for 16 hours prior to imaging. The specimens were imaged in a 5-inch diameter transmit-and-receive solenoid coil in a 1.5-T imager. Sagittal and axial T1-weighted images were acquired (650/40/2 [TR/TE/excitations]) using a 1-mm slice thickness, an 8 × 8-cm field of view, and a 512 × 256 matrix. Sagittal and axial T2-weighted images were acquired (2000/90/2) with a 1-mm slice thickness, 8 × 8-cm field of view, and 512 × 256 matrix. One investigator experienced in spine MR imaging evaluated the MR-revealed appearance of each intervertebral disk. Each disk was classified as normal in height, mildly reduced in height (less than 50% reduction), or severely reduced in height (more than 50%). Each disk also was classified on the basis of T2-weighted images as normal or reduced in signal intensity. Regions of high signal intensity in the annulus fibrosus were classified as concentric, transverse, or radial tears on the basis of conventional criteria (6). Each disk ultimately was classified as: 1) normal; 2) having transverse or concentric tears if MR imaging showed only these abnormalities; 3) having radial tears if MR imaging showed high intensity in the annulus fibrosus or decreased signal intensity in the disk and bulging of the annulus fibrosus characteristic of a radial tear; or 4) advanced degeneration if the disk had lost more than 50% height or the vertebrae had developed large osteophytes. After imaging, the specimen was refrozen.
For biomechanical testing, the specimen was thawed. The inferior vertebra was fastened to a platform (Fig 1). Rods were attached to the superior vertebra in the midline plane perpendicular to the spinal axis. Torque was applied to the ends of the rod in the opposite direction with deadweights, cords, and pulleys to produce pure moments of axial rotation (8). A moment arm of 600 mm and dead weights of 1100 g were used to produce a moment of 6.6 Newton-meters (Nm) first in the left axial rotation and then in the right axial rotation. As the torques were applied to each motion segment, the movements of three reflective markers attached to the upper vertebra were recorded at 60 Hz by VICON cameras. Translation and rotation (6° of freedom) of the superior vertebra, with respect to the inferior vertebral body, were calculated from changes in the marker position (8). The stiffness of the motion segments (Nm/degrees) was calculated as the ratio of applied torque to the motion. The stiffness for each group was plotted. The stiffness for the entire group was divided into quartiles, and the number of each disk type in each quartile was calculated. Differences between groups were tested with the analysis of variance without replication.
fig 1.
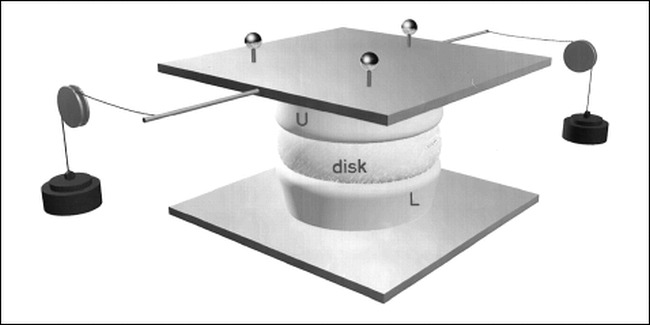
Artist's sketch of the biomechanical testing device to measure disk stiffness. The lower (L) and upper (U) vertebrae are attached to plates. The lower plate is fixed. By means of weights and pulleys, a torque is applied to the upper plate. The motion produced by the torque is calculated from the displacements of the reflective targets attached to the plate (see Methods).
Results
Eighty-two motion segments were studied. The average stiffness was 2.9 Nm/degree and the range was 0.7 to 16.0 Nm/degree. In general, the greatest stiffness was found in the motion segments with normal disks and the least in motion segments with radial tears in the annulus fibrosus. The intervertebral disks in 13 motion segments were classified as having normal structure (Fig 2A); in 42, as having transverse or concentric small tears in the annulus fibrosus (Fig 2B); in 16, as having radial tears in the annulus fibrosus (Fig 2C); and in 11, as having advanced degeneration (Fig 2D). Stiffness averaged 7.0 Nm/degree for the normal group; 1.9 Nm/degree, for the disks with transverse and concentric tears; 1.7 Nm/degree, for disks with radial tears; and 3.1 Nm/degree, for disks with advanced degeneration.
fig 2.
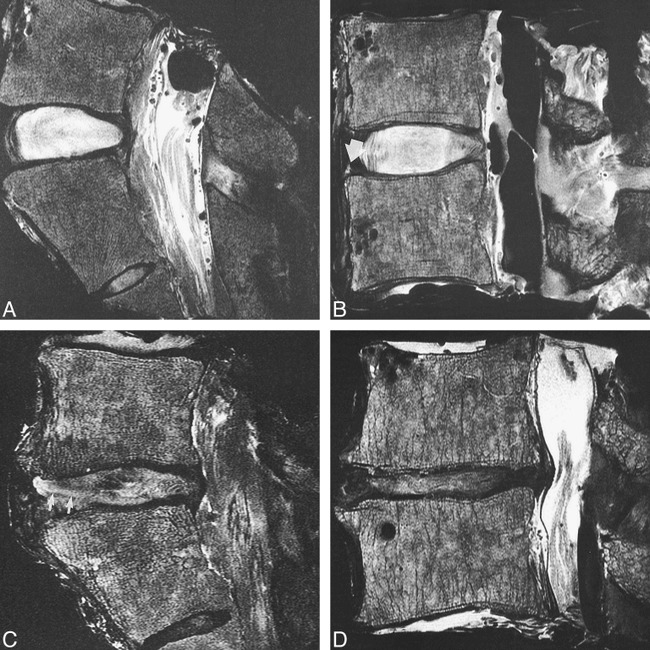
Sagittal MR images (2000/90[TR/TE]) of intervertebral disks classified as normal (A), transverse tear (B), radial tear (C), and advanced degeneration (D)
Stiffness by disk type is illustrated in Figure 3. We found that stiffness of normal disks exceeded that in other groups. The stiffness of disks with transverse, concentric, or radial tears of the annulus fibrosus was diminished. Disks with radial tears of the annulus fibrosus had the lowest stiffness. Disks with collapsed disk space and large osteophytes had increased stiffness when compared with radial tears.
fig 3.
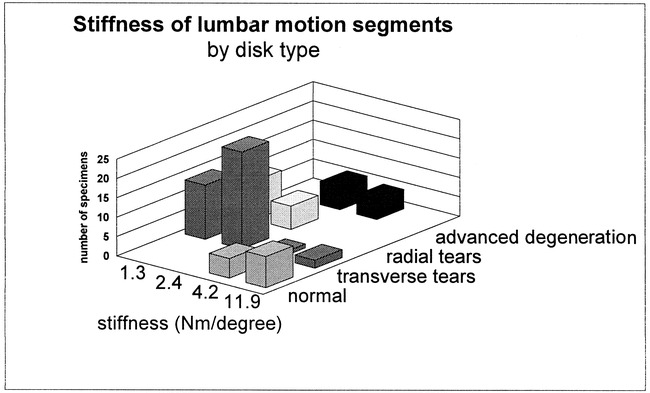
Graph illustrating the relationship between stiffness and disk classification
The number of disks of each type in each quartile is illustrated graphically in Figure 4. The quartiles had average stiffnesses of 1.3, 2.4, 4.2 and 11.9 Nm/degree, and contained 23, 36, 11, and 10 specimens, respectively. Disks with normal structure were found only in the two stiffest groups. Disks with radial tears were found in only the least stiff groups. Disks with concentric and transverse tears were found mostly in the two intermediate quartiles. The disks with advanced degeneration were not found in the most or the least stiff quartiles but in the two groups with intermediate stiffness. The relationship of stiffness and disk type was significant (P = .014).
fig 4.
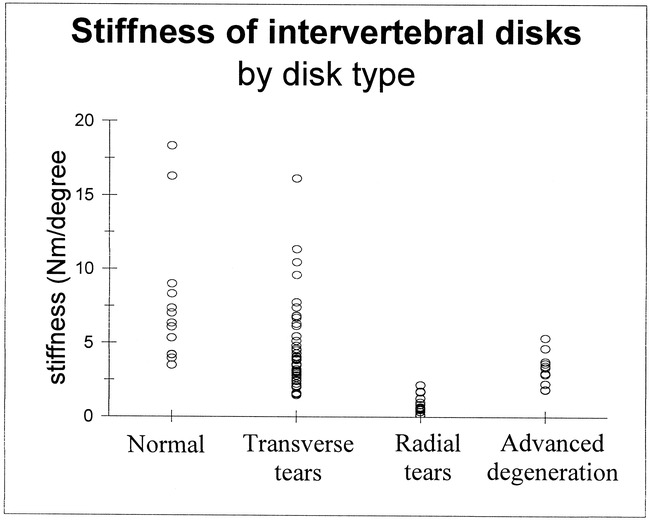
Graph illustrating the distribution of the individual stiffness measurements for the normal, transverse tear, radial tear, and advanced degeneration groups.
Discussion
The study shows that MR findings of transverse, concentric, or radial tears in the annulus fibrosus enabled us to predict decreased stiffness in the intervertebral disk. In the presence of a radial tear, the stiffness was more severely reduced than with a transverse or concentric tear or advanced disk degeneration. In specimens with disk collapse and large osteophytes, stiffness was increased when compared with radial tears.
MR imaging revealed tears of the annulus fibrosus and changes in intervertebral disk height. Transverse tears of the annulus fibrosus, also called rim lesions in the orthopedic literature, are common in disks of individuals over 40-years-old (9–12). On MR images, they appear as small foci of high signal intensity that are located within the low signal region of the annulus fibrosus near the vertebral endplates. Concentric tears of the annulus fibrosus, which occur as commonly as transverse tears, are identified less effectively on MR images. Concentric tears represent delamination between lamellae of the annulus fibrosus. MR imaging shows radial tears of the annulus fibrosus (or “high-intensity zones”) as a thin zone of high signal intensity that traverses the annulus fibrosus (13, 14). The radial tear usually is located midway between the endplates rather than near the endplates. The sensitivity of MR imaging for the detection of a radial tear as a region of high signal intensity is about 75% (15). Diminished signal intensity and bulging of the annulus fibrosus are also signs of a radial tear, even if the high-intensity zone is not identified (10). Radial tears can be identified on contrast-enhanced MR images as a linear or curvilinear zone of enhancement (13).
This study of motions at lumbar disk levels in cadaver material was limited. We restricted the study to an axial rotational torque because normal and degenerating disks differ more in stiffness to axial rotation than to flexion, extension, or lateral bending torques (8). The obliquely oriented fibers in the annulus fibrosus probably explain the high degree of stiffness we found with normal intervertebral disks that had an intact annular fibrosus (16). We did not attempt to correlate the amount of rotation that occurred with these specimens to the amount of translation secondary to a flexion or extension force. Any history of back pain prior to death generally was not available for analysis. The loads applied were intentionally small to prevent failure of the vertebral body or intervertebral disk. Therefore, the loads were well within physiologic limits. Other factors that may have contributed to segmental spinal instability, such as facet joint arthritis and muscle conditions, were not investigated specifically in this study. Intraabdominal pressure and muscle tone, which affect spinal stability in vivo, were not factors in this study. For the load levels used in this study, the disk was the major factor in stiffness (17). Because of the limited number of specimens, the effect of facet joint changes at different levels of the spine could not be compared statistically.
The relationship between back pain and reduced stiffness in the intervertebral disk has not been clarified, despite extensive study. Instability secondary to disk degeneration, according to some investigators, accounts for as much as one-third of all cases of back pain (18). As stiffness in the intervertebral disk is reduced, the forces normally affecting the spine produce greater motion. These motions may result in greater stress in adjacent innervated connective tissue, which may hypothetically cause pain (19, 20). In addition, reduced stiffness increases the risk that the neural foramen will be critically narrowed as forces are applied to the spine (7).
The effect of disk degeneration on stiffness of the spine and the motions of the spine in response to physiologic forces needs more study. Conventional radiographic and imaging studies do not provide an effective means to detect instability. Criteria for detection of instability from flexion/extension radiographs are arbitrary and imprecise. In patients with a clinical diagnosis of spinal instability, inconsistent results are obtained with flexion/extension radiographic methods, despite efforts to optimize methods (3, 21). One group has reported that from flexion/extension radiographs, little reliable information can be obtained (22). Spinal segmental instability needs additional radiographic and imaging studies. Better methods are needed to measure the motions of the lumbar spine, and to distinguish unstable segments. A radial tear of the annulus fibrosus revealed by MR imaging indicates a reduction in the stiffness of the intervertebral disk and increased motion of that lumbar segment in response to an axial rotational torque. The reduced stiffness may be one mechanism by which a radial tear produces pain. Further work is needed to determine when reduced stiffness may produce clinical symptoms.
Conclusion
A transverse tear in the annulus fibrosus on an MR image enables one to predict reduced stiffness in the intervertebral disk. A radial tear in the annulus fibrosus or decreased signal intensity in the disk indicates a severe reduction in stiffness. Further study is needed to determine the relationship of stiffness and clinical symptoms.
Acknowledgments
This work was supported by National Institutes of Health (NIH) Grant No. RO1 AR33667.
Footnotes
Address reprint requests to Victor Haughton, M.D., Department of Radiology, University of Wisconsin, 600 Highland Avenue, Madison, WI 53792-3252.
References
- 1.Sonntag VK, Marciano FF. Is fusion indicated for lumbar spinal disorders? Spine 1995;20:138S-142S [PubMed] [Google Scholar]
- 2.Pope MH, Frymoyer JW, Krag MH. Diagnosing instability. Clin Orthop 1982;279:60-67 [PubMed] [Google Scholar]
- 3.Quinnell R, Stockdale HR. Flexion and extension radiography of the lumbar spine: comparison with lumbar discography. Clin Radiol 1983;34:405-411 [DOI] [PubMed] [Google Scholar]
- 4.Toyone T, Takahashi K, Kitahara H, Yamagata M, Murakami M, Moriya H. Vertebral bone marrow changes in degenerative lumbar disc disease. J Bone and Joint Surg 1995;765:757-764 [PubMed] [Google Scholar]
- 5.Bram J, Zanetti M, Min K, Hodler J. MR abnormalities of the intervertebral disks and adjacent bone marrow as predictors of segmental instability of the lumbar spine. Acta Radiologica 1998;39:18-23 [DOI] [PubMed] [Google Scholar]
- 6.Yu S, Sether L, Wagner M, Haughton VM. Tears of the anulus fibrosus: correlation between MR and pathologic findings in cadavers. AJR Am J Roentgenol 1988;9:367-370 [PMC free article] [PubMed] [Google Scholar]
- 7.Nowicki BH, Haughton VM, Schmidt T, et al. Occult lumbar lateral spinal stenosis in neural foramina subjected to physiologic loading. AJNR Am J Neuroradiology 1996;17:1605-1614 [PMC free article] [PubMed] [Google Scholar]
- 8.Schmidt TA, An HS, Lim T-H, Nowicki BH, Haughton VM. The stiffness of lumbar spinal motion segments with a ‘high intensity zone’ in the annulus fibrosus. Spine 1998;23:2167-2173 [DOI] [PubMed] [Google Scholar]
- 9.Yu S, Haughton VM, Ho PSP, Sether LA, Wagner M, Ho KC. Progressive and regressive changes in the nucleus pulposus. Part II: the adult. Radiology 1988;169:93-97 [DOI] [PubMed] [Google Scholar]
- 10.Yu S, Haughton VM, Sether LA, Wagner M. Anulus fibrosus in bulging intervertebral discs. Radiology 1988;169:761-763 [DOI] [PubMed] [Google Scholar]
- 11.Wagner M, Sether LA, Yu S, Ho PSP, Haughton VM. Age changes in the lumbar intervertebral disc studied with magnetic resonance and cryomicrotomy. Clin Anat 1988;1:93-103 [Google Scholar]
- 12.Yu S, Haughton VM, Sether L, Ho K, Wagner M. Criteria for classifying normal and degenerated lumbar intervertebral discs. Radiology 1989;170:523-526 [DOI] [PubMed] [Google Scholar]
- 13.Ross JS, Modic MT, Masaryk TJ. Tears of the anulus fibrosus: assessment with Gd-DTPA-enhanced MR imaging. AJNR Am J Neuroradiology 1989;10:1251-1254 [PMC free article] [PubMed] [Google Scholar]
- 14.Aprill C, Bogduk N. High intensity zone: a diagnostic sign of painful lumbar disc on magnetic resonance imaging. Br J Radiol 1992;65:361-369 [DOI] [PubMed] [Google Scholar]
- 15.Yu F, Haughton VM, Sether L. Comparison of MR and discography in detecting radial tears of the anulus: a postmortem study. Radiology 1989;10:1077-1081 [PMC free article] [PubMed] [Google Scholar]
- 16.Broberg KB. On the mechanical behavior of intervertebral discs. Spine 1983;8:151-165 [DOI] [PubMed] [Google Scholar]
- 17.McGill SM, Norman RW. Effects of an anatomically detailed erector spine model on L4/L5 disc compression and shear. J Biomechanics 1987;20:591-600 [DOI] [PubMed] [Google Scholar]
- 18.Friberg S, Hirsch C. Anatomical and clinical studies on lumbar disc degeneration. Acta Orthop Scand 1949;19:222-242 [DOI] [PubMed] [Google Scholar]
- 19.Knutsson F. The instability associated with disc degeneration in the lumbar spine. Acta Radiol 1944;25:593-598 [Google Scholar]
- 20.Kirkaldy-Willis WH, Farfan HF. Instability of the lumbar spine. Clin Orthop Rel Res 1982;165:110-121 [PubMed] [Google Scholar]
- 21.Morgan FP, King T. Primary instability of lumbar vertebrae as a common cause of low back pain. J Bone Joint Surg 1957;39B:6-22 [DOI] [PubMed] [Google Scholar]
- 22.Stokes IAF, Frymoyer JW. Segmental motion and instability. Spine 1987;12:688-691 [DOI] [PubMed] [Google Scholar]


