Abstract
Background The OpenNotes initiative launched an international movement aimed at making health care more transparent by improving communication with, and access to, information for patients through provider note sharing. Little has been written either on provider note sharing in pediatric and adolescent populations or on the impact of system default settings versus voluntary provider note sharing.
Objective We describe our journey as a pediatric integrated delivery network to default share notes in ambulatory specialty practices not only with parent proxies but also with teens and discuss the methods that led to a successful implementation.
Methods Retrospective analysis of every ambulatory shareable medical provider note written in pediatric subspecialty clinics within an integrated pediatric delivery network from April 2017 through March 2019.
Results From April 2017 to February 2018, a total of 221,655 notes were shareable based on organizational policies, yet only 224 (0.1%) were actually shared with patients and families. After implementing a system of default release of notes from March 2018 to January 2019, a total of 224,960 notes were shareable, of which 191,379 (85%) were shared.
Conclusion Requiring providers to take an action to share notes (opt-in) results in few notes being shared while requiring providers to take an action to not share notes (opt-out) results in high levels of note sharing. We demonstrate that default release of notes in pediatric organizations to both proxies and teens is not only achievable but also likely to lead to increased provider note sharing with patients without obvious negative impact on providers or the organization.
Keywords: information sharing, open access to information, electronic health records and systems, communication, patient-provider, encounter notes, patient portal
Background and Significance
OpenNotes is an international movement dedicated to making health care more transparent by encouraging health care professionals to share clinical notes with patients ( www.opennotes.org ). In 2010, The Robert Wood Johnson foundation led an initiative for the first OpenNotes implementation and shared primary care provider (PCP) notes with over 20,000 adult patients. While providers expressed concerns that provider note sharing would impact workload and relationships with patients, 1 their findings demonstrated that provider note sharing did not have a significant impact on physician workload as measured by whether there were observed increases in messages or emails received from patients. 2 This and work from others have shown that patients and family members obtain significant satisfaction and improvement in care when they are able to review their medical notes. 2 3
Sharing of medical notes includes the processes of note sharing, that is, the sharing of notes by providers to patients, and note reading by patients as well as outcomes and consequences related to these respective processes. If notes are not shared, patients cannot read them, and if patients do not read notes, the notes cannot provide benefits to the patient. For the purposes of this discussion, we focus on the process of provider note sharing. The original OpenNotes study recruited primary care adult physicians to voluntarily participate in provider note sharing. 2 Application of provider note sharing at the organizational level provides an opportunity to offer other options outside of volunteer note sharing (opt-in) including whether to share notes by default, to allow providers to opt-out entirely, or to allow providers to select which notes to share. Provider note sharing rates based on these different approaches have not been detailed in the literature. Additionally, differences in provider note sharing rates among non-PCPs and between specialties have not been studied.
Much of the research on provider note sharing to date has centered on adult patient populations. 4 While OpenNotes lists over 130 pediatric health systems actively sharing notes with their patients, 5 there is a paucity of data on experiences by those systems. The unique challenges faced by pediatric organizations sharing notes based on legal mandates and confidentiality concerns require careful consideration of privacy settings, a challenge for many electronic health record (EHR) vendors. 6
We report a unique perspective from pediatric subspecialty settings in contrast to adult primary care populations. We will focus on the process of provider note sharing and its consequences, and to that end, describe our journey as a pediatric integrated delivery network inclusive of both medical and surgical subspecialties that now shares notes by default with caregiver proxies and teens.
Journey
Fig. 1 displays our timeline of events in provider note sharing as defined by making a note available to be shared in the patient portal irrespective of whether the patient has signed up for portal access. Opt-in refers to manual note sharing (provider chooses to share the note) and opt-out refers to system default provider note sharing where the provider must choose to not share the note. The journey began in August 2015 with presentations regarding OpenNotes at medical staff meetings based on a pilot project in the Developmental Services Department. Buy-in from physicians was initially tenuous. Cited concerns regarding consequences of provider note sharing included: increased volume of patient messages, families unable to understand medical documentation, need for providers to document differently, increased requests to amend provider visit notes, damage to the provider–patient relationship, and inadvertent sharing of sensitive information. Faced with these concerns, we began with opt-in provider sharing (manual release) of provider visit notes across most clinical arenas over the subsequent 2 to 3 years. However, provider note sharing rates were universally poor (see Fig. 2 and the “Results” section).
Fig. 1.

Timeline of events in note sharing.
Fig. 2.
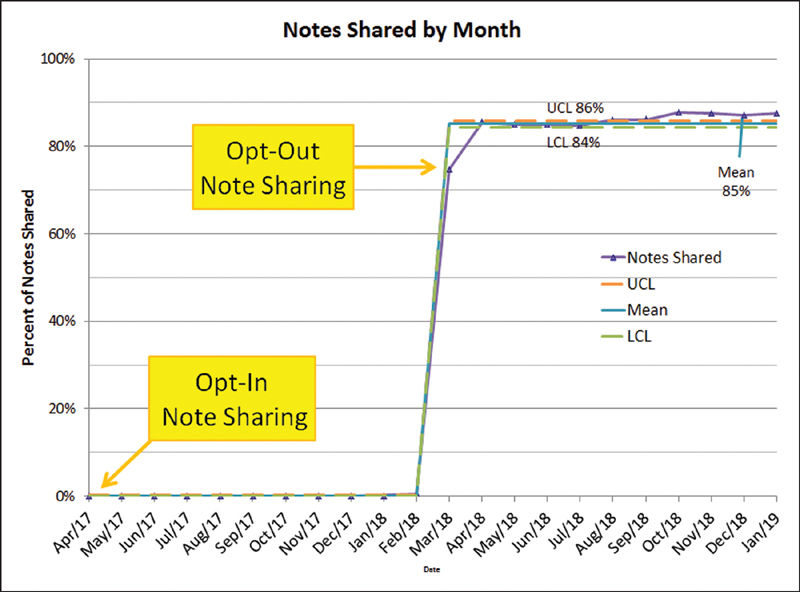
Control chart of shared notes plotted against opt-in and opt-out note sharing.
Faced with almost nonexistent provider note sharing, in February 2017, the Rady Children's Health Network (RCHN) Family Advisory Council wrote a letter to the Chief Medical Information Officer requesting universal note sharing, citing four advantages: better understanding of treatment plans and goals, increased family involvement, patient safety, and added value to the patient portal. Furthermore, they stated, “to those who might believe that the notes will cause unnecessary worry, we would argue to the contrary. Information is a wonderful antidote to fear.” This letter prompted us to issue a call for opt-out provider note sharing in November 2017 receiving rapid approval from physician leaders. We began universal opt-out provider note sharing of subspecialty provider visit notes in March 2018, inpatient discharge summaries in June 2018, and emergency department and urgent care provider notes in August 2018.
Our journey has led to our current system settings to default share clinical notes unless marked as sensitive by the authoring provider. Child abuse and psychotherapy notes are default set to not be shared per our system settings. For patients less than 12 years old and/or with diminished capacity, default release of shared notes occurs to the proxy (generally parent/guardian). For patients aged 12 years and older, notes are only released to the patient, ensuring the protection of reproductive health information. Teen access requires parental consent.
Methods
We present results from our evaluation of every shareable note from April 2017 through March 2019. This timeframe was chosen to provide an equal duration for comparison between the preintervention or opt-in period (April 2017–February 2018) and the postintervention or opt-out period (March 2018–January 2019). Given the different timelines in note release settings across various arenas, we focused our analysis on ambulatory subspecialty provider notes excluding emergency department, urgent care, and discharge summary notes.
An individual note written by a provider is defined as shareable if it is available for viewing in the patient portal. The decision to mark a note as sensitive or to block from sharing occurs at the note level by the provider, a process that formally changes the note's sharing status. During the opt-in period, the provider was required to manually select “share note with patient.” During the opt-out period, notes were automatically shared with the patient or proxy unless the provider manually unselected “share note with patient.” Notes are not shareable if they are (1) written in a child abuse or mental health clinic, (2) marked as sensitive by the provider, or (3) blocked from sharing by the provider. Notes originating from a child abuse or mental health clinic or those marked as sensitive are never shared. For a patient 12 years and older, the notes shared are only viewable by the patient him/herself/themselves unless he/she/they have diminished capacity. For a patient younger than 12 years or a patient with diminished capacity, the notes are shared with the medical proxy.
We developed a Structured Query Language-based report to determine the sharing status of each note written, that is, whether or not it was available for viewing in the patient portal. This enabled us to evaluate which providers and specialties were sharing notes and how note sharing changed over time. For patients whose note was written at a time when they did not have an active portal account, the note sharing status reflects whether the note would be available in the future should the portal account become activated.
We limited our analysis to notes written about youth 0 to 17 years and authored by a provider (fellows, physicians, or advance practice providers). Notes authored by residents require cosignature by the attending physician per policy and thus were counted as a note written by the attending physician. Subspecialty clinical area share rates are presented before and following opt-out note sharing. We also examined share rates according to subspecialty with share rate percentages determined by dividing number of shared notes by number of total notes by providers of a given subspecialty.
To evaluate whether medical note sharing resulted in an increased work burden to providers, and as a balancing measure, we measured overall patient message volume during both the opt-in and opt-out periods for comparison. We also reviewed patient health information management (HIM) requests for amendments to medical notes.
RCHN utilizes Epic Systems Corporation's EHR, which includes the Epic MyChart patient portal. Note release settings (i.e., share with patients and note sensitivity) are based on standard built-in functionality. We did perform a custom build to flag patients with diminished capacity and to ensure that notes, when shared, would be released to the medical proxy rather than the patient once he/she/they reached an age of 12 years.
Results
Opt-In Provider Note Sharing Period
From April 2017 to February 2018, during the opt-in provider note sharing period, a total of 221,655 notes were shareable based on organizational policies. Providers marked 77 of these notes as sensitive, leaving 221,578 not sensitive and thus available to be shared. Of these nonsensitive shareable notes, only 224 (0.1%) were actually shared meaning that the provider opted-in to share the note with the patient or proxy. A total of 34 notes shared were read by patients or their proxies (13.8%). During this time, providers received a total of 33,415 patient messages via the patient portal, which equates to about one message for every 6.6 notes written. The HIM department received four formal chart amendment requests during this time.
Opt-Out Provider Note Sharing Period
From March 2018 to January 2019, during the opt-out provider note sharing period, providers wrote a total of 224,960 shareable notes. Providers marked 343 of these notes as sensitive, leaving 224,617 not sensitive and thus available to be shared ( Fig. 2 ). Of the nonsensitive shareable notes, 191,379 (85%) were actually shared with patients or proxies meaning that the provider did not override the system default to share. Equivalent portions of notes written on patients with (86%) and without (87%) an active portal account were shared. While this difference was statistically significant ( p < 0.001), it does not appear to be meaningful. Overall note sensitivity rates increased during the opt-out period (0.15% vs. 0.03%, p < 0.001), which may reflect provider hesitancy in sharing some note content with patients. Note sensitivity status, however, did not differ based on patient portal activation status (0.15% vs. 0.16%, active vs. not active, p = 0.45). A total of 3,159 (1.7%) of the notes shared and accessible via the patient portal were read by either patients or their proxies. During this time period, a total of 38,076 patient messages were received by providers via the patient portal, which equates to about one message for every 5.9 notes written. The HIM department received five formal chart amendment requests during this time.
There is notable variation in note sharing across subspecialties at our institution. Among 34 subspecialty clinical areas (26 medical and 8 surgical), provider share rates ranged from a low of 9 to 100%. Of the 34 subspecialty clinical areas, one demonstrated poor provider share rates (0–25%); none demonstrated fair provider share rates (26–50%), 7 demonstrated good provider share rates (51–75%), and 26 demonstrated excellent provider share rates (76–100%). Provider share rates did not particularly differ according to provider classification by medical versus surgical subspecialty ( p > 0.05). Anecdotally, providing divisional and individual level note sharing data to low share rate specialties after the study period has resulted, in most cases, in a substantial increase in note sharing.
Discussion
Our journey to improve provider note sharing in a pediatric subspecialty setting has provided several insights. Default release of notes with an opt-out option was the most effective system setting to achieve widespread provider note sharing with patients or proxies. Even though stakeholders and providers endorsed provider note sharing, requiring providers to actively opt-in by adding an extra click to their workflow proved to be a significant barrier. Behavioral economics may provide additional insight into our success with opt-out provider note sharing. It likely reflects the status quo bias where people frequently exhibit inertia tending not to deviate from the default option, as has been shown in other case scenarios (organ donation, 7 retirement savings, 8 and flu vaccination 9 ).
The Agency for Healthcare Research and Quality 10 recommends early and extensive patient and provider engagement when implementing open access to clinical notes, and we began this journey by getting buy-in from both patient and provider stakeholders. Given provider concerns, we began by allowing providers to opt-in to share notes. We discovered quickly that this was not effective and thus pivoted to default release of notes with immediate demonstration of marked improvement in provider note sharing rates ( Fig. 2 ). Provider concerns that note sharing would lead to increased workload and/or increased requests for editing of medical documentation did not materialize.
Institutional share rates may mask variability in share rates by specialties and providers, making it difficult to address specific provider concerns about note sharing. Having granular data by specialty and provider allowed us to evaluate differences in provider note sharing. While we have yet to extensively evaluate the reasons underlying these differences, we recognize that anecdotal experiences can significantly influence note sharing. However, simply feeding back data on share rates to individual specialties has positively influenced provider share rates. Allowing providers within a specialty to see how their share rate compares to that of peers within and relative to other specialties has prompted dialogue to address concerns and build confidence that note sharing will not be unduly burdensome. Further, sharing provider note share rates may have leveraged the behavioral economic principles of social forces and comparisons to further promote provider note sharing. 11 Success often breeds success. Our positive provider note sharing experience in ambulatory subspecialty clinics subsequently translated to noneventful default provider note sharing of emergency, urgent care, and discharge summary notes.
To facilitate adoption of this functionality, we shared information from the literature on the benefits to the patient and limited risks to the provider. We leveraged experience from our developmental services experience as well as from providers who were early adopters in embracing the technology. We also engaged patients through our Family Advisory Council bringing the message from the patients directly to the providers. This proved the most effective as it shifted the conversation away from how note sharing would impact providers to how it would benefit patients.
One area of concern raised is the appropriateness of providers' sharing notes with adolescents. Currently, we default release notes to patients 12 years and older and have had no issues although the number of youth with their own portal account is low. Commonly cited reasons for providers to not share medical notes with adolescents include potential harm via loss of confidentiality and inability to comprehend medical notes. Prior work at our institution disputes this. Since our default release of medical notes, a cohort of adolescents and young adults with chronic gastrointestinal disease demonstrated notable satisfaction with their provider visit documentation, adequate health literacy, and comprehension of their medical notes without any reported adverse events. 12
There are limitations to our findings. First, data presented only reflect the experience at a single institution. However, there are limited data in the literature regarding note sharing particularly in the pediatric setting and we hope that broad sharing of our experience will help other pediatric institutions to improve provider note sharing. Second, we demonstrate very low note reading rates by patients. The current work focused on the necessary preamble to note reading, that is, note sharing. Moving forward, we are now focusing on how to improve note reading rates so that the benefits of note sharing can be fully realized by our patients and families.
Future areas of improvement include continued improvement in provider note sharing practices and the evaluation of the subsequent process of note sharing, note reading, including studying how note reading impacts patient or proxy understanding of medical conditions and improves health outcomes. We also plan to allow the patient or proxy to contribute directly to the note, which we believe will not only promote patient safety through more accurate documentation but also improve provider efficiency. Behavioral health note sharing also has the potential to improve outcomes and increase patient engagement. 13 While we have yet to provide routine access to behavioral health notes at our institution, we are currently collecting pilot data toward such sharing to inform efforts to promote sharing of these notes. Through the work presented, we submit that we have made strides in, and added to the conversation regarding note sharing, governance, and deployment in the pediatric setting.
Conclusion
We found that system-wide default settings to share significantly improved provider note sharing rates. Marked differences in provider note sharing, however, do exist between specialties and by providers within specialties. Requiring providers to actively share notes did not produce meaningful provider note sharing rates. Following institution of opt-out default note sharing, provider-cited concerns regarding increased patient message volumes have not materialized. Of note, while default provider note sharing led to a significant increase in provider notation of notes as sensitive, rates of notes marked sensitive remained quite low. The adequacy and/or appropriateness of such denotation require further evaluation.
Clinical Relevance Statement
Patients and families have increasing expectations of improved communication and medical decision sharing with their medical providers. As organizations move toward a more open and transparent method of sharing medical information and decision making by making notes available to patients, it is important to recognize the methods that can lead to a successful implementation of note sharing.
Multiple Choice Questions
-
When implementing provider note sharing at your organization which method would you choose based on our experience and findings?
Opt-in (manual) release of provider notes requiring the provider the mark the note for sharing the EHR.
Automatic/default release of provider notes with the ability to opt-out for individual notes.
Natural language processing-driven algorithm to select notes appropriate for sharing.
Using a machine learning algorithm that evaluates the diagnoses and problem list for the patient to decide whether to share the note.
Correct Answer: The correct answer is option b, our experience and our data demonstrate that providers are unlikely to change the default option in the EHR. The greatest success in note sharing was when our organization pivoted to default release of notes leading to a share rate of 85%. Allowing providers to manually select which notes to release did not lead to any substantial sharing of notes with patients.
-
When evaluating note sharing at your organization what level of detail provides more clarity of note sharing practices?
Overall organization note share rate.
Note share rate by geographic area of the clinics.
Individual provider note share rate.
Department or medical specialty note share rate.
Correct Answer: The correct answer is option c, although a great deal of information can be gleaned at the overall organization level, delving deeper into the data can provide more information about and help identify provider groups with low share rates. We also found that, although looking at individual departments may provide important group information, if one does not look at the individual providers, low provider share rates can be obscured by the higher share rates of their colleagues. Therefore, we recommend looking at note sharing rates at the provider level.
Conflict of Interest None declared.
Protection of Human and Animal Subjects
Our project was performed in compliance with the World Medical Association Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Subjects, and was reviewed by the University of California, San Diego Institutional Review Board and given a waiver as a quality improvement project.
References
- 1.Walker J, Darer J D, Elmore J G, Delbanco T. The road toward fully transparent medical records. N Engl J Med. 2014;370(01):6–8. doi: 10.1056/NEJMp1310132. [DOI] [PubMed] [Google Scholar]
- 2.Delbanco T, Walker J, Bell S K et al. Inviting patients to read their doctors' notes: a quasi-experimental study and a look ahead. Ann Intern Med. 2012;157(07):461–470. doi: 10.7326/0003-4819-157-7-201210020-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weinert C. Giving doctors' daily progress notes to hospitalized patients and families to improve patient experience. Am J Med Qual. 2017;32(01):58–65. doi: 10.1177/1062860615610424. [DOI] [PubMed] [Google Scholar]
- 4.Sarabu C, Pageler N, Bourgeois F. OpenNotes: toward a participatory pediatric health system. Pediatrics. 2018;142(04):e20180601. doi: 10.1542/peds.2018-0601. [DOI] [PubMed] [Google Scholar]
- 5.OpenNotes.org. Pediatrics & Adolescents. Available at:https://www.opennotes.org/tools-resources/for-health-care-providers/pediatrics-adolescents-clinicians. Accessed 2019
- 6.Bourgeois F C, DesRoches C M, Bell S K. Ethical challenges raised by OpenNotes for pediatric and adolescent patients. Pediatrics. 2018;141(06):e20172745. doi: 10.1542/peds.2017-2745. [DOI] [PubMed] [Google Scholar]
- 7.Johnson E J, Goldstein D G. Defaults and donation decisions. Transplantation. 2004;78(12):1713–1716. doi: 10.1097/01.tp.0000149788.10382.b2. [DOI] [PubMed] [Google Scholar]
- 8.Madrian B C, Shea D F. The power of suggestion: inertia in 401(k) participation and savings behavior. Q J Econ. 2001;116(04):1149–1187. [Google Scholar]
- 9.Chapman G B, Li M, Colby H, Yoon H. Opting in vs opting out of influenza vaccination. JAMA. 2010;304(01):43–44. doi: 10.1001/jama.2010.892. [DOI] [PubMed] [Google Scholar]
- 10.Agency for Healthcare Research and Quality.Patient Access to Medical Notes in Primary Care: Improving Engagement and Safety Rockville, MD: Department of Health and Human Services, Agency for Healthcare Research and Quality; 2016 [Google Scholar]
- 11.Jenssen B P, Buttenheim A M, Fiks A G. Using behavioral economics to encourage parent behavior change: opportunities to improve clinical effectiveness. Acad Pediatr. 2019;19(01):4–10. doi: 10.1016/j.acap.2018.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang J S, Yueh R, Ma S, Cruz R, Bauman L, Choi L J. Adolescents' and young adults' satisfaction with and understanding of medical notes from a pediatric gastroenterology practice: a cross-sectional cohort study. J Pediatr. 2019;215:264–266. doi: 10.1016/j.jpeds.2019.06.052. [DOI] [PubMed] [Google Scholar]
- 13.Galvin H K, Petersen C, Subbian V, Solomonides A. Patients as agents in behavioral health research and service provision: recommendations to support the learning health system. Appl Clin Inform. 2019;10(05):841–848. doi: 10.1055/s-0039-1700536. [DOI] [PMC free article] [PubMed] [Google Scholar]


