Dear Editor,
Approximately 422 million individuals have diabetes mellitus worldwide (1). The most widely accepted risk factor for type 2 diabetes mellitus (T2DM), and the focus of much of the research attention, is excess body weight (2). Age is also a risk factor for diabetes (3) and consequently, some (4) but not all (5) practice guidelines incorporate an age threshold as an independent criteria for performing clinical diabetes screening. However, the degree to which aging impacts the risk of diabetes across the BMI spectrum, in particular the magnitude of the aging effect in those with a normal BMI in whom obesity is not a contributing factor, has not been well described. This provided rationale to revisit the dynamics of the effect of aging on T2DM as a function of BMI (6).
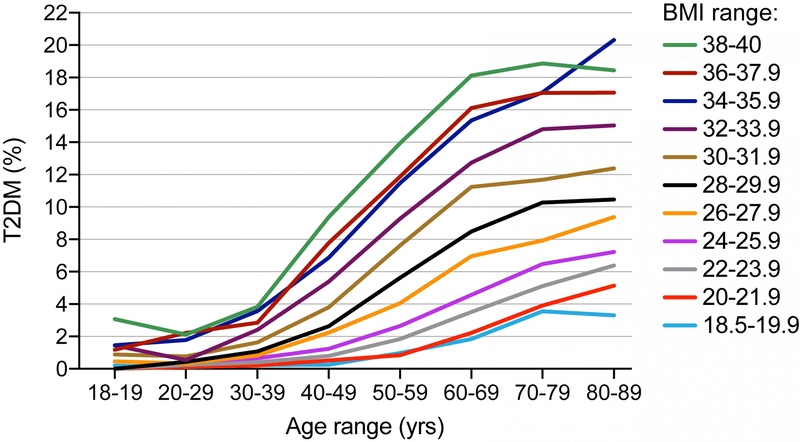
We examined the effect of age on the prevalence of T2DM within narrow BMI ranges, using the patient database registry at a large academic health system [the Research Patient Data registry (RPDR) of Partners HealthCare System]. The Partners HealthCare institutional review board approved this study and informed consent was waived. We included adult patients between the ages of 18–90 years with a BMI between 18.5–40 kg/m2 who were seen within the health system between 1/1/2016 and 12/31/2016. The study population consisted of 296,824 patients, divided into groups based on age (18–19 years, 20–29 years, 30–39 years, 40–49 years, 50002D59 years, 60–69 years, 70–79 years and 80–90 years) and BMI (18.5–19.99 kg/m2; 20–21.99 kg/m2; 22–23.99 kg/m2; 24–25.99 kg/m2; 26–27.99 kg/m2; 28–29.99 kg/m2; 30–31.99 kg/m2; 32–33.99 kg/m2; 34–35.99 kg/m2; 36–37.99 kg/m2; 38–40 kg/m2). We calculated the prevalence of T2DM within each age and BMI group, using ICD 10 diagnosis codes for T2DM. We found a significant increase in prevalence of T2DM with age (p<0.0001 using log-linear Poisson regression), inclusive of BMI groups in the normal range (Figure 1). The aging effect was particularly evident after 40 years of age, at which time there was a statistically significant inflection point (p<0.0001, Poisson regression). As a consequence of the aging effect, individuals older than 70 with a normal BMI have a similar prevalence of T2DM relative to those in their 30’s with a BMI at the high end of the obese range.
Figure 1: Type 2 diabetes mellitus prevalence as a function of age.
The prevalence of type 2 diabetes mellitus (T2DM) was determined using ICD 10 codes in a patient database registry at a large academic health system limited to patients seen in 2016 (n=296,824). The prevalence is shown within narrow BMI categories and as a function of decade of adult life through the 9th decade, revealing a significant effect of age on T2DM prevalence inclusive of those with a BMI in the normal range (log-linear Poisson regression, p<0.0001). A significant inflection point between the 4th and 5th decades is also evident (p<0.0001, Poisson regression).
Much of the public health and research focus surrounding the diabetes epidemic has centered on modifiable risk attributable to a Western lifestyle and obesity. We hypothesized that the effect of age is an important and underappreciated risk factor for T2DM whose magnitude has been difficult to quantify. Our analysis of a large database registry allowed us to quantify the effect of age within narrow BMI ranges, thereby demonstrating a powerful and consistent effect of aging on prevalence of T2DM, even in individuals with a low-normal BMI. One limitation of our study is the utilization of an ICD 10 diagnosis code to identify T2DM cases, which may have resulted in both under-reporting of T2DM cases and also over-reporting, for example patients being classified as having T2DM but instead having an autoimmune cause of diabetes mellitus such as latent autoimmune diabetes in adults (LADA). A second limitation is that we did not control for additional covariates. We assumed, however, that our large population size inclusive of all individuals with a BMI between 18.5–40 kg/m2 and the fact that we controlled for BMI - a key mediator of the effects of other potential factors influencing prevalence of T2DM - would minimize the effect of other covariates on our central observation of an aging effect across the BMI spectrum.
Although the prevalence of T2DM is increasing, predominantly due to excess weight (7), these data illustrate that 1) lowering the rates of obesity will not eliminate the incidence of T2DM, especially as the average life expectancy increases and 2) T2DM is a heterogeneous syndrome. Indeed, our data suggest that aging may augment T2DM risk through pathophysiological mechanisms independent of obesity. This underscores the unmet need for further research on the mechanisms of the age-associated increase in the prevalence of T2DM, which may reveal novel avenues for therapeutic development. Finally, these data also provide important additional support for the recommendation to screen all patients above a given age-threshold for T2DM and not only those who are overweight or obese (4).
Acknowledgements
Funding Sources: Harvard Catalyst/The Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award UL 1TR002541). The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic healthcare centers, or the National Institutes of Health.
Footnotes
Disclosure Statement: The authors have no conflicts of interest to declare.
References:
- 1.World Health Organization. Global Report on Diabetes. 2016.
- 2.Eckel RH, Kahn SE, Ferrannini E, Goldfine AB, Nathan DM, Schwartz MW, et al. Obesity and type 2 diabetes: what can be unified and what needs to be individualized? J Clin Endocrinol Metab. 2011;96(6):1654–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Caspersen CJ, Thomas GD, Boseman LA, Beckles GL, Albright AL. Aging, diabetes, and the public health system in the United States. Am J Public Health. 2012;102(8):1482–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Diabetes Association. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S13–S28. [DOI] [PubMed] [Google Scholar]
- 5.Siu AL, United States Preventive Services Task Force. Screening for Abnormal Blood Glucose and Type 2 Diabetes Mellitus: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2015;163(11):861–8. [DOI] [PubMed] [Google Scholar]
- 6.Amati F, Dube JJ, Coen PM, Stefanovic-Racic M, Toledo FG, Goodpaster BH. Physical inactivity and obesity underlie the insulin resistance of aging. Diabetes Care. 2009;32(8):1547–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Menke A, Rust KF, Fradkin J, Cheng YJ, Cowie CC. Associations between trends in race/ethnicity, aging, and body mass index with diabetes prevalence in the United States: a series of cross-sectional studies. Ann Intern Med. 2014;161(5):328–35. [DOI] [PubMed] [Google Scholar]