Abstract
Background.
The end-of-life trajectory for persons with dementia is often protracted and difficult to predict, placing these individuals at heightened risk of live discharge from hospice. Risks for live discharge due to condition stabilization or failure to decline among patients with dementia are not well established.
Objective.
Identify demographic, health, and hospice service factors associated with live discharge due to condition stabilization or failure to decline among hospice patients with dementia.
Design.
Retrospective cohort study.
Participants.
2,629 hospice patients with dementia age 65 years and older served from 2013–2017 at a large not-for-profit agency in New York City.
Measures.
Primary outcome was live discharge from hospice due to condition stabilization, or failure to decline (versus death). Measures include demographic factors (race/ethnicity, Medicaid, gender, age, marital status, parental status), health characteristics (primary dementia diagnosis, comorbidities, functional status, prior hospitalization), and hospice service (location, length of service, number and timing of nurse visits).
Results.
Logistic regression models indicated that compared to white hospice patients with dementia, African American and Hispanic hospice patients with dementia experienced increased risk of live discharge (African American: AOR: 2.42, 95% CI: 1.34–4.38; Hispanic: AOR: 2.99, 95% CI: 1.81–4.94). Home hospice (AOR: 7.57, 95% CI: 4.04–14.18), longer length of service (AOR: 1.04, 95% CI: 1.04–1.05), and more days between nurse visits and discharge (AOR: 1.86, 95% CI: 1.56–2.21) were also associated with live discharge.
Conclusion.
To avoid burdensome and disruptive transitions out of hospice in patients with dementia, interventions to reduce live discharge due to condition stabilization or failure to decline should be tailored to meet the needs of African American, Hispanic, and home hospice patients. Policies regarding sustained hospice eligibility should account for the variable and protracted end-of-life trajectory of patients with dementia.
Keywords: hospice, live discharge, dementia, health disparities
Introduction
Roughly 20% of hospice patients experience live discharge from hospice before death.1–5 Live discharge is frequently a burdensome and disruptive transition for patients and their family members, who may lose services and support they have come to depend upon, including nursing, social work, home health aide and spiritual care.6–8 Live discharge occurs for several reasons, including patient/family preferences and distressing symptoms which lead to calling emergency services. Perhaps of greatest concern to persons with dementia (PWD) is live discharge because of condition stabilization or failure to decline (“stabilization”) to the point where a patient is no longer deemed to be terminally ill.3,9,10
PWD, who represent a growing proportion of the hospice population,11 have an increased live discharge risk due to condition stabilization.6–8 This live discharge type most often occurs around 90 and 180 days of service, points at which hospice patients must be recertified as terminally ill. Higher rates of live discharge due to condition stabilization are partially explained by PWDs’ unclear disease trajectory and the lack of reliable prognostic tools. Neither the Palliative Performance Scale nor the FAST scale, which provide a gauge for hospice of mortality risk, have good predictive values in PWD.12 Therefore, some PWD far outlive their prognosis; others die sooner. This situation is further complicated by aggressive audits by the Office of the Inspector General towards hospices with high rates of PWD, particularly those in nursing homes.13 Due to these and other unexplored factors, PWD are frequently discharged from hospice alive because their condition stabilizes and/or fails to decline, extending their expected life span beyond six months. This is a disruptive and burdensome transition for frail, older adults and their family members. When discharged alive, patients and their family members lose support from hospice nurses, home health aides, social workers, spiritual care, and hospice-provided medical equipment, medications, and supplies. Patients and families must transition to other healthcare and service providers to fill these gaps.8
Race and ethnicity play an important role in PWDs’ experiences receiving hospice. Dementia is more prevalent amongst African Americans and Hispanics than non-Hispanic whites.14 African American and Hispanic individuals however are less likely to enroll in hospice than non-Hispanic whites.15 When they do enroll, they are more likely to be disenrolled.2,5,16 African Americans are less likely to reenroll in hospice after experiencing a live discharge.17 Thus, African American and Hispanic PWD may be at heightened risk for live discharge from hospice, the effects of which are compounded by lower hospice reenrollment rates.
Many studies have examined characteristics associated with live discharge among patients from the general hospice population.2,5,18,19 However, less is known about how demographic and health characteristics related to risk for live discharge due to condition stabilization in PWD. One large study of PWD receiving hospice from 1999–2003 indicated older age, being African American, and female were associated with live discharge due to condition stabilization.20 Moreover, few studies have examined how hospice service delivery characteristics relate to live discharge risk due to condition stabilization in PWD. Receiving home hospice16,21 and longer length of service20,22 are associated with experiencing a live discharge. The relationship between number and timing of nurse visits and live discharge is not well established, although previous studies suggest a nonlinear relationship, with more intensive service utilization at the beginning and end of hospice service.23,24
This study aims to 1) identify demographic and health correlates of live discharge due to condition stabilization in PWD, and 2) explore how hospice service delivery factors relate to this live discharge type in PWD. We focus on live discharge due to condition stabilization because of its particular importance in PWD,12 whose odds of experiencing this disenrollment type are more than 13 times greater than for patients with cancer.5 We use a sample of hospice PWD who did not die within 7 days of enrollment25–27 and did not exceed the initial six-month period for which the Medicare hospice benefit is intended. Hospice patients can receive hospice services indefinitely provided a physician certifies they are within six months of dying at two 90-day and 60-day intervals thereafter.10 However, focusing on a 7–180 day length of service eliminates individuals who experienced late referrals or exceeded the initial six-month Medicare hospice benefit period. We focus on the role of race/ethnicity as members of underrepresented racial and ethnic groups are at heightened risk for poor hospice outcomes.6,20 We extend previous research by examining the role of hospice service characteristics, including hospice location, and timing and quantity of nursing visits, as potentially modifiable factors for this type of live discharge risk among PWD. We explore nursing visits specifically because nurses comprise the largest proportion of hospice professionals and are the professional care team members with the most frequent and regular contact with all hospice patients, following the Medicare-regulated minimum of one nurse visit every fourteen days.24 Although social workers and chaplains also visit hospice patients, their contact is less regular and differentially distributed:24 non-religious patients may not receive chaplain services, social workers’ involvement depends on patients’ needs for supplementary resources, whereas nurses are well-positioned to influence hospice care plans and outcomes.
Methods
Data.
This retrospective cohort study analyzed structured fields in electronic medical records for a population of 23,526 patients who received hospice care between 2013 and 2017 from a large not-for-profit hospice agency in New York City (NYC). The agency serves an average daily census of more than 1,100 patients in all five NYC boroughs. We limited our analysis to patients age 65 and older (n=19,501), with a primary or comorbid dementia diagnosis (n=5,503). We limited the sample to patients who either died while in hospice (the intended outcome for hospice care) or experienced a live discharge from hospice due to stabilized condition (n=4,706), excluding 797 patients who disenrolled from hospice due to hospitalization, electively choosing to leave hospice, or transferring to another service area or care provider. We exclude 2,019 patients who spent less than 7 or more than 180 days in hospice (n=2,687) and 58 patients with missing data on one or more study variables. Of the final analytic sample (n=2,629), 93% (2,440) of patients died in hospice and 7% (n=189) experienced a live discharge due to condition stabilization. All study procedures were approved by the Institutional Review Boards at Weill Cornell Medicine and Visiting Nurse Service of New York.
Measures.
We measure hospice discharge reason dichotomously (died=0, live discharge due to condition stabilization=1). To measure key predictors, we included dummy variables for patient race/ethnicity (reference=non-Hispanic white), a dichotomous measure of hospice location (home=1; nursing home, long-term care facility, hospital, hospice residence=0), and continuous measures of length of service (in days), number of nurse visits, and total days between last nurse visit and hospice discharge (discharge date subtracted from date of the last nurse visit). Because prior research indicates service utilization is greater at the beginning and end of hospice service,23 we included nonlinear terms for nurse visits and time from nurse visit to discharge. We focus on nurse visits as nurses because of their frequent contact with patients and position to influence hospice care plans and outcomes.
We also controlled for patient demographic and health factors prior studies find are associated with live discharge for any reason. Demographic factors included: gender, 5,16,18,28,29 age, 18,19,29 marital and parental status, 22 and Medicaid insurance (a proxy for low income).5,29 Health factors included referral to hospice from the hospital,20,30 functional status at hospice enrollment, and comorbidities.5,31,32 Functional status was measured using responsiveness and the Palliative Performance Scale (PPS) upon admission. The PPS evaluates functional status in hospice and palliative care settings with values between 0 (death) and 100 (full health).33 Comorbidities were measured using the Charlson Comorbidity Index31 and the total number of serious illnesses (heart failure or myocardial infarction, stroke or cerebrovascular disease, pulmonary issues, cancer, HIV, liver disease, kidney problems, cancer, diabetes, rheumatic disease).
Analysis.
Descriptive statistics for the analytic sample (Table 1) were calculated. We used logistic regression models to identify risk factors for live discharge from hospice (versus death) (Table 2 and Figure 1). We tested whether nonlinear terms for hospice delivery (length of service, number of nurse visits, timing of nurse visits) resulted in significantly improved model fit using likelihood ratio tests, McFadden’s R2, and Bayesian measures (AIC and BIC) (Table 2). We graphed predicted probabilities for key findings (Figure 2). All analyses were completed using Stata/MP 15.1.34
Table 1.
Demographic and clinical characteristics for 2,629 hospice patients age 65+ with dementia in hospice for 7–180 days, overall and by discharge type
| Total sample n=2,629 % / Mean (SD) | Died n=2,440 % / Mean (SD) | Live discharge n=189 % / Mean (SD) | p value | |
|---|---|---|---|---|
| Outcome | ||||
| Live discharge due to condition stabilization | 7 | |||
| Death (reference) | 93 | |||
| Demographic/Health Characteristics | ||||
| Race/Ethnicity | 0.001a | |||
| African American | 16 | 16 | 16 | |
| Hispanic | 20 | 19 | 32 | |
| Other race/ethnicity | 9 | 9 | 7 | |
| Non-Hispanic white (reference) | 55 | 56 | 45 | |
| Female | 72 | 72 | 73 | 0.75a |
| Age (R: 65–111 years old) | 89.8 | 89.9 | 88.9 | 0.71b |
| (7.4) | (7.3) | (7.5) | ||
| Medicaid recipient | 2 | 2 | 3 | 0.55a |
| Not married | 73 | 73 | 76 | 0.35a |
| No children | 26 | 26 | 28 | 0.55a |
| Primary dementia diagnosis | 68 | 68 | 74 | 0.11a |
| Number of serious diagnoses (R: 1–4) | 2.0 | 2.0 | 2.0 | 0.15b |
| (0.4) | (0.4) | (0.4) | ||
| Charlson Score (R: 1–12) | 2.6 | 2.6 | 2.40 | 0.0000b |
| (1.5) | (1.5) | (1.0) | ||
| Palliative Performance Scale (R: 10–100) | 31.5 | 31.3 | 35.1 | 0.23b |
| (9.7) | (9.7) | (9.1) | ||
| Unresponsive | 14 | 15 | 11 | 0.18a |
| Hospital referral | 37 | 38 | 28 | 0.006a |
| Hospice Delivery Characteristics | ||||
| Home hospice | 77 | 76 | 84 | 0.01a |
| Length of service (R: 7–180 days) | 52.6 | 46.4 | 132.2 | 0.90b |
| (49.8) | (44.6) | (44.9) | ||
| Number of nurse visits (R: 1–92) | 9.9 | 9.5 | 15.4 | 0.0000b |
| (8.5) | (8.5) | (5.9) | ||
| Time from last nurse visit to discharge | 2.3 | 2.0 | 5.4 | 0.0000b |
| (R: 0–33 days) | (3.5) | (3.2) | (5.2) | |
. Chi square test.
. ANOVA . R=range. SD=standard deviation.
Table 2.
Logistic regression, live discharge risk due to condition stabilization (versus death) for 2,629 hospice patients age 65+ with dementia and hospice stays of 7–180 days
| Model 1: Demographic & Health Factors | Model 2: Model 1 + Hospice Services | Model 3: Model 2 + Nonlinear Terms | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AOR | 95% CI | p value | AOR | 95% CI | p value | AOR | 95% CI | p value | ||||
| Race/Ethnicity (ref=white) | ||||||||||||
| African American | 1.36 | 0.87 | 2.12 | 0.18 | 2.41 | 1.34 | 4.32 | 0.003 | 2.42 | 1.34 | 4.38 | 0.004 |
| Hispanic | 2.32 | 1.61 | 3.34 | 0.000 | 2.76 | 1.70 | 4.49 | 0.000 | 2.99 | 1.81 | 4.94 | 0.000 |
| Other race/ethnicity | 1.20 | 0.66 | 2.18 | 0.55 | 0.78 | 0.36 | 1.70 | 0.53 | 0.78 | 0.35 | 1.76 | 0.55 |
| Female | 1.03 | 0.71 | 1.50 | 0.89 | 1.00 | 0.62 | 1.61 | 0.99 | 1.02 | 0.62 | 1.66 | 0.95 |
| Age (years) | 0.98 | 0.96 | 1.00 | 0.04 | 0.97 | 0.94 | 1.00 | 0.03 | 0.98 | 0.95 | 1.00 | 0.09 |
| Medicaid recipient | 1.25 | 0.47 | 3.27 | 0.66 | 0.56 | 0.17 | 1.87 | 0.35 | 0.58 | 0.16 | 2.09 | 0.40 |
| Not married | 1.22 | 0.82 | 1.80 | 0.33 | 1.15 | 0.70 | 1.89 | 0.58 | 1.12 | 0.67 | 1.87 | 0.66 |
| No children | 1.26 | 0.89 | 1.76 | 0.19 | 1.58 | 1.02 | 2.46 | 0.04 | 1.53 | 0.96 | 2.42 | 0.07 |
| Primary dementia diagnosis | 1.39 | 0.90 | 2.14 | 0.14 | 1.55 | 0.89 | 2.69 | 0.12 | 1.83 | 1.03 | 3.24 | 0.04 |
| Number of serious diagnoses | 1.02 | 0.64 | 1.63 | 0.92 | 0.94 | 0.52 | 1.69 | 0.84 | 0.92 | 0.50 | 1.69 | 0.78 |
| Charlson Score | 0.88 | 0.77 | 1.00 | 0.06 | 0.90 | 0.76 | 1.08 | 0.26 | 0.92 | 0.77 | 1.10 | 0.36 |
| Palliative Performance Scale | 1.59 | 1.35 | 1.86 | 0.000 | 1.36 | 1.10 | 1.69 | 0.005 | 1.35 | 1.09 | 1.69 | 0.007 |
| Unresponsive at admission | 0.69 | 0.42 | 1.11 | 0.13 | 0.75 | 0.41 | 1.38 | 0.36 | 0.83 | 0.45 | 1.52 | 0.54 |
| Hospital referral | 0.66 | 0.47 | 0.93 | 0.02 | 0.74 | 0.48 | 1.15 | 0.18 | 0.75 | 0.48 | 1.18 | 0.22 |
| Home hospicea | 7.99 | 4.29 | 14.88 | 0.000 | 7.57 | 4.04 | 14.18 | 0.000 | ||||
| Length of service (days) | 1.05 | 1.04 | 1.05 | 0.000 | 1.04 | 1.04 | 1.05 | 0.000 | ||||
| Number of nurse (RN) visits | 0.86 | 0.82 | 0.90 | 0.000 | 1.08 | 0.93 | 1.25 | 0.31 | ||||
| RN visits squared | 0.9939 | 0.9899 | 0.9979 | 0.003 | ||||||||
| Time from last RN visit to discharge (days) | 1.15 | 1.10 | 1.20 | 0.000 | 1.86 | 1.56 | 2.21 | 0.000 | ||||
| Timing squared | 0.96 | 0.94 | 0.97 | 0.000 | ||||||||
| Timing cubed | 1.0009 | 1.0005 | 1.0014 | 0.000 | ||||||||
| McFadden’s R2 | 0.05 | 0.46 | 0.49 | |||||||||
| AIC / BIC | 1317.90 / 1406.01 | 775.89 / 887.50 | 735.26 / 864.50 | |||||||||
. Reference category=patients receiving hospice care in nursing homes, long-term care facilities, hospitals, or residential hospice facilities. AOR=adjusted odds ratio. CI=confidence interval. Bolded results indicate adjusted odds ratios with p values<0.05.
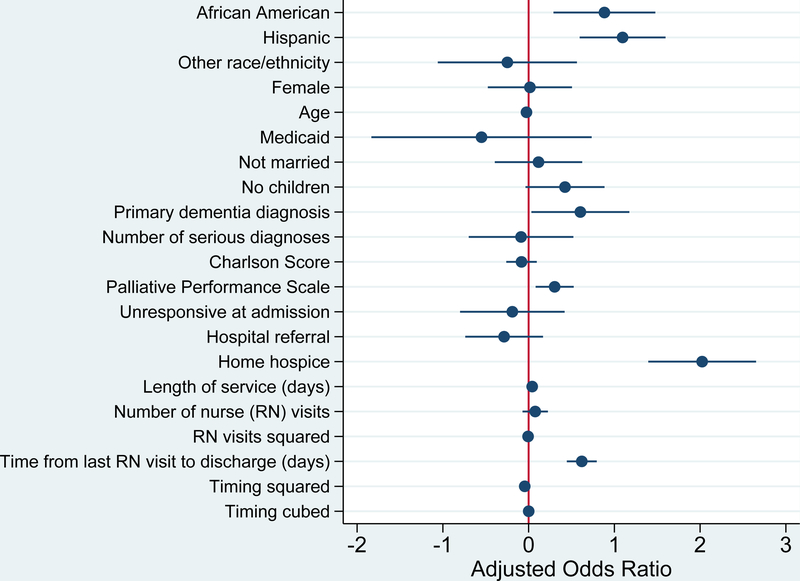
Figure 1.
Forest plot of live discharge due to condition stabilization (versus death) for 2,693 hospice patients with dementia: adjusted odds ratios and 95% confidence intervals from Table 2, Model 3.
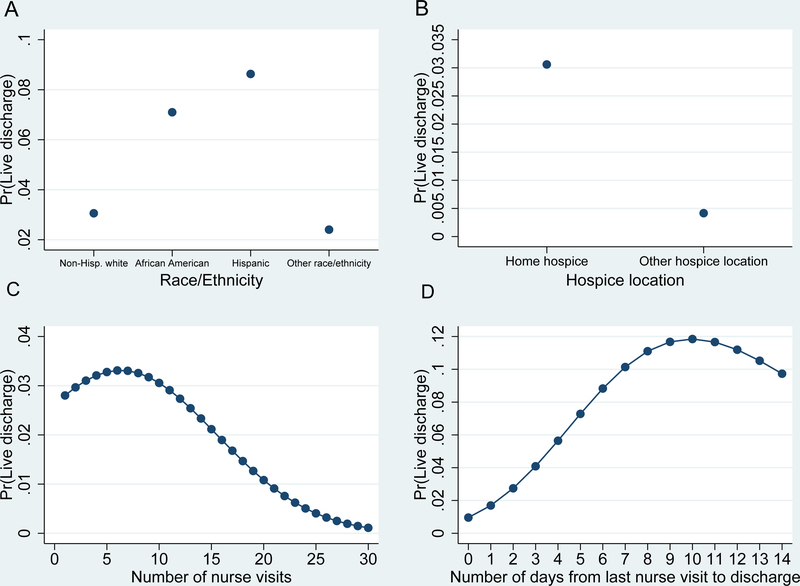
Figure 2.
Predicted probabilities of hospitalization by race/ethnicity (A), hospice location (B), number of nurse visits (C), and days between last nurse visit and discharge (D).
Note: Models hold demographic, clinical, and hospice service characteristics from Table 1 at model (for categorical variables) and mean (for continuous variables) values.
Results
Table 1 shows descriptive statistics for the analytic sample, deceased patients, and those discharged alive. In our sample, 7% of PWD experienced live discharge. Deceased hospice patients and those discharged alive did not differ on most sociodemographic and health characteristics. Overall, patients were most often female (72%), without Medicaid (98%), were not currently married (73%), and were parents (74%). Hispanic patients represented a larger proportion of the patients discharged alive than the deceased (32% vs 19%). Patients were diagnosed with an average of 2 serious illnesses and did not differ on functional status measures in a clinically meaningful way.35 Patients discharged alive were referred from hospitals less often and received home hospice more often than deceased patients (hospital referrals: 28% vs 38%, p=0.006; home hospice: 84% vs 76%, p=0.01). On average, patients discharged alive had a longer length of service (132 vs 46 days, p=0.000) and received more nurse visits than deceased patients (15.4 vs 9.5, p=0.000). More days passed between the last nurse visit and discharge date for patients discharged alive than deceased patients (5.4 vs 2.0, p=0.000).
Table 2 presents results from multivariable logistic regression models showing live discharge odds from hospice due to condition stabilization, controlling for patient demographic and clinical factors (Model 1), hospice service characteristics (Model 2) and significant nonlinear hospice service characteristics (Model 3). Figure 1 graphs the results from Model 3. AIC and BIC statistics were lowest and McFadden’s R2 was highest for Model 3, indicating this model best fits the data. Race/ethnicity and functional status significantly predicted live discharge across all models. In Model 3, African American and Hispanic patients had 142% and 199% higher odds of experiencing a live discharge compared to non-Hispanic whites (African American: AOR=2.42, 95%CI=1.34, 4.38; Hispanic: AOR=2.99, 95%CI=1.81, 4.94). Holding all other covariates at mean (for continuous) and modal (for categorical) values, African American and Hispanic patients had 0.07 and 0.09 predicted probabilities of hospitalization, respectively, compared to only 0.03 among non-Hispanic whites (Figure 2a). Having a primary (versus comorbid) dementia diagnosis was associated with increased live discharge odds (AOR: 1.83, 95%CI: 1.03, 3.24). For every ten-point increase on the PPS, patients’ live discharge odds increased by 35% (AOR=1.35, 95%CI=1.09, 1.69).
Hospice service provision factors were also strongly associated with live discharge due to condition stabilization. Home hospice patients had 657% higher odds of live discharge than hospice patients in other settings including nursing homes and inpatient facilities (AOR=7.57, 95% CI=4.04, 14.18). Each additional day of hospice service increased live discharge odds by 4% (AOR=1.04, 95% CI=1.04, 1.05). Number of nurses’ visits and days from the last nurse visit to hospice discharge date were also associated with live discharge risk. Notably, these factors had a nonlinear relationship to live discharge. For nurses’ visits, the live discharge risk increased as the number of nurses’ visits increased until 6 visits were completed. After 6 visits, the live discharge risk decreased (Figure 2c). As the total days between the last nurse visit and discharge increased from 0 to 6, live discharge risk also increased. From 6–14 days between the last nurse visit and discharge, live discharge risk reduced slightly, and then increased again at more than 14 days (Figure 2d).
Discussion
Live discharge from hospice is a burdensome and disruptive transition for PWD and their caregivers. Family members may need to resume caregiving responsibilities once hospice services cease and adjust to the idea there loved one is no longer considered “terminally” ill.36 In a sample of PWD age 65 and older with hospice stays of 7–180 days, our findings identify subsets of PWD most vulnerable to live discharge due to condition stabilization: African American and Hispanic patients, and those who receive home hospice care. These findings are concerning, given that African American patients who disenroll from hospice return to hospice at lower rates,17 a pattern we observed in supplementary analyses. Moreover, hospice care is most often home-based: 56% of hospice care is home-based and 45% of hospice patients die at home.15
Although these results concur with prior studies of general hospice patient populations,2,5,16 reasons for this disparity are unclear and not linked to hospice-level effects.37 One explanation is that African American and Hispanic hospice patients receive systematically different care than non-Hispanic whites. However, supplementary analyses revealed no significant racial/ethnic differences in service use among PWD discharged alive: PWD who experienced a live discharge received nurse visits in similar numbers and frequency, regardless of race/ethnicity. Alternatively, because African American individuals live longer with dementia than non-Hispanic whites,38 their end-of-life trajectory may be more protracted, increasing their risk of becoming ineligible for hospice once enrolled. African American hospice patients’ family members may not advocate for continuous hospice care when live discharge looms due to misconceptions of hospice or negative attitudes towards hospice services.39
Alternatively, higher live discharge rates due to condition stabilization among African American and Hispanic PWD may result from systematic differences in hospice referral patterns and access to clinical services. In these data African American and Hispanic patients were referred from a hospital more often than non-Hispanic whites. African American and Hispanic patients are less likely to have a regular care source.40–42 Referrals from hospital physicians caring for acutely ill PWD, who may be unable to consult with a physician familiar with the patient’s condition and trajectory, may lead to premature hospice referrals among these groups.
While more than one-third of patients in our study population were referred to hospice from the hospital, over half of African American and Hispanic patients were referred to hospice from non-hospital sources including home care agencies and primary care physicians. Physicians and other clinicians that refer African American and Hispanic patients to hospice outside of a hospital setting may be less familiar with end-of-life trajectories in dementia and/or individual patients’ health trajectories, have a poor understanding of hospice care, and/or be unable to connect their patients with palliative care services. African Americans also comprise a disproportionate share of nursing home residents overall (a pattern we observed) and often live in poorer performing nursing homes,46 where staff may not be well-trained in making appropriate hospice referrals. As a result of referrals from hospital physicians unfamiliar with PWDs trajectories or referrals from community and nursing home clinicians with less training and/or knowledge about hospice, patients from underrepresented racial/ethnic groups may receive premature referrals to hospice. Future research should examine the decision-making process behind referring PWD to hospice to identify areas for improvement. To the extent premature referrals contribute to racial/ethnic disparities in hospice care, improving knowledge regarding end-stage dementia and hospice services among non-geriatric clinicians may result in fewer premature referrals to hospice care. Alternatively, although hospices have thorough screening and intake procedures in place, the trajectory of PWD may be affected if an acute episode prompted hospitalization and hospice admission, and the PWD’s condition subsequently stabilized during their hospice stay. If live discharge is unavoidable, PWD and family members may require additional support to transition smoothly to needed services.47 Additionally, PWD may benefit from monitoring for a period after live discharge to encourage a timely readmission when their condition worsens.48
We found that individuals receiving home hospice care were over 7 times as likely to be discharged alive as those receiving hospice in other settings such as nursing homes and hospice inpatient facilities. In these data, home hospice patients had higher functioning levels upon hospice enrollment, and so may have been more likely to demonstrate stability or failure to decline in their condition with the addition of hospice services such as home health aides, medication, medical supplies and equipment, and social work. Physicians may also refer seriously ill, community-dwelling patients to hospice earlier in their illness trajectory. The earlier referrals for hospice-eligible patients may afford the time needed to obtain additional support and services for which patient with limited economic resources might otherwise not be eligible. Physicians may recommend hospice for additional support to help patients with limited social or caregiving resources remain safely and comfortably at home as their illness progresses. In both instances, additional support from hospice may result in stabilization and/or failure to decline in patients’ conditions, leading to live discharge. Education about appropriate hospice referrals, careful screening of potential home hospice patients to determine eligibility and linking community dwelling patients to alternative programs such as Medicaid could help PWD get the services they need until they become hospice eligible.
The relationship between fewer nurse visits and increased probability of live discharge held even when controlling for length of service and was increasingly pronounced until 6 nursing visits were completed. Given that care plans, which are tailored to individual patient needs, often stipulate nurses visit a relatively stable hospice patient every two weeks, these first 6 visits might naturally coincide with the 90-day point at which the hospice team is required to reevaluate the patient’s hospice eligibility. If a patient’s condition has remained stable or failed to decline during that period, their life expectancy may extend beyond six months, resulting in live discharge from hospice under current Medicare eligibility requirements. Indeed, supplementary analysis revealed a spike in live discharge at 85–89 days of service, which may help explain the relationship between the number of nurse visits and live discharge risk due to condition stabilization.
Condition stabilization or failure to decline is a common reason for live discharge.3,9,49 However, prior research indicates that once patients enroll in hospice, it is optimal for them to remain until death for various reasons. Stabilization or failure to decline in condition is often a temporary state. One-third of discharged patients die within six months of hospice disenrollment,49 suggesting they could have benefitted from continued hospice services. Moreover, patients who experience a live discharge can face barriers to re-enrollment. Only a quarter of patients discharged alive eventually return to hospice,17 and one-third were discharged alive who die within six months do so without hospice readmission. Hospice readmission rates are even lower among African American patients,17 which is alarming given they had increased risk for experiencing live discharge. Supplementary data analysis revealed a significantly lower reenrollment rate among African American and Hispanic patients compared to non-Hispanic whites. Allowing hospices to delay discharge for PWD whose condition stabilizes for an extended observation period to see if stabilization in condition is sustained may allow hospices to avoid discharging patients who show a failure to decline, but for whom that stabilization proves to be temporary. However, this change would be required at the policy level, as hospice providers currently are not allowed to recertify hospice patients who do not demonstrate a decline in condition within a given certification period. Given that end-of-life prognostication for PWD is incredibly difficult, even for clinicians with substantial experience with this population, live discharges among PWD are likely to continue as long as stable condition leads to disenrollment.
In addition to number, we found that the timing of nurse visits is correlated with live discharge from hospice. As the total days between the last nurse visit and discharge date increases, so does live discharge risk due to condition stabilization. Probability of discharge from hospice on the same day a nurse visits was low: 1%. However, this probability increased to over 13% when ten days passed since the last nurse visit. This relationship was independent of total number of nurse visits and length of service. More days between nurse visits and live discharge may reflect reduced patient need for nursing services if their conditions stabilized or failed to decline. Alternatively, the plan of care, tailored to individual patient needs, for discharge planning may stipulate a nurse visit two weeks prior to discharge, helping to explain the increase live discharge risk as the time between nurse visit and hospice discharge increases.
This study has limitations. First, it relies on data from a single, non-profit hospice agency in the northeast, and so results may not be generalizable to other hospices. Second, observed racial and ethnic differences may be associated with socioeconomic status. While we controlled for Medicaid status as a proxy for low income, we were unable to account for other aspects of socioeconomic status, such as education and wealth, which may influence interactions with healthcare and hospice providers.50 Third, the electronic data we analyzed does not provide detailed information about reasons for live discharge due to condition stabilization. Future research should explore social processes and other mechanisms underlying live discharge from hospice due to condition stabilization. For example, the availability of family caregivers, may facilitate symptom management and communication with hospice clinicians, helping to keep PWD comfortable and safe at home.
Conclusion.
Our analysis identified racial/ethnic disparities in live discharge risk from hospice due to condition stabilization among PWD: African American and Hispanic PWD had increased live discharge risk. PWD receiving home hospice care also had increased live discharge risk. Improving education about end-stage dementia and hospice services among clinicians making hospice referrals may reduce the number of premature referrals. Policy regarding hospice eligibility should be aligned to allow hospices to better address end of life for PWD, which is characterized by difficult prognostication and a protracted decline including periods of stabilization or temporary failure to decline. Future research could inform the ways in which the Medicare hospice benefit may be adapted to meet the needs of hospice PWD.
Acknowledgements
The authors would like to thank Rosemary Baughn and Bonnie Lauder for their contributions to this article. Elizabeth Luth's work on this grant was supported by T32 AG049666.
Sponsor’s Role. Not applicable.
Footnotes
Conflict of Interest. The authors have no conflicts to report.
References
- 1.Prsic E, Plotzke M, Christian TJ, Gozalo P, Teno JM. A National Study of Live Hospice Discharges between 2000 and 2012. J Palliat Med. 2016;19(9):987–990. [DOI] [PubMed] [Google Scholar]
- 2.Teno JM, Plotzke M, Gozalo P, Mor V. A National Study of Live Discharges from Hospice. J Palliat Med. 2014;17(10):1121–1127. [DOI] [PubMed] [Google Scholar]
- 3.Wu S, Volker DL. Live Discharge From Hospice: A Systematic Review. Journal of hospice and palliative nursing: JHPN: the official journal of the Hospice and Palliative Nurses Association. 2019. [DOI] [PubMed] [Google Scholar]
- 4.Taylor DH Jr, Steinhauser K, Tulsky JA, Rattliff J, Van Houtven CH. Characterizing hospice discharge patterns in a nationally representative sample of the elderly, 1993–2000. Am J Hospice Palliat Med. 2008;25(1):9–15. [DOI] [PubMed] [Google Scholar]
- 5.Russell D, Diamond EL, Lauder B, et al. Frequency and Risk Factors for Live Discharge from Hospice. J Am Geriatric Soc. 2017;65(8):1726–1732. [DOI] [PubMed] [Google Scholar]
- 6.Unroe KT, Greiner MA, Johnson KS, Curtis LH, Setoguchi S. Racial differences in hospice use and patterns of care after enrollment in hospice among Medicare beneficiaries with heart failure. Am Heart J. 2012;163(6):987–993.e983. [DOI] [PubMed] [Google Scholar]
- 7.Watson Campbell R Being Discharged from Hospice Alive: The Lived Experience of Patients and Families. J Palliat Med. 2015;18(6):495–499. [DOI] [PubMed] [Google Scholar]
- 8.Wladkowski SP. Dementia Caregivers and Live Discharge from Hospice: What Happens When Hospice Leaves? J Gerontol Soc Work. 2017;60(2):138–154. [DOI] [PubMed] [Google Scholar]
- 9.Dolin R, Holmes GM, Stearns SC, et al. A positive association between hospice profit margin and the rate at which patients are discharged before death. Health Affairs. 2017;36(7):1291–1298. [DOI] [PubMed] [Google Scholar]
- 10.Services CfMM. Medicare, Benefit Policy Manual Chapter 9. Coverage of Hospice Services under Hospital Insurance. Baltimore, MD 2018. [Google Scholar]
- 11.Aldridge MD, Canavan M, Cherlin E, Bradley EH. Has Hospice Use Changed? 2000–2010 Utilization Patterns. Med Care. 2015;53(1):95–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harris PS, Stalam T, Ache KA, et al. Can Hospices Predict which Patients Will Die within Six Months? J Palliat Med. 2014;17(8):894–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Health USDo, General HSOoI, Levinson DR. Medicare hospices that focus on nursing facility residents. Department of Health and Human Services; 2011. [Google Scholar]
- 14.Association As. 2018 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia. 2018;14(3):367–429. [Google Scholar]
- 15.National Hospice and Palliative Care O. NHPCO Facts and Figures: Hospice Care in America, 2017 Edition. Alexandria, VA: NHPCO; March 2018. [Google Scholar]
- 16.Ankuda CK, Fonger E, O’Neil T. Electing Full Code in Hospice: Patient Characteristics and Live Discharge Rates. J Palliat Med. 2018;21(3):297–301. [DOI] [PubMed] [Google Scholar]
- 17.Kapo J, Macmoran H, Casarett D. “Lost to Follow-up”: Ethnic Disparities in Continuity of Hospice Care at the End of Life. J Palliat Med. 2005;8(3):603–608. [DOI] [PubMed] [Google Scholar]
- 18.De Vleminck A, Morrison RS, Meier DE, Aldridge MD. Hospice Care for Patients With Dementia in the United States: A Longitudinal Cohort Study. J Am Med Dir Assoc. 2018;19(7):633–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang S- Y, Aldridge MD, Gross CP, et al. Transitions Between Healthcare Settings Among Hospice Enrollees at the End of Life. J Am Geriatric Soc. 2016;64(2):314–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johnson KS, Elbert-Avila K, Kuchibhatla M, Tulsky JA. Characteristics and Outcomes of Hospice Enrollees with Dementia Discharged Alive. J Am Geriatric Soc. 2012;60(9):1638–1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.MacKenzie MA, Smith-Howell E, Bomba PA, Meghani SH. Respecting Choices and Related Models of Advance Care Planning: A Systematic Review of Published Evidence. Am J Hospice Palliat Med®. 2017;0(0):1049909117745789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kutner JS, Blake M, Meyer SA. Predictors of live hospice discharge: Data from the National Home and Hospice Care Survey (NHHCS). Am J Hospice Palliat Med. 2002;19(5):331–337. [DOI] [PubMed] [Google Scholar]
- 23.Stearns SC, Sheingold S, Zuckerman RB. Explaining variation in hospice visit intensity for routine home care. Med Care. 2014;52(1):56–62. [DOI] [PubMed] [Google Scholar]
- 24.Bogasky S, Sheingold S, Stearns SC. Medicare’s hospice benefit: analysis of utilization and resource use. Medicare Medicaid Res Rev. 2014;4(2):mmrr2014–2004-2002-b2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson KS, Kuchibhatla M, Tulsky JA. Racial differences in location before hospice enrollment and association with hospice length of stay. J Am Geriatric Soc. 2011;59(4):732–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rickerson E, Harrold J, Kapo J, Carroll JT, Casarett D. Timing of Hospice Referral and Families’ Perceptions of Services: Are Earlier Hospice Referrals Better? J Am Geriatric Soc. 2005;53(5):819–823. [DOI] [PubMed] [Google Scholar]
- 27.Teno JM, Casarett D, Spence C, Connor S. It Is “Too Late” or Is It? Bereaved Family Member Perceptions of Hospice Referral When Their Family Member Was on Hospice for Seven Days or Less. J Pain Symp Manage. 2012;43(4):732–738. [DOI] [PubMed] [Google Scholar]
- 28.Dolin R, Silberman P, Kirk DA, et al. Do Live Discharge Rates Increase as Hospices Approach Their Medicare Aggregate Payment Caps? J Pain Symp Manage. 2018;55(3):775–784. [DOI] [PubMed] [Google Scholar]
- 29.Casarett DJ, Marenberg ME, Karlawish JHT. Predictors of Withdrawal from Hospice. J Palliat Med. 2001;4(4):491–497. [DOI] [PubMed] [Google Scholar]
- 30.Carrion IV, Park NS, Lee BS. Hospice Use Among African Americans, Asians, Hispanics, and Whites: Implications for Practice. Am J Hospice Palliat Med®. 2011;29(2):116–121. [DOI] [PubMed] [Google Scholar]
- 31.Quan H, Li B, Couris CM, et al. Updating and Validating the Charlson Comorbidity Index and Score for Risk Adjustment in Hospital Discharge Abstracts Using Data From 6 Countries. Am J Epidemiol. 2011;173(6):676–682. [DOI] [PubMed] [Google Scholar]
- 32.Head B, Ritchie CS, Smoot TM. Prognostication in hospice care: can the palliative performance scale help? J Palliat Med. 2005;8(3):492–502. [DOI] [PubMed] [Google Scholar]
- 33.Anderson F, Downing GM, Hill J, Casorso L, Lerch N. Palliative Performance Scale (PPS): A New Tool. J Palliat Care. 1996;12(1):5–11. [PubMed] [Google Scholar]
- 34.Stata/MP 15.1 for Windows [computer program]. Version 15.1. College Station, TX 2019.
- 35.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of chronic diseases. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 36.Wladkowski SP. Live Discharge from Hospice and the Grief Experience of Dementia Caregivers. J Soc Work End of Life Palliat Care. 2016;12(1–2):47–62. [DOI] [PubMed] [Google Scholar]
- 37.Rizzuto J, Aldridge MD. Racial Disparities in Hospice Outcomes: A Race or Hospice-Level Effect? J Am Geriatric Soc. 2018;66(2):407–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Farina MP, Hayward MD, Kim JK, Crimmins EM. Racial and Educational Disparities in Dementia and Dementia-Free Life Expectancy. J Gerontol: Series B 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dillon PJ, Basu A. African Americans and Hospice Care: A Culture-Centered Exploration of Enrollment Disparities. Health Comm. 2016;31(11):1385–1394. [DOI] [PubMed] [Google Scholar]
- 40.Ryvicker M, Russell D. Individual and Environmental Determinants of Provider Continuity Among Urban Older Adults With Heart Failure: A Retrospective Cohort Study. Gertontol Geriatric Med. 2018;4:2333721418801027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gaskin DJ, Arbelaez JJ, Brown JR, Petras H, Wagner FA, Cooper LA. Examining racial and ethnic disparities in site of usual source of care. J Nat Med Assoc. 2007;99(1):22–30. [PMC free article] [PubMed] [Google Scholar]
- 42.Arnett MJ, Thorpe RJ, Gaskin DJ, Bowie JV, LaVeist TA. Race, Medical Mistrust, and Segregation in Primary Care as Usual Source of Care: Findings from the Exploring Health Disparities in Integrated Communities Study. J Urban Health. 2016;93(3):456–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary Care Physicians Who Treat Blacks and Whites. New Engl J Med. 2004;351(6):575–584. [DOI] [PubMed] [Google Scholar]
- 44.Burgess DJ. Are Providers More Likely to Contribute to Healthcare Disparities Under High Levels of Cognitive Load? How Features of the Healthcare Setting May Lead to Biases in Medical Decision Making. Med Decision Making. 2009;30(2):246–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Varkey AB, Manwell LB, Williams ES, et al. Separate and Unequal: Clinics Where Minority and Nonminority Patients Receive Primary Care. JAMA Intern Med. 2009;169(3):243–250. [DOI] [PubMed] [Google Scholar]
- 46.Smith DB, Feng Z, Fennell ML, Zinn JS, Mor V. Separate And Unequal: Racial Segregation And Disparities In Quality Across U.S. Nursing Homes. Health Affairs. 2007;26(5):1448–1458. [DOI] [PubMed] [Google Scholar]
- 47.Wladkowski SP, Wallace CL. Current Practices of Live Discharge from Hospice: Social Work Perspectives. Health Soc Work. 2018;44(1):30–38. [DOI] [PubMed] [Google Scholar]
- 48.Feld A, Madden-Baer R, McCorkle R. Evolution of a 90-day model of care for bundled episodic payments for congestive heart failure in home care. Home Health Care Services Quarterly. 2016;35(2):53–68. [DOI] [PubMed] [Google Scholar]
- 49.Kutner JS, Meyer SA, Beaty BL, Kassner CT, Nowels DE, Beehler C. Outcomes and Characteristics of Patients Discharged Alive from Hospice. J Am Geriatric Soc. 2004;52(8):1337–1342. [DOI] [PubMed] [Google Scholar]
- 50.Dubbin LA, Chang JS, Shim JK. Cultural health capital and the interactional dynamics of patient-centered care. Soc Sci Med. 2013;93:113–120. [DOI] [PMC free article] [PubMed] [Google Scholar]